Primary Malignant Melanoma of the Cervical Spinal ... - E-kjs.org
Primary Malignant Melanoma of the Cervical Spinal ... - E-kjs.org
Primary Malignant Melanoma of the Cervical Spinal ... - E-kjs.org
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
CASE REPORT<br />
Kor J Spine 6(1):40-42, 2009<br />
<strong>Primary</strong> <strong>Malignant</strong> <strong>Melanoma</strong> <strong>of</strong> <strong>the</strong> <strong>Cervical</strong><br />
<strong>Spinal</strong> Nerve Root<br />
- A Case Report -<br />
Byoung Ill Roh, M.D., Jin Woo Hur, M.D., Jong Joo Rhee, M.D., Hyun Koo Lee, M.D.<br />
Department <strong>of</strong> Neurosurgery, Cheongju Saint Mary's Hospital, Cheongju, Korea<br />
<strong>Primary</strong> malignant melanoma <strong>of</strong> <strong>the</strong> nervous system is a rare disease, and accounts for only 1% <strong>of</strong> melanoma cases.<br />
<strong>Primary</strong> melanomas on <strong>the</strong> spinal nerve root, particulary <strong>the</strong> cervical spinal nerve root, are extremely rare. Only a few<br />
cases <strong>of</strong> primary melanoma arising from <strong>the</strong> spinal nerve root have been reported. We report our experience with a case<br />
<strong>of</strong> primary malignant melanoma <strong>of</strong> <strong>the</strong> cervical spinal nerve root.<br />
Key Words: <strong>Malignant</strong> melanoma ․ <strong>Cervical</strong> spine<br />
INTRODUCTION<br />
<strong>Malignant</strong> melanoma <strong>of</strong> <strong>the</strong> central nervous system is well<br />
known as a result <strong>of</strong> <strong>the</strong> relatively high frequency <strong>of</strong> cerebral<br />
metastases. <strong>Primary</strong> melanotic tumor <strong>of</strong> <strong>the</strong> nervous system have<br />
also been described, as have benign melanocytic tumors 3,6,12) .<br />
<strong>Primary</strong> malignant melanoma <strong>of</strong> <strong>the</strong> nervous system is a rare<br />
disease, and accounts for only 1% <strong>of</strong> melanoma cases. Melanocytoma<br />
is distinguished from melanoma based on <strong>the</strong> histological<br />
findings and clinical behavior. In <strong>the</strong> spinal region,<br />
several reports and studies <strong>of</strong> meningeal melanocytoma, melanotic<br />
schwannoma, and intramedullary melanoma have been<br />
reported, but only a few cases <strong>of</strong> primary malignant melanoma<br />
limited to cervical spinal nerve root have been described.<br />
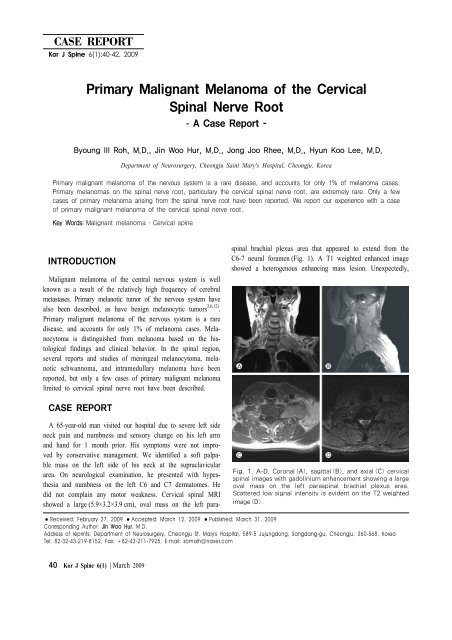
spinal brachial plexus area that appeared to extend from <strong>the</strong><br />
C6-7 neural foramen (Fig. 1). A T1 weighted enhanced image<br />
showed a heterogenous enhancing mass lesion. Unexpectedly,<br />
CASE REPORT<br />
A 65-year-old man visited our hospital due to severe left side<br />
neck pain and numbness and sensory change on his left arm<br />
and hand for 1 month prior. His symptoms were not improved<br />
by conservative management. We identified a s<strong>of</strong>t palpable<br />
mass on <strong>the</strong> left side <strong>of</strong> his neck at <strong>the</strong> supraclavicular<br />
area. On neurological examination, he presented with hypes<strong>the</strong>sia<br />
and numbness on <strong>the</strong> left C6 and C7 dermatomes. He<br />
did not complain any motor weakness. <strong>Cervical</strong> spinal MRI<br />
showed a large (5.9×3.2×3.9 cm), oval mass on <strong>the</strong> left para-<br />
Fig. 1. A-D, Coronal (A), sagittal (B), and axial (C) cervical<br />
spinal images with gadolinium enhancement showing a large<br />
oval mass on <strong>the</strong> left paraspinal brachial plexus area.<br />
Scattered low signal intensity is evident on <strong>the</strong> T2 weighted<br />
image (D).<br />
● Received: February 27, 2009 ● Accepted: March 12, 2009 ● Published: March 31, 2009<br />
Corresponding Author: Jin Woo Hur, M.D.<br />
Address <strong>of</strong> reprints: Department <strong>of</strong> Neurosurgery, Cheongju St. Mary's Hospital, 589-5 Jujungdong, Sangdang-gu, Cheongju, 360-568, Korea<br />
Tel: 82-32-43-219-8152, Fax: +82-43-211-7925, E-mail: somalh@naver.com<br />
40 Kor J Spine 6(1) March 2009
<strong>Primary</strong> <strong>Malignant</strong> <strong>Melanoma</strong> <strong>of</strong> <strong>the</strong> <strong>Cervical</strong> <strong>Spinal</strong> Nerve Root<br />
Fig. 2. <strong>Malignant</strong> melanoma composed <strong>of</strong> highly anaplastic cells with hyperchromaic nuclei, abundant<br />
eosinophilic cytoplasm, and melanin pigments (×200) (A). Positive findings for vimentin, s-100 protein,<br />
and HMB-45 (×200) (B).<br />
scattered low signal intensity lesions within <strong>the</strong> mass were<br />
identified on <strong>the</strong> T2 weighted image; <strong>the</strong>se were thought to be<br />
due to <strong>the</strong> presence <strong>of</strong> melanin, later (Fig. 1). Preoperative clini<br />
cal and radiographic diagnosis was nerve sheath tumor such as<br />
neur<strong>of</strong>ibroma or schwannoma. An operation using <strong>the</strong> anterolateral<br />
approach at left supraclavicular area between <strong>the</strong> carotid<br />
sheath and sternocleidomastoid muscle was performed. The<br />
bulk <strong>of</strong> <strong>the</strong> mass was removed. At surgery an encapsulated pitch<br />
black mass was found. It was large, firmly attached to brachial<br />
plexus and C6-7 neural foramen. Pathological examination confirmed<br />
<strong>the</strong> diagnosis <strong>of</strong> malignant melanoma. It is composed <strong>of</strong><br />
highly anaplastic cells with hyperchromaic nuclei, abundant<br />
eosinophilic cytoplasm, and melanin pigments. And it presented<br />
positive findings for vimentin, s-100 protein, and HMB-45<br />
(Fig. 2). The tumor had a high Ki-67 labeling index (35%). The<br />
patient’s symptoms improved totally after <strong>the</strong> operation. The<br />
patient wanted to transfer to o<strong>the</strong>r hospital for more thorough<br />
evaluation on post-op 11th day. So we could not proceed adjuvant<br />
<strong>the</strong>rapy and follow-up observation.<br />
DISCUSSION<br />
The cell <strong>of</strong> origin <strong>of</strong> melanotic tumors involving <strong>the</strong> spinal<br />
nerve root can be ei<strong>the</strong>r a melanocyte, a Schwann cell, or an<br />
uncharacterized cell type 11) . Melanocytes are melanin-producing<br />
cells that arise from <strong>the</strong> neural crest during embryogenesis, and<br />
migrate to <strong>the</strong> skin, mucous membranes, and central nervous<br />
system. Tumors arising from melanocytic cells (primary and<br />
metastatic melanoma) and Schwann cells (melanotic nerve sheath<br />
tumors) have a common embryological origin in <strong>the</strong> neural<br />
crest 8,11) .<br />
Because <strong>of</strong> rarity <strong>of</strong> primary melanoma in spinal nerve root,<br />
<strong>the</strong> diagnosis can be difficult. Radiological studies may not be<br />
specific. Magnetic resonance imaging may <strong>of</strong>fer some indication<br />
<strong>of</strong> a melanotic lesion, melanin can show a hyperintense<br />
or isointense signal on T1 weighted images and decreased signal<br />
on T2 weighted images 7,9,12) .<br />
The pathological differential diagnosis <strong>of</strong> primary melanoma<br />
includes metastatic melanoma, melanocytoma, melanotic schwannoma,<br />
and melanotic clear-cell sarcoma. Melanocytoma lacks<br />
anaplastic features such as necrosis, significant mitotic activity,<br />
and pleomorphism, in contrast with primary melanoma. The<br />
characteristics <strong>of</strong> primary malignant melanomas are considerable,<br />
including nuclear pleomorphisms leading to large and bizarreshaped<br />
tumor cells with multinucleated giant cells 13) . A high<br />
mitotic rate, coagulative necrosis and hemorrhage are also commonly<br />
found in primary malignant melanoma 1,13) . Immunohistochemical<br />
staining is also helpful for differentiation. Significant<br />
s-100 protein expression without <strong>the</strong> expression <strong>of</strong> epi<strong>the</strong>lial<br />
membrane antigen supports <strong>the</strong> diagnosis <strong>of</strong> a schwannoma<br />
or melanoma 5,13) . Negative immunoreactivity for Leu-7<br />
rules out schwannoma whereas <strong>the</strong> detection <strong>of</strong> HMB-45 favors<br />
<strong>the</strong> diagnosis <strong>of</strong> a melanocytic tumor 5,13) .<br />
Schneider et al. 11) reported a case <strong>of</strong> primary melanoma arising<br />
from <strong>the</strong> L3 spinal nerve root that was treated by wide<br />
en-bloc resection. Skarli et al. 12) reported a similar case <strong>of</strong> primary<br />
malignant melanoma arising in a cervical spinal nerve<br />
root that did not recur or metastasize over 3 years without adjuvant<br />
chemo<strong>the</strong>rapy or radiation <strong>the</strong>rapy after surgical operation.<br />
Also Kwon et al. 4) reported a case <strong>of</strong> primary malignant melanoma<br />
<strong>of</strong> <strong>the</strong> C7 nerve root in 2004 that was treated with adjuvant<br />
radiation <strong>the</strong>rapy.<br />
Because <strong>of</strong> <strong>the</strong> rarity <strong>of</strong> <strong>the</strong>se lesions, <strong>the</strong> prognosis and proper<br />
adjuvant <strong>the</strong>rapy (chemo<strong>the</strong>rapy, radio<strong>the</strong>rapy) have not been<br />
established yet.<br />
It is important to differentiate primary melanoma from metastasis.<br />
The prognosis for patients with metastatic melanoma to<br />
central nervous system is dismal, with a life expectancy <strong>of</strong> less<br />
than 1 year in most studies 2,4,10) . In contrast, primary melanoma<br />
has long-term survival and better prognosis than metastatic lesion.<br />
Kor J Spine 6(1) March 2009 41
BI Roh, et al.<br />
In our case, we could not find any o<strong>the</strong>r tumor mass or pigmented<br />
skin lesion through radiological and physical examinations.<br />
CONCLUSION<br />
<strong>Primary</strong> CNS melanoma is a rare disease entity and melanomas<br />
arising from and limited to <strong>the</strong> spinal nerve roots are<br />
extremely rare. At present, <strong>the</strong> prognosis and optimal treatment<br />
(surgery, radio<strong>the</strong>rapy, chemo<strong>the</strong>rapy) <strong>of</strong> primary melanoma <strong>of</strong><br />
<strong>the</strong> spinal nerve root have not been established. More cases<br />
and fur<strong>the</strong>r follow-up is needed to establish guidelines for <strong>the</strong><br />
treatment <strong>of</strong> this rare disease entity.<br />
REFERENCES<br />
1. Brat DJ, Giannini C, Scheithauer BW, Burger PC: <strong>Primary</strong><br />
melanocytic neoplasm <strong>of</strong> <strong>the</strong> central nervous system. Am<br />
J Surg Pathol 23:745-754, 1999<br />
2. Bullard DE, Cox EB, Seigler HF: Central nervous system<br />
metastasis in malignant melanoma. Neurosurgery 8:6-30,<br />
1981<br />
3. Jellinger K, Bock F, Brenner H: Meningeal melanocytoma,<br />
report <strong>of</strong> a case and review <strong>of</strong> <strong>the</strong> literature. Acta Neurochirur<br />
94:78-87, 1988<br />
4. Kwon SC, Rhim SC, Lee DH, Roh SW, Kang SK: <strong>Primary</strong><br />
malignant melanoma <strong>of</strong> <strong>the</strong> cervical spinal nerve root.<br />
Yonsei Med J 45:345-348, 2004<br />
5. Lit<strong>of</strong>sky NS, Zee CS, Breeze RE, Chandrasoma PT: Meningeal<br />
melanocytoma: diagnostic criteria for a rare lesion.<br />
Neurosurgery 31:945-948, 1992<br />
6. Mndybur TI: Melanotic nerve sheath tumors. J Neurosurg<br />
41:187-192, 1974<br />
7. Monajati A, Wayne WS, Rauschning W, Ekholm SE: MR<br />
<strong>of</strong> <strong>the</strong> cauda equina. AJNR 8:893-900, 1987<br />
8. Myers JL, Bernreuter W, Dunham W: Melanotic schwannoma,<br />
clinicopathologic, immunohistochemical, and ultrastructural<br />
features <strong>of</strong> a rare primary bone tumor. Am J Clin<br />
Pathol 93:424-429, 1990<br />
9. Naul LG, Hise JH, Bauserman SCS, Todd FD: CT and<br />
MR <strong>of</strong> meningeal melanocytoma. AJNR 12:315-316, 1991<br />
10. Retsas S, Gershuny AR: Central nervous system involvement<br />
in malignant melanoma. Cancer 61:1926-1934, 1988<br />
11. Schneider SJ, Blacklock JB, Bruner JM: <strong>Melanoma</strong> arising<br />
in a spinal nerve root. J Neurosurg 67:923-927, 1987<br />
12. Skarli SO, Wolf AL, Kristt DA, Numaguchi Y: <strong>Melanoma</strong><br />
arising in a cervical spinal nerve root: Report <strong>of</strong> a case<br />
with a benign course and malignant features. Neurosurgery<br />
34:533-537, 1994.<br />
13. Wang F, Li X, Chen L, Pu X: <strong>Malignant</strong> transformation<br />
<strong>of</strong> spinal meningeal melanocytoma, case report and review<br />
<strong>of</strong> <strong>the</strong> literature. J Neurosurg Spine 6:451-454, 2007<br />
42 Kor J Spine 6(1) March 2009