RESUSCITATION
RESUSCITATION
RESUSCITATION
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Ventricular fibrillation<br />
at the earliest possible opportunity. Basic life support should be<br />
started if the defibrillator is not available immediately, but it<br />
should not delay delivery of the shock. If the arrest was<br />
witnessed, particularly in patients who are already monitored,<br />
and a defibrillator is not immediately available, a precordial<br />
thump should be given.<br />
In the presence of VF (or pulseless ventricular tachycardia)<br />
the left-hand side of the universal algorithm should be<br />
followed. Up to three shocks are given initially. In machines<br />
that deliver a monophasic waveform, energy levels of 200 J, 200 J,<br />
and 360 J should be used. Shocks of equivalent energy should<br />
be used with defibrillators that administer biphasic shocks. If<br />
more than one shock is required, the paddles or adhesive<br />
electrodes should be left in position on the patient’s chest<br />
while the defibrillator is recharged, and the monitor observed<br />
for any change in rhythm. When all three shocks are required,<br />
the objective should be to deliver these within one minute. This<br />
sequence should not normally need to be interrupted by basic<br />
life support, but if a delay occurs, because the equipment<br />
available does not permit rapid recharging between shocks, it is<br />
appropriate to consider providing basic life support between<br />
shocks.<br />
The carotid pulse should be checked only if the<br />
ECG changes to a rhythm compatible with a cardiac output.<br />
However, it is important to remember that after a shock is given<br />
a delay of a few seconds often occurs before the ECG display is<br />
again of diagnostic quality. In addition, successful defibrillation<br />
is often followed by a period of apparent asystole before a<br />
coordinated rhythm is established. Even if a rhythm that is<br />
normally compatible with a cardiac output is obtained, a period<br />
of impaired myocardial contractility often occurs, resulting in<br />
a weak or impalpable carotid pulse. It is important not to make<br />
a spurious diagnosis of pulseless electrical activity under these<br />
circumstances; for this reason the algorithm recommends only<br />
one minute of cardiopulmonary resuscitation (CPR) before<br />
reassessment of the rhythm and a further pulse check.<br />
After tracheal intubation chest compressions should<br />
continue uninterrupted at a rate of 100 per minute (except for<br />
defibrillation, pulse checks, or other procedures), while<br />
ventilation is continued at a rate of about 12 ventilations per<br />
minute. Continuous chest compressions may be possible with a<br />
laryngeal mask airway (LMA), but the seal around the larynx<br />
must prevent gas leaking and permit adequate ventilation of<br />
the lungs. If this is not possible, chest compressions should be<br />
interrupted to allow the usual 15 : 2 compression : ventilation ratio.<br />
Intravenous access should be established at an early stage in<br />
the management of cardiac arrest. Although cannulation of the<br />
central veins allows drugs to be delivered rapidly into the<br />
circulation, more complications can occur, some of which are<br />
serious. In most circumstances peripheral venous cannulation is<br />
quicker, easier, and safer. The choice will be determined by the<br />
skills of those present and the equipment available.<br />
In recent recommendations on the treatment of patients<br />
with VF refractory to initial attempts at defibrillation,<br />
anti-arrhythmic drugs have achieved less prominence.<br />
Amiodarone is currently recommended in the United Kingdom<br />
as the agent most likely to be successful in this situation.<br />
Lidocaine (lignocaine) may be considered as an alternative if<br />
amiodarone is not available but should not be given if the<br />
patient has previously received amiodarone. Procainamide is<br />
another alternative, although it is not widely employed in the<br />
United Kingdom. Further information about vasoconstrictor<br />
drugs and anti-arrhythmic agents is given in Chapter 16.<br />
If the patient remains in VF after one minute of CPR, then<br />
up to three further shocks should be given, each at 360 J<br />
(or the equivalent with a biphasic defibrillator), and the<br />
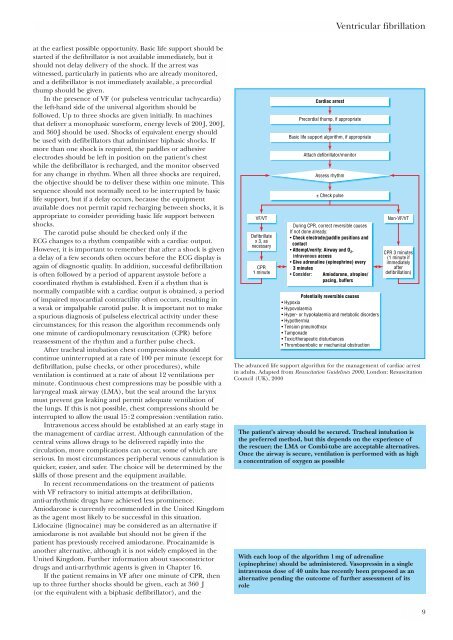
VF/VT<br />
Defibrillate<br />
x 3, as<br />
necessary<br />
CPR<br />
1 minute<br />
Cardiac arrest<br />
Precordial thump, if appropriate<br />
Basic life support algorithm, if appropriate<br />
Attach defibrillator/monitor<br />
Assess rhythm<br />
± Check pulse<br />
During CPR, correct reversible causes<br />
If not done already:<br />
• Check electrode/paddle positions and<br />
contact<br />
• Attempt/verify: Airway and O 2 ,<br />
intravenous access<br />
• Give adrenaline (epinephrine) every<br />
3 minutes<br />
• Consider: Amiodarone, atropine/<br />
pacing, buffers<br />
Potentially reversible causes<br />
• Hypoxia<br />
• Hypovolaemia<br />
• Hyper- or hypokalaemia and metabolic disorders<br />
• Hypothermia<br />
• Tension pneumothrax<br />
• Tamponade<br />
• Toxic/therapeutic disturbances<br />
• Thromboembolic or mechanical obstruction<br />
Non-VF/VT<br />
CPR 3 minutes<br />
(1 minute if<br />
immediately<br />
after<br />
defibrillation)<br />
The advanced life support algorithm for the management of cardiac arrest<br />
in adults. Adapted from Resuscitation Guidelines 2000, London: Resuscitation<br />
Council (UK), 2000<br />
The patient’s airway should be secured. Tracheal intubation is<br />
the preferred method, but this depends on the experience of<br />
the rescuer; the LMA or Combi-tube are acceptable alternatives.<br />
Once the airway is secure, ventilation is performed with as high<br />
a concentration of oxygen as possible<br />
With each loop of the algorithm 1 mg of adrenaline<br />
(epinephrine) should be administered. Vasopressin in a single<br />
intravenous dose of 40 units has recently been proposed as an<br />
alternative pending the outcome of further assessment of its<br />
role<br />
9