March/April - West Virginia State Medical Association
March/April - West Virginia State Medical Association
March/April - West Virginia State Medical Association
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Scientific Article |<br />
Table 1: Class I indications for ICD implantation in patients with structural heart disease. Adapted from ACC<br />
Guidelines, 2008. 12<br />
Class I ICD indications in patients with structural heart disease<br />
1) In survivors of cardiac arrest due to VF or hemodynamically unstable VT after excluding any completely reversible<br />
cause<br />
2) With structural heart disease and spontaneous sustained VT<br />
3) With syncope of undetermined origin with sustained VT or VF induced at EP study<br />
4) With LVEF < 35% who are at least 40-days post MI or 3-months post intervention (PCI or CABG) and who are<br />
NYHA CHF class II or III<br />
5) With nonischemic dilated cardiomyopathy and LVEF < 35% and who are NYHA CHF class II or III<br />
6) LVEF < 30 % who are at least 40-days post MI or 3-months post intervention (PCI or CABG) and who are NYHA<br />
CHF class I<br />
7) With non-sustained VT and prior MI, LVEF < 40%, and inducible VF or sustained VT at EP study<br />
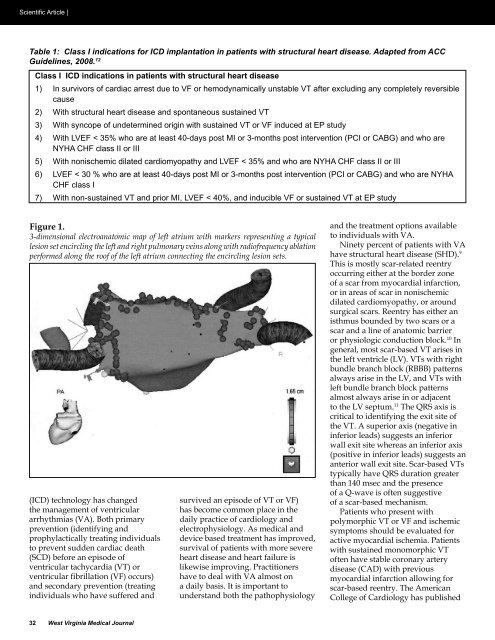
Figure 1.<br />
3-dimensional electroanatomic map of left atrium with markers representing a typical<br />
lesion set encircling the left and right pulmonary veins along with radiofrequency ablation<br />
performed along the roof of the left atrium connecting the encircling lesion sets.<br />
(ICD) technology has changed<br />
the management of ventricular<br />
arrhythmias (VA). Both primary<br />
prevention (identifying and<br />
prophylactically treating individuals<br />
to prevent sudden cardiac death<br />
(SCD) before an episode of<br />
ventricular tachycardia (VT) or<br />
ventricular fibrillation (VF) occurs)<br />
and secondary prevention (treating<br />
individuals who have suffered and<br />
survived an episode of VT or VF)<br />
has become common place in the<br />
daily practice of cardiology and<br />
electrophysiology. As medical and<br />
device based treatment has improved,<br />
survival of patients with more severe<br />
heart disease and heart failure is<br />
likewise improving. Practitioners<br />
have to deal with VA almost on<br />
a daily basis. It is important to<br />
understand both the pathophysiology<br />
and the treatment options available<br />
to individuals with VA.<br />
Ninety percent of patients with VA<br />
have structural heart disease (SHD). 9<br />
This is mostly scar-related reentry<br />
occurring either at the border zone<br />
of a scar from myocardial infarction,<br />
or in areas of scar in nonischemic<br />
dilated cardiomyopathy, or around<br />
surgical scars. Reentry has either an<br />
isthmus bounded by two scars or a<br />
scar and a line of anatomic barrier<br />
or physiologic conduction block. 10 In<br />
general, most scar-based VT arises in<br />
the left ventricle (LV). VTs with right<br />
bundle branch block (RBBB) patterns<br />
always arise in the LV, and VTs with<br />
left bundle branch block patterns<br />
almost always arise in or adjacent<br />
to the LV septum. 11 The QRS axis is<br />
critical to identifying the exit site of<br />
the VT. A superior axis (negative in<br />
inferior leads) suggests an inferior<br />
wall exit site whereas an inferior axis<br />
(positive in inferior leads) suggests an<br />
anterior wall exit site. Scar-based VTs<br />
typically have QRS duration greater<br />
than 140 msec and the presence<br />
of a Q-wave is often suggestive<br />
of a scar-based mechanism.<br />
Patients who present with<br />
polymorphic VT or VF and ischemic<br />
symptoms should be evaluated for<br />
active myocardial ischemia. Patients<br />
with sustained monomorphic VT<br />
often have stable coronary artery<br />
disease (CAD) with previous<br />
myocardial infarction allowing for<br />
scar-based reentry. The American<br />
College of Cardiology has published<br />
32 <strong>West</strong> <strong>Virginia</strong> <strong>Medical</strong> Journal