Whirlpool Communication Plan - HealthSCOPE Benefits
Whirlpool Communication Plan - HealthSCOPE Benefits
Whirlpool Communication Plan - HealthSCOPE Benefits
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
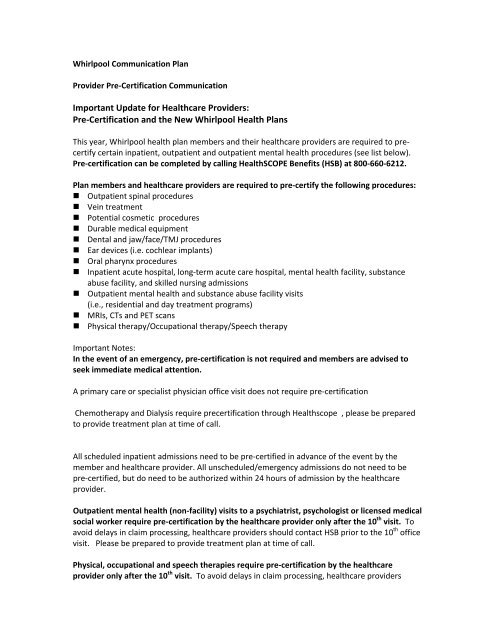
<strong>Whirlpool</strong> <strong>Communication</strong> <strong>Plan</strong><br />
Provider Pre‐Certification <strong>Communication</strong><br />
Important Update for Healthcare Providers:<br />
Pre‐Certification and the New <strong>Whirlpool</strong> Health <strong>Plan</strong>s<br />
This year, <strong>Whirlpool</strong> health plan members and their healthcare providers are required to precertify<br />
certain inpatient, outpatient and outpatient mental health procedures (see list below).<br />
Pre‐certification can be completed by calling <strong>HealthSCOPE</strong> <strong>Benefits</strong> (HSB) at 800‐660‐6212.<br />
<strong>Plan</strong> members and healthcare providers are required to pre‐certify the following procedures:<br />
• Outpatient spinal procedures<br />
• Vein treatment<br />
• Potential cosmetic procedures<br />
• Durable medical equipment<br />
• Dental and jaw/face/TMJ procedures<br />
• Ear devices (i.e. cochlear implants)<br />
• Oral pharynx procedures<br />
• Inpatient acute hospital, long‐term acute care hospital, mental health facility, substance<br />
abuse facility, and skilled nursing admissions<br />
• Outpatient mental health and substance abuse facility visits<br />
(i.e., residential and day treatment programs)<br />
• MRIs, CTs and PET scans<br />
• Physical therapy/Occupational therapy/Speech therapy<br />
Important Notes:<br />
In the event of an emergency, pre‐certification is not required and members are advised to<br />
seek immediate medical attention.<br />
A primary care or specialist physician office visit does not require pre‐certification<br />
Chemotherapy and Dialysis require precertification through Healthscope , please be prepared<br />
to provide treatment plan at time of call.<br />
All scheduled inpatient admissions need to be pre‐certified in advance of the event by the<br />
member and healthcare provider. All unscheduled/emergency admissions do not need to be<br />
pre‐certified, but do need to be authorized within 24 hours of admission by the healthcare<br />
provider.<br />
Outpatient mental health (non‐facility) visits to a psychiatrist, psychologist or licensed medical<br />
social worker require pre‐certification by the healthcare provider only after the 10 th visit. To<br />
avoid delays in claim processing, healthcare providers should contact HSB prior to the 10 th office<br />
visit. Please be prepared to provide treatment plan at time of call.<br />
Physical, occupational and speech therapies require pre‐certification by the healthcare<br />
provider only after the 10 th visit. To avoid delays in claim processing, healthcare providers
should contact HSB prior to the 10 th visit. Please be prepared to provide treatment plan at time<br />
of call.<br />
For the complete list of all procedures, with CPT code, requiring pre‐certification, healthcare<br />
providers may log on to www.healthscopebenefits.com. CPT list does not confirm benefit<br />
coverage under plan.<br />
When calling for pre‐certification, please be prepared to verify the name of the referring<br />
physician, physician performing the procedure, name and address of facility where procedure<br />
will be performed, and CPT code of the procedure for which you are seeking to authorize. For<br />
oncology and dialysis, please be prepared to provide treatment plan at time of call.<br />
Please note that if a procedure or admission is not pre‐certified, there will be a $500 fee<br />
assessed to the member when the claim is processed.<br />
If you have questions, or to pre‐certify a procedure or admission, members and providers should<br />
contact HSB at 800‐660‐6212.<br />
Other Helpful Information:<br />
Claims status, eligibility, and benefit information may be verified at<br />
www.healthscopebenefits.com or by using the <strong>HealthSCOPE</strong> Interactive Voice Recording system<br />
New! There is a primary care physician co‐payment for Rewards <strong>Plan</strong> (Level 2) members.<br />
Primary care is defined as general practice, family practice, internal medicine, and pediatrics.<br />
Medco is <strong>Whirlpool</strong>’s pharmacy benefit manager. They have a dedicated Physician Service<br />
Center line available to answer your questions. You can reach Medco by calling 800‐211‐1456.<br />
<strong>Whirlpool</strong> offers a wellness benefit for all active and retired health plan members. The benefit is<br />
not subject to a deductible or co‐pay and covers the following services:
<strong>Whirlpool</strong> Health <strong>Plan</strong> Pre‐Certification Process<br />
Follow these steps to pre‐certify an admission or procedure.<br />
1. Contact <strong>HealthSCOPE</strong> <strong>Benefits</strong> (HSB) at 800‐660‐6212.<br />
2. Choose healthcare provider or facility option.<br />
3. You will know have the option of choosing to:<br />
pre‐certify an admission or procedure for an active employee;<br />
pre‐certify an admission or procedure for a retiree; or<br />
pre‐certify chemotherapy or dialysis.<br />
You may check eligibility by visiting the HSB website at www.healthscopebenefits.com<br />
or by using the <strong>HealthSCOPE</strong> Interactive Voice Recording system.<br />
4. You will now be routed directly to the pre‐certification department. At this point:<br />
A Case Associate will open a case and ask you to verify the name and address of the<br />
referring physician, physician performing the procedure, and the facility. Be prepared to<br />
provide the diagnosis and procedure code(s). If all requested information is provided, a<br />
pre‐certification authorization number will be issued. If additional information is<br />
needed, a temporary pre‐certification reference number will be assigned. A nurse will<br />
contact you to discuss the additional requested documentation. After the<br />
documentation has been received and medical necessity has been established, a full<br />
authorization will be granted to the provider. If medical necessity has not been met, the<br />
case will be directed to a Medical Director for review, with determination being<br />
communicated to provider.<br />
5. If a member needs a procedure or test performed immediately due to the severity of an<br />
injury or illness, the member does not need to pre‐certify the procedure. We ask that<br />
the healthcare provider contact <strong>HealthSCOPE</strong> <strong>Benefits</strong> after the event.