Annals of Diagnostic Paediatric Pathology
Annals of Diagnostic Paediatric Pathology
Annals of Diagnostic Paediatric Pathology
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
18<br />
types were diagnosed in participating patients. A medullary<br />
thyroid carcinoma was present in one patient with MEN 2B<br />
syndrome. Renal cell carcinoma (RCC) occurred in two patients<br />
– in SDHB mutation carrier and in patient with von<br />
Hippel – Lindau disease. Pancreatic islet tumors and haemangioblastoma<br />
<strong>of</strong> IV brain ventricle were found in patient<br />
with VHL. In the cohort presented here, there were also two<br />
reports <strong>of</strong> multiple head and neck paraganglioma in SDHD<br />
gene mutation carriers [Table 4].<br />
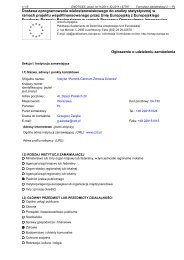
Table 4<br />
Clinical characteristic <strong>of</strong> patients with hereditary syndromes<br />
<strong>of</strong> pheochromocytoma<br />
Characteristics <strong>of</strong> pheochromocytoma patients with<br />
hereditary syndromes under 20 years <strong>of</strong> age<br />
Multiple tumors – 12 patients (80%)<br />
Extra – adrenal tumors – 7 patients (47%)<br />
Bilateral adrenal tumors – 6 patients (40%)<br />
Thoracic localization <strong>of</strong> tumors – 2 patients (13%) – only in<br />
SDHD gene mutations<br />
Recurrence <strong>of</strong> the disease – 5 patients (33%)<br />
Malignant – 0<br />
Associated tumors:<br />
! Renal cell carcinoma – 2 patients: VHL and SDHB<br />
! Pancreatic islet tumors – 1 patient – VHL<br />
! haemangioblastoma <strong>of</strong> IV brain ventricle<br />
! Multiple head and neck paraganglioma – 2 patients –<br />
SDHD<br />
! Medullary thyroid carcinoma – 1 patient – MEN 2B<br />
Multiple or extraadrenal or bilateral adrenal pheochromocytoma<br />
– 13 patients (87%)<br />
Discussion<br />
Our clinical and molecular evaluation <strong>of</strong> 136 unrelated<br />
patients who presented with pheochromocytoma revealed<br />
that 34 patients (24,8%) had a hereditary predisposition<br />
to von Hippel–Lindau disease, MEN-2, neur<strong>of</strong>ibromatosis<br />
type 1, or the syndromes associated with pheochromocytoma<br />
and paraganglioma. Among the 34 patients with mutations,<br />
32% had mutations <strong>of</strong> RET, 18% had germ-line mutations<br />
<strong>of</strong> VHL, 12 percent had clinical signs <strong>of</strong> NF1 syndrome,<br />
and 18 and 21% had mutations <strong>of</strong> two newly<br />
identified genes, SDHD and SDHB. Patients with hereditary<br />
syndromes were younger that those with sporadic disease<br />
and multiple and extra- adrenal tumors were more frequent<br />
in this group. Our results are consistent with other population-based<br />
studies [2, 4, 7, 8, 9]. In our registry almost one<br />
half <strong>of</strong> patients with hereditary pheochromocytoma was under<br />
20 years <strong>of</strong> age. We can state that 87% <strong>of</strong> all multifocal<br />
(including bilateral tumors) and extra – adrenal tumors in<br />
patients with onset <strong>of</strong> the disease at the age <strong>of</strong> 20 years or<br />
younger were found to be hereditary. All these findings po-<br />
inted out, that extra – adrenal and/or multiple pheochromocytomas<br />
as well as young age at presentation may be striking<br />
features <strong>of</strong> hereditary disease [9]. Interestingly, 91% <strong>of</strong><br />
probands found to have hereditary disease with the use <strong>of</strong><br />
molecular testing had no associated signs and symptoms at<br />
presentation. Only three (9%) <strong>of</strong> them had positive family<br />
history at presentation. A partial explanation for the high<br />
frequency <strong>of</strong> hereditary pheochromocytoma without family<br />
history <strong>of</strong> disease might include spontaneous mutation in<br />
one <strong>of</strong> the susceptibility genes, decreased penetrance, and<br />
maternal imprinting [9]. In our registry, spontaneous mutations<br />
in one <strong>of</strong> four susceptibility genes occurred in two patients<br />
with hereditary von Hippel–Lindau disease, one with<br />
MEN 2B syndrome, one with SDHD gene mutation and one<br />
with SDHB mutation (Table 5).<br />
Today, more than 200 different VHL mutations have<br />
been identified which appear to be equally distributed throughout<br />
the gene. De novo mutations at hypermutable sequences<br />
result in most <strong>of</strong> the recurrent mutations. In large German<br />
registry <strong>of</strong> von Hippel–Lindau disease, frequency <strong>of</strong><br />
spontaneous mutation in VHL is thirteen percent <strong>of</strong> all cases<br />
[9, 10]. In MEN 2B syndrome, which is the most distinct and<br />
aggressive <strong>of</strong> the MEN 2 variants, de novo mutations are very<br />
<strong>of</strong>ten and reach fifty percent [12]. A little is known about<br />
spontaneous mutations in SDHD and SDHB genes because<br />
they are newly identified genes.<br />
Penetrance is known to be relatively high (approximately<br />
70 percent by the age <strong>of</strong> 70) among patients with MEN-<br />
2 and von Hippel–Lindau disease, overall [9, 10]. Benn et al.<br />
reported a statistically significant age-related penetrance difference<br />
for SDHB and SDHD mutation carriers. By age 30<br />
yr, 29% <strong>of</strong> SDHB mutation carriers and 48% <strong>of</strong> SDHD mutation<br />
carriers were diagnosed with paraganglioma; by age<br />
40 yr, 45% <strong>of</strong> SDHB mutation carriers and 73% <strong>of</strong> SDHD<br />
mutation carriers were diagnosed with paraganglioma [3,<br />
13]. As discussed by authors, SDHD and SDHB mutations<br />
have an age-related penetrance, and the lifetime risk <strong>of</strong> developing<br />
paraganglioma (s)/pheochromocytoma (s) approaches<br />
100% by age 70 yr [3, 13].<br />
In patients with SDHD mutations, penetrance depends<br />
on whether the individual inherited the mutation from<br />
the mother or the father [11, 13]. The disease is not manifested<br />
when the mutation is inherited from the mother, but is<br />
highly penetrant when inherited from the father. This phenomenon<br />
is known as maternal imprinting.<br />
Overall, therefore, pheochromocytomas in patients<br />
without family histories are due to spontaneous mutations,<br />
decreased penetrance, or maternal imprinting, although other<br />
causes such as gene–gene interactions and gene–environment<br />
interactions may be possible. Genetic testing can be<br />
a powerful aid to the identification <strong>of</strong> a syndrome in such cases.<br />
Since disease is likely to develop in virtually all patients<br />
with a family specific mutation, it seems reasonable to subject<br />
such patients to lifelong surveillance.<br />
This report highlights the value <strong>of</strong> genetic testing for<br />
affected patients and at-risk asymptomatic family members.<br />
Genetic testing should be considered in all patients with pa-