Annals of Diagnostic Paediatric Pathology
Annals of Diagnostic Paediatric Pathology
Annals of Diagnostic Paediatric Pathology
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
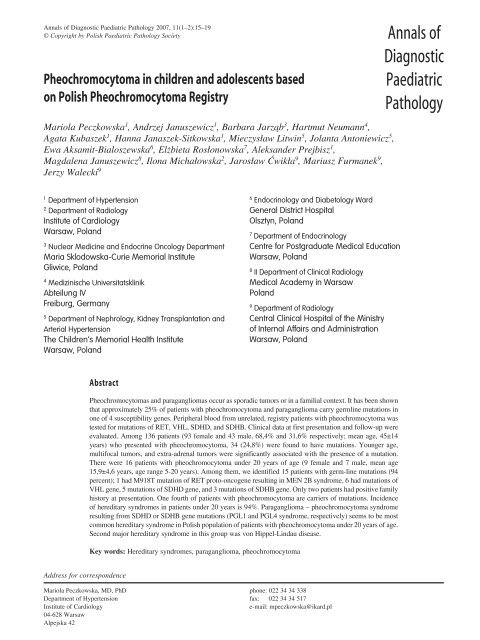
<strong>Annals</strong> <strong>of</strong> <strong>Diagnostic</strong> <strong>Paediatric</strong> <strong>Pathology</strong> 2007, 11(1–2):15–19<br />
© Copyright by Polish <strong>Paediatric</strong> <strong>Pathology</strong> Society <strong>Annals</strong> <strong>of</strong><br />
Pheochromocytoma in children and adolescents based<br />
on Polish Pheochromocytoma Registry<br />
Mariola Peczkowska 1 , Andrzej Januszewicz 1 , Barbara Jarz¹b 3 , Hartmut Neumann 4 ,<br />
Agata Kubaszek 1 , Hanna Janaszek-Sitkowska 1 , Mieczys³aw Litwin 5 , Jolanta Antoniewicz 5 ,<br />
Ewa Aksamit-Bialoszewska 6 , El¿bieta Ros³onowska 7 , Aleksander Prejbisz 1 ,<br />
Magdalena Januszewicz 8 , Ilona Micha³owska 2 , Jaros³aw Æwik³a 9 , Mariusz Furmanek 9 ,<br />
Jerzy Walecki 9<br />
<strong>Diagnostic</strong><br />
<strong>Paediatric</strong><br />
<strong>Pathology</strong><br />
1<br />
Department <strong>of</strong> Hypertension<br />
2<br />
Department <strong>of</strong> Radiology<br />
Institute <strong>of</strong> Cardiology<br />
Warsaw, Poland<br />
3<br />
Nuclear Medicine and Endocrine Oncology Department<br />
Maria Sklodowska−Curie Memorial Institute<br />
Gliwice, Poland<br />
4<br />
Medizinische Universitatsklinik<br />
Abteilung IV<br />
Freiburg, Germany<br />
5<br />
Department <strong>of</strong> Nephrology, Kidney Transplantation and<br />
Arterial Hypertension<br />
The Children's Memorial Health Institute<br />
Warsaw, Poland<br />
6<br />
Endocrinology and Diabetology Ward<br />
General District Hospital<br />
Olsztyn, Poland<br />
7<br />
Department <strong>of</strong> Endocrinology<br />
Centre for Postgraduate Medical Education<br />
Warsaw, Poland<br />
8<br />
II Department <strong>of</strong> Clinical Radiology<br />
Medical Academy in Warsaw<br />
Poland<br />
9<br />
Department <strong>of</strong> Radiology<br />
Central Clinical Hospital <strong>of</strong> the Ministry<br />
<strong>of</strong> Internal Affairs and Administration<br />
Warsaw, Poland<br />
Abstract<br />
Pheochromocytomas and paragangliomas occur as sporadic tumors or in a familial context. It has been shown<br />
that approximately 25% <strong>of</strong> patients with pheochromocytoma and paraganglioma carry germline mutations in<br />
one <strong>of</strong> 4 susceptibility genes. Peripheral blood from unrelated, registry patients with pheochromocytoma was<br />
tested for mutations <strong>of</strong> RET, VHL, SDHD, and SDHB. Clinical data at first presentation and follow-up were<br />
evaluated. Among 136 patients (93 female and 43 male, 68,4% and 31,6% respectively; mean age, 45±14<br />
years) who presented with pheochromocytoma, 34 (24,8%) were found to have mutations. Younger age,<br />
multifocal tumors, and extra-adrenal tumors were significantly associated with the presence <strong>of</strong> a mutation.<br />
There were 16 patients with pheochromocytoma under 20 years <strong>of</strong> age (9 female and 7 male, mean age<br />
15,9±4,6 years, age range 5-20 years). Among them, we identified 15 patients with germ-line mutations (94<br />
percent); 1 had M918T mutation <strong>of</strong> RET proto-oncogene resulting in MEN 2B syndrome, 6 had mutations <strong>of</strong><br />
VHL gene, 5 mutations <strong>of</strong> SDHD gene, and 3 mutations <strong>of</strong> SDHB gene. Only two patients had positive family<br />
history at presentation. One fourth <strong>of</strong> patients with pheochromocytoma are carriers <strong>of</strong> mutations. Incidence<br />
<strong>of</strong> hereditary syndromes in patients under 20 years is 94%. Paraganglioma – pheochromocytoma syndrome<br />
resulting from SDHD or SDHB gene mutations (PGL1 and PGL4 syndrome, respectively) seems to be most<br />
common hereditary syndrome in Polish population <strong>of</strong> patients with pheochromocytoma under 20 years <strong>of</strong> age.<br />
Second major hereditary syndrome in this group was von Hippel-Lindau disease.<br />
Key words: Hereditary syndromes, paraganglioma, pheochromocytoma<br />
Address for correspondence<br />
Mariola Peczkowska, MD, PhD phone: 022 34 34 338<br />
Department <strong>of</strong> Hypertension fax: 022 34 34 517<br />
Institute <strong>of</strong> Cardiology<br />
e-mail: mpeczkowska@ikard.pl<br />
04-628 Warsaw<br />
Alpejska 42
16<br />
Introduction<br />
Familial pheochromocytomas<br />
Pheochromocytomas are rare tumors <strong>of</strong> the adrenal gland<br />
that arise from chromaffin cells in the adrenal medulla.<br />
Paragangliomas arise from extra – adrenal chromaffin<br />
cells and can originate in either the sympathetic nervous<br />
system or parasympathetic ganglia. Paragangliomas that arise<br />
from sympathetic nervous system occur most frequently<br />
in the retroperitoneum and are traditionally<br />
termed extra – adrenal pheochro-<br />
Table 1<br />
mocytoma. Paragangliomas have been<br />
broadly categorized into two groups:<br />
those in the head and neck region with<br />
carotid body as the major site and those<br />
located elsewhere, with adrenal medulla<br />
as the major site. Tumors in the<br />
head and neck are anatomically associated<br />
with parasympathetic nervous system<br />
and are located close to the major<br />
arteries and nerves, whereas the adrenal<br />
medulla and other paraganglia below<br />
neck and head are closer associated<br />
with the sympathetic nervous system.<br />
Parasympathetic tumors are usually<br />
present as an asymptomatic slow growing<br />
mass, lacking endocrine activity,<br />
whereas sympathetic tumors are hormonally<br />
active and secret excess amount <strong>of</strong><br />
catecholamines. Pheochromocytomas<br />
and paragangliomas occur as sporadic<br />
tumors or may be associated with hereditary<br />
syndromes [2]. Several genetic<br />
syndromes are known to be associated<br />
with increased risk for pheochromocytoma,<br />
including von Hippel – Lindau<br />
(VHL) syndrome, multiple endocrine<br />
neoplasia typ 2 (MEN 2) and neur<strong>of</strong>ibromatosis<br />
type 1 (NF1), occurring as<br />
a result <strong>of</strong> germline mutations in VHL,<br />
RET, or NF1 genes, respectively. More<br />
recently, nuclear genes encoding mitochondrial<br />
complex II subunit proteins<br />
have been associated with the development<br />
<strong>of</strong> pheochromocytomas and paragangliomas<br />
and newly discovered paraganglioma/pheochromocytoma<br />
syndrome<br />
(PPS) was added to the list <strong>of</strong><br />
hereditary syndrome in pheochromocytoma<br />
and paraganglioma. Neumann et<br />
al. showed that close to 24% <strong>of</strong> patients<br />
with pheochromocytomas and paragangliomas<br />
carry a germline mutation [8].<br />
This was confirmed by Amar et al. who<br />
even found 27% carrying germline mutations<br />
[1]. Therefore, the historically<br />
established rule <strong>of</strong> tens’, stating that approximately<br />
10% <strong>of</strong> pheochromocytomas<br />
are hereditary, 10% are malignant, 10% are bilateral,<br />
10% are extra-adrenal, 10% are not associated with hypertension<br />
and 10% occur in children, is no longer valid concerning<br />
genetics. Molecular medicine makes it possible to<br />
differentiate sporadic from hereditary disease, which will<br />
affect medical management not only for the patient but also<br />
for the family. Familial syndromes <strong>of</strong> pheochromocytoma<br />
are presented in Table 1.<br />
Syndrome and prevalence Gene Gene locus<br />
<strong>of</strong> pheochromocytomas<br />
Multiple endocrine neoplasia Type 2A Ret-protooncogene 10q11.2<br />
(30–60%)<br />
Medullary thyroid carcinoma<br />
Pheochromocytoma<br />
Hyperparathyroidism<br />
Multiple endocrine neoplasia Type 2B Ret-protooncogene 10q11.2<br />
(MEN2B) (30-60%)<br />
Medullary thyroid carcinoma<br />
Pheochromocytoma<br />
Marfanoid habitus<br />
Skeletal deformation<br />
Mucosal neuromas<br />
Ganglioneuromatosis <strong>of</strong> the intestinal tract<br />
Von Hippel-Lindau disesase (VHL) VHL-tumor 3p25-26<br />
(15–20%) type 2 suppressor gene<br />
A: Retinal and CNS<br />
haemangioblastomas<br />
Pheochromocytomas<br />
Endolymphatic sac tumors<br />
Epididymal cystadenomas<br />
B: As in VHL type 2A +<br />
renal cell cysts and carcinomas<br />
As in VHL type 2A + pancreatic<br />
neoplasmas and cysts<br />
C: Pheochromocytomas only<br />
Neur<strong>of</strong>ibromatosis type 1 (NF1) NF-1-gene 1 7q11.2<br />
(3–5%)<br />
Multiple fibromas on skin<br />
Cafe au lait spots<br />
Lisch nodules <strong>of</strong> the iris<br />
Pheochromocytoma-paraganglioma SDHB-gene 1p35-36<br />
syndrome (PGL, 70-80%) SDHD-gene 11q21-23<br />
Head and neck tumors<br />
Extra – adrenal and adrenal pheochromocytomas
17<br />
In the present study, we analyzed the known susceptibility<br />
genes for pheochromocytoma – VHL, RET, SDHD,<br />
and SDHB – in a large, unselected series <strong>of</strong> patients collected<br />
in Polish Registry <strong>of</strong> Pheochromocytoma who presented<br />
with this tumor in order to classify them as having either<br />
sporadic or hereditary disease. In addition, we analyzed hereditary<br />
syndrome prevalence and clinical characteristic in<br />
young pheochromocytoma patients under 20 years <strong>of</strong> age.<br />
Material and methods<br />
The population based registry for pheochromocytoma was<br />
conducted in Poland. Patients were recruited from thirty five<br />
centres and clinical, radiological and demographical data<br />
was collected. One hundred thirty-six consecutive, unrelated<br />
patients with histologically confirmed pheochromocytoma<br />
from whom blood-leukocyte DNA was available were enrolled.<br />
All patients provided written or oral informed consent.<br />
For classification we used term paraganglioma for tumors <strong>of</strong><br />
location in the head and neck area whereas those <strong>of</strong> adrenal,<br />
extraadrenal abdominal and thoracic location were named<br />
pheochromocytomas.<br />
All eight exons <strong>of</strong> SDHB, all four exons <strong>of</strong> SDHD, all<br />
three exons <strong>of</strong> VHL, and exons 10, 11, and 13 through 16 <strong>of</strong><br />
RET were examined by analysis <strong>of</strong> single-strand conformation<br />
polymorphisms and direct sequencing, as previously described<br />
[5].<br />
Missense mutations were diagnosed if the DNA variants<br />
were absent in 100 healthy controls. All molecular examinations<br />
were performed in Department <strong>of</strong> Nephrology and<br />
Hypertension, Albert Ludwigs University, Freiburg, Germany.<br />
Results<br />
A total <strong>of</strong> 136 patients (93 female and 43 male, 68,4% and<br />
31,6% respectively; mean age, 45±14 years) with pheochromocytoma<br />
were enrolled in the study. We identified 34 patients<br />
with deleterious germ-line mutations (24,8%). Only<br />
3 patients had family history at the presentation. Among the<br />
34 patients with mutations, 32% had mutations <strong>of</strong> RET, 18%<br />
had germ-line mutations <strong>of</strong> VHL, 12% had clinical signs <strong>of</strong><br />
NF1 syndrome, and 18 and 21% presented mutations <strong>of</strong> two<br />
newly identified genes, SDHD and SDHB.<br />
The age at the onset <strong>of</strong> symptoms was statistically lower<br />
in all carriers <strong>of</strong> mutations than in patients with sporadic<br />
disease. Multiple, extra – adrenal, and bilateral adrenal<br />
pheochromocytomas as well as recurrences <strong>of</strong> the disease<br />
were statistically more frequent among patients with mutations<br />
than among patients without mutations. Incidence <strong>of</strong><br />
malignant pheochromocytoma did not differ between study<br />
groups (Table 2).<br />
The most frequent symptom <strong>of</strong> the disease was hypertension<br />
(86%), then palpitations (67%), sweating (56%), headache<br />
(40%), blanching <strong>of</strong> the skin (40%), severe cardiovascular<br />
complications (myocardial infarction, stroke, severe<br />
arrhythmia, etc.) (7,4%). Asymptomatic clinical course was<br />
observed in 8,8% <strong>of</strong> patients (Table 3).<br />
Table 2<br />
Comparison between hereditary pheochromocytoma and<br />
sporadic pheochromocytoma groups<br />
Hereditary Sporadic p<br />
Age (years) 34,3±13,2 48,7±13,4 p
18<br />
types were diagnosed in participating patients. A medullary<br />
thyroid carcinoma was present in one patient with MEN 2B<br />
syndrome. Renal cell carcinoma (RCC) occurred in two patients<br />
– in SDHB mutation carrier and in patient with von<br />
Hippel – Lindau disease. Pancreatic islet tumors and haemangioblastoma<br />
<strong>of</strong> IV brain ventricle were found in patient<br />
with VHL. In the cohort presented here, there were also two<br />
reports <strong>of</strong> multiple head and neck paraganglioma in SDHD<br />
gene mutation carriers [Table 4].<br />
Table 4<br />
Clinical characteristic <strong>of</strong> patients with hereditary syndromes<br />
<strong>of</strong> pheochromocytoma<br />
Characteristics <strong>of</strong> pheochromocytoma patients with<br />
hereditary syndromes under 20 years <strong>of</strong> age<br />
Multiple tumors – 12 patients (80%)<br />
Extra – adrenal tumors – 7 patients (47%)<br />
Bilateral adrenal tumors – 6 patients (40%)<br />
Thoracic localization <strong>of</strong> tumors – 2 patients (13%) – only in<br />
SDHD gene mutations<br />
Recurrence <strong>of</strong> the disease – 5 patients (33%)<br />
Malignant – 0<br />
Associated tumors:<br />
! Renal cell carcinoma – 2 patients: VHL and SDHB<br />
! Pancreatic islet tumors – 1 patient – VHL<br />
! haemangioblastoma <strong>of</strong> IV brain ventricle<br />
! Multiple head and neck paraganglioma – 2 patients –<br />
SDHD<br />
! Medullary thyroid carcinoma – 1 patient – MEN 2B<br />
Multiple or extraadrenal or bilateral adrenal pheochromocytoma<br />
– 13 patients (87%)<br />
Discussion<br />
Our clinical and molecular evaluation <strong>of</strong> 136 unrelated<br />
patients who presented with pheochromocytoma revealed<br />
that 34 patients (24,8%) had a hereditary predisposition<br />
to von Hippel–Lindau disease, MEN-2, neur<strong>of</strong>ibromatosis<br />
type 1, or the syndromes associated with pheochromocytoma<br />
and paraganglioma. Among the 34 patients with mutations,<br />
32% had mutations <strong>of</strong> RET, 18% had germ-line mutations<br />
<strong>of</strong> VHL, 12 percent had clinical signs <strong>of</strong> NF1 syndrome,<br />
and 18 and 21% had mutations <strong>of</strong> two newly<br />
identified genes, SDHD and SDHB. Patients with hereditary<br />
syndromes were younger that those with sporadic disease<br />
and multiple and extra- adrenal tumors were more frequent<br />
in this group. Our results are consistent with other population-based<br />
studies [2, 4, 7, 8, 9]. In our registry almost one<br />
half <strong>of</strong> patients with hereditary pheochromocytoma was under<br />
20 years <strong>of</strong> age. We can state that 87% <strong>of</strong> all multifocal<br />
(including bilateral tumors) and extra – adrenal tumors in<br />
patients with onset <strong>of</strong> the disease at the age <strong>of</strong> 20 years or<br />
younger were found to be hereditary. All these findings po-<br />
inted out, that extra – adrenal and/or multiple pheochromocytomas<br />
as well as young age at presentation may be striking<br />
features <strong>of</strong> hereditary disease [9]. Interestingly, 91% <strong>of</strong><br />
probands found to have hereditary disease with the use <strong>of</strong><br />
molecular testing had no associated signs and symptoms at<br />
presentation. Only three (9%) <strong>of</strong> them had positive family<br />
history at presentation. A partial explanation for the high<br />
frequency <strong>of</strong> hereditary pheochromocytoma without family<br />
history <strong>of</strong> disease might include spontaneous mutation in<br />
one <strong>of</strong> the susceptibility genes, decreased penetrance, and<br />
maternal imprinting [9]. In our registry, spontaneous mutations<br />
in one <strong>of</strong> four susceptibility genes occurred in two patients<br />
with hereditary von Hippel–Lindau disease, one with<br />
MEN 2B syndrome, one with SDHD gene mutation and one<br />
with SDHB mutation (Table 5).<br />
Today, more than 200 different VHL mutations have<br />
been identified which appear to be equally distributed throughout<br />
the gene. De novo mutations at hypermutable sequences<br />
result in most <strong>of</strong> the recurrent mutations. In large German<br />
registry <strong>of</strong> von Hippel–Lindau disease, frequency <strong>of</strong><br />
spontaneous mutation in VHL is thirteen percent <strong>of</strong> all cases<br />
[9, 10]. In MEN 2B syndrome, which is the most distinct and<br />
aggressive <strong>of</strong> the MEN 2 variants, de novo mutations are very<br />
<strong>of</strong>ten and reach fifty percent [12]. A little is known about<br />
spontaneous mutations in SDHD and SDHB genes because<br />
they are newly identified genes.<br />
Penetrance is known to be relatively high (approximately<br />
70 percent by the age <strong>of</strong> 70) among patients with MEN-<br />
2 and von Hippel–Lindau disease, overall [9, 10]. Benn et al.<br />
reported a statistically significant age-related penetrance difference<br />
for SDHB and SDHD mutation carriers. By age 30<br />
yr, 29% <strong>of</strong> SDHB mutation carriers and 48% <strong>of</strong> SDHD mutation<br />
carriers were diagnosed with paraganglioma; by age<br />
40 yr, 45% <strong>of</strong> SDHB mutation carriers and 73% <strong>of</strong> SDHD<br />
mutation carriers were diagnosed with paraganglioma [3,<br />
13]. As discussed by authors, SDHD and SDHB mutations<br />
have an age-related penetrance, and the lifetime risk <strong>of</strong> developing<br />
paraganglioma (s)/pheochromocytoma (s) approaches<br />
100% by age 70 yr [3, 13].<br />
In patients with SDHD mutations, penetrance depends<br />
on whether the individual inherited the mutation from<br />
the mother or the father [11, 13]. The disease is not manifested<br />
when the mutation is inherited from the mother, but is<br />
highly penetrant when inherited from the father. This phenomenon<br />
is known as maternal imprinting.<br />
Overall, therefore, pheochromocytomas in patients<br />
without family histories are due to spontaneous mutations,<br />
decreased penetrance, or maternal imprinting, although other<br />
causes such as gene–gene interactions and gene–environment<br />
interactions may be possible. Genetic testing can be<br />
a powerful aid to the identification <strong>of</strong> a syndrome in such cases.<br />
Since disease is likely to develop in virtually all patients<br />
with a family specific mutation, it seems reasonable to subject<br />
such patients to lifelong surveillance.<br />
This report highlights the value <strong>of</strong> genetic testing for<br />
affected patients and at-risk asymptomatic family members.<br />
Genetic testing should be considered in all patients with pa-
19<br />
Table 5<br />
Germ-line mutations in the four genes detected in the series <strong>of</strong> patients with pheochromocytoma under 20 years <strong>of</strong> age<br />
Independent cases Gene Exon cDNA nucleotide Amino-acid change Mutation type Family history<br />
1. SDHB 3 402 C>T R90X Stopcodon hereditary<br />
2. 6 721 G>A C196Y Missense unknown<br />
3. 6 847-50delTCTC F238frameshift Frameshift spontaneous<br />
4. SDHD 1 33 C>A C11X Stopcodon spontaneous<br />
5. 1 33 C>A C11X Stopcodon hereditary<br />
6. 1 33 C>A C11X Stopcodon unknown<br />
7. 1 33 C>A C11X Stopcodon hereditary<br />
8. 1 33 C>A C11X Stopcodon hereditary<br />
9. VHL 3 712 C>T A167Y Missense spontaneous<br />
10. 3 764 T>A L184H Missense unknown<br />
11. 1 451A>G S80G Missense hereditary<br />
12. 1 451A>G S80G Missense hereditary<br />
13. 1 451A>G S80G Missense hereditary<br />
14. 1 404G>C R64P Missense spontaneous<br />
15. RET 16 918 ATG>ACG M918T Missense spontaneous<br />
raganglioma and/or pheochromocytoma [6, 9, 13]. Familial<br />
pheochromocytoma/paraganglioma is inherited in an autosomal<br />
dominant manner; thus, an affected person has a 50%<br />
chance <strong>of</strong> passing the mutation on to each child.<br />
The surveillance strategy for a germline mutation-positive<br />
asymptomatic patient should include: annual history<br />
and physical examination by a clinician experienced with<br />
pheochromocytoma and paraganglioma; annual biochemical<br />
testing, e. g. 24-h urine for metanephrines and catecholamines<br />
and computed tomography or magnetic resonance imaging<br />
every 2 yr taking into consideration the tumour locations<br />
typically associated with the mutated gene [6, 13]. Given<br />
the observation that children <strong>of</strong> female SDHD mutation<br />
carriers do not manifest the disease when the mutation has<br />
been inherited, rigorous clinical surveillance is probably not<br />
warranted for these <strong>of</strong>fspring.<br />
References<br />
1. Amar L, Bertherat J, Baudin E, et al<br />
(2005) Genetic testing in pheochromocytoma<br />
or functional paraganglioma. J<br />
Clin Oncol 23: 8812–8818<br />
2. Baysal BE, Ferrell RE, Willett-Brozick<br />
JE, et al (2000) Mutations in SDHD,<br />
a mitochondrial complex II gene, in hereditary<br />
paraganglioma. Science 287:<br />
848–851<br />
3. al (2006) Clinical presentation and penetrance<br />
<strong>of</strong> pheochromocytoma/paraganglioma<br />
syndromes. J Clin Endocrinol<br />
Metab 91 (3): 827–836<br />
4. Elder EE, Elder G, Larsson C (2005)<br />
Pheochromocytoma and functional paraganglioma<br />
syndrome: No longer the<br />
10% tumor. J Surg Oncol 89: 193–201<br />
5. Gimm O, Armanios M, Dziema H,<br />
Neumann HPH, Eng C (2000) Somatic<br />
and occult germ-line mutations in<br />
SDHD, a mitochondrial complex II gene,<br />
in nonfamilial pheochromocytoma.<br />
Cancer Res 60: 6822–6825<br />
6. Grupa robocza PTNT (2006) Zalecenia<br />
Polskiego Towarzystwa Nadcisnienia<br />
Tetniczego dotyczace diagnostyki i leczenia<br />
pheochromocytoma. Nadcisnienie<br />
Tetnicze 76–78 (in Polish)<br />
7. Januszewicz W, Wocial B, Sznajderman<br />
M, Januszewicz A (2000) Guz<br />
chromochlonny. Wydawnictwo Lekarskie<br />
PZWL, Warszawa (in Polish)<br />
8. Jarzab B (2004) Dziedziczne uwarunkowania<br />
guzow chromochlonnych. In:<br />
Nadcisnienie tetnicze. Red. Januszewicz<br />
A, Januszewicz W, Szczepanska-<br />
-Sadowska E, Sznajderman M. Medycyna<br />
Praktyczna, Krakow (in Polish)<br />
9. Neumann HP, Bausch B, McWhinney<br />
SR, et al (2002) Germ-line mutations in<br />
nonsyndromic pheochromocytoma. N<br />
Engl J Med 346: 1459–1466<br />
10. Neumann HP, Berger DP, Sigmund G,<br />
et al. (1993) Pheochromocytomas, multiple<br />
endocrine neoplasia type 2, and<br />
von Hippel-Lindau disease. N Engl J<br />
Med 329: 1531–1538<br />
11. Neumann HPH, Pawlu C, Peczkowska<br />
M, et al. (2004) Distinct clinical features<br />
<strong>of</strong> paraganglioma syndromes associated<br />
with SDHB and SDHD gene mutations.<br />
JAMA 292: 943–951<br />
12. Peczkowska M, Januszewicz A (2005)<br />
Multiple endocrine neoplasia type 2.<br />
Familial Cancer 4: 25–36<br />
13. Young WF, Abboud AL (2006) Paraganglioma<br />
– All in the family J Clin Endocrinol<br />
Metab 91: 790–792