MANAGEMENT OF FISTULA IN ANO SURGICAL TECHNIQUES ...
MANAGEMENT OF FISTULA IN ANO SURGICAL TECHNIQUES ...
MANAGEMENT OF FISTULA IN ANO SURGICAL TECHNIQUES ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
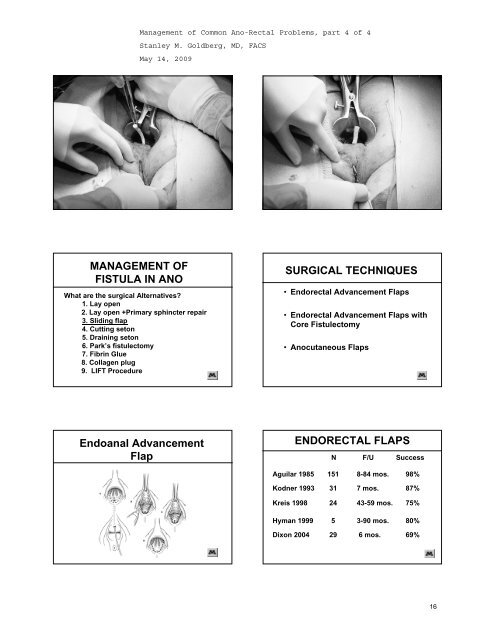
<strong>MANAGEMENT</strong> <strong>OF</strong><br />
<strong>FISTULA</strong> <strong>IN</strong> <strong>ANO</strong><br />
What are the surgical Alternatives<br />
1. Lay open<br />
2. Lay open +Primary sphincter repair<br />
3. Sliding flap<br />
4. Cutting seton<br />
5. Draining seton<br />
6. Park’s fistulectomy<br />
7. Fibrin Glue<br />
8. Collagen plug<br />
9. LIFT Procedure<br />
<strong>SURGICAL</strong> <strong>TECHNIQUES</strong><br />
• Endorectal Advancement Flaps<br />
• Endorectal Advancement Flaps with<br />
Core Fistulectomy<br />
• Anocutaneous Flaps<br />
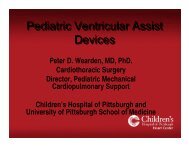
Endoanal Advancement<br />
Flap<br />
ENDORECTAL FLAPS<br />
N F/U Success<br />
Aguilar 1985<br />
151<br />
8-84 mos.<br />
98%<br />
Kodner 1993<br />
31<br />
7 mos.<br />
87%<br />
Kreis 1998<br />
24<br />
43-59 mos.<br />
75%<br />
Hyman 1999<br />
5<br />
3-90 mos.<br />
80%<br />
Dixon 2004<br />
29<br />
6 mos.<br />
69%<br />
16
<strong>MANAGEMENT</strong> <strong>OF</strong><br />
<strong>FISTULA</strong> <strong>IN</strong> <strong>ANO</strong><br />
What are the surgical Alternatives<br />
1. Lay open<br />
2. Lay open +Primary sphincter repair<br />
3. Sliding flap<br />
4. Cutting seton<br />
5. Draining seton<br />
6. Park’s fistulectomy<br />
7. Fibrin Glue<br />
8. Collagen plug<br />
9. LIFT Procedure<br />
<strong>MANAGEMENT</strong> <strong>OF</strong><br />
<strong>FISTULA</strong> <strong>IN</strong> <strong>ANO</strong><br />
When will we use a draining seton<br />
1. In patients with inflammatory bowel disease<br />
2. More than 50% sphincter muscle involved<br />
3. Patient with poor continence<br />
4. When advancement flap is not technically<br />
feasible<br />
<strong>MANAGEMENT</strong> <strong>OF</strong><br />
<strong>FISTULA</strong> <strong>IN</strong> <strong>ANO</strong><br />
What are the surgical Alternatives<br />
1. Lay open<br />
2. Lay open +Primary sphincter repair<br />
3. Sliding flap<br />
4. Cutting seton<br />
5. Draining seton<br />
6. Park’s fistulectomy<br />
7. Fibrin Glue<br />
8. Collagen plug<br />
9. LIFT Procedure<br />
17
LIFT PROCEDURE<br />
L – Lateral<br />
I – Intrasphincteric<br />
F – Fistula<br />
T – Transection<br />
DATA FROM THAILAND<br />
Number<br />
PATIENTS 17<br />
SUCCESS 16<br />
PERCENTAGE 94%<br />
Rojanasakul A, J Med Assoc Thai 2007<br />
LIFT Procedure<br />
• Overall success rate 85%<br />
100 Patients<br />
• Complex fistulas (horseshoe type) 30 cases approximately<br />
90%<br />
• Unhealed fistulas after LIFT procedure 15%<br />
Personal Communication<br />
July 7, 2008<br />
Dr. Arun Rojanasakul<br />
LIFT Procedure<br />
University of Minnesota<br />
Follow up for 4.4 months<br />
Number<br />
Patients 12<br />
Success 10<br />
Percentage 88%<br />
Continence Unchanged<br />
18
LIFT Procedure<br />
University of Minnesota<br />
Number<br />
Patients 31<br />
Male 16<br />
Female 15<br />
Mean Age 46.5<br />
Median follow up<br />
8 months<br />
Failed Prior Operation 84%<br />
Follow up<br />
• 90% follow up (28/31); median 35 weeks<br />
• Success rate: 58% (18/31)<br />
– Median time to failure: 19 weeks (range<br />
4-63); 2 failures resulted in<br />
intersphincteric fistulas<br />
– Post-op complication: 1/31 (3%) -<br />
persistent pain<br />
• Incontinence: 0%<br />
Principles of Surgical Treatment<br />
• Confirmation of Anatomy of Fistula<br />
• Not every fistula needs an operation<br />
• Be conservative<br />
• Use staged procedures<br />
HOW DO I DO IT<br />
Leave Seton until all Wounds are Healed (> 6months)<br />
Remove Seton and Asses Symptoms<br />
Tolerable<br />
Non-tolerable<br />
• Reduce to a simple tract - draining seton<br />
• Use non division techniques<br />
Follow<br />
Fibrin Glue/plug<br />
• Reassess the situation after each intervention<br />
Flap or LIFT<br />
R.S.K. Phillips<br />
THANK<br />
YOU<br />
19