Neonatal Jaundice - Associates in Newborn Medicine
Neonatal Jaundice - Associates in Newborn Medicine
Neonatal Jaundice - Associates in Newborn Medicine
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Neonatal</strong> <strong>Jaundice</strong><br />
M. Jeffrey Maisels<br />
Pediatr. Rev. 2006;27;443-454<br />
DOI: 10.1542/pir.27-12-443<br />
The onl<strong>in</strong>e version of this article, along with updated <strong>in</strong>formation and services, is<br />
located on the World Wide Web at:<br />
http://peds<strong>in</strong>review.aappublications.org/cgi/content/full/27/12/443<br />
Pediatrics <strong>in</strong> Review is the official journal of the American Academy of Pediatrics. A monthly<br />
publication, it has been published cont<strong>in</strong>uously s<strong>in</strong>ce 1979. Pediatrics <strong>in</strong> Review is owned,<br />
published, and trademarked by the American Academy of Pediatrics, 141 Northwest Po<strong>in</strong>t<br />
Boulevard, Elk Grove Village, Ill<strong>in</strong>ois, 60007. Copyright © 2006 by the American Academy of<br />
Pediatrics. All rights reserved. Pr<strong>in</strong>t ISSN: 0191-9601. Onl<strong>in</strong>e ISSN: 1526-3347.<br />
Downloaded from http://peds<strong>in</strong>review.aappublications.org by J Michael Coleman on June 4, 2010
Article neonatology<br />
<strong>Neonatal</strong> <strong>Jaundice</strong><br />
M. Jeffrey Maisels, MB,<br />
BCh*<br />
Author Disclosure<br />
Dr Maisels did not<br />
disclose any f<strong>in</strong>ancial<br />
relationships relevant<br />
to this article.<br />
To view additional<br />
figures and tables for<br />
this article, visit<br />
peds<strong>in</strong>review.org and<br />
click on the title of this<br />
article.<br />
Objectives After review<strong>in</strong>g this article, readers should be able to:<br />
1. Understand the metabolism of bilirub<strong>in</strong>.<br />
2. Describe the factors that place an <strong>in</strong>fant at risk for develop<strong>in</strong>g severe<br />
hyperbilirub<strong>in</strong>emia.<br />
3. Describe the physiologic mechanisms that result <strong>in</strong> neonatal jaundice.<br />
4. List the common causes of <strong>in</strong>direct hyperbilirub<strong>in</strong>emia <strong>in</strong> the newborn.<br />
5. Del<strong>in</strong>eate the criteria for diagnos<strong>in</strong>g ABO hemolytic disease.<br />
6. Discuss the major cl<strong>in</strong>ical features of acute bilirub<strong>in</strong> encephalopathy and chronic<br />
bilirub<strong>in</strong> encephalopathy (kernicterus).<br />
7. List the key elements of the American Academy of Pediatrics guidel<strong>in</strong>es for the<br />
management of hyperbilirub<strong>in</strong>emia.<br />
8. Describe the factors that affect the dosage and efficacy of phototherapy.<br />
Case Report<br />
A 23-year-old primiparous mother delivered a 36 weeks’ gestation male <strong>in</strong>fant follow<strong>in</strong>g an<br />
uncomplicated pregnancy. The <strong>in</strong>fant <strong>in</strong>itially had some difficulty latch<strong>in</strong>g on for breastfeed<strong>in</strong>g,<br />
but subsequently appeared to nurse adequately, although his nurs<strong>in</strong>g quality was considered<br />
“fair.” At age 25 hours, he appeared slightly jaundiced, and his bilirub<strong>in</strong> concentration<br />
was 7.5 mg/dL (128.3 mcmol/L). He was discharged at age 30 hours, with a follow-up visit<br />
scheduled for 1 week after discharge. On postnatal day 5, at about 4:30 PM, the mother called<br />
the pediatrician’s office because her <strong>in</strong>fant was not nurs<strong>in</strong>g well and was becom<strong>in</strong>g <strong>in</strong>creas<strong>in</strong>gly<br />
sleepy. On question<strong>in</strong>g, she also reported that he had become more jaundiced over the<br />
previous 2 days. The mother was given an appo<strong>in</strong>tment to see the pediatrician the follow<strong>in</strong>g<br />
morn<strong>in</strong>g. Exam<strong>in</strong>ation <strong>in</strong> the office revealed a markedly jaundiced <strong>in</strong>fant who had a<br />
high-pitched cry and <strong>in</strong>termittently arched his back. His total serum bilirub<strong>in</strong> (TSB) concentration<br />
was 36.5 mg/dL (624.2 mcmol/L). He was admitted to the hospital, and an<br />
immediate exchange transfusion was performed. Neurologic evaluation at age 18 months<br />
showed profound neuromotor delay, choreoathetoid movements, an upward gaze paresis, and<br />
a sensor<strong>in</strong>eural hear<strong>in</strong>g loss.<br />
This <strong>in</strong>fant had acute bilirub<strong>in</strong> encephalopathy and eventually developed chronic<br />
bilirub<strong>in</strong> encephalopathy or kernicterus. Kernicterus, although rare, is one of the known<br />
causes of cerebral palsy. Unlike other causes of cerebral palsy, kernicterus almost always can<br />
be prevented through a relatively straightforward process of identification, monitor<strong>in</strong>g,<br />
follow-up, and treatment of the jaundiced newborn. Because kernicterus is uncommon,<br />
pediatricians are required to monitor and treat many jaundiced <strong>in</strong>fants—most of whom will<br />
be healthy—to prevent substantial harm to a few.<br />
<strong>Jaundice</strong> <strong>in</strong> the newborn is a unique problem because elevation of serum bilirub<strong>in</strong> is<br />
potentially toxic to the <strong>in</strong>fant’s develop<strong>in</strong>g central nervous system. Although it was<br />
considered almost ext<strong>in</strong>ct, kernicterus still occurs <strong>in</strong> the United States and western Europe.<br />
To prevent kernicterus, cl<strong>in</strong>icians need to understand the physiology of bilirub<strong>in</strong> production<br />
and excretion and develop a consistent, systematic approach to the management of<br />
jaundice <strong>in</strong> the <strong>in</strong>fant.<br />
*Department of Pediatrics, William Beaumont Hospital, Royal Oak, Mich.<br />
Pediatrics <strong>in</strong> Review Vol.27 No.12 December 2006 443<br />
Downloaded from http://peds<strong>in</strong>review.aappublications.org by J Michael Coleman on June 4, 2010
neonatology<br />
neonatal jaundice<br />
Table 1. Physiologic Mechanisms<br />
of <strong>Neonatal</strong> <strong>Jaundice</strong><br />
Increased Bilirub<strong>in</strong> Load on Liver Cell<br />
● Increased erythrocyte volume<br />
● Decreased erythrocyte survival<br />
● Increased early-labeled bilirub<strong>in</strong>*<br />
● Increased enterohepatic circulation of bilirub<strong>in</strong><br />
Decreased Hepatic Uptake of Bilirub<strong>in</strong> From Plasma<br />
● Decreased ligand<strong>in</strong><br />
Decreased Bilirub<strong>in</strong> Conjugation<br />
● Decreased urid<strong>in</strong>e diphosphoglucuronosyl transferase<br />
activity<br />
Defective Bilirub<strong>in</strong> Excretion<br />
● Excretion impaired but not rate limit<strong>in</strong>g<br />
*Early-labeled bilirub<strong>in</strong> refers to the bilirub<strong>in</strong> that does not come from<br />
the turnover of effete red blood cells. This bilirub<strong>in</strong> is derived from<br />
<strong>in</strong>effective erythropoiesis and the turnover of nonhemoglob<strong>in</strong> heme,<br />
primarily <strong>in</strong> the liver.<br />
Repr<strong>in</strong>ted with permission from Maisels MJ. <strong>Jaundice</strong>. In: MacDonald<br />
MG, Seshia MMK, Mullett MD, eds. Neonatology: Pathophysiology and<br />
Management of the <strong>Newborn</strong>. Philadelphia, Pa: Lipp<strong>in</strong>cott Co;<br />
2005:768–846.<br />
Figure 1. <strong>Neonatal</strong> bile pigment metabolism. RBCerythrocytes,<br />
R.E.reticuloendothelial. Repr<strong>in</strong>ted with permission<br />
from Maisels MJ. <strong>Jaundice</strong>. In: MacDonald MG, Seshia MMK,<br />
Mullett MD, eds. Neonatology: Pathophysiology and Management<br />
of the <strong>Newborn</strong>. Philadelphia, Pa: Lipp<strong>in</strong>cott Co; 2005:<br />
768–846.<br />
Bilirub<strong>in</strong> Metabolism<br />
Bilirub<strong>in</strong> is produced from the catabolism of heme <strong>in</strong> the<br />
reticuloendothelial system (Fig. 1). This unconjugated<br />
bilirub<strong>in</strong> is released <strong>in</strong>to the circulation where it is reversibly<br />
but tightly bound to album<strong>in</strong>. When the bilirub<strong>in</strong>album<strong>in</strong><br />
complex reaches the liver cell, it is transported<br />
<strong>in</strong>to the hepatocyte where it comb<strong>in</strong>es enzymatically<br />
with glucuronic acid, produc<strong>in</strong>g bilirub<strong>in</strong> mono- and<br />
diglucuronides. The conjugation reaction is catalyzed by<br />
urid<strong>in</strong>e diphosphate glucuronosyl transferase (UGT-<br />
1A1). The mono- and diglucuronides are excreted <strong>in</strong>to<br />
the bile and the gut. In the newborn, much of the<br />
conjugated bilirub<strong>in</strong> <strong>in</strong> the <strong>in</strong>test<strong>in</strong>e is hydrolyzed back<br />
to unconjugated bilirub<strong>in</strong>, a reaction catalyzed by the<br />
enzyme beta glucuronidase that is present <strong>in</strong> the <strong>in</strong>test<strong>in</strong>al<br />
mucosa. The unconjugated bilirub<strong>in</strong> is reabsorbed<br />
<strong>in</strong>to the blood stream by way of the enterohepatic circulation,<br />
add<strong>in</strong>g an additional bilirub<strong>in</strong> load to the already<br />
overstressed liver. This enterohepatic circulation of bilirub<strong>in</strong><br />
is an important contributor to neonatal jaundice.<br />
By contrast, <strong>in</strong> the adult, conjugated bilirub<strong>in</strong> is reduced<br />
rapidly by the action of colonic bacteria to urobil<strong>in</strong>ogens,<br />
and very little enterohepatic circulation occurs.<br />
Physiologic <strong>Jaundice</strong><br />
Follow<strong>in</strong>g ligation of the umbilical cord, the neonate<br />
must dispose of the bilirub<strong>in</strong> load that previously was<br />
cleared through the placenta. Because neonatal hyperbilirub<strong>in</strong>emia<br />
is an almost universal f<strong>in</strong>d<strong>in</strong>g dur<strong>in</strong>g the first<br />
postnatal week, this transient elevation of the serum<br />
bilirub<strong>in</strong> has been termed physiologic jaundice. The<br />
mechanisms responsible for physiologic jaundice are<br />
summarized <strong>in</strong> Table 1.<br />
The TSB concentration reflects a comb<strong>in</strong>ation of the<br />
effects of bilirub<strong>in</strong> production, conjugation, and enterohepatic<br />
circulation. The factors that affect these processes<br />
account for the bilirub<strong>in</strong>emia that occurs <strong>in</strong> virtually all<br />
newborns.<br />
444 Pediatrics <strong>in</strong> Review Vol.27 No.12 December 2006<br />
Downloaded from http://peds<strong>in</strong>review.aappublications.org by J Michael Coleman on June 4, 2010
neonatology<br />
neonatal jaundice<br />
Breastfeed<strong>in</strong>g and <strong>Jaundice</strong><br />
An important change <strong>in</strong> the United States population has<br />
been the dramatic <strong>in</strong>crease <strong>in</strong> breastfeed<strong>in</strong>g at hospital<br />
discharge from 30% <strong>in</strong> the 1960s to almost 70% today. In<br />
some hospitals, 85% or more of <strong>in</strong>fants are breastfed.<br />
Multiple studies have found a strong association between<br />
breastfeed<strong>in</strong>g and an <strong>in</strong>creased <strong>in</strong>cidence of neonatal<br />
hyperbilirub<strong>in</strong>emia. The jaundice associated with breastfeed<strong>in</strong>g<br />
<strong>in</strong> the first 2 to 4 postnatal days has been called<br />
“breastfeed<strong>in</strong>g jaundice” or “breastfeed<strong>in</strong>g-associated<br />
jaundice”; that which appears later (onset at 4 to 7 d with<br />
prolonged jaundice) has been called “the human milk<br />
jaundice syndrome,” although there is considerable<br />
overlap between the two entities.<br />
Prolonged <strong>in</strong>direct-react<strong>in</strong>g hyperbilirub<strong>in</strong>emia (beyond<br />
age 2 to 3 wk) occurs <strong>in</strong> 20% to 30% of all breastfeed<strong>in</strong>g<br />
<strong>in</strong>fants and may persist for up to 3 months <strong>in</strong><br />
some <strong>in</strong>fants. Such <strong>in</strong>fants have an <strong>in</strong>creased <strong>in</strong>cidence of<br />
Gilbert syndrome (diagnosed by UGT-1A1 genotyp<strong>in</strong>g<br />
from a peripheral blood sample).<br />
The jaundice associated with breastfeed<strong>in</strong>g <strong>in</strong> the first<br />
few days after birth appears to be related to an <strong>in</strong>crease <strong>in</strong><br />
the enterohepatic circulation of bilirub<strong>in</strong>. This occurs <strong>in</strong><br />
the first few days because until the milk has “come <strong>in</strong>,”<br />
breastfed <strong>in</strong>fants receive fewer calories, and the decrease<br />
<strong>in</strong> caloric <strong>in</strong>take is an important stimulus to <strong>in</strong>creas<strong>in</strong>g<br />
the enterohepatic circulation.<br />
Pathologic Causes of <strong>Jaundice</strong><br />
Table 2 lists the causes of pathologic <strong>in</strong>direct-react<strong>in</strong>g<br />
hyperbilirub<strong>in</strong>emia <strong>in</strong> the neonate.<br />
ABO Hemolytic Disease<br />
The use of Rh immunoglob<strong>in</strong> has dramatically decreased<br />
the <strong>in</strong>cidence of Rh erythroblastosis fetalis, and hemolysis<br />
from ABO <strong>in</strong>compatibility is by far the most common<br />
cause of isoimmune hemolytic disease <strong>in</strong> newborns. In<br />
about 15% of pregnancies, an <strong>in</strong>fant who has blood type<br />
A or B is carried by a mother who is type O. About one<br />
third of such <strong>in</strong>fants have a positive direct antiglobul<strong>in</strong><br />
test (DAT or Coombs test), <strong>in</strong>dicat<strong>in</strong>g that they have<br />
anti-A or anti-B antibodies attached to the red cells. Of<br />
these <strong>in</strong>fants, only 20% develop a peak TSB of more than<br />
12.8 mg/dL (219 mcmol/L). Consequently, although<br />
ABO-<strong>in</strong>compatible, DAT-positive <strong>in</strong>fants are about<br />
twice as likely as their compatible peers to have moderate<br />
hyperbilirub<strong>in</strong>emia (TSB 13 mg/dL [222.3 mcmol/<br />
L]), severe jaundice (TSB 20 mg/dL [ [342 mcmol/<br />
L]) <strong>in</strong> the <strong>in</strong>fants is uncommon. Nevertheless, ABO<br />
hemolytic disease can cause severe hyperbilirub<strong>in</strong>emia<br />
and kernicterus.<br />
Table 2. Causes of Indirect<br />
Hyperbilirub<strong>in</strong>emia <strong>in</strong><br />
<strong>Newborn</strong>s<br />
Increased Production or Bilirub<strong>in</strong> Load on the Liver<br />
Hemolytic Disease<br />
● Immune-mediated<br />
—Rh alloimmunization, ABO and other blood group<br />
<strong>in</strong>compatibilities<br />
● Heritable<br />
—Red cell membrane defects: Hereditary<br />
spherocytosis, elliptocytosis, pyropoikilocytosis,<br />
stomatocytosis<br />
—Red cell enzyme deficiencies: Glucose-6-<br />
phosphate dehydrogenase deficiency, a pyruvate<br />
k<strong>in</strong>ase deficiency, and other erythrocyte enzyme<br />
deficiencies<br />
—Hemoglob<strong>in</strong>opathies: Alpha thalassemia, beta<br />
thalassemia<br />
—Unstable hemoglob<strong>in</strong>s: Congenital He<strong>in</strong>z body<br />
hemolytic anemia<br />
Other Causes of Increased Production<br />
● Sepsis a, b<br />
● Dissem<strong>in</strong>ated <strong>in</strong>travascular coagulation<br />
● Extravasation of blood: Hematomas; pulmonary,<br />
abdom<strong>in</strong>al, cerebral, or other occult hemorrhage<br />
● Polycythemia<br />
● Macrosomia <strong>in</strong> <strong>in</strong>fants of diabetic mothers<br />
Increased Enterohepatic Circulation of Bilirub<strong>in</strong><br />
● Breast milk jaundice<br />
● Pyloric stenosis a<br />
● Small or large bowel obstruction or ileus<br />
Decreased Clearance<br />
● Prematurity<br />
● Glucose-6-phosphate dehydrogenase deficiency<br />
Inborn Errors of Metabolism<br />
—Crigler-Najjar syndrome, types I and II<br />
—Gilbert syndrome<br />
—Galactosemia b<br />
—Tyros<strong>in</strong>emia b<br />
—Hypermethion<strong>in</strong>emia b<br />
Metabolic<br />
—Hypothyroidism<br />
—Hypopituitarism b<br />
a Decreased clearance also part of pathogenesis.<br />
b Elevation of direct-read<strong>in</strong>g bilirub<strong>in</strong> also occurs.<br />
Repr<strong>in</strong>ted with permission from Maisels MJ. <strong>Jaundice</strong>. In: MacDonald<br />
MG, Seshia MMK, Mullett MD, eds. Neonatology: Pathophysiology and<br />
Management of the <strong>Newborn</strong>. Philadelphia, Pa: Lipp<strong>in</strong>cott Co;<br />
2005:768–846.<br />
Diagnos<strong>in</strong>g ABO Hemolytic Disease<br />
ABO hemolytic disease has a highly variable cl<strong>in</strong>ical<br />
presentation. Most affected <strong>in</strong>fants present with a rapid<br />
Pediatrics <strong>in</strong> Review Vol.27 No.12 December 2006 445<br />
Downloaded from http://peds<strong>in</strong>review.aappublications.org by J Michael Coleman on June 4, 2010
neonatology<br />
neonatal jaundice<br />
Table 3. Criteria for Diagnos<strong>in</strong>g<br />
ABO Hemolytic Disease as the<br />
Cause of <strong>Neonatal</strong><br />
Hyperbilirub<strong>in</strong>emia<br />
Mother group O, <strong>in</strong>fant group A or B<br />
AND<br />
● Positive DAT<br />
● <strong>Jaundice</strong> appear<strong>in</strong>g with<strong>in</strong> 12 to 24 h after birth<br />
● Microspherocytes on blood smear<br />
● Negative DAT but homozygous for Gilbert<br />
syndrome<br />
Repr<strong>in</strong>ted with permission from Maisels MJ. <strong>Jaundice</strong>. In: MacDonald<br />
MG, Seshia MMK, Mullett MD, eds. Neonatology: Pathophysiology and<br />
Management of the <strong>Newborn</strong>. Philadelphia, Pa: Lipp<strong>in</strong>cott Co;<br />
2005:768–846.<br />
<strong>in</strong>crease <strong>in</strong> TSB concentrations with<strong>in</strong> the first 24 hours,<br />
but the TSB subsequently decl<strong>in</strong>es, <strong>in</strong> many <strong>in</strong>fants,<br />
often without any <strong>in</strong>tervention. ABO hemolytic disease is<br />
a relatively common cause of early hyperbilirub<strong>in</strong>emia<br />
(before the <strong>in</strong>fant leaves the nursery), but it is a relatively<br />
rare cause of hyperbilirub<strong>in</strong>emia <strong>in</strong> <strong>in</strong>fants who have been<br />
discharged and readmitted. The criteria for diagnos<strong>in</strong>g<br />
ABO hemolytic disease as the cause of neonatal hyperbilirub<strong>in</strong>emia<br />
are listed <strong>in</strong> Table 3. Recently, it has been<br />
shown that DAT-negative, ABO-<strong>in</strong>compatible <strong>in</strong>fants<br />
who also have Gilbert syndrome are at risk for hyperbilirub<strong>in</strong>emia.<br />
This may expla<strong>in</strong> the occasional ABO<strong>in</strong>compatible<br />
<strong>in</strong>fant who has a negative DAT and nevertheless<br />
develops early hyperbilirub<strong>in</strong>emia.<br />
Glucose-6-phosphate Dehydrogenase (G-6PD)<br />
Deficiency<br />
G-6PD deficiency is the most common and cl<strong>in</strong>ically<br />
significant red cell enzyme defect, affect<strong>in</strong>g as many as<br />
4,500,000 newborns worldwide each year. Although<br />
known for its prevalence <strong>in</strong> the populations of the Mediterranean,<br />
Middle East, Arabian Pen<strong>in</strong>sula, southeast<br />
Asia, and Africa, G-6PD has been transformed by immigration<br />
and <strong>in</strong>termarriage <strong>in</strong>to a global problem. Nevertheless,<br />
most pediatricians <strong>in</strong> the United States do not<br />
th<strong>in</strong>k of G-6PD deficiency when confronted with a jaundiced<br />
<strong>in</strong>fant. This possibility should be considered,<br />
though, particularly when see<strong>in</strong>g African-American <strong>in</strong>fants.<br />
Although African-American newborns, as a group,<br />
tend to have lower TSB concentrations than do caucasian<br />
newborns, G-6PD deficiency is found <strong>in</strong> 11% to 13% of<br />
African-American newborns. This translates to 32,000 to<br />
Table 4. Major Cl<strong>in</strong>ical Features<br />
of Acute Bilirub<strong>in</strong><br />
Encephalopathy<br />
Initial Phase<br />
● Slight stupor (“lethargic,” “sleepy”)<br />
● Slight hypotonia, paucity of movement<br />
● Poor suck<strong>in</strong>g, slightly high-pitched cry<br />
Intermediate Phase<br />
● Moderate stupor—irritable<br />
● Tone variable, usually <strong>in</strong>creased; some have<br />
retrocollis-opisthotonos<br />
● M<strong>in</strong>imal feed<strong>in</strong>g, high-pitched cry<br />
Advanced Phase<br />
● Deep stupor to coma<br />
● Tone usually <strong>in</strong>creased; some have retrocollisopisthotonos<br />
● No feed<strong>in</strong>g, shrill cry<br />
Repr<strong>in</strong>ted with permission from Maisels MJ. <strong>Jaundice</strong>. In: MacDonald<br />
MG, Seshia MMK, Mullett MD, eds. Neonatology: Pathophysiology and<br />
Management of the <strong>Newborn</strong>. Philadelphia, Pa: Lipp<strong>in</strong>cott Co;<br />
2005:768–846.<br />
39,000 African-American male G-6PD-deficient hemizygous<br />
newborns born annually <strong>in</strong> the United States. As<br />
many as 30% of <strong>in</strong>fants <strong>in</strong> the United States who have<br />
kernicterus have been found to be G-6PD-deficient.<br />
The G-6PD gene is located on the X chromosome,<br />
and hemizygous males have the full enzyme deficiency,<br />
although female heterozygotes are also at risk for hyperbilirub<strong>in</strong>emia.<br />
G-6PD-deficient neonates have an <strong>in</strong>crease<br />
<strong>in</strong> heme turnover, although overt evidence of<br />
hemolysis often is not present. In addition, affected<br />
<strong>in</strong>fants have an impaired ability to conjugate bilirub<strong>in</strong>.<br />
Bilirub<strong>in</strong> Encephalopathy<br />
In the case described at the beg<strong>in</strong>n<strong>in</strong>g of this article, the<br />
<strong>in</strong>fant developed extreme hyperbilirub<strong>in</strong>emia and the<br />
classic signs of acute bilirub<strong>in</strong> encephalopathy (Table 4).<br />
He also developed the typical features of chronic bilirub<strong>in</strong><br />
encephalopathy or kernicterus (Table 5).<br />
How Could This Have Been Prevented<br />
The <strong>in</strong>fant <strong>in</strong> the case report had many of the factors that<br />
<strong>in</strong>crease the risk of severe hyperbilirub<strong>in</strong>emia (Table 6).<br />
A key recommendation <strong>in</strong> the American Academy of<br />
Pediatrics (AAP) cl<strong>in</strong>ical practice guidel<strong>in</strong>e (Table 7) is<br />
that every <strong>in</strong>fant be assessed for the risk of subsequent<br />
severe hyperbilirub<strong>in</strong>emia before discharge, particularly<br />
446 Pediatrics <strong>in</strong> Review Vol.27 No.12 December 2006<br />
Downloaded from http://peds<strong>in</strong>review.aappublications.org by J Michael Coleman on June 4, 2010
neonatology<br />
neonatal jaundice<br />
Table 5. Major Cl<strong>in</strong>ical Features<br />
of Chronic Postkernicteric<br />
Bilirub<strong>in</strong> Encephalopathy<br />
● Extrapyramidal abnormalities, especially athetosis<br />
● Gaze abnormalities, especially of upward gaze<br />
● Auditory disturbance, especially sensor<strong>in</strong>eural hear<strong>in</strong>g<br />
loss<br />
● Intellectual deficits, but m<strong>in</strong>ority <strong>in</strong> mentally<br />
retarded range<br />
Repr<strong>in</strong>ted with permission from Maisels MJ. <strong>Jaundice</strong>. In: MacDonald<br />
MG, Seshia MMK, Mullett MD, eds. Neonatology: Pathophysiology and<br />
Management of the <strong>Newborn</strong>. Philadelphia, Pa: Lipp<strong>in</strong>cott Co; 2005:<br />
768–846.<br />
<strong>in</strong>fants discharged before age 72 hours. The <strong>in</strong>fant described<br />
<strong>in</strong> the case was a 36 weeks’ gestation, breastfed<br />
male who was discharged at age 30 hours. Two of the risk<br />
factors that have been shown repeatedly to be very important<br />
are a gestational age less than 38 weeks and<br />
breastfeed<strong>in</strong>g, particularly if nurs<strong>in</strong>g is not go<strong>in</strong>g well.<br />
Almost every recently described case of kernicterus has<br />
occurred <strong>in</strong> a breastfed <strong>in</strong>fant, and <strong>in</strong>fants of 35 to<br />
36 weeks’ gestation are about 13 times more likely than<br />
those at 40 weeks’ gestation to be readmitted for severe<br />
jaundice. These so called “near-term” <strong>in</strong>fants receive care<br />
<strong>in</strong> well-baby nurseries, but unlike their term peers, they<br />
are much more likely to nurse <strong>in</strong>effectively, receive fewer<br />
calories, and have greater weight loss. In addition, the<br />
immaturity of the liver’s conjugat<strong>in</strong>g system <strong>in</strong> the preterm<br />
newborn makes it much more difficult for the<br />
<strong>in</strong>fants to clear bilirub<strong>in</strong> effectively. Thus, it is not surpris<strong>in</strong>g<br />
that they become more jaundiced.<br />
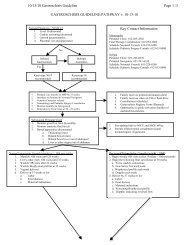
In addition, the <strong>in</strong>fant’s TSB was 7.5 mg/dL<br />
(128.3 mcmol/L) at age 25 hours, a value very close to<br />
the 95th percentile (Fig. 2). Another TSB measurement<br />
should have been obta<strong>in</strong>ed with<strong>in</strong> 24 hours and a<br />
follow-up visit scheduled no less than 48 hours after<br />
discharge. In addition, when the doctor’s office was told<br />
that the <strong>in</strong>fant was not nurs<strong>in</strong>g well, was sleepy, and was<br />
jaundiced, the <strong>in</strong>fant should have been seen immediately.<br />
The mother was describ<strong>in</strong>g the first stage of acute bilirub<strong>in</strong><br />
encephalopathy (Table 4).<br />
Appropriate Follow-up is Essential<br />
If the <strong>in</strong>fant <strong>in</strong> the case had been seen with<strong>in</strong> 48 hours of<br />
discharge (before he was 4 days old), significant jaundice<br />
certa<strong>in</strong>ly would have been noted, bilirub<strong>in</strong> would have<br />
been measured, and he would have been treated with<br />
phototherapy, thus prevent<strong>in</strong>g the disastrous outcome<br />
Table 6. Risk Factors for<br />
Development of Severe<br />
Hyperbilirub<strong>in</strong>emia <strong>in</strong> Infants<br />
>35 Weeks’ Gestation (In<br />
Approximate Order of<br />
Importance)<br />
Major Risk Factors<br />
● Predischarge TSB or TcB level <strong>in</strong> the high-risk zone<br />
(Fig. 2)<br />
● <strong>Jaundice</strong> observed <strong>in</strong> the first 24 h<br />
● Blood group <strong>in</strong>compatibility with positive direct<br />
antiglobul<strong>in</strong> test, other known hemolytic disease (eg,<br />
G-6PD deficiency), elevated ETCOc<br />
● Gestational age 35 to 36 wk<br />
● Previous sibl<strong>in</strong>g received phototherapy<br />
● Cephalhematoma or significant bruis<strong>in</strong>g<br />
● Exclusive breastfeed<strong>in</strong>g, particularly if nurs<strong>in</strong>g is not<br />
go<strong>in</strong>g well and weight loss is excessive<br />
● East Asian race*<br />
M<strong>in</strong>or Risk Factors<br />
● Predischarge TSB or TcB <strong>in</strong> the high- to<br />
<strong>in</strong>termediate-risk zone (Fig. 2)<br />
● Gestational age 37 to 38 wk<br />
● <strong>Jaundice</strong> observed before discharge<br />
● Previous sibl<strong>in</strong>g had jaundice<br />
● Macrosomia <strong>in</strong> an <strong>in</strong>fant of a diabetic mother<br />
● Maternal age >25 y<br />
● Male sex<br />
Decreased Risk<br />
(These factors are associated with decreased risk of<br />
significant jaundice, listed <strong>in</strong> order of decreas<strong>in</strong>g<br />
importance.)<br />
● TSB or TcB <strong>in</strong> the low-risk zone (Fig. 2)<br />
● Gestational age >41 wk<br />
● Exclusive formula feed<strong>in</strong>g<br />
● Black race*<br />
● Discharge from hospital after 72 h<br />
*Race as def<strong>in</strong>ed by mother’s description. TSBtotal serum bilirub<strong>in</strong>,<br />
TcBtranscutaneous bilirub<strong>in</strong>, G-6PDglucose-6-phosphate dehydrogenase,<br />
ETCOcend tidal carbon monoxide concentration corrected<br />
for ambient carbon monoxide<br />
Repr<strong>in</strong>ted with permission from Maisels MJ, Baltz RD, Bhutani V, et<br />
al. Management of hyperbilirub<strong>in</strong>emia <strong>in</strong> the newborn <strong>in</strong>fant 35 or<br />
more weeks of gestation. Pediatrics. 2004;114:297–316.<br />
that occurred. The AAP now recommends that any <strong>in</strong>fant<br />
discharged at less than 72 hours of age should be<br />
seen with<strong>in</strong> 2 days of discharge. Infants who have many<br />
risk factors might need to be seen earlier (with<strong>in</strong> 24 h of<br />
discharge), which would have been appropriate for this<br />
<strong>in</strong>fant. Such follow-up is critical to protect <strong>in</strong>fants from<br />
Pediatrics <strong>in</strong> Review Vol.27 No.12 December 2006 447<br />
Downloaded from http://peds<strong>in</strong>review.aappublications.org by J Michael Coleman on June 4, 2010
neonatology<br />
neonatal jaundice<br />
Table 7. The Ten Commandments<br />
for Prevent<strong>in</strong>g and Manag<strong>in</strong>g<br />
Hyperbilirub<strong>in</strong>emia<br />
1. Promote and support successful breastfeed<strong>in</strong>g.<br />
2. Establish nursery protocols for the jaundiced<br />
newborn and permit nurses to obta<strong>in</strong> TSB levels<br />
without a physician’s order.<br />
3. Measure the TSB or TcB concentrations of <strong>in</strong>fants<br />
jaundiced <strong>in</strong> the first 24 h after birth.<br />
4. Recognize that visual diagnosis of jaundice is<br />
unreliable, particularly <strong>in</strong> darkly pigmented <strong>in</strong>fants.<br />
5. Interpret all TSB levels accord<strong>in</strong>g to the <strong>in</strong>fant’s<br />
age <strong>in</strong> hours, not days.<br />
6. Do not treat a near-term (35 to 38 wk) <strong>in</strong>fant as<br />
a term <strong>in</strong>fant; a near-term <strong>in</strong>fant is at much<br />
higher risk of hyperbilirub<strong>in</strong>emia.<br />
7. Perform a predischarge systematic assessment on<br />
all <strong>in</strong>fants for the risk of severe<br />
hyperbilirub<strong>in</strong>emia.<br />
8. Provide parents with <strong>in</strong>formation about newborn<br />
jaundice.<br />
9. Provide follow-up based on the time of discharge<br />
and the risk assessment.<br />
10. When <strong>in</strong>dicated, treat the newborn with<br />
phototherapy or exchange transfusion.<br />
TSBtotal serum bilirub<strong>in</strong>, TcBtranscutaneous bilirub<strong>in</strong><br />
Repr<strong>in</strong>ted with permission from Maisels MJ. <strong>Jaundice</strong> <strong>in</strong> a newborn.<br />
How to head off an urgent situation. Contemp Pediatr. 2005;22:<br />
41–54, with permission. Adapted from Pediatrics. 2004;114:297–316.<br />
severe hyperbilirub<strong>in</strong>emia and kernicterus. Nevertheless,<br />
cl<strong>in</strong>ical judgment is required at the time of discharge. If a<br />
41-weeks’ gestation, formula-fed, nonjaundiced <strong>in</strong>fant is<br />
discharged and has no significant risk factors (Table 6), a<br />
follow-up visit after 3 or 4 days is acceptable. The absence<br />
of risk factors and any decision for a later follow up<br />
should be documented <strong>in</strong> the chart. If, on the other<br />
hand, a 36-weeks’ gestation breastfed newborn is discharged<br />
on a Friday, he or she should be seen no later<br />
than Sunday.<br />
If follow-up cannot be assured and there is a significant<br />
risk of severe hyperbilirub<strong>in</strong>emia, the cl<strong>in</strong>ician may<br />
need to delay discharge. If weekend follow-up is difficult<br />
or impossible, a reasonable option is to have the <strong>in</strong>fant<br />
brought to a laboratory for a bilirub<strong>in</strong> measurement (or a<br />
transcutaneous bilirub<strong>in</strong> measurement).<br />
Management of <strong>Jaundice</strong> <strong>in</strong> the Infant<br />
Interpret<strong>in</strong>g Serum Bilirub<strong>in</strong> Levels<br />
TSB (or transcutaneous bilirub<strong>in</strong> [TcB]) concentrations<br />
generally peak by the third to fifth day after birth (Fig.<br />
2 and Fig. 1-E). (The latter figure is available only <strong>in</strong> the<br />
onl<strong>in</strong>e edition of this article.) In the past, when newborns<br />
rema<strong>in</strong>ed <strong>in</strong> the hospital for 3 or 4 days, jaundiced babies<br />
could be identified before discharge and appropriately<br />
evaluated and treated. Today, because almost all <strong>in</strong>fants<br />
delivered vag<strong>in</strong>ally leave the hospital before they are<br />
48 hours old, the bilirub<strong>in</strong> concentration peaks after<br />
discharge. Because the TSB has not yet peaked at the<br />
time of discharge, the AAP provides str<strong>in</strong>gent guidel<strong>in</strong>es<br />
for follow-up of all <strong>in</strong>fants discharged before 72 hours of<br />
age: They should be seen with<strong>in</strong> 2 days of discharge.<br />
In addition, it is essential that all TSB values be<br />
<strong>in</strong>terpreted <strong>in</strong> terms of the <strong>in</strong>fant’s age <strong>in</strong> hours and not<br />
<strong>in</strong> days. Although cl<strong>in</strong>icians often talk about a TSB<br />
concentration on day 2 or day 3, Figure 2 (and Figure<br />
1-E <strong>in</strong> the onl<strong>in</strong>e edition) shows how mislead<strong>in</strong>g this<br />
thought process can be. A TSB of 8 mg/dL (136.8<br />
mcmol/L) at 24.1 hours is above the 95th percentile and<br />
calls for evaluation and close follow-up, whereas the same<br />
level at 47.9 hours is <strong>in</strong> the low-risk zone (Fig. 2) and<br />
probably warrants no further concern. Yet, both values<br />
occur on postnatal day 2. In the case, the TSB value at<br />
25 hours was 7.5 mg/dL (128.3 mcmol/L), very close<br />
to the 95th percentile. Consideration should have been<br />
given to additional <strong>in</strong>vestigations to try to determ<strong>in</strong>e why<br />
the <strong>in</strong>fant was jaundiced, a subsequent TSB should have<br />
been measured with<strong>in</strong> 24 hours, and follow-up should<br />
have been scheduled no later than 48 hours after discharge.<br />
When to Seek a Cause for <strong>Jaundice</strong><br />
In some <strong>in</strong>fants, the cause of hyperbilirub<strong>in</strong>emia is apparent<br />
from the history and physical exam<strong>in</strong>ation f<strong>in</strong>d<strong>in</strong>gs.<br />
For example, jaundice <strong>in</strong> a severely bruised <strong>in</strong>fant needs<br />
no further explanation, nor is there a need to <strong>in</strong>vestigate<br />
why a 5-day-old breastfed <strong>in</strong>fant has a TSB value of<br />
15 mg/dL (256.5 mcmol/L). On the other hand, if the<br />
TSB concentration is above the 95th percentile or ris<strong>in</strong>g<br />
rapidly and cross<strong>in</strong>g percentiles (Fig. 2 and Fig.1-E <strong>in</strong> the<br />
onl<strong>in</strong>e edition), and this cannot be readily expla<strong>in</strong>ed by<br />
the history and physical exam<strong>in</strong>ation results, certa<strong>in</strong> laboratory<br />
tests should be performed (Table 8).<br />
Predict<strong>in</strong>g the Risk of Hyperbilirub<strong>in</strong>emia<br />
Before discharge, every newborn needs to be assessed for<br />
the risk of subsequent severe hyperbilirub<strong>in</strong>emia. This<br />
can be accomplished by us<strong>in</strong>g cl<strong>in</strong>ical criteria (Table 6) or<br />
measur<strong>in</strong>g a TSB or TcB concentration prior to discharge.<br />
In the case described, the <strong>in</strong>fant had several risk<br />
factors for hyperbilirub<strong>in</strong>emia, and his TSB measured at<br />
26 hours was <strong>in</strong> the high <strong>in</strong>termediate-risk zone (Fig. 2),<br />
448 Pediatrics <strong>in</strong> Review Vol.27 No.12 December 2006<br />
Downloaded from http://peds<strong>in</strong>review.aappublications.org by J Michael Coleman on June 4, 2010
neonatology<br />
neonatal jaundice<br />
Figure 2. Establish<strong>in</strong>g “risk zones” for the prediction of hyperbilirub<strong>in</strong>emia <strong>in</strong> newborns. This nomogram is based on hour-specific<br />
bilirub<strong>in</strong> values obta<strong>in</strong>ed from 2,840 well newborns >36 weeks gestational age whose birthweights were >2,000 g or >35 weeks<br />
gestational age whose birthweights were >2,500 g. The serum bilirub<strong>in</strong> concentration was measured before discharge. The risk zone<br />
<strong>in</strong> which the value fell predicted the likelihood of a subsequent bilirub<strong>in</strong> level exceed<strong>in</strong>g the 95th percentile. Repr<strong>in</strong>ted with<br />
permission from Bhutani VK, Johnson L, Sivieri EM. Predictive ability of a predischarge hour-specific serum bilirub<strong>in</strong> for subsequent<br />
significant hyperbilirub<strong>in</strong>emia <strong>in</strong> healthy-term and near-term newborns. Pediatrics. 1999;103:6–14.<br />
plac<strong>in</strong>g him at significant risk for subsequent development<br />
of hyperbilirub<strong>in</strong>emia.<br />
Visual Assessment of <strong>Jaundice</strong><br />
Traditional identification of jaundice relied on blanch<strong>in</strong>g<br />
the sk<strong>in</strong> with digital pressure to reveal the underly<strong>in</strong>g<br />
color of the sk<strong>in</strong> and subcutaneous tissue. Although this<br />
rema<strong>in</strong>s a fundamentally important cl<strong>in</strong>ical sign, it has<br />
limitations and can be unreliable, particularly <strong>in</strong> darkly<br />
pigmented <strong>in</strong>fants. The difference between a TSB value<br />
of 5 mg/dL (85.5 mcmol/L) and 8 mg/dL (136.8<br />
mcmol/L) cannot be perceived by the eye, but this<br />
represents the difference between the 50th and the 95th<br />
percentiles at 24 hours (Fig. 2). The potential errors<br />
associated with visual diagnosis have led some experts to<br />
recommend that all newborns have a TSB or TcB measured<br />
prior to discharge. The TSB can be obta<strong>in</strong>ed at the<br />
same time as the metabolic screen, spar<strong>in</strong>g the <strong>in</strong>fant an<br />
additional heel stick.<br />
Non<strong>in</strong>vasive Bilirub<strong>in</strong> Measurement<br />
Two hand-held electronic devices are available <strong>in</strong> the<br />
United States for measur<strong>in</strong>g TcB. They provide an estimate<br />
of the TSB concentration, and a close correlation<br />
has been found between TcB and TSB measurements <strong>in</strong><br />
different racial populations.<br />
TcB measurement (Fig. 1-E <strong>in</strong> the onl<strong>in</strong>e edition) is<br />
not a substitute for TSB measurement, but TcB can be<br />
very helpful. When used as a screen<strong>in</strong>g tool, TcB measurement<br />
can help to answer the questions, “Should I<br />
worry about this <strong>in</strong>fant” and “Should I obta<strong>in</strong> a TSB on<br />
this <strong>in</strong>fant” Because the goal is to avoid miss<strong>in</strong>g a<br />
significantly elevated TSB value, the value for the TcB<br />
measurement (based on the <strong>in</strong>fant’s age <strong>in</strong> hours and<br />
Pediatrics <strong>in</strong> Review Vol.27 No.12 December 2006 449<br />
Downloaded from http://peds<strong>in</strong>review.aappublications.org by J Michael Coleman on June 4, 2010
neonatology<br />
neonatal jaundice<br />
Table 8. Laboratory Tests for the <strong>Jaundice</strong>d Infant<br />
When there is a f<strong>in</strong>d<strong>in</strong>g of:<br />
<strong>Jaundice</strong> <strong>in</strong> first 24 h<br />
<strong>Jaundice</strong> that appears excessive for the <strong>in</strong>fant’s age<br />
An <strong>in</strong>fant receiv<strong>in</strong>g phototherapy or hav<strong>in</strong>g a TSB that is<br />
above the 75th percentile or ris<strong>in</strong>g rapidly (ie, cross<strong>in</strong>g<br />
percentiles) and unexpla<strong>in</strong>ed by history or f<strong>in</strong>d<strong>in</strong>gs on<br />
physical exam<strong>in</strong>ation<br />
A TSB approach<strong>in</strong>g exchange level or not respond<strong>in</strong>g to<br />
phototherapy<br />
An elevated direct (or conjugated) bilirub<strong>in</strong> level<br />
<strong>Jaundice</strong> present at or beyond age 3 wk or the <strong>in</strong>fant<br />
is sick<br />
Obta<strong>in</strong>:<br />
Total serum bilirub<strong>in</strong> (TSB)<br />
TSB<br />
Blood type; also, perform a Coombs test, if not obta<strong>in</strong>ed with<br />
cord blood<br />
Complete blood count, smear, and reticulocyte count<br />
Direct (or conjugated) bilirub<strong>in</strong><br />
(Repeat TSB <strong>in</strong> 4 to 24 hours, depend<strong>in</strong>g on <strong>in</strong>fant’s age and<br />
TSB level)<br />
Consider the possibility of glucose-6-phosphate<br />
dehydrogenase (G-6PD) deficiency, particularly <strong>in</strong> African-<br />
American <strong>in</strong>fants<br />
Reticulocyte count, G-6PD test, album<strong>in</strong><br />
Ur<strong>in</strong>alysis and ur<strong>in</strong>e culture; evaluate for sepsis if <strong>in</strong>dicated<br />
by history and physical exam<strong>in</strong>ation<br />
Total and direct bilirub<strong>in</strong> concentration; if direct bilirub<strong>in</strong> is<br />
elevated, evaluate for causes of cholestasis<br />
(Also check results of newborn thyroid and galactosemia<br />
screen and evaluate <strong>in</strong>fant for signs or symptoms of<br />
hypothyroidism)<br />
Repr<strong>in</strong>ted with permission from Maisels MJ. <strong>Jaundice</strong> <strong>in</strong> a newborn. How to head off an urgent situation. Contemp Pediatr. 2005;22:41–54. Adapted with<br />
permission from Pediatrics. 2004;14:297–316.<br />
other risk factors) always should be one above which a<br />
TSB value always will be obta<strong>in</strong>ed. In our nursery, we<br />
rout<strong>in</strong>ely evaluate <strong>in</strong>fants via a TcB measurement and<br />
obta<strong>in</strong> a TSB whenever the TcB is above the 75th percentile<br />
(Fig. 2) (or the 95th percentile <strong>in</strong> Fig. 1-E).<br />
Treatment<br />
Hyperbilirub<strong>in</strong>emia can be treated via: 1) exchange<br />
transfusion to remove bilirub<strong>in</strong> mechanically; 2) phototherapy<br />
to convert bilirub<strong>in</strong> to products that can bypass<br />
the liver’s conjugat<strong>in</strong>g system and be excreted <strong>in</strong> the bile<br />
or <strong>in</strong> the ur<strong>in</strong>e without further metabolism; and 3) pharmacologic<br />
agents to <strong>in</strong>terfere with heme degradation and<br />
bilirub<strong>in</strong> production, accelerate the normal metabolic<br />
pathways for bilirub<strong>in</strong> appearance, or <strong>in</strong>hibit the enterohepatic<br />
circulation of bilirub<strong>in</strong>. Guidel<strong>in</strong>es for the use of<br />
phototherapy and exchange transfusion <strong>in</strong> term and<br />
near-term <strong>in</strong>fants are provided <strong>in</strong> Figs. 3 and 4 and Table<br />
9.<br />
Phototherapy<br />
Phototherapy works by <strong>in</strong>fus<strong>in</strong>g discrete photons of energy<br />
similar to the molecules of a drug. These photons<br />
are absorbed by bilirub<strong>in</strong> molecules <strong>in</strong> the sk<strong>in</strong> and<br />
subcutaneous tissue, just as drug molecules b<strong>in</strong>d to a<br />
receptor. The bilirub<strong>in</strong> then undergoes photochemical<br />
reactions to form excretable isomers and breakdown<br />
products that can bypass the liver’s conjugat<strong>in</strong>g system<br />
and be excreted without further metabolism. Some<br />
photo products also are excreted <strong>in</strong> the ur<strong>in</strong>e.<br />
Phototherapy displays a clear dose-response effect,<br />
and a number of variables <strong>in</strong>fluence how light works to<br />
lower the TSB level. (In the onl<strong>in</strong>e edition of this article,<br />
Table 1-E shows the radiometric units used to measure<br />
the dose of phototherapy and Tables 2-E and 3-E show<br />
the factors that affect the dose and efficacy of phototherapy,<br />
<strong>in</strong>clud<strong>in</strong>g type of light source, the <strong>in</strong>fant’s distance<br />
from the light, and the surface area exposed.) Because of<br />
the optical properties of bilirub<strong>in</strong> and sk<strong>in</strong>, the most<br />
effective lights are those that have wavelengths predom<strong>in</strong>ately<br />
<strong>in</strong> the blue-green spectrum (425 to 490 nm). At<br />
these wavelengths, light penetrates the sk<strong>in</strong> well and is<br />
absorbed maximally by bilirub<strong>in</strong>.<br />
Us<strong>in</strong>g Phototherapy Effectively<br />
Phototherapy was used <strong>in</strong>itially <strong>in</strong> low-birthweight and<br />
term <strong>in</strong>fants primarily to prevent slowly ris<strong>in</strong>g bilirub<strong>in</strong><br />
concentrations from reach<strong>in</strong>g levels that might require<br />
exchange transfusion. Today, phototherapy often is used<br />
<strong>in</strong> term and near-term <strong>in</strong>fants who have left the hospital<br />
and are readmitted on days 4 to 7 for treatment of TSB<br />
concentrations of 20 mg/dL (342 mcmol/L) or more.<br />
Such <strong>in</strong>fants require a full therapeutic dose of phototherapy<br />
(now termed <strong>in</strong>tensive phototherapy) to reduce the<br />
450 Pediatrics <strong>in</strong> Review Vol.27 No.12 December 2006<br />
Downloaded from http://peds<strong>in</strong>review.aappublications.org by J Michael Coleman on June 4, 2010
neonatology<br />
neonatal jaundice<br />
Figure 3. The risk factors listed for this figure <strong>in</strong>crease the likelihood of bra<strong>in</strong> damage at different bilirub<strong>in</strong> concentrations. Infants<br />
are designated as “higher risk” because of the potential negative effects of the conditions listed on album<strong>in</strong> b<strong>in</strong>d<strong>in</strong>g of bilirub<strong>in</strong>, the<br />
blood-bra<strong>in</strong> barrier, and the susceptibility of the bra<strong>in</strong> cells to damage by bilirub<strong>in</strong>. “Intensive phototherapy” implies irradiance <strong>in</strong><br />
the blue-green spectrum (wavelengths of approximately 430 to 490 nm) of at least 30 mcW/cm 2 per nanometer (measured at the<br />
<strong>in</strong>fant’s sk<strong>in</strong> directly below the center of the phototherapy unit) and delivered to as much of the <strong>in</strong>fant’s surface area as possible.<br />
Note that irradiance measured below the center of the light source is much greater than that measured at the periphery.<br />
Measurements should be made with a radiometer specified by the manufacturer of the phototherapy system. If total serum bilirub<strong>in</strong><br />
values approach or exceed the exchange transfusion l<strong>in</strong>e, the sides of the bass<strong>in</strong>et, <strong>in</strong>cubator, or warmer should be l<strong>in</strong>ed with<br />
alum<strong>in</strong>um foil or white material to <strong>in</strong>crease the surface area of the <strong>in</strong>fant exposed and <strong>in</strong>crease the efficacy of phototherapy. If the<br />
total serum bilirub<strong>in</strong> value does not decrease or cont<strong>in</strong>ues to rise <strong>in</strong> an <strong>in</strong>fant who is receiv<strong>in</strong>g <strong>in</strong>tensive phototherapy, this strongly<br />
suggests the presence of hemolysis. Infants who receive phototherapy and have an elevated direct-react<strong>in</strong>g or conjugated bilirub<strong>in</strong><br />
level (cholestatic jaundice) may develop the bronze baby syndrome. Repr<strong>in</strong>ted with permission from Maisels MJ, Baltz RD, Bhutani<br />
V, et al. Management of hyperbilirub<strong>in</strong>emia <strong>in</strong> the newborn <strong>in</strong>fant 35 or more weeks of gestation. Pediatrics. 2004;114:297–316.<br />
bilirub<strong>in</strong> concentration as soon as possible. Intensive<br />
phototherapy implies the use of irradiance <strong>in</strong> the 430 to<br />
490-nm band of at least 30 mcW/cm 2 per nanometer<br />
delivered to as much of the <strong>in</strong>fant’s surface area as possible<br />
(Table 2-E <strong>in</strong> the onl<strong>in</strong>e edition of this article).<br />
Increas<strong>in</strong>g the surface area exposed to phototherapy<br />
improves the therapy’s efficacy significantly. This is accomplished<br />
by plac<strong>in</strong>g fiberoptic pads or a light-emitt<strong>in</strong>g<br />
diode (LED) mattress below the <strong>in</strong>fant or us<strong>in</strong>g a phototherapy<br />
device that delivers phototherapy from special<br />
blue fluorescent tubes both above and below the <strong>in</strong>fant.<br />
When <strong>in</strong>tensive phototherapy is applied appropriately, a<br />
Pediatrics <strong>in</strong> Review Vol.27 No.12 December 2006 451<br />
Downloaded from http://peds<strong>in</strong>review.aappublications.org by J Michael Coleman on June 4, 2010
neonatology<br />
neonatal jaundice<br />
Figure 4. The risk factors listed for this figure are factors that <strong>in</strong>crease the likelihood of bra<strong>in</strong> damage at different bilirub<strong>in</strong> levels.<br />
Infants are designated as “higher risk” because of the potential negative effects of the conditions listed on album<strong>in</strong> b<strong>in</strong>d<strong>in</strong>g of<br />
bilirub<strong>in</strong>, the blood-bra<strong>in</strong> barrier, and the susceptibility of the bra<strong>in</strong> cells to damage by bilirub<strong>in</strong>.<br />
30% to 40% decrement <strong>in</strong> the bilirub<strong>in</strong> concentration can<br />
be expected <strong>in</strong> the first 24 hours, with the most significant<br />
decl<strong>in</strong>e occurr<strong>in</strong>g <strong>in</strong> the first 4 to 6 hours.<br />
Pharmacologic Treatment<br />
Pharmacologic agents such as phenobarbital and ursodeoxycholic<br />
acid improve bile flow and can help to lower<br />
bilirub<strong>in</strong> concentrations. T<strong>in</strong> mesoporphyr<strong>in</strong> <strong>in</strong>hibits<br />
heme oxygenase and, therefore, the production of bilirub<strong>in</strong><br />
(Fig. 1). To date, more than 500 newborns have<br />
received t<strong>in</strong> mesoporphyr<strong>in</strong> <strong>in</strong> control trials, but the drug<br />
still is await<strong>in</strong>g United States Food and Drug Adm<strong>in</strong>istration<br />
approval. Other drugs have been used to <strong>in</strong>hibit<br />
the enterohepatic circulation of bilirub<strong>in</strong>. A recent controlled<br />
trial showed that agents that <strong>in</strong>hibit beta glucuronidase<br />
can decrease bilirub<strong>in</strong> levels <strong>in</strong> breastfed new-<br />
452 Pediatrics <strong>in</strong> Review Vol.27 No.12 December 2006<br />
Downloaded from http://peds<strong>in</strong>review.aappublications.org by J Michael Coleman on June 4, 2010
neonatology<br />
neonatal jaundice<br />
Table 9. Additional Guidel<strong>in</strong>es for Exchange Transfusion<br />
These ratios can be used together with but not <strong>in</strong> lieu of the TSB concentration as an additional factor <strong>in</strong> determ<strong>in</strong><strong>in</strong>g the need<br />
for exchange transfusion.<br />
Risk Category<br />
Bilirub<strong>in</strong>/Album<strong>in</strong> Ratio at Which Exchange Transfusion<br />
Should be Considered<br />
TSB (mg/dL)-to-Album<strong>in</strong><br />
(dL)<br />
Infants >38 0/7 wk 8.0 0.94<br />
Infants 35 0/7 to 37 6/7 wk and well or >38 0/7 wk 7.2 0.84<br />
if higher risk or isoimmune hemolytic disease or G-<br />
6PD deficiency<br />
Infants 35 0/7 to 37 6/7 wk if higher risk or<br />
isoimmune hemolytic disease or G-6PD deficiency<br />
6.8 0.80<br />
TSB (mcmol/L)-to-Album<strong>in</strong><br />
(mcmol/L)<br />
TSBtotal serum bilirub<strong>in</strong>, G-6PDglucose–6–phosphate dehydrogenase. Repr<strong>in</strong>ted with permission from Maisels MJ, Baltz RD, Bhutani V, et al.<br />
Management of hyperbilirub<strong>in</strong>emia <strong>in</strong> the newborn <strong>in</strong>fant 35 or more weeks of gestation. Pediatrics. 2004;114:297–316.<br />
borns. For <strong>in</strong>fants who have isoimmune hemolytic<br />
disease, the adm<strong>in</strong>istration of <strong>in</strong>travenous immunoglobul<strong>in</strong><br />
significantly reduces the need for exchange transfusion.<br />
Suggested Read<strong>in</strong>g<br />
Bhutani V, Gourley GR, Adler S, Kreamer B, Dalman C, Johnson<br />
LH. Non<strong>in</strong>vasive measurement of total serum bilirub<strong>in</strong> <strong>in</strong> a<br />
multiracial predischarge newborn population to assess the risk of<br />
severe hyperbilirub<strong>in</strong>emia. Pediatrics. 2000;106:e17. Available<br />
at: http://pediatrics.aappublications.org/cgi/content/full/<br />
106/2/e17<br />
Bhutani VK, Johnson LH, Maisels MJ, et al. Kernicterus: epidemiological<br />
strategies for its prevention through systems-based<br />
approaches. J Per<strong>in</strong>atol. 2004;24:650–662<br />
Bhutani VK, Johnson L, Sivieri EM. Predictive ability of a predischarge<br />
hour-specific serum bilirub<strong>in</strong> for subsequent significant<br />
hyperbilirub<strong>in</strong>emia <strong>in</strong> healthy term and near-term newborns.<br />
Pediatrics. 1999;103:6–14<br />
Ennever JF. Blue light, green light, white light, more light: treatment<br />
of neonatal jaundice. Cl<strong>in</strong> Per<strong>in</strong>atol. 1990;17:467–481<br />
Kaplan M, Hammerman C. Severe neonatal hyperbilirub<strong>in</strong>emia: a<br />
potential complication of glucose-6-phosphate dehydrogenase<br />
deficiency. Cl<strong>in</strong> Per<strong>in</strong>atol. 1998;25:575–590<br />
Kaplan M, Hammerman C, Maisels MJ. Bilirub<strong>in</strong> genetics for the<br />
nongeneticist: hereditary defects of neonatal bilirub<strong>in</strong> conjugation.<br />
Pediatrics. 2003;111:886–893<br />
Kappas A. A method for <strong>in</strong>terdict<strong>in</strong>g the development of severe<br />
jaundice <strong>in</strong> newborns by <strong>in</strong>hibit<strong>in</strong>g the production of bilirub<strong>in</strong>.<br />
Pediatrics. 2004;113:119–123<br />
Maisels MJ. A primer on phototherapy for the jaundiced newborn.<br />
Contemp Pediatr. 2005;22:38–57<br />
Maisels MJ. <strong>Jaundice</strong>. In: MacDonald MG, Seshia MMK, Mullett<br />
MD, eds. Neonatology: Pathophysiology and Management of the<br />
<strong>Newborn</strong>. Philadelphia, Pa: Lipp<strong>in</strong>cott Co; 2005:768–846<br />
Maisels MJ. <strong>Jaundice</strong> <strong>in</strong> a newborn. Answers to questions about a<br />
common cl<strong>in</strong>ical problem. Contemp Pediatr. 2005;22:34–40<br />
Maisels MJ. <strong>Jaundice</strong> <strong>in</strong> a newborn. How to head off an urgent<br />
situation. Contemp Pediatr. 2005;22:41–54<br />
Maisels MJ. Why use homeopathic doses of phototherapy Pediatrics.<br />
1996;98:283–287<br />
Maisels MJ, Baltz RD, Bhutani V, et al. Management of hyperbilirub<strong>in</strong>emia<br />
<strong>in</strong> the newborn <strong>in</strong>fant 35 or more weeks of gestation.<br />
Pediatrics. 2004;114:297–316<br />
Maisels MJ, Kr<strong>in</strong>g EA. Transcutaneous bilirub<strong>in</strong> levels <strong>in</strong> the first<br />
96 hours <strong>in</strong> a normal newborn population of 35 weeks’<br />
gestation. Pediatrics. 2006;117:1169–1173<br />
Maisels MJ. Ostrea EJ Jr, Touch S, et al. Evaluation of a new transcutaneous<br />
bilirub<strong>in</strong>ometer. Pediatrics. 2004;113:1628–1635<br />
Newman TB, Liljestrand P, Jeremy RJ, et al. Outcomes among<br />
newborns with total serum bilirub<strong>in</strong> levels of 25 mg per deciliter<br />
or more. N Engl J Med. 2006;354:1889–1900<br />
Newman TB, Xiong B, Gonzales VM, Escobar GJ. Prediction and<br />
prevention of extreme neonatal hyperbilirub<strong>in</strong>emia <strong>in</strong> a mature<br />
health ma<strong>in</strong>tenance organization. Arch Pediatr Adolesc Med.<br />
2000;154:1140–1147<br />
Stevenson DK, Dennery PA, H<strong>in</strong>tz SR. Understand<strong>in</strong>g newborn<br />
jaundice. J Per<strong>in</strong>atol. 2001;21:S21–S24<br />
Pediatrics <strong>in</strong> Review Vol.27 No.12 December 2006 453<br />
Downloaded from http://peds<strong>in</strong>review.aappublications.org by J Michael Coleman on June 4, 2010
neonatology<br />
neonatal jaundice<br />
PIR Quiz<br />
Quiz also available onl<strong>in</strong>e at www.peds<strong>in</strong>review.org.<br />
1. In expla<strong>in</strong><strong>in</strong>g breastfeed<strong>in</strong>g-associated jaundice to the third-year students on your service, you note that<br />
jaundice seen <strong>in</strong> the first postnatal week results from an <strong>in</strong>crease <strong>in</strong> the enterohepatic circulation due<br />
primarily to:<br />
A. Decreased caloric <strong>in</strong>take.<br />
B. Gilbert syndrome.<br />
C. Increased prote<strong>in</strong> b<strong>in</strong>d<strong>in</strong>g.<br />
D. Insufficient free water.<br />
E. Polycythemia.<br />
2. The American Academy of Pediatrics now recommends that any <strong>in</strong>fant discharged before 72 hours of age<br />
be seen for follow-up no longer than how many hours later<br />
A. 24.<br />
B. 36.<br />
C. 48.<br />
D. 72.<br />
E. 96.<br />
3. Almost all <strong>in</strong>fants experience a transient <strong>in</strong>crease <strong>in</strong> bilirub<strong>in</strong> concentrations known as physiologic jaundice<br />
dur<strong>in</strong>g the first week after birth. Among the follow<strong>in</strong>g, which is most likely to contribute to the<br />
development of this condition<br />
A. Decreased enterohepatic circulation.<br />
B. Decreased erythrocyte survival.<br />
C. Decreased erythrocyte volume.<br />
D. Increased bilirub<strong>in</strong> conjugation.<br />
E. Increased ligand<strong>in</strong> levels.<br />
4. A 36 weeks’ gestation breastfed African-American <strong>in</strong>fant is be<strong>in</strong>g discharged at 36 hours of age. The<br />
transcutaneous bilirub<strong>in</strong> level is above the 75th percentile. Of the follow<strong>in</strong>g, the next most appropriate step<br />
<strong>in</strong> the management of this <strong>in</strong>fant is to:<br />
A. Advise the mother to <strong>in</strong>crease the frequency of breastfeed<strong>in</strong>g.<br />
B. Check the mother’s and the baby’s blood groups.<br />
C. Obta<strong>in</strong> a complete blood count and differential count.<br />
D. Obta<strong>in</strong> a serum bilirub<strong>in</strong> measurement.<br />
E. Start phototherapy.<br />
454 Pediatrics <strong>in</strong> Review Vol.27 No.12 December 2006<br />
Downloaded from http://peds<strong>in</strong>review.aappublications.org by J Michael Coleman on June 4, 2010
<strong>Neonatal</strong> <strong>Jaundice</strong><br />
M. Jeffrey Maisels<br />
Pediatr. Rev. 2006;27;443-454<br />
DOI: 10.1542/pir.27-12-443<br />
Updated Information<br />
& Services<br />
Supplementary Material<br />
Subspecialty Collections<br />
Permissions & Licens<strong>in</strong>g<br />
Repr<strong>in</strong>ts<br />
<strong>in</strong>clud<strong>in</strong>g high-resolution figures, can be found at:<br />
http://peds<strong>in</strong>review.aappublications.org/cgi/content/full/27/12/44<br />
3<br />
Supplementary material can be found at:<br />
http://peds<strong>in</strong>review.aappublications.org/cgi/content/full/27/12/44<br />
3/DC1<br />
This article, along with others on similar topics, appears <strong>in</strong> the<br />
follow<strong>in</strong>g collection(s):<br />
Fetus and <strong>Newborn</strong> Infant<br />
http://peds<strong>in</strong>review.aappublications.org/cgi/collection/fetus_new<br />
born_<strong>in</strong>fant Gastro<strong>in</strong>test<strong>in</strong>al Disorders<br />
http://peds<strong>in</strong>review.aappublications.org/cgi/collection/gastro<strong>in</strong>te<br />
st<strong>in</strong>al_disorders<br />
Information about reproduc<strong>in</strong>g this article <strong>in</strong> parts (figures,<br />
tables) or <strong>in</strong> its entirety can be found onl<strong>in</strong>e at:<br />
http://peds<strong>in</strong>review.aappublications.org/misc/Permissions.shtml<br />
Information about order<strong>in</strong>g repr<strong>in</strong>ts can be found onl<strong>in</strong>e:<br />
http://peds<strong>in</strong>review.aappublications.org/misc/repr<strong>in</strong>ts.shtml<br />
Downloaded from http://peds<strong>in</strong>review.aappublications.org by J Michael Coleman on June 4, 2010