Neonatal Jaundice - Associates in Newborn Medicine
Neonatal Jaundice - Associates in Newborn Medicine
Neonatal Jaundice - Associates in Newborn Medicine
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
neonatology<br />
neonatal jaundice<br />
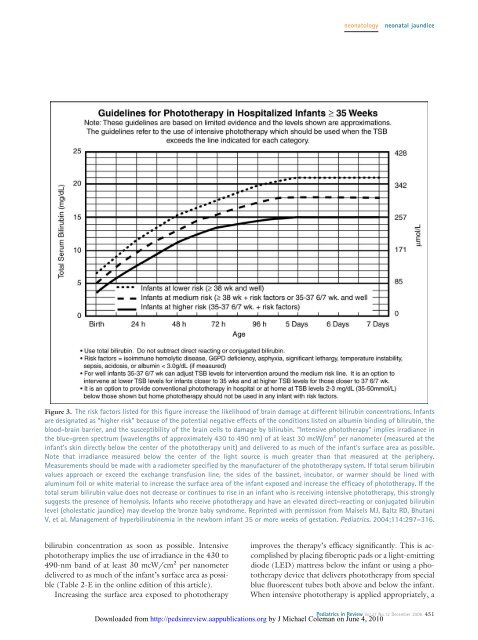
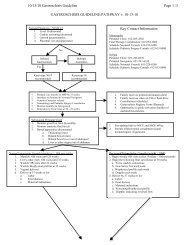
Figure 3. The risk factors listed for this figure <strong>in</strong>crease the likelihood of bra<strong>in</strong> damage at different bilirub<strong>in</strong> concentrations. Infants<br />
are designated as “higher risk” because of the potential negative effects of the conditions listed on album<strong>in</strong> b<strong>in</strong>d<strong>in</strong>g of bilirub<strong>in</strong>, the<br />
blood-bra<strong>in</strong> barrier, and the susceptibility of the bra<strong>in</strong> cells to damage by bilirub<strong>in</strong>. “Intensive phototherapy” implies irradiance <strong>in</strong><br />
the blue-green spectrum (wavelengths of approximately 430 to 490 nm) of at least 30 mcW/cm 2 per nanometer (measured at the<br />
<strong>in</strong>fant’s sk<strong>in</strong> directly below the center of the phototherapy unit) and delivered to as much of the <strong>in</strong>fant’s surface area as possible.<br />
Note that irradiance measured below the center of the light source is much greater than that measured at the periphery.<br />
Measurements should be made with a radiometer specified by the manufacturer of the phototherapy system. If total serum bilirub<strong>in</strong><br />
values approach or exceed the exchange transfusion l<strong>in</strong>e, the sides of the bass<strong>in</strong>et, <strong>in</strong>cubator, or warmer should be l<strong>in</strong>ed with<br />
alum<strong>in</strong>um foil or white material to <strong>in</strong>crease the surface area of the <strong>in</strong>fant exposed and <strong>in</strong>crease the efficacy of phototherapy. If the<br />
total serum bilirub<strong>in</strong> value does not decrease or cont<strong>in</strong>ues to rise <strong>in</strong> an <strong>in</strong>fant who is receiv<strong>in</strong>g <strong>in</strong>tensive phototherapy, this strongly<br />
suggests the presence of hemolysis. Infants who receive phototherapy and have an elevated direct-react<strong>in</strong>g or conjugated bilirub<strong>in</strong><br />
level (cholestatic jaundice) may develop the bronze baby syndrome. Repr<strong>in</strong>ted with permission from Maisels MJ, Baltz RD, Bhutani<br />
V, et al. Management of hyperbilirub<strong>in</strong>emia <strong>in</strong> the newborn <strong>in</strong>fant 35 or more weeks of gestation. Pediatrics. 2004;114:297–316.<br />
bilirub<strong>in</strong> concentration as soon as possible. Intensive<br />
phototherapy implies the use of irradiance <strong>in</strong> the 430 to<br />
490-nm band of at least 30 mcW/cm 2 per nanometer<br />
delivered to as much of the <strong>in</strong>fant’s surface area as possible<br />
(Table 2-E <strong>in</strong> the onl<strong>in</strong>e edition of this article).<br />
Increas<strong>in</strong>g the surface area exposed to phototherapy<br />
improves the therapy’s efficacy significantly. This is accomplished<br />
by plac<strong>in</strong>g fiberoptic pads or a light-emitt<strong>in</strong>g<br />
diode (LED) mattress below the <strong>in</strong>fant or us<strong>in</strong>g a phototherapy<br />
device that delivers phototherapy from special<br />
blue fluorescent tubes both above and below the <strong>in</strong>fant.<br />
When <strong>in</strong>tensive phototherapy is applied appropriately, a<br />
Pediatrics <strong>in</strong> Review Vol.27 No.12 December 2006 451<br />
Downloaded from http://peds<strong>in</strong>review.aappublications.org by J Michael Coleman on June 4, 2010