Neonatal Jaundice - Associates in Newborn Medicine
Neonatal Jaundice - Associates in Newborn Medicine
Neonatal Jaundice - Associates in Newborn Medicine
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
neonatology<br />
neonatal jaundice<br />
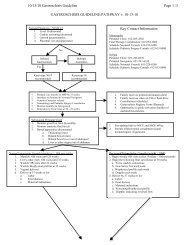
Table 8. Laboratory Tests for the <strong>Jaundice</strong>d Infant<br />
When there is a f<strong>in</strong>d<strong>in</strong>g of:<br />
<strong>Jaundice</strong> <strong>in</strong> first 24 h<br />
<strong>Jaundice</strong> that appears excessive for the <strong>in</strong>fant’s age<br />
An <strong>in</strong>fant receiv<strong>in</strong>g phototherapy or hav<strong>in</strong>g a TSB that is<br />
above the 75th percentile or ris<strong>in</strong>g rapidly (ie, cross<strong>in</strong>g<br />
percentiles) and unexpla<strong>in</strong>ed by history or f<strong>in</strong>d<strong>in</strong>gs on<br />
physical exam<strong>in</strong>ation<br />
A TSB approach<strong>in</strong>g exchange level or not respond<strong>in</strong>g to<br />
phototherapy<br />
An elevated direct (or conjugated) bilirub<strong>in</strong> level<br />
<strong>Jaundice</strong> present at or beyond age 3 wk or the <strong>in</strong>fant<br />
is sick<br />
Obta<strong>in</strong>:<br />
Total serum bilirub<strong>in</strong> (TSB)<br />
TSB<br />
Blood type; also, perform a Coombs test, if not obta<strong>in</strong>ed with<br />
cord blood<br />
Complete blood count, smear, and reticulocyte count<br />
Direct (or conjugated) bilirub<strong>in</strong><br />
(Repeat TSB <strong>in</strong> 4 to 24 hours, depend<strong>in</strong>g on <strong>in</strong>fant’s age and<br />
TSB level)<br />
Consider the possibility of glucose-6-phosphate<br />
dehydrogenase (G-6PD) deficiency, particularly <strong>in</strong> African-<br />
American <strong>in</strong>fants<br />
Reticulocyte count, G-6PD test, album<strong>in</strong><br />
Ur<strong>in</strong>alysis and ur<strong>in</strong>e culture; evaluate for sepsis if <strong>in</strong>dicated<br />
by history and physical exam<strong>in</strong>ation<br />
Total and direct bilirub<strong>in</strong> concentration; if direct bilirub<strong>in</strong> is<br />
elevated, evaluate for causes of cholestasis<br />
(Also check results of newborn thyroid and galactosemia<br />
screen and evaluate <strong>in</strong>fant for signs or symptoms of<br />
hypothyroidism)<br />
Repr<strong>in</strong>ted with permission from Maisels MJ. <strong>Jaundice</strong> <strong>in</strong> a newborn. How to head off an urgent situation. Contemp Pediatr. 2005;22:41–54. Adapted with<br />
permission from Pediatrics. 2004;14:297–316.<br />
other risk factors) always should be one above which a<br />
TSB value always will be obta<strong>in</strong>ed. In our nursery, we<br />
rout<strong>in</strong>ely evaluate <strong>in</strong>fants via a TcB measurement and<br />
obta<strong>in</strong> a TSB whenever the TcB is above the 75th percentile<br />
(Fig. 2) (or the 95th percentile <strong>in</strong> Fig. 1-E).<br />
Treatment<br />
Hyperbilirub<strong>in</strong>emia can be treated via: 1) exchange<br />
transfusion to remove bilirub<strong>in</strong> mechanically; 2) phototherapy<br />
to convert bilirub<strong>in</strong> to products that can bypass<br />
the liver’s conjugat<strong>in</strong>g system and be excreted <strong>in</strong> the bile<br />
or <strong>in</strong> the ur<strong>in</strong>e without further metabolism; and 3) pharmacologic<br />
agents to <strong>in</strong>terfere with heme degradation and<br />
bilirub<strong>in</strong> production, accelerate the normal metabolic<br />
pathways for bilirub<strong>in</strong> appearance, or <strong>in</strong>hibit the enterohepatic<br />
circulation of bilirub<strong>in</strong>. Guidel<strong>in</strong>es for the use of<br />
phototherapy and exchange transfusion <strong>in</strong> term and<br />
near-term <strong>in</strong>fants are provided <strong>in</strong> Figs. 3 and 4 and Table<br />
9.<br />
Phototherapy<br />
Phototherapy works by <strong>in</strong>fus<strong>in</strong>g discrete photons of energy<br />
similar to the molecules of a drug. These photons<br />
are absorbed by bilirub<strong>in</strong> molecules <strong>in</strong> the sk<strong>in</strong> and<br />
subcutaneous tissue, just as drug molecules b<strong>in</strong>d to a<br />
receptor. The bilirub<strong>in</strong> then undergoes photochemical<br />
reactions to form excretable isomers and breakdown<br />
products that can bypass the liver’s conjugat<strong>in</strong>g system<br />
and be excreted without further metabolism. Some<br />
photo products also are excreted <strong>in</strong> the ur<strong>in</strong>e.<br />
Phototherapy displays a clear dose-response effect,<br />
and a number of variables <strong>in</strong>fluence how light works to<br />
lower the TSB level. (In the onl<strong>in</strong>e edition of this article,<br />
Table 1-E shows the radiometric units used to measure<br />
the dose of phototherapy and Tables 2-E and 3-E show<br />
the factors that affect the dose and efficacy of phototherapy,<br />
<strong>in</strong>clud<strong>in</strong>g type of light source, the <strong>in</strong>fant’s distance<br />
from the light, and the surface area exposed.) Because of<br />
the optical properties of bilirub<strong>in</strong> and sk<strong>in</strong>, the most<br />
effective lights are those that have wavelengths predom<strong>in</strong>ately<br />
<strong>in</strong> the blue-green spectrum (425 to 490 nm). At<br />
these wavelengths, light penetrates the sk<strong>in</strong> well and is<br />
absorbed maximally by bilirub<strong>in</strong>.<br />
Us<strong>in</strong>g Phototherapy Effectively<br />
Phototherapy was used <strong>in</strong>itially <strong>in</strong> low-birthweight and<br />
term <strong>in</strong>fants primarily to prevent slowly ris<strong>in</strong>g bilirub<strong>in</strong><br />
concentrations from reach<strong>in</strong>g levels that might require<br />
exchange transfusion. Today, phototherapy often is used<br />
<strong>in</strong> term and near-term <strong>in</strong>fants who have left the hospital<br />
and are readmitted on days 4 to 7 for treatment of TSB<br />
concentrations of 20 mg/dL (342 mcmol/L) or more.<br />
Such <strong>in</strong>fants require a full therapeutic dose of phototherapy<br />
(now termed <strong>in</strong>tensive phototherapy) to reduce the<br />
450 Pediatrics <strong>in</strong> Review Vol.27 No.12 December 2006<br />
Downloaded from http://peds<strong>in</strong>review.aappublications.org by J Michael Coleman on June 4, 2010