How to Order and Interpret Radiology Studies
How to Order and Interpret Radiology Studies
How to Order and Interpret Radiology Studies
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
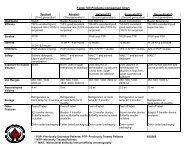
<strong>How</strong> <strong>to</strong> <strong>Order</strong> <strong>and</strong> <strong>Interpret</strong> <strong>Radiology</strong> <strong>Studies</strong><br />
Thomas <strong>How</strong>ard, MD<br />
327
Musculoskeletal Imaging in Sports Medicine<br />
Thomas <strong>How</strong>ard, MD, FACSM<br />
Garry W. K. Ho, MD<br />
Objectives<br />
1. Review the<br />
musculoskeletal<br />
imaging modalities<br />
available<br />
2. Discuss radiographic<br />
evaluation of specific<br />
musculoskeletal<br />
injuries<br />
Plain Film X-Ray X<br />
Radiography<br />
Ionizing-radiation x-ray x<br />
emitter<br />
Detec<strong>to</strong>r<br />
– Pho<strong>to</strong>graphic plate<br />
– Pho<strong>to</strong>stimulable phosphor<br />
– Others<br />
Radio-opacity opacity / radio-lucency<br />
328
Plain Film X-Ray X<br />
Radiography<br />
Advantages<br />
– Inexpensive<br />
– Readily available<br />
– Excellent spatial resolution<br />
– “Real-time” availability as<br />
fluoroscopy<br />
Limitations<br />
– Two-dimensional<br />
Need > two orthogonal views<br />
– Relatively poor soft tissue<br />
contrast resolution<br />
Useful for radio-opaque<br />
opaque<br />
foreign bodies<br />
Useful if emphysema<br />
or free air present<br />
– Ionizing radiation exposure<br />
Plain Film X-Ray X<br />
Radiography<br />
– Contraindications<br />
Pregnancy<br />
– More of concern for<br />
L-spine & pelvis XR<br />
– Minimal radiation<br />
exposure <strong>to</strong> fetus<br />
with shielding when<br />
imaging other areas<br />
Computed Tomography<br />
CT uses an array of x-raysx<br />
X-ray beams directed at several<br />
different angles<br />
Processed by computer <strong>to</strong><br />
produce cross sectional images<br />
Findings are described as<br />
radio-opaque opaque or radio-lucent<br />
329
Computed Tomography<br />
Images reconstructed - 2D or 3D<br />
Kinematic CT - imaging of joint motion<br />
Computed Tomography<br />
Advantages<br />
– High contrast resolution of images<br />
– Excellent images of bones <strong>and</strong> lungs<br />
IV contrast infrequently needed for<br />
orthopedic trauma<br />
– Wide availability<br />
– Faster than MRI<br />
Computed Tomography<br />
Limitations<br />
– Can produce artifacts (motion, metal)<br />
– Less soft-tissue tissue contrast than MRI<br />
– Exposure <strong>to</strong> ionizing<br />
radiation<br />
Radiation dose much higher<br />
than for conventional<br />
radiography<br />
– Higher cost than<br />
conventional x-rayx<br />
330
Computed Tomography<br />
Contraindications<br />
– Pregnant women should not have CT<br />
scans<br />
Except in life-threatening<br />
emergencies<br />
Can be scanned with<br />
shielding depending<br />
on body part (minimal<br />
radiation exposure <strong>to</strong><br />
fetus if ankle or knee<br />
is scanned)<br />
– Scanner weight-limits for obese patients<br />
Bone Scan (Scintigraphy(<br />
Scintigraphy)<br />
Biologically active<br />
drugs are labeled<br />
with radioiso<strong>to</strong>pes<br />
Radioiso<strong>to</strong>pe<br />
administered <br />
Giving off gamma<br />
rays<br />
Detected by<br />
gamma camera<br />
Processed by<br />
computer<br />
Bone Scan (Scintigraphy(<br />
Scintigraphy)<br />
Forms a functional image<br />
of soft tissues <strong>and</strong> bone<br />
Two main types:<br />
– Planar (“traditional(<br />
bone scan”)<br />
Three phase bone scan<br />
– SPECT – cross-<br />
sectional <strong>and</strong><br />
reconstructed bone<br />
scans<br />
331
Bone Scan (Scintigraphy(<br />
Scintigraphy)<br />
Triple phase bone scan:<br />
– Flow (perfusion) study<br />
60 seconds after injection<br />
Blood flow<br />
– Blood Pool<br />
Increased circulation, blood<br />
vessel dilation<br />
– Delayed<br />
2 -33 hrs after injection<br />
Bone uptake<br />
– Clearance from extraosseous<br />
tissues<br />
Scintigraphy - SPECT Imaging<br />
(Single Pho<strong>to</strong>n Emission Computed Tomography)<br />
Three-dimensional imaging technique used in<br />
conjunction with radioiso<strong>to</strong>pe injection<br />
Enhanced tissue contrast<br />
Improved sensitivity <strong>and</strong> specificity of lesion<br />
detection & localization<br />
Bone Scan (Scintigraphy(<br />
Scintigraphy)<br />
Advantages<br />
– Images metabolic activity<br />
of osteoblasts<br />
Very sensitive for acute<br />
fractures & tumors<br />
Old, less metabolically<br />
active fractures & tumors<br />
may not show up<br />
– Less radiation exposure<br />
than chest x-ray x<br />
& CT<br />
332
Bone Scan (Scintigraphy(<br />
Scintigraphy)<br />
Limitations<br />
– Lacks significant detail<br />
– Poor spatial resolution<br />
– Poor specificity<br />
– Displays activity of osteoblasts<br />
Old fractures (eg(<br />
eg. . pars defects) may not show up<br />
Certain tumors with little osteoblastic activity (eg(<br />
eg.<br />
multiple myeloma <strong>and</strong> lytic mets) ) not reliably seen<br />
Contraindications<br />
– Exposes patient <strong>to</strong> ionizing radiation<br />
– Children & pregnant women should be carefully<br />
shielded<br />
Magnetic Resonance<br />
Imaging (MRI)<br />
Majority of clinical MRI utilizes the magnetic<br />
moment of hydrogen nuclei (pro<strong>to</strong>ns)<br />
Magnetic Resonance Imaging<br />
Magnetic field pro<strong>to</strong>ns excited alignment<br />
Pro<strong>to</strong>ns snap back in<strong>to</strong> original alignment <br />
detectable rotating magnetic field<br />
Pro<strong>to</strong>ns in different tissues realign at different<br />
speeds detected as differing signal intensities<br />
333
Magnetic Resonance Imaging<br />
MRI studies – many different type of studies,<br />
sequences, <strong>and</strong> pro<strong>to</strong>cols<br />
Basically two types:<br />
– T1<br />
Ideal for studying ana<strong>to</strong>my<br />
Fat is white<br />
– T2<br />
More valuable in studying<br />
pathology<br />
Water is white (H2O)<br />
Contrast studies<br />
– Highlight certain structures<br />
& abnormalities<br />
Magnetic Resonance Imaging<br />
Advantages<br />
– Excellent contrast<br />
resolution<br />
Especially for<br />
soft tissue pathology<br />
– High sensitivity in<br />
bone marrow<br />
diseases<br />
– Electromagnetic radiation instead of<br />
ionizing radiation<br />
Magnetic Resonance Imaging<br />
Limitations<br />
– Most sensitive <strong>to</strong> artifact from motion & metal<br />
– Claustrophobia<br />
– Some findings are subtle<br />
Dependent upon<br />
interpretation<br />
Eg. labral tears<br />
– High cost; lower availability<br />
334
Magnetic Resonance Imaging<br />
Contraindications<br />
– Pacemakers<br />
(under investigation)<br />
Pracically, , an absolute<br />
contraindication<br />
– Prosthetic cardiac valves<br />
safe after 6 weeks<br />
– Stents & grafts<br />
Non-ferromagnetic are safe<br />
Ferromagnetic are safe after 6 weeks<br />
– Due <strong>to</strong> epithelialization<br />
Abdominal aortic aneurysm stents check with<br />
radiologist<br />
– Pumps – check with radiologist<br />
– Other devices may malfunction or be contraindicated<br />
Magnetic Resonance Imaging<br />
Contraindications (continued)<br />
– Metal objects<br />
Can migrate, heat up, <strong>to</strong>rque<br />
Foreign bodies, body piercings, jewelry<br />
Situational clearance<br />
– Fragment in brain or<br />
eye contraindicated<br />
– Bullet in femur or<br />
muscle likely OK<br />
– Tat<strong>to</strong>os & cosmetics can<br />
heat up<br />
Metallic dyes<br />
Magnetic Resonance Imaging<br />
Contraindications (continued)<br />
– Obese patients<br />
Scanner table weight limits<br />
Gantry opening might be<br />
<strong>to</strong>o small<br />
– Pregnancy<br />
Animal studies conflicting<br />
Avoid during 1 st trimester<br />
No gadolinium unless<br />
absolutely necessary<br />
335
Ultrasonography<br />
Uses high-frequency sound<br />
waves <strong>to</strong> produce images<br />
Can define masses, fluid, &<br />
localize foreign bodies<br />
Findings are described as<br />
hyperechoic, hypoechoic, , or<br />
anisotropy<br />
Allows for dynamic<br />
evaluation<br />
Newer systems are more<br />
compact with higher<br />
resolution<br />
Ultrasonography - Tendons<br />
Bright structure with longitudinally oriented bundles<br />
Ultrasonography - Tendons<br />
Blurring, thickening, loss of normal architecture<br />
336
Ultrasonography - Muscles<br />
Gastrocnemius<br />
with hema<strong>to</strong>ma<br />
Complete disruption<br />
of fibers on dynamic<br />
evaluation of rectus<br />
femoris<br />
Low Back Pain<br />
Who do you image<br />
Ask yourself:<br />
– Do you have a<br />
pathoana<strong>to</strong>mic<br />
diagnosis<br />
– Do you need <strong>to</strong> rule out<br />
tumor, infection, or<br />
fracture<br />
– Will imaging change<br />
your treatment<br />
“Red Flags” for imaging:<br />
– major trauma<br />
– age > 50<br />
– unrelenting pain at<br />
rest or night pain<br />
– fever, chills, sweats<br />
– unexplained weight loss<br />
– his<strong>to</strong>ry of cancer<br />
Low Back Pain<br />
– incontinence of bowel or bladder<br />
– progressive weakness<br />
337
Low Back Pain<br />
Conventional x-rayx<br />
(plain films)<br />
– AP<br />
– Lateral<br />
– Lumbosacral (LS) spot view<br />
L5 centered view<br />
Minimizes potential for over-read<br />
read<br />
of disk space narrowing<br />
– Disk space narrowing,<br />
osteophytes, , fracture, tumor,<br />
or spondylolisthesis<br />
Low Back Pain<br />
Conventional x-rayx<br />
– Oblique views<br />
Best if concern for<br />
pars interarticularis<br />
fracture<br />
(spondylolysis)<br />
– Pars interarticularis<br />
narrow portion of<br />
bone between<br />
superior & inferior<br />
articular facets<br />
Low Back Pain<br />
Bone Scan / Scintigraphy<br />
– Suspected spondylolysis not seen on plain<br />
film x-raysx<br />
– Determine old versus new spondylolysis<br />
338
Low Back Pain<br />
Lumbar Spine MRI<br />
– Excellent for<br />
Disc disease & herniation<br />
Cord compression<br />
– Also will demonstrate:<br />
Spinal cord anomalies<br />
Tumors<br />
Discitis<br />
Vertebral osteomyelitis<br />
Low Back Pain<br />
CT Scan<br />
– Excellent bone study for vertebral fracture<br />
Usually done in conjunction with MRI<br />
– Useful for spondylolysis<br />
Chronic non-union / fibrous union<br />
Chronic Low Back Pain<br />
Consider guided injections<br />
– Fluoroscopic SI, facet injections,<br />
epidural steroids<br />
339
Cervical Spine Injuries<br />
Initial C-spine C<br />
trauma series<br />
– Cross-table lateral<br />
– Anteroposterior (AP)<br />
– Open-mouth<br />
odon<strong>to</strong>id<br />
Cervical Spine Injuries<br />
Lateral view<br />
All vertebrae on the<br />
lateral<br />
Presence of lordosis<br />
Vertebral alignment<br />
– Anterior vertebral line<br />
– Posterior vertebral line<br />
– Spinolaminal line<br />
– Posterior spinous line<br />
Soft tissue examination<br />
Cervical Spine Injuries<br />
Anterior soft tissue<br />
– “66 at 2 <strong>and</strong> 2 at 6” 6 rule<br />
< 6 mm at C2<br />
< 2 cm (20 mm) at C6<br />
– C1-C3 C3 < 5-7mm5<br />
– C4-C7 C7 = 14-22 mm<br />
– Increased soft tissue<br />
space suggests occult<br />
fracture<br />
340
Cervical Spine Injuries<br />
AP view<br />
– Spinous processes<br />
should line up<br />
midline<br />
– Vertebral bodies &<br />
articular pillars also<br />
line up<br />
– Vertebral body<br />
height<br />
Cervical Spine Injuries<br />
Odon<strong>to</strong>id view<br />
– C1-2 2 articulation<br />
– Alignment<br />
Gaps between C1<br />
lateral masses &<br />
C2 dens (odon<strong>to</strong>id(<br />
odon<strong>to</strong>id)<br />
Lateral margins of<br />
C2 articulating<br />
facet & C1 lateral<br />
masses<br />
– Fractures<br />
Dens<br />
Jefferson fracture – ring of C1 broken<br />
from axial loading<br />
Cervical Spine Injuries<br />
Dynamic flexion-extension<br />
extension<br />
– Active voluntary test<br />
– Undetected<br />
ligament<br />
disruption or<br />
instability<br />
– Requires alert,<br />
cooperative<br />
patient<br />
s<strong>to</strong>pping for<br />
pain or<br />
paresthesias<br />
341
Cervical Spine Injuries<br />
Widening of the predental space from rupture of<br />
the transverse ligament<br />
Cervical Spine Injuries<br />
CT scan<br />
– Suspect bony injury<br />
despite normal plain<br />
films<br />
– Suspect instability on<br />
plain films<br />
– Better visualize<br />
fracture, evaluate for<br />
displacement<br />
MRI<br />
– Evaluate spinal canal,<br />
nerve roots, <strong>and</strong>/or<br />
soft tissue injury<br />
Shoulder Injury<br />
“St<strong>and</strong>ard” series<br />
– AP in external rotation<br />
& internal rotation<br />
– Axillary lateral view<br />
342
Shoulder Injury<br />
Scapular Y view<br />
– AKA: supraspinatus outlet view,<br />
scapular lateral view<br />
– Dislocation & angulation of<br />
proximal humerus fractures<br />
– Acromial morphology<br />
– Good lateral view when patient<br />
cannot <strong>to</strong>lerate an axillary view<br />
Shoulder Injury<br />
MRI <strong>and</strong> MRI arthrography<br />
– Nonsurgical diagnostic test of choice for<br />
internal derangements <strong>and</strong> structural<br />
instability assessment<br />
– Soft tissue <strong>and</strong> bone lesions well demonstrated<br />
Shoulder Injury<br />
Ultrasound<br />
– Non-invasive<br />
– Allows for dynamic<br />
evaluation<br />
– Both opera<strong>to</strong>r &<br />
equipment<br />
dependent<br />
343
St<strong>and</strong>ard views<br />
– PA view:<br />
2 mm intercarpal<br />
joint space<br />
3 arcs<br />
– Lateral view:<br />
4 Cs<br />
Wrist Injury<br />
Wrist Injury<br />
Complex joints may<br />
require additional views<br />
Scaphoid fracture:<br />
– Scaphoid views<br />
– If initially negative<br />
Immobilize x 2 - 3 weeks<br />
Repeat plain films<br />
– If still negative <strong>and</strong><br />
symp<strong>to</strong>matic MRI<br />
Chronic Wrist Pain<br />
Hamate Fracture<br />
– CT scan<br />
Keinbock’s Disease<br />
– X-ray, bone scan, MRI<br />
Carpal Instability<br />
– X-ray angles,<br />
MR arthrogram<br />
TFCC Injury<br />
– MR arthrogram<br />
Occult Ganglion<br />
– MR arthrogram<br />
Complex Regional Pain<br />
Syndrome, Type I<br />
– Bone scan<br />
344
Plain film X-raysX<br />
Hip Pain/Injury<br />
– Good initial study<br />
– Arthritis<br />
– Late avascular necrosis<br />
– Initial evaluation for<br />
femoral neck stress<br />
fracture<br />
– Can miss grade 4<br />
cartilage damage<br />
Hip Pain/Injury<br />
MRI<br />
– At least 1.5 T magnet<br />
– Surface coil<br />
– Poor for for IA cartilaginous injuries<br />
– Good for evaluation of femoral neck<br />
stress fractures<br />
MR Arthrogram<br />
– Labral pathology<br />
Increased sensitivity, but also<br />
increased false positive<br />
– Gad sequences can obscure bone<br />
– Diagnostic anesthetic injection<br />
Bone Scan<br />
– Good study for stress fractures<br />
Ultrasound<br />
Hip Pain/Injury<br />
345
X-rays<br />
AP<br />
view<br />
Knee Injuries<br />
Lateral<br />
view<br />
Sunrise /<br />
Merchant view<br />
Tunnel /<br />
Notch view<br />
Advanced imaging<br />
Knee Injuries<br />
– CT scan – more detailed evaluation of bony injuries<br />
– MRI -- imaging modality of choice for soft tissue<br />
Exertional Leg Pain<br />
Shin splints (MTSS) vs. stress fracture<br />
Shin Splints<br />
– Clinical diagnosis<br />
– Plain films: look for stress fracture<br />
– Triple Phase Bone Scan<br />
346
• Stress fractures<br />
Exertional Leg Pain<br />
• Initial radiograph:<br />
normal in up <strong>to</strong> 70%<br />
• Fluffy, ill-defined<br />
sclerotic line<br />
perpendicular <strong>to</strong> major<br />
trabecular lines<br />
• Periosteal reaction<br />
Stress Fractures<br />
• Thin incomplete lucent line<br />
• May proceed <strong>to</strong> completion<br />
• Beware of the “DBL”<br />
• Bone scan helpful<br />
Imaging of Early Stress Fractures<br />
• MRI <strong>and</strong> bone scan near 100% sensitivity<br />
• MRI improved specificity<br />
347
Exertional Leg Pain<br />
Exertional Compartment<br />
Syndrome<br />
– Routine MRI & bone<br />
scan not helpful<br />
– Compartment pressure<br />
testing<br />
Popliteal Artery<br />
Entrapment<br />
– MRA<br />
– Angiography<br />
Acute Ankle Trauma<br />
When do you x-ray x<br />
– Ottawa Ankle Rules:<br />
Stiell IG, McKnight RD, Greenberg GH, McDowell I, Nair RC, Wells GA, et al. Implementation of the<br />
Ottawa ankle rules. JAMA 1994;271:827-32.<br />
Ankle Injuries<br />
Normal ankle<br />
(AP view)<br />
Normal ankle<br />
(Lateral view)<br />
Normal ankle<br />
(Mortise view)<br />
348
Don’t t forget the foot films!<br />
AP, lateral <strong>and</strong> oblique<br />
Contralateral foot films<br />
Weight-bearing views<br />
Lateral view<br />
– Metatarsal shafts &<br />
tarsal bones align<br />
AP <strong>and</strong> obliques<br />
– 2nd met medial<br />
border & middle<br />
cuneiform align<br />
Chronic Ankle Pain<br />
MRI<br />
– Imaging modality of choice for soft-tissue tissue <strong>and</strong><br />
osteochondral lesions<br />
CT<br />
– Ankle fractures & bony pathology<br />
Bone scan<br />
– Diffuse, non-specific pain<br />
– F/U CT if needed for further evaluation of stress<br />
fractures<br />
Conclusions<br />
Initial imaging of choice: plain radiography<br />
– Image before injection<br />
– Image all trauma<br />
CT: good for bone<br />
MRI: good for soft tissue<br />
– T1: ana<strong>to</strong>my; T2: pathology<br />
Scintigraphy: : good for metabolic activity<br />
Ultrasound: great potential<br />
– Opera<strong>to</strong>r / interpreter & technology dependent<br />
Imaging selection<br />
– Based on his<strong>to</strong>ry <strong>and</strong> physical<br />
– Know your specialists’ imaging preferences<br />
– Consult radiologist as needed<br />
349
Thank You<br />
350