Combat Stress Management.pdf - UNC Charlotte Army ROTC
Combat Stress Management.pdf - UNC Charlotte Army ROTC
Combat Stress Management.pdf - UNC Charlotte Army ROTC
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Personal Development Track<br />
Section<br />
3<br />
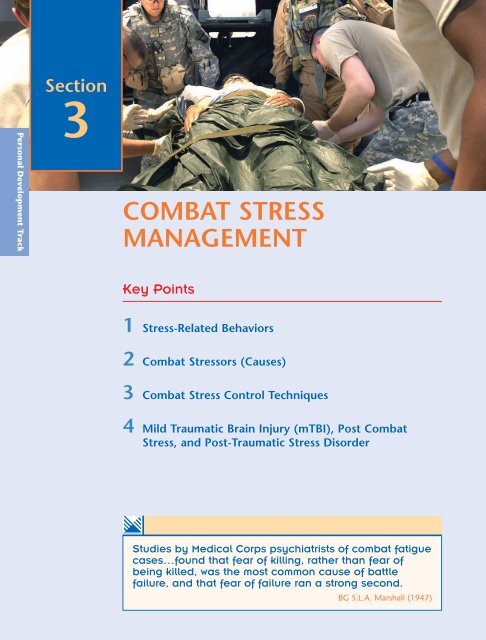
COMBAT STRESS<br />
MANAGEMENT<br />
Key Points<br />
1 <strong>Stress</strong>-Related Behaviors<br />
2 <strong>Combat</strong> <strong>Stress</strong>ors (Causes)<br />
3 <strong>Combat</strong> <strong>Stress</strong> Control Techniques<br />
4 Mild Traumatic Brain Injury (mTBI), Post <strong>Combat</strong><br />
<strong>Stress</strong>, and Post-Traumatic <strong>Stress</strong> Disorder<br />
e<br />
Studies by Medical Corps psychiatrists of combat fatigue<br />
cases…found that fear of killing, rather than fear of<br />
being killed, was the most common cause of battle<br />
failure, and that fear of failure ran a strong second.<br />
BG S.L.A. Marshall (1947)
<strong>Combat</strong> <strong>Stress</strong> <strong>Management</strong> ■ 45<br />
Introduction<br />
Battle fatigue is the approved <strong>Army</strong> term (AR 40-216) for combat-stress symptoms<br />
and reactions that:<br />
• Feel unpleasant<br />
• Interfere with mission performance<br />
• Are best treated with reassurance, rest, replenishment of physical needs, and<br />
activities that restore confidence.<br />
Battle fatigue can also be present in Soldiers who have been physically wounded or<br />
who have non-battle injuries or diseases caused by stressors in the combat area. It may<br />
be necessary to treat both the battle fatigue and the other problems. Battle fatigue<br />
may coexist with misconduct stress behaviors, which are inappropriate or illegal<br />
behaviors resulting from an increase in stress. Misconduct stress behaviors include<br />
refusing to obey orders, drug or alcohol abuse, fighting with allies, combat refusal,<br />
AWOL or desertion, malingering, mutilating enemy dead, torturing prisoners, killing<br />
noncombatants, looting, pillage, and rape. But battle fatigue itself, by definition, does<br />
not warrant legal or disciplinary action. Several US allies use other terms for battle<br />
fatigue, such as combat reaction, combat-stress reaction, or battle shock. As a Soldier<br />
and a leader it is your responsibility to identify and take action to reduce or remove<br />
stressors that can lead to battle fatigue. To do this you must be able to recognize<br />
stress-related behaviors.<br />
This chapter will focus on the effects of combat stress (i.e., the behavior of those<br />
with combat stress) rather than the causes and will discuss methods to manage it.<br />
Injured Veteran Uses Own Experience to Inspire Others With Traumatic Brain Injuries<br />
battle fatigue<br />
traumatic<br />
psychoneurotic reaction<br />
or an acute psychotic<br />
reaction occurring under<br />
conditions (such as<br />
wartime combat) that<br />
cause intense stress<br />
stress-related<br />
behaviors<br />
symptoms or behaviors<br />
signaling the presence or<br />
onset of physical or<br />
emotional stress<br />
Pfc. Chris Lynch, a former 82nd Airborne Division Soldier who has been living<br />
with traumatic brain injury for the past seven years is reaching out to recently<br />
wounded veterans of Iraq and Afghanistan to help them learn to live with the<br />
disease.<br />
Pfc. Chris Lynch was attending a French commando school in July 2000 when<br />
he fell 26 feet and landed directly on his head. He went into a coma for 45 days<br />
before arriving at Walter Reed <strong>Army</strong> Medical Center.<br />
Pfc. Lynch was later diagnosed with traumatic brain injury or TBI—an affliction<br />
that’s become a signature injury of the war on terror.<br />
Roadside bombs, mortars and other explosives are taking their toll on<br />
deployed troops’ brains as well as their bodies. Even with Kevlar helmets, there’s<br />
a critical organ this protective gear simply doesn’t adequately protect: the<br />
gelatin-like material that can shift violently inside the skull when confronted by<br />
explosions, sudden jolts or shock waves from blasts.<br />
”When they explode, your skull gets pounded against your Kevlar (helmet),“<br />
Pfc. Lynch said. ”Your brain gets tossed around like an egg in a bucket of water.“
46 ■ SECTION 3<br />
TBI symptoms run the gamut, from slower reaction times to severe emotional<br />
and cognitive problems.<br />
Pfc. Lynch remembers his own experience. When he awoke from his coma, he<br />
had a breathing tube, had lost about a third of his body weight and was<br />
paralyzed on his left side. Even more shocking, he was unable to speak, walk, eat<br />
or dress without assistance.<br />
After months of intensive therapy, both at Walter Reed and at the James A.<br />
Haley Veterans Administration Hospital in Tampa, Fla., Pfc. Lynch slowly relearned<br />
how to walk, talk and do other everyday tasks he once took for granted.<br />
”The 82nd gave me the mentality to drive on,“ he said. ”There are a lot of<br />
speed bumps in life. TBI is just a bigger one.“<br />
Now back at his hometown of Pace, Fla., and medically retired from the <strong>Army</strong>,<br />
Pfc. Lynch said he understands the trauma troops go through when they’re<br />
diagnosed with TBI. He said he hopes his own experience helps them recognize<br />
that there’s life after a TBI diagnosis and to inspire them to press on.<br />
”It’s definitely eye opening,“ Pfc. Lynch said of his own injury. ”But it makes<br />
you more empathetic and gives you a love for life.“<br />
Seven years after his injury, Pfc. Lynch lives in his parents’ home and continues<br />
to keep a ”drive on“ mentality as he rebuilds his life. He walks 5 to 10 miles a day<br />
along the beach in Pensacola, Fla., ran eight marathons last year, and attended<br />
the National Disabled Veterans Winter Sports Clinic in Snowmass, Colo., in April.<br />
Meanwhile, he just graduated from Pensacola Junior College, where he studied<br />
recreational technology, and plans to continue his studies so he can someday<br />
teach physical education to underprivileged and handicapped children.<br />
But as he looks to his future, Pfc. Lynch said his main focus is on helping other<br />
troops suffering from traumatic brain injuries. He travels extensively to increase<br />
awareness about TBI and launched a Web site that details his own recovery.<br />
”I’ve learned a lot about interpersonal communications and become a public<br />
speaker,“ he said. ”The bottom line is, I try to inspire other people.“<br />
Pfc. Lynch still goes through his own personal hard times. He gets frustrated<br />
when people who hear his still-distorted speech think he’s drunk.<br />
And he still misses his fellow 307th Engineer Battalion Soldiers and pines for<br />
the military career he had to leave behind.<br />
”I miss it,“ he said. ”I miss it every day.“<br />
<strong>Army</strong> News Service<br />
<strong>Stress</strong>-Related Behaviors<br />
You should always take preventive actions and address stress symptoms as they appear. If<br />
you ignore the early warning signs, the severity of stress reactions that lead to battle fatigue<br />
can increase. Following are examples of stress-related behaviors:
<strong>Combat</strong> <strong>Stress</strong> <strong>Management</strong> ■ 47<br />
Simple Fatigue. The simple fatigue or exhaustion form of battle fatigue is the most common.<br />
It involves tiredness, loss of initiative, indecisiveness, inattention, and—when extreme—<br />
general apathy. These cases may show some features of the other forms of stress-related<br />
behaviors, especially anxiety and pessimism, but not to the degree that Soldiers cannot rest<br />
and recover in their own unit (duty cases) or in a nonmedical support unit (rest cases).<br />
The tactical situation may call for them to rest in any suitable place that is practical.<br />
Anxiety. The anxious form of battle fatigue is naturally one of the most common, given<br />
the dangers of combat. Symptoms include verbal expressions of fear; marked startle<br />
responses to sights and sounds that are not true threats; overreaction to loud noises; tremors;<br />
sweating; rapid heartbeat; insomnia with terror dreams; and other symptoms of<br />
overexcitement. This form is often seen while Soldiers are close to the danger. Soldiers’<br />
stress may shift to simple fatigue or depressed forms as they evacuate toward the rear.<br />
Depression. The depressed form of battle fatigue is also common. It may resemble the slowed<br />
speech and movement of the simple fatigue form or the restlessness and startle responses<br />
of the anxious form. A Soldier suffering from the depressed form will also have serious<br />
feelings of self-doubt, self-blame, hopelessness, grief, and bereavement. The Soldier may<br />
be pessimistic about the chance for victory or survival. The self-blame and guilt may result<br />
from a Soldier’s perceived or actual failures or mistakes in combat. It may be related to<br />
home-front issues. Or it may be survivor guilt—a survivor’s irrational feeling that he should<br />
have died with members of his unit or in a buddy’s place.<br />
Memory Loss. The memory-loss form of battle fatigue is less common, especially in its<br />
extreme versions. Mild forms include an inability to remember recent orders and<br />
instructions. More serious examples are inability to perform well-learned skills or discrete<br />
loss of memory about an especially traumatic event or period of time. Extreme forms<br />
include disorientation and regression to a pre-combat (for example, childhood) state. Total<br />
amnesia, in which the Soldier leaves the threatening situation altogether, forgets his or<br />
her own past, and is found wandering somewhere else (having taken on another superficial<br />
identity), can also occur. Medical experts who treat Soldiers for stress-related behavior<br />
must also rule out potential physical causes of amnesia such as concussion or substance<br />
misuse (of alcohol, for example).<br />
Physical Function Disturbance. This form of battle fatigue involves disturbances of physical<br />
functions such as disruptions of motor, sensory, and speech functions. The Soldier has<br />
no physical injuries or has injuries that by themselves do not explain the symptoms.<br />
Psychologists and grief<br />
counselors recognize<br />
that people often go<br />
through five stages of<br />
grief when facing a<br />
terminal illness. The<br />
stages can also be<br />
applied to combatrelated<br />
stress situations:<br />
Denial – This can’t be<br />
happening.<br />
Anger – Why me? This<br />
isn’t fair!<br />
Bargaining – Just let<br />
me live to see my<br />
children graduate.<br />
Depression – I’m so<br />
sad. Why bother with<br />
anything?<br />
Acceptance – It’s going<br />
to be OK.<br />
• Motor disturbance includes:<br />
Weakness or paralysis of hands, limbs, or body<br />
Sustained contractions of muscles (for example, being unable to straighten up or<br />
to straighten out the elbow)<br />
Gross tremors; pseudo-convulsive seizures (sometimes with loss of consciousness).<br />
• Visual symptoms may include:<br />
Blurred or double vision<br />
Tunnel vision<br />
Total blindness.<br />
• Hearing-related symptoms may involve:<br />
Ringing (or other noises) in the ears<br />
Deafness<br />
Dizziness.
48 ■ SECTION 3<br />
• Tactile (skin) sensory changes include:<br />
Loss of sensations (anesthesia)<br />
Abnormal sensations, such as “pins and needles” (paresthesia).<br />
• Speech disturbance may involve:<br />
Stuttering<br />
Hoarseness<br />
Muteness.<br />
A Soldier’s physical symptoms often begin as normal but temporary coordination problems,<br />
speech difficulties, or sensory disruption. Physical events, such as explosions, mild<br />
concussion, or simple fatigue can trigger these symptoms. The symptoms are magnified<br />
when the Soldier cannot express emotions because of social pressure or heroic self-image.<br />
Such symptoms may appear more often, therefore, in the “elite” units or groups that show<br />
few other cases of battle fatigue—such as the airborne and Rangers in World War II.<br />
In some cases, the Soldier’s physical “disability” may have a clear symbolic relationship<br />
to the specific emotional trauma or conflict of motivation that the Soldier has experienced.<br />
The disability may make the Soldier unable to do his or her job and so remove the danger,<br />
such as classic “trigger-finger palsy.” Reducing the Soldier’s anxiety and eliminating his or<br />
her internal conflict over combat duties may reinforce the symptoms. The Soldier’s obtaining<br />
the relative luxury of rear-area food, hygiene, and sleep may also reinforce the symptoms.<br />
Not all cases fit that pattern, however. Some Soldiers with significant loss of function<br />
from battle fatigue have continued to perform their missions under great danger.<br />
Psychosomatic Forms. The psychosomatic forms of battle fatigue commonly appear as<br />
physical (rather than emotional) symptoms due to stress. These include:<br />
According to some World<br />
War II battalion<br />
surgeons, the<br />
psychosomatic form of<br />
battle fatigue was the<br />
most common form they<br />
saw at battalion level.<br />
This type of case may<br />
have accounted for a<br />
large percentage of all<br />
patients seen at<br />
battalion aid stations<br />
(BASs) during times of<br />
heavy fighting.<br />
Leaders, medics, and<br />
combat stress control<br />
personnel must never<br />
refer to battle-fatigue<br />
casualties as “psychiatric<br />
casualties.”<br />
• Cardiorespiratory:<br />
Rapid or irregular heartbeat<br />
Shortness of breath<br />
Light-headedness<br />
Tingling and cramping of toes, fingers, and lips.<br />
• Gastrointestinal:<br />
Stomach pain<br />
Indigestion<br />
Nausea/vomiting<br />
Diarrhea.<br />
• Musculoskeletal:<br />
Back or joint pain<br />
Excessive pain and disability from minor or healed wounds<br />
Headache.<br />
Disruptive Forms. Disruptive forms of battle fatigue include disorganized, bizarre, impulsive<br />
or violent behavior; total withdrawal; or persistent hallucinations. These are uncommon<br />
forms, but they do occur. Battle-fatigue symptoms are a way for Soldiers to communicate<br />
without words to comrades and leaders that they have had all they can stand at the moment.<br />
It is important for leaders to create positive expectations and to eliminate the belief that<br />
Soldiers suffering from battle fatigue usually do crazy, senseless, or violent things. Leaders,<br />
medics, and combat-stress control personnel must never refer to battle-fatigue casualties<br />
as “psychiatric casualties.”
<strong>Combat</strong> <strong>Stress</strong> <strong>Management</strong> ■ 49<br />
<strong>Combat</strong> <strong>Stress</strong>ors (Causes)<br />
Two common themes interact in varying combinations in most battle-fatigue casualties—<br />
loss of confidence and internal conflict of motives.<br />
Loss of Confidence<br />
Battle-fatigued Soldiers have often lost confidence in:<br />
• Themselves—their own strength, alertness, and abilities, or the adequacy of their<br />
training<br />
• Equipment—their weapons and the supporting arms<br />
• Buddies—other members of the small unit, or in the reliability of supporting units<br />
• Leaders, to include:<br />
o The skill and competence of the small-unit leader or the senior leadership<br />
o<br />
o<br />
The leaders’ concern for the Soldiers’ well-being and survival<br />
The leaders’ candor (honesty) or courage.<br />
combat stressors<br />
contributing factors<br />
(sudden exposure,<br />
cumulative exposure,<br />
physical stressors and<br />
stress symptoms, and<br />
home-front and other<br />
existing problems) that<br />
cause battle fatigue<br />
These doubts, plus the Soldiers’ estimate of the threat situation, raise questions in Soldiers’<br />
minds about their chances of surviving and/or succeeding with the mission. Loss of faith<br />
in whether the “cause” is worth suffering and dying for also plays a role. It has been said<br />
that Soldiers join the military services for patriotism, but they fight and die for their buddies<br />
and trusted leaders. Soldiers do not want their comrades or themselves to die for an unjust<br />
cause or for others’ mistakes. A Soldier’s loss of faith in such cases may even spread to a<br />
painful loss of belief in the goodness of life and other spiritual and religious values.
50 ■ SECTION 3<br />
Internal Conflict of Motives<br />
<strong>Combat</strong>, by its nature, creates conflicts among motives within an individual. The desire<br />
for survival and comfort conflicts with the fears of failure or disgrace and the Soldier’s<br />
loyalty to buddies.<br />
Four Major Contributing Factors<br />
Four major contributing factors cause battle fatigue. When you mix in the two themes<br />
just covered (loss of confidence and internal conflict of motives), you understand better<br />
why battle fatigue happens. The four major contributing factors are:<br />
1. Sudden exposure<br />
2. Cumulative exposure<br />
3. Physical stressors and stress symptoms<br />
4. Home-front and other personal problems.<br />
Any one factor may suffice to produce battle fatigue if it is intense enough. Usually two,<br />
three, or all four factors can collectively produce battle fatigue.<br />
In the transitional, fluid<br />
nonlinear characteristics<br />
of the contemporary<br />
operating environment<br />
(COE), “rear areas” can<br />
no longer be considered<br />
“safe” as in traditional<br />
wars and conflicts of the<br />
past.<br />
Sudden Exposure. This first factor is the sudden exposure or transition to the intense<br />
fear, shocking stimuli, and life-and-death consequences of battle. This occurs most<br />
commonly when Soldiers are committed to battle the first time, but it can happen even to<br />
veteran Soldiers when they come under sudden, intense attack. Soldiers in traditionally<br />
“safe” rear areas may be overwhelmed by the horrible sights, sounds, and consequences<br />
of war without themselves being under fire. This is an occupational hazard for rearward<br />
command and support personnel, including medical staff.<br />
Cumulative Exposure. This second factor is the cumulative exposure to dangers,<br />
responsibilities, and horrible consequences. Such exposure can cause repeated grief and guilt<br />
over the loss of fellow Soldiers. It can also give a Soldier the sense that his or her own luck,<br />
skill, and courage have run out. The rate of accumulation depends on the rate of losses<br />
and the number of “close calls” with disaster and death in the unit, including the Soldier’s<br />
own close calls and injuries. Giving Soldiers periods of rest, recreation, and retraining in<br />
which they can form new supportive, cohesive bonds may temporarily reverse the<br />
accumulation but not stop it completely.<br />
Physical <strong>Stress</strong>ors and <strong>Stress</strong> Symptoms. This third factor includes the physical stressors and<br />
stress symptoms that reduce a Soldier’s ability to cope. Loss of sleep and dehydration are<br />
especially strong contributors to battle fatigue. Also important are physical overload,<br />
cold, heat, dampness, noise, vibration, blast, fumes, lack of oxygen, chronic discomfort,<br />
poor hygiene, disrupted nutrition, low-grade fevers, infections, and other environmental<br />
illnesses. Preventive medicine can help ward off such stressors. In moderate amounts, such<br />
physical stressors contribute to battle fatigue, but rest and time for restoration reverse them.<br />
In higher doses, they cause serious illness or injury requiring specific medical or surgical<br />
treatment. When the major contributing factors to battle fatigue are physical stresses that<br />
leaders can relieve, treatment is usually simple and recovery is rapid. Physical factors are<br />
not necessarily the cause of battle fatigue, however. When the Soldier is diagnosed, the<br />
absence of obvious physical stressors should not detract from a positive expectation that<br />
the Soldier will rapidly and fully recover.<br />
Home-Front and Other Preexisting Problems. The fourth factor is home-front and<br />
preexisting problems. Israeli studies found that the strongest factor that distinguished
<strong>Combat</strong> <strong>Stress</strong> <strong>Management</strong> ■ 51<br />
Soldiers who were decorated for heroic acts from those who became battle-shock casualties<br />
was whether the casualties had experienced many recent changes on the home front.<br />
Negative home-front problems may be a “Dear John” letter, a sick parent or child, or bad<br />
debts. Or it may be something positive—such as a recent marriage or becoming a parent.<br />
Worrying about what is happening back home distracts Soldiers from focusing their<br />
psychological defenses on combat stressors. It creates internal conflict between performing<br />
their combat duty and resolving their home-front problems or concerns.<br />
Other <strong>Stress</strong> Factors<br />
The second-strongest factor the Israeli studies found was unit cohesion: The Soldiers<br />
who became stress casualties often went into battle alongside strangers, while those who<br />
became heroes fought alongside unit members they knew well, trusted, and depended<br />
on. These findings confirm observations from previous wars. Other stressors that experts<br />
often cite include lack of information; lack of confidence in leaders, supporting units, or<br />
equipment in comparison with the enemy’s; and lack of belief in the justness of the war.<br />
It is worth noting that individual personality makeup does not predict susceptibility<br />
to battle fatigue. Careful studies by the <strong>Army</strong> after World War II and by the Israelis since<br />
the Yom Kippur War all show that no clear relationship exists between neurotic traits or<br />
personality disorders and battle fatigue. People with these traits were no more likely to<br />
become battle fatigue casualties and no less likely to be decorated for valor than were those<br />
Soldiers who tested as normal.<br />
There are personality factors that may predict who will be a poor Soldier (or who<br />
may be prone to commit acts of misconduct if given opportunities or excuses). But<br />
these factors will not predict who<br />
will get battle fatigue. There are<br />
good predictors of battle fatigue, but<br />
individual personality type is not<br />
one of them. Anyone may become<br />
a battle fatigue casualty if he or<br />
she confronts too many high-risk<br />
factors. Personality factors, however,<br />
may help predict who is likely to<br />
recover slowly from disabling battle<br />
fatigue. We’ve reviewed what to look<br />
for in the way of battle-fatigue<br />
behaviors, and what can cause them.<br />
Now let’s look at how you can<br />
combat and control battle fatigue.
52 ■ SECTION 3<br />
Soldiers can manage<br />
light battle fatigue by<br />
themselves and with the<br />
help of buddies, unit<br />
medics, and leaders.<br />
Most Soldiers in combat<br />
will have light battle<br />
fatigue at some time.<br />
Duty and rest cases are<br />
not medical casualties<br />
because they are still<br />
available for some duty<br />
in their units. Those<br />
heavy cases who cannot<br />
return to duty or rest in<br />
their unit the same day,<br />
however, are battlefatigue<br />
casualties.<br />
The hold and refer sublabels<br />
of heavy battle<br />
fatigue do not<br />
necessarily mean that a<br />
Soldier is less likely to<br />
recover or will take<br />
longer to recover than<br />
cases treated as rest.<br />
The holding or<br />
evacuation itself often<br />
prolongs the treatment,<br />
however, and decreases<br />
likelihood of full recovery<br />
and return to duty.<br />
<strong>Combat</strong> <strong>Stress</strong> Control Techniques<br />
Soldiers can manage light battle fatigue by themselves and with the help of buddies, unit<br />
medics, and leaders. Most Soldiers in combat will have light battle fatigue at some time.<br />
This includes the normal/common signs of battle fatigue listed previously. You do not need<br />
to send Soldiers with these symptoms immediately for medical evaluation; they can usually<br />
continue on duty. If the symptoms persist after rest, however, you should send the Soldiers<br />
to their unit surgeon or physician assistant at routine sick call as cases of heavy battle fatigue.<br />
Heavy battle fatigue requires immediate medical evaluation at a medical treatment facility.<br />
The Soldier’s symptoms may be:<br />
• Behavior that is temporarily too disruptive to the unit’s missions<br />
• A medical or surgical condition that requires observation and diagnosis to rule out<br />
the need for emergency treatment. Medical triage sorts Soldiers with heavy battle<br />
fatigue according to where they can best be treated.<br />
Duty cases are those in which a physician or physician’s assistant sees the Soldier, but can<br />
treat the Soldier immediately and return him or her to duty in his or her unit.<br />
Rest cases must be sent to their unit’s nonmedical combat service support (CSS) elements<br />
for brief rest and light duties. Rest cases do not require continual medical observation.<br />
Hold cases are those whom the triager can hold for treatment at the triager’s own medical<br />
facility because both the tactical situation and the battle-fatigue casualties’ symptoms<br />
permit. This should be done whenever feasible.<br />
Refer cases are those who must be referred (and transported) to a more secure or betterequipped<br />
medical facility, either because of the tactical situation or the battle fatigue<br />
casualties’ symptoms. A refer case becomes a hold case when Soldiers reach a medical<br />
treatment facility where they can be held and treated.<br />
There is no easy rule for deciding whether any specific symptom of battle fatigue makes<br />
the Soldier a case of duty, rest, hold, or refer battle fatigue. That will require your best<br />
judgment based on:<br />
• What you know about the individual Soldier<br />
• The stressors involved<br />
• The Soldier’s response to help<br />
• What is likely to happen to the unit next<br />
• The resources available.<br />
Battle-fatigue symptoms can change rapidly, depending on a Soldier’s expectations. A<br />
successful program to control combat stress prevents unnecessary evacuation and shifts battlefatigue<br />
cases from refer to the hold triage category. More importantly, such a program shifts<br />
many Soldiers from the hold category to the rest and duty categories. This allows them to<br />
recover in their units and keeps them from overloading the health-service support system.
<strong>Combat</strong> <strong>Stress</strong> <strong>Management</strong> ■ 53<br />
Mild Traumatic Brain Injury (mTBI), Post <strong>Combat</strong> <strong>Stress</strong>,<br />
and Post-Traumatic <strong>Stress</strong> Disorder<br />
Both mild Traumatic Brain Injury (mTBI) and post combat stress can negatively affect<br />
Soldiers’ ability to perform their jobs. Whether in combat or in garrison, Soldiers’ inability<br />
to perform as well as they can puts both themselves and their teammates at increased<br />
risk.<br />
This is a serious issue that affects everyone differently – you, your immediate and<br />
extended family, friends, and fellow Soldiers. This issue is as important as any other Soldier<br />
health issue or challenge. The <strong>Army</strong>’s war-fighting capability depends on it.<br />
Both mTBI and post combat stress may result without visible physical injuries and<br />
may impact on your performance and readiness. Post combat stress is also called Post<br />
Traumatic <strong>Stress</strong> Disorder, although there are slight differences between the two. If post<br />
combat stress interferes with a Soldier’s ability to do his or her job and enjoy life, and it<br />
seems to continually get worse, it could lead to the mental health diagnosis known as<br />
Post Traumatic <strong>Stress</strong> Disorder.<br />
Most Soldiers will do well, but for some, persistent symptoms of post combat stress<br />
may require support or medical care.<br />
A Soldier may experience effects of either mTBI or post combat stress following a<br />
significant combat or operational experience. It is also important to understand that a<br />
Soldier may experience effects of both conditions at the same time.<br />
mild Traumatic Brain<br />
Injury (mTBI)<br />
a type of concussion<br />
that results from a blow<br />
to the head and does<br />
not result in an obvious<br />
physical injury<br />
post combat stress<br />
long-term reaction to<br />
combat and operational<br />
exposure that can impact<br />
a person’s quality of life<br />
Post Traumatic <strong>Stress</strong><br />
Disorder (PTSD)<br />
a severe form of post<br />
combat stress<br />
Mild Traumatic Brain Injury (mTBI)<br />
It is useful to think of mTBI as a concussion. Unlike a severe Traumatic Brain Injury, in<br />
which there may be a penetrating head injury with an obvious wound, a mild TBI or<br />
concussion results from a hard blow or jolt to the head, a series of blows, or blast exposure<br />
that causes the brain to be shaken within the skull. A good example would be exposure to<br />
the shock wave of an improvised explosive device (IED) explosion. Concussions do not<br />
result in any obvious physical injury. However, they can result in a disruption of brain<br />
functions. Blasts, particularly from IEDs of all types, can result in concussions where the<br />
Soldier may suffer a brief loss of consciousness, confusion, or brief loss of memory about<br />
events before or after the incident. Sometimes people refer to this as “getting your bell<br />
rung.” Some Soldiers who have concussions may “see stars,” feel dazed or confused, report<br />
ringing in the ears, or just feel “not quite right.”<br />
A common mTBI injury is hearing loss. Injured Soldiers may not even realize that they<br />
have a significant hearing loss, and that may add to their frustration. This type of complaint<br />
is common for concussions. It is important for you as a leader to ensure that Soldiers<br />
who experience blasts are evaluated by a medical officer immediately upon returning to<br />
the base camp or forward operating base. Concussions rarely are life threatening. However,<br />
if a Soldier sustains a head injury during combat missions, it is critical that he or she be<br />
evaluated at the earliest possible opportunity.<br />
Many Soldiers who have had a concussion may say that they are “fine,” although their<br />
behavior or manners are temporarily altered immediately after the event. This is where<br />
both leadership and buddy aid are critical.<br />
It is your responsibility to ensure that all your Soldiers suspected of having concussions<br />
are evaluated by a medical officer. You must take into account the medical recommendations<br />
resulting from the evaluation, even if that includes having the Soldier “take a knee” for a<br />
few days. This is necessary because if a Soldier suffers another concussion without having
54 ■ SECTION 3<br />
recovered from the first, the second concussion may cause permanent brain damage. You<br />
may be required to make field decisions to continue executing a mission or use valuable<br />
resources to extract the Soldier. If a Soldier remains oriented and alert, you may delay the<br />
evaluation. However, you must ensure that the Soldier is evaluated as soon as practical.<br />
Soldiers suffering from mTBI are a risk to your unit’s ability to execute missions effectively.<br />
Other Soldiers must be aware of this type of injury and make sure to inform you if<br />
someone is hurt. It is important that medical assistance be provided to any Soldier who is<br />
exposed to a blast or receives a head injury, or begins to complain of symptoms typically<br />
associated with concussion—especially if the Soldier acts differently after that event.<br />
The key to recovery from a concussion is time, knowledge, and education. Nearly all<br />
Soldiers have recovered or will recover.<br />
Remember, however, that concussions are not always combat related. They can also<br />
occur during training, such as combatives or airborne and air assault exercises. That is why<br />
Soldiers must wear safety equipment and you, the platoon leader, must conduct appropriate<br />
risk assessments.<br />
In any case, it is essential that you and your Soldiers know, understand, and recognize<br />
the signs and symptoms of mTBI and post combat stress.<br />
Post <strong>Combat</strong> <strong>Stress</strong><br />
No amount of training can totally prepare a Soldier for the realities of combat. Post combat<br />
stress is a possible outcome of all combat and operational missions. It may develop after<br />
someone has experienced or witnessed an actual or threatened traumatic event.<br />
Most Soldiers are resilient and work through their experiences. The resiliency displayed<br />
by these Soldiers is referred to as mental toughness or Battlemind. Battlemind skills,<br />
developed in military training, provide Soldiers the inner strength to face fear, adversity,<br />
and hardship during combat with confidence and resolution; the will to persevere and win.<br />
Figure 3.1<br />
Concussion Versus Post <strong>Combat</strong> <strong>Stress</strong>
<strong>Combat</strong> <strong>Stress</strong> <strong>Management</strong> ■ 55<br />
Figure 3.2<br />
<strong>Combat</strong> and Operational Missions, and Post <strong>Combat</strong> <strong>Stress</strong><br />
Figure 3.3<br />
What to Look For
56 ■ SECTION 3<br />
However, sometimes even the strongest Soldiers are affected so severely that they will<br />
need additional help. Both the good and bad experiences can follow for a lifetime. Many<br />
warriors will come back better leaders, fathers, or mothers, often more resilient and not<br />
taking life for granted.<br />
But this transition may not be easy for everyone. Every Soldier is at risk of post combat<br />
stress, and between 20 and 30 percent of US military personnel returning from current<br />
combat operations report psychological symptoms. Some may still struggle with anger,<br />
withdraw from those they care about, or have sleep problems. All of these are normal<br />
reactions to abnormal experiences. Soldiers can deal with these problems in positive ways.<br />
Relaxing, resting, and exercise are three good ways to adjust.<br />
If a Soldier continues to have difficulty adjusting to what he or she experienced on<br />
the battlefield, however, this may negatively impact the Soldier’s intimacy with his or her<br />
spouse or other close relationships with friends, family, and coworkers. Soldiers may also<br />
begin to abuse alcohol or other drugs to try to deal with the stress. Casual drinking is<br />
common with many Soldiers, but when used excessively as an attempt to manage post<br />
combat stress, it can actually create more problems. A few beers may help you sleep on a<br />
given night, but it may also slow down your long-term recovery. Those Soldiers who require<br />
significant assistance to cope with the reactions they are having due to their military<br />
experience may be diagnosed with PTSD.<br />
There are three main things you should look out for in the weeks or months after the<br />
event is over and you’re in a safe environment. They include:<br />
1. Re-experiencing the event over and over again<br />
2. Avoiding people, places, or feelings that remind you of the event<br />
3. Feeling “keyed up” or on-edge all the time.<br />
If you or a fellow Soldier is struggling, seek help. It is important to remember, although<br />
a Soldier may not be struggling, his or her battle buddy may be. <strong>Combat</strong> and operational<br />
experience will affect every Soldier differently.<br />
Soldiers with the highest combat exposure and those conducting missions outside<br />
the wire have higher rates of post combat stress. Those Soldiers experiencing post combat<br />
stress may continue to struggle with symptoms long after redeployment. Some do not<br />
“reset” quickly after coming home and may continue to struggle, even 12 months later.<br />
The Leader’s Responsibility<br />
You must recognize the continued effects of exposure to combat and operational stress.<br />
Understanding these effects will help you and your Soldiers to support one another.<br />
You and your Soldiers have a responsibility to maintain yourselves and to help your<br />
units and battle buddies. The key is to be aware of the symptoms of combat and operational<br />
stress, and to watch for these symptoms in yourself and in your battle buddies. You and<br />
your Soldiers have a duty not to hide symptoms of an illness and to do the right thing:<br />
Seek help when it is needed.<br />
As a leader, you will need to recognize changes and have the courage to step up and<br />
make sure you get help for yourself and your Soldiers. You, more than anyone else, will<br />
recognize if something doesn’t seem right with one of your Soldiers. Do something about<br />
it—nobody needs to go it alone.<br />
Leaders at all levels also have specific responsibilities. <strong>Stress</strong> conditions affecting Soldiers<br />
are no different than any other injury or illness that causes loss of combat effectiveness.<br />
You need to know where to find help and how to get it to your Soldiers.<br />
Remember that combat and operational stress are part of a Soldier’s experience, and<br />
most Soldiers will successfully adapt to combat conditions. Bear in mind, however, that<br />
some Soldiers may suffer from concussions or may develop post combat stress. Some<br />
may be affected by both. If you get help for your Soldiers, their recovery will be faster and<br />
more complete.
<strong>Combat</strong> <strong>Stress</strong> <strong>Management</strong> ■ 57<br />
The <strong>Army</strong> has resources to assist Soldiers affected by concussion and post combat<br />
stress. As a leader, you should be aware of them and ensure that your Soldiers get the help<br />
they need.<br />
You should keep two key leadership points in mind:<br />
1. Lead by example. You are not exempt from struggling with concussions or post<br />
combat stress. It is imperative that you take action and lead by example by getting<br />
the help you need.<br />
2. Manage risk. Identify and assess hazards to your Soldiers’ health from mTBI and<br />
post combat stress. As part of controlling or minimizing these hazards, ensure that<br />
your Soldiers receive appropriate care and support. Make sure that you have<br />
coordinated for the resources they need and that those resources are ready to<br />
provide the assistance your Soldiers may require.<br />
You are responsible not only for recognizing symptoms, but also for playing an active<br />
role in facilitating access to, and allowing Soldiers to seek, help and referral.<br />
Always remember that not everyone reacts the same way to potentially traumatic events.<br />
What may be upsetting to one Soldier may not be for another. Do not assume that a Soldier<br />
is unaffected by an event just because you or others were not affected. To do so promotes<br />
a dangerous stigma, which may discourage Soldiers from getting the help they need. You<br />
must act to reduce the stigma associated with seeking help. Not seeking help can worsen<br />
Soldiers’ conditions. It works against a Soldier’s readiness and effectiveness.<br />
Military One Source is a resource that does not treat PTSD but provides up to six free<br />
counseling sessions for needs associated with PTSD—such as stress management, couple’s<br />
counseling, or parent-child problems. These services are confidential, and spouses and<br />
dependents can also use them. The Veterans Affairs Department provides resources for<br />
retired or separated Soldiers and their families, including treatment of PTSD.<br />
Critical Thinking<br />
You are the platoon leader conducting a platoon ambush. Your 3rd Squad Leader,<br />
SSG Suttles, is the security element leader for the ambush. SSG Suttles’ security<br />
element must provide left, right, and rear flank security for the ambush. You took<br />
SSG Suttles on the leaders’ recon so that he could identify where to place his<br />
security teams. During the leaders’ recon, he showed signs of combat stress,<br />
including heightened startle response and excessive sweating. During the final<br />
planning in the objective rally point (ORP), he seemed to have difficulty paying<br />
attention and remembering his key tasks for the ambush. These symptoms seem to<br />
be getting worse as you make final preparations at the ORP. You have less than<br />
three hours to have your ambush in place, and you are two hours from your<br />
forward operating base (FOB). You do not have time to move him back to the FOB<br />
and get a replacement. Requesting a MEDEVAC could compromise the location of<br />
your patrol base and compromise the ambush mission itself. Do you leave SSG<br />
Suttles in the ORP and make his team leader, SGT Newby, the security element<br />
leader, or do you keep SSG Suttles as the security element leader based on his past<br />
performance? SGT Newby reported to your unit three months ago, fresh from the<br />
Primary Leadership Development Course. He did not participate in the leaders’<br />
recon, and there is no time for you to take him back to the objective to recon the<br />
security team positions. What will you do? How can you use the information<br />
presented in this chapter to help you assess SSG Suttles’ condition?<br />
e<br />
• Assistance for<br />
Soldiers and Families<br />
Unit – chaplain/<br />
leadership/buddy<br />
• Post hospital, clinic, or<br />
troop medical clinic<br />
• Mental – Behavioral<br />
Health Services<br />
• Off-post – mental<br />
health professional<br />
• Military One Source:<br />
1-800-342-9647<br />
• Veterans Affairs (VA)<br />
Health care:<br />
1-877-222-8887<br />
PTSD Information Line:<br />
1-802-296-6300
58 ■ SECTION 3<br />
e<br />
CONCLUSION<br />
Know your troops, and<br />
be alert for any sudden,<br />
persistent, or progressive<br />
change in their behavior<br />
that threatens the<br />
functioning and safety of<br />
your unit.<br />
<strong>Combat</strong>. You and your troops will experience danger and profound physical and<br />
emotional reactions to it. Some reactions sharpen Soldiers’ abilities to survive and<br />
win. Other reactions may produce disruptive behaviors that threaten individual<br />
and unit safety. Soldiers in combat experience a range of emotions, but their<br />
behavior influences their immediate safety and mission success. You must keep<br />
yourself and your unit working at the level of stress that sustains performance and<br />
confidence. When troops begin to lose confidence in themselves and their leader,<br />
they are more likely to suffer adverse stress reactions that cause battle fatigue.<br />
It is important for you to recognize these adverse behaviors at the onset in<br />
order to intervene promptly for the safety and benefit of individual Soldiers and<br />
the unit. These behaviors may take many forms and can range from subtle to dramatic.<br />
Any Soldier who shows persistent, progressive behavior that deviates from<br />
his or her normal behavior may be demonstrating the early warning signs and<br />
symptoms of combat stress. Rather than trying to memorize every possible sign<br />
and symptom, you’ll be able to diagnose combat stress more quickly if you keep<br />
one simple rule in mind: Know your troops. Be alert for any sudden, persistent, or<br />
progressive change in their behavior that threatens the functioning and safety of<br />
your unit.<br />
Concussions (mTBI) and post combat stress are legitimate medical and<br />
psychological conditions, which may require the attention of health-care<br />
professionals. Remember, all Soldiers who have deployed to combat are affected<br />
in some way or another. You need to work to educate yourself and your<br />
subordinates. This is about taking care of each other—and this is about trust.<br />
That trust will sustain you and your unit in combat and will help you to deal with<br />
mTBI and combat stress. Every Soldier needs to trust that the <strong>Army</strong> is there for<br />
him or her.<br />
Learning Assessment<br />
1. List the seven major categories of behaviors that may indicate the onset of<br />
battle fatigue.<br />
2. Describe some of the physical functions that may be impaired when a Soldier<br />
has battle fatigue.<br />
3. List and explain the two most common themes that are present in Soldiers<br />
with battle fatigue.<br />
4. Define the four major contributing factors to battle fatigue.
<strong>Combat</strong> <strong>Stress</strong> <strong>Management</strong> ■ 59<br />
5. List some of the methods used by Soldiers and medical personnel to manage<br />
or control combat stress.<br />
6. Define PTSD.<br />
7. Define mTBI.<br />
8. Explain the two major leader actions you can take to help your Soldiers<br />
reduce their susceptibility to combat stress or battle fatigue.<br />
Key Words<br />
battle fatigue<br />
stress-related behaviors<br />
combat stressors<br />
mild Traumatic Brain Injury (mTBI)<br />
post combat stress<br />
Post Traumatic <strong>Stress</strong> Disorder (PTSD)<br />
References<br />
DoD Directive 6490.5, <strong>Combat</strong> <strong>Stress</strong> Control (CSC) Programs. 24 November 2003.<br />
DoD Instruction 6490.3, Deployment Health. 7 August 1997.<br />
Field Manual 4-02.51, <strong>Combat</strong> and Operational <strong>Stress</strong> Control. July 2006,<br />
Field Manual 6-22.5, A Leader’s Guide to <strong>Combat</strong> and Operational <strong>Stress</strong> (Small Unit)<br />
DRAFT. February 2007.<br />
Field Manual 8-51, <strong>Combat</strong> <strong>Stress</strong> Control in a Theater of Operations—Tactics, Techniques,<br />
and Procedures. 29 September 1994.<br />
Field Manual 22-51, Leaders’ Manual for <strong>Combat</strong> <strong>Stress</strong> Control. 29 September 1994.<br />
Miles, D. (27 June 2007). Injured Veteran Uses Own Experience to Inspire Others With<br />
Traumatic Brain Injuries. <strong>Army</strong> News Service. Retrieved 25 April 2008 from<br />
http://www.army.mil/-news/2007/06/28/3839-injured-veteran-uses-own-experienceto-inspire-others-with-traumatic-brain-injuries/<br />
Quick Facts: Traumatic Brain Injury; Post-Traumatic <strong>Stress</strong> Disorder. (23 April 2007).<br />
Department of Defense. Retrieved 17 July 2008 from http://fhp.osd.mil/pdhrainfo/media<br />
/TBI_and_PTSD_Quick_Facts.<strong>pdf</strong>