The Challenges Of Testing For And Diagnosing Porphyrias
The Challenges Of Testing For And Diagnosing Porphyrias
The Challenges Of Testing For And Diagnosing Porphyrias
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
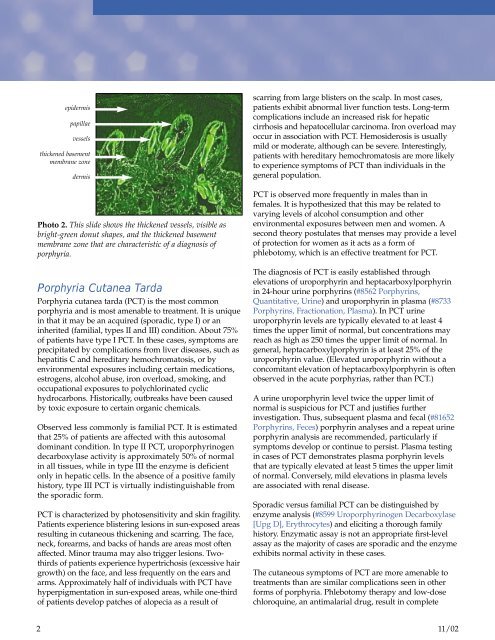
epidermis<br />
papillae<br />
vessels<br />
thickened basement<br />
membrane zone<br />
dermis<br />
Photo 2. This slide shows the thickened vessels, visible as<br />
bright-green donut shapes, and the thickened basement<br />
membrane zone that are characteristic of a diagnosis of<br />
porphyria.<br />
Porphyria Cutanea Tarda<br />
Porphyria cutanea tarda (PCT) is the most common<br />
porphyria and is most amenable to treatment. It is unique<br />
in that it may be an acquired (sporadic, type I) or an<br />
inherited (familial, types II and III) condition. About 75%<br />
of patients have type I PCT. In these cases, symptoms are<br />
precipitated by complications from liver diseases, such as<br />
hepatitis C and hereditary hemochromatosis, or by<br />
environmental exposures including certain medications,<br />
estrogens, alcohol abuse, iron overload, smoking, and<br />
occupational exposures to polychlorinated cyclic<br />
hydrocarbons. Historically, outbreaks have been caused<br />
by toxic exposure to certain organic chemicals.<br />
Observed less commonly is familial PCT. It is estimated<br />
that 25% of patients are affected with this autosomal<br />
dominant condition. In type II PCT, uroporphyrinogen<br />
decarboxylase activity is approximately 50% of normal<br />
in all tissues, while in type III the enzyme is deficient<br />
only in hepatic cells. In the absence of a positive family<br />
history, type III PCT is virtually indistinguishable from<br />
the sporadic form.<br />
PCT is characterized by photosensitivity and skin fragility.<br />
Patients experience blistering lesions in sun-exposed areas<br />
resulting in cutaneous thickening and scarring. <strong>The</strong> face,<br />
neck, forearms, and backs of hands are areas most often<br />
affected. Minor trauma may also trigger lesions. Twothirds<br />
of patients experience hypertrichosis (excessive hair<br />
growth) on the face, and less frequently on the ears and<br />
arms. Approximately half of individuals with PCT have<br />
hyperpigmentation in sun-exposed areas, while one-third<br />
of patients develop patches of alopecia as a result of<br />
scarring from large blisters on the scalp. In most cases,<br />
patients exhibit abnormal liver function tests. Long-term<br />
complications include an increased risk for hepatic<br />
cirrhosis and hepatocellular carcinoma. Iron overload may<br />
occur in association with PCT. Hemosiderosis is usually<br />
mild or moderate, although can be severe. Interestingly,<br />
patients with hereditary hemochromatosis are more likely<br />
to experience symptoms of PCT than individuals in the<br />
general population.<br />
PCT is observed more frequently in males than in<br />
females. It is hypothesized that this may be related to<br />
varying levels of alcohol consumption and other<br />
environmental exposures between men and women. A<br />
second theory postulates that menses may provide a level<br />
of protection for women as it acts as a form of<br />
phlebotomy, which is an effective treatment for PCT.<br />
<strong>The</strong> diagnosis of PCT is easily established through<br />
elevations of uroporphyrin and heptacarboxylporphyrin<br />
in 24-hour urine porphyrins (#8562 Porphyrins,<br />
Quantitative, Urine) and uroporphyrin in plasma (#8733<br />
Porphyrins, Fractionation, Plasma). In PCT urine<br />
uroporphyrin levels are typically elevated to at least 4<br />
times the upper limit of normal, but concentrations may<br />
reach as high as 250 times the upper limit of normal. In<br />
general, heptacarboxylporphyrin is at least 25% of the<br />
uroporphyrin value. (Elevated uroporphyrin without a<br />
concomitant elevation of heptacarboxylporphyrin is often<br />
observed in the acute porphyrias, rather than PCT.)<br />
A urine uroporphyrin level twice the upper limit of<br />
normal is suspicious for PCT and justifies further<br />
investigation. Thus, subsequent plasma and fecal (#81652<br />
Porphyrins, Feces) porphyrin analyses and a repeat urine<br />
porphyrin analysis are recommended, particularly if<br />
symptoms develop or continue to persist. Plasma testing<br />
in cases of PCT demonstrates plasma porphyrin levels<br />
that are typically elevated at least 5 times the upper limit<br />
of normal. Conversely, mild elevations in plasma levels<br />
are associated with renal disease.<br />
Sporadic versus familial PCT can be distinguished by<br />
enzyme analysis (#8599 Uroporphyrinogen Decarboxylase<br />
[Upg D], Erythrocytes) and eliciting a thorough family<br />
history. Enzymatic assay is not an appropriate first-level<br />
assay as the majority of cases are sporadic and the enzyme<br />
exhibits normal activity in these cases.<br />
<strong>The</strong> cutaneous symptoms of PCT are more amenable to<br />
treatments than are similar complications seen in other<br />
forms of porphyria. Phlebotomy therapy and low-dose<br />
chloroquine, an antimalarial drug, result in complete<br />
2<br />
11/02