Uterine evacuation with manual vacuum aspiration ... - CommonHealth
Uterine evacuation with manual vacuum aspiration ... - CommonHealth
Uterine evacuation with manual vacuum aspiration ... - CommonHealth
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Uterine</strong> Evacuation <strong>with</strong><br />
Manual Vacuum Aspiration (MVA)<br />
A Training<br />
Manual for<br />
Conducting<br />
Short Courses
ISBN:1-933095-50-4<br />
©2009 Ipas.<br />
Produced in the United States of America.<br />
Suggested Citation: Ipas. 2009. <strong>Uterine</strong> Evacuation <strong>with</strong> Manual Vacuum Aspiration (MVA): A Training Manual for<br />
Conducting Short Courses. Chapel Hill, NC: Ipas.<br />
Ipas is a nonprofit organization that works globally to increase women’s ability to exercise their sexual and<br />
reproductive rights and to reduce abortion-related deaths and injuries. We seek to expand the availability,<br />
quality and sustainability of abortion and related reproductive health services, as well as to improve the enabling<br />
environment. Ipas believes that no woman should have to risk her life or health because she lacks safe reproductive<br />
health choices.<br />
WomanCare Global LLC is an exclusive distributor of Ipas instruments. For information regarding availability or to<br />
report an adverse event contact WomanCare Global at customerservice@womancareglobal.com or 919 442-2600.<br />
Ipas<br />
PO Box 5027<br />
Chapel Hill, North Carolina 27514, USA<br />
Web site: www.ipas.org<br />
Email: training@ipas.org<br />
Graphic Design: Jamie McLendon<br />
Editor: Jennifer Daw Holloway<br />
Printed on recycled paper<br />
An Ipas international publication
Manual Vacuum Aspiration (MVA)<br />
Each year, nearly 67,000 women die from unsafe abortion and about 5 million<br />
more are injured, often permanently (WHO 2007). Many of these women could<br />
be saved and their injuries prevented if clinicians in their communities were<br />
trained and equipped to use a simple, inexpensive medical device — the <strong>manual</strong><br />
<strong>vacuum</strong> <strong>aspiration</strong> (MVA) instrument.<br />
MVA involves the use of a plastic aspirator to evacuate the uterus for miscarriage<br />
management (incomplete, missed or inevitable abortion), first-trimester abortion<br />
(also called menstrual regulation), and endometrial biopsy. The <strong>manual</strong> <strong>vacuum</strong><br />
aspirator consists of a cylinder, plunger and valve. To evacuate the uterus, the<br />
aspirator is attached to a cannula which is inserted through the cervix to aspirate<br />
the contents of the uterus.<br />
The MVA device is handheld and portable. The procedure is quiet, fast and<br />
inexpensive (Dalton 2006) and can be performed in a wide variety of clinical<br />
settings because it does not rely on electricity. Unlike traditional dilatation and<br />
curettage <strong>with</strong> a sharp curette, an MVA procedure does not typically require<br />
general anesthesia. In a small percentage of cases (
Because of its importance to obstetric care, WHO and the United Nations<br />
Population Fund (UNFPA) have included MVA instruments on their proposed list<br />
of essential drugs and other commodities for reproductive health care (WHO and<br />
UNFPA 2003) and in technical guidance for uterine <strong>evacuation</strong> (WHO 2003).<br />
This Resource<br />
Historically, Ipas and other international nongovernmental organizations have<br />
supported training events of five days or more <strong>with</strong> the goal of health-care<br />
facilities adopting a model of more comprehensive care for women (either<br />
postabortion care or abortion care, including MVA for treatment, as well as<br />
contraceptive services, counseling for other health needs, provision of other<br />
reproductive health services and community partnerships for prevention of<br />
unsafe abortion).<br />
Though many health-care professionals are eager to gain the knowledge and skills<br />
necessary to provide obstetric care <strong>with</strong> MVA, they cannot take significant time<br />
away from clinical responsibilities to take part in lengthy training events. Ipas<br />
recognizes that every clinician does not need a comprehensive course designed<br />
to help a team adopt a new model of care and notes that professionals come to<br />
training events <strong>with</strong> existing ranges of knowledge and skills and varying learning<br />
needs. Clinicians can avail themselves of a broad continuum of educational<br />
options to gain the knowledge and skills they need at a particular point in<br />
their professional careers and practices. The courses outlined in this <strong>manual</strong><br />
are designed to meet the middle range of training needs in MVA use. For<br />
example, attending these courses requires more effort/time and results in more<br />
knowledge/skill-building than simply reading MVA product inserts or studying a<br />
wallchart, but not as much as performing several procedures one-on-one <strong>with</strong> an<br />
experienced clinical trainer supervising or attending a multi-day clinical course.<br />
This <strong>manual</strong>, which is specific to MVA (excluding the other elements of<br />
comprehensive models), will serve as a guide for MVA training facilitators to<br />
provide three standard courses — each <strong>with</strong> different objectives, prerequisites<br />
and course lengths, based on the participants’ level of familiarity <strong>with</strong> MVA and<br />
experience <strong>with</strong> transvaginal procedures. The courses include up-to-date content<br />
and are based on principles of adult learning. Participants who successfully<br />
complete the courses will gain the specified knowledge and skills offered in each of<br />
the courses. Variations of these standard courses have been delivered around the<br />
world.<br />
2 ·UTERINE EVACUATION WITH MANUAL VACUUM ASPIRATION (MVA): A TRAINING MANUAL FOR CONDUCTING SHORT COURSES
The Courses<br />
The three courses vary in length and scope and can be offered separately or in<br />
a series so that participants can attend more than one course in a convenient<br />
timeframe. The basic course themes are:<br />
• MVA and its clinical applications;<br />
• How to perform MVA on a pelvic model and all local instrument processing<br />
options (where regulatory conditions approve re-use);<br />
• The above topics plus supervised clinical practice, management of<br />
complications and guidance on monitoring of services.<br />
Training facilitators should select course materials based on the environmental<br />
context in which the learners will put their new knowledge and skills to use. The<br />
two key issues of environmental context to identify for course content selection<br />
are:<br />
1. Clinical applications for<br />
use of MVA<br />
In every country of the world, there are at least two clinical applications for MVA: treatment of incomplete or missed abortion<br />
(miscarriage) and endometrial biopsy. Additionally, in most countries, therapeutic abortion is legally permitted to save the<br />
woman’s life or preserve her health and/or for other indications. Most women live in countries where induced abortion is<br />
permitted, <strong>with</strong> or <strong>with</strong>out restrictions (CRLP 2007).<br />
Materials on the CD-ROM included <strong>with</strong> this <strong>manual</strong> are labeled <strong>Uterine</strong> Evacuation for either<br />
• INCOMPLETE/MISSED ABORTION: for use in contexts that focus on treatment of incomplete/missed abortion, whether<br />
miscarriage management or treatment of complications of an induced procedure, and endometrial biopsy<br />
• Or, ALL INDICATIONS: for contexts that include treatment of incomplete/missed abortion, first-trimester induced abortion<br />
and endometrial biopsy<br />
2. Regulatory Context: Are<br />
cannulae labeled for<br />
single or multiple use?<br />
The use and re-use of cannulae varies among countries and clinical practices. In the United States and some other countries,<br />
Ipas EasyGrip ® cannulae are labeled for single use and should be discarded after use. Where local regulations permit, these<br />
cannulae can be reused after high-level disinfection or sterilization. Please note that flexible Karman cannulae and 3mm<br />
cannulae for endometrial biopsy are labeled for single use in all countries and should be discarded after use.<br />
Trainers should plan to follow country-specific labeling regarding single-use or processing of instruments for reuse. Materials<br />
on the CD-ROM included <strong>with</strong> this <strong>manual</strong> are labeled either<br />
• SINGLE USE: for settings where cannulae are used once and discarded<br />
• Or, MULTIPLE USE: for settings where cannulae are processed for reuse<br />
UTERINE EVACUATION WITH MANUAL VACUUM ASPIRATION (MVA): A TRAINING MANUAL FOR CONDUCTING SHORT COURSES · 3
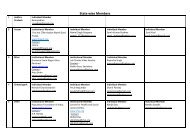
The Courses at a Glance<br />
Title Course 101<br />
Introduction to MVA<br />
Course 201<br />
Pelvic Model Practice <strong>with</strong> MVA<br />
Course 301<br />
Supervised Clinical Practice <strong>with</strong> MVA<br />
Description • Introduction to MVA • Practice MVA on a Pelvic Model<br />
• Processing MVA instruments for reuse,<br />
where allowed<br />
• Supervised Clinical Practice <strong>with</strong> MVA<br />
• Monitoring of Services<br />
• Management of Complications<br />
Program Length ~ three hours ~ four hours ~ One six to eight hour day<br />
Prerequisites None • Course 101 or equivalent IpasUniversity<br />
course completions, which are:<br />
– MVA Facts and Features<br />
– <strong>Uterine</strong> Evacuation <strong>with</strong> Ipas MVA Plus ®<br />
– Stocking Facilities <strong>with</strong> MVA<br />
• Course 101 or equivalent IpasUniversity<br />
course completions, which are:<br />
– MVA Facts and Features<br />
– <strong>Uterine</strong> Evacuation <strong>with</strong> Ipas MVA Plus<br />
– Stocking Facilities <strong>with</strong> MVA<br />
AND<br />
• Course 201<br />
Topics Covered<br />
• <strong>Uterine</strong> <strong>evacuation</strong> methods<br />
• MVA facts and features: Clinical<br />
application and product features<br />
• Supervised practice on pelvic model<br />
• Processing instruments for reuse, where<br />
allowed<br />
• Perform a supervised MVA procedure in a<br />
clinical facility*<br />
• Monitoring of services<br />
• Overview of MVA procedure<br />
• Management of complications<br />
• MVA stocking and resupply<br />
Learning<br />
Objectives<br />
Upon completion<br />
participants will:<br />
• Be familiar <strong>with</strong> the Ipas MVA<br />
instruments and know how and<br />
when to resupply<br />
• Be able to simulate MVA on a pelvic model<br />
• Be able to process MVA instruments in<br />
accordance <strong>with</strong> local regulations and <strong>with</strong><br />
locally available products/systems<br />
• Have performed a supervised MVA<br />
procedure in a local clinical facility*<br />
• Be familiar <strong>with</strong> key tools for monitoring<br />
services <strong>with</strong> a goal toward quality<br />
improvement<br />
• Be able to manage potential complications<br />
Recommended<br />
Trainers/<br />
Presenters<br />
• 1 clinical trainer<br />
• 1 representative from local MVA<br />
distributor who can facilitate<br />
stocking and resupply of<br />
instruments<br />
• 1 clinical trainer<br />
• 1 representative from local MVA distributor<br />
who can facilitate stocking and resupply of<br />
instruments<br />
• 1 clinical trainer and 2 additional clinical<br />
trainers for part of the workshop<br />
• 1 representative from local MVA distributor<br />
who can facilitate stocking and resupply of<br />
instruments<br />
Recommended<br />
Participants<br />
Up to 20 participants Up to 10 participants per clinical trainer Up to 5 participants per clinical trainer<br />
Please note that while endometrial biopsy is an indication for MVA, specific training on endometrial biopsy is not a part of these course models.<br />
4 ·UTERINE EVACUATION WITH MANUAL VACUUM ASPIRATION (MVA): A TRAINING MANUAL FOR CONDUCTING SHORT COURSES
Ipas policy/guidelines on clinical training<br />
<strong>with</strong> live patients<br />
Promoting quality care for women is a top Ipas priority. To that end, participants<br />
in course 301 (Supervised Clinical Practice of MVA) must have completed course<br />
201. Clinical trainers and participants in course 301 must meet all professional<br />
requirements of the facility where supervised clinical practice is offered.<br />
Options for Delivering Courses<br />
These short courses offer training facilitators and participants great flexibility in<br />
finding the course and schedule that best meets participants’ needs and available<br />
time. For example:<br />
Courses offered separately<br />
First ___ day of the month Course 101<br />
Monthly, or occasionally to meet demand Course 201<br />
Monthly, or occasionally to meet demand Course 301<br />
Or, courses offered as a series<br />
Example 1: Courses offered on closely-scheduled days<br />
Tuesday Evening Course 101<br />
Thursday Evening Course 201<br />
Saturday all day Course 301<br />
Example 2: Courses offered on two successive days<br />
Friday Morning Course 101<br />
Friday Afternoon Course 201<br />
Saturday all day Course 301<br />
UTERINE EVACUATION WITH MANUAL VACUUM ASPIRATION (MVA): A TRAINING MANUAL FOR CONDUCTING SHORT COURSES · 5
The Trainers/Presenters<br />
The trainers/presenters for these courses should be clinicians skilled in uterine<br />
<strong>evacuation</strong> <strong>with</strong> MVA and capable of training on all elements in the courses.<br />
Ideally, clinical trainers will be a member of Ipas’s Global Trainers’ Network<br />
(GTN), a network for clinical trainers and organizations that provide sexual and<br />
reproductive health training. Ipas ensures that GTN trainers are able to:<br />
• Follow current clinical guidelines<br />
• Utilize Ipas clinical training curricula<br />
• Employ effective teaching methodologies based on adult learning principles<br />
• Serve as effective presenters and facilitators<br />
For information on how to find an Ipas GTN trainer in your area, please send an<br />
e-mail to training@ipas.org.<br />
For Course 301, depending on the number of participants and clinical practice<br />
volume, there may be concurrent sessions that require additional clinical trainers<br />
or local monitoring experts during a one-hour period.<br />
Ipas recommends that a representative from a local MVA distributor also serve as<br />
a trainer/presenter at these courses. It is important that participants know where<br />
they can procure a sustainable supply of instruments following completion of<br />
a course.<br />
The Materials<br />
This <strong>manual</strong> and accompanying CD-ROM includes all the information and<br />
tools necessary to plan and implement Course 101, Course 201 and Course 301,<br />
including:<br />
• Course overviews for instructors<br />
• Participant agendas<br />
• Materials checklists <strong>with</strong> links to learning and instructional aids<br />
• Planning checklists<br />
• Learning assessments <strong>with</strong> answer keys<br />
• Evaluation forms<br />
• Certificates for course completion<br />
• Information on MVA instruments and local availability<br />
Please note that the CD-ROM also contains all of the PowerPoint® course slide<br />
sets. The slides are not reproduced in this <strong>manual</strong>.<br />
The detailed course overviews include the number of PowerPoint slides per topic<br />
and all suggested supporting materials and activities. For ease of presenter use,<br />
the entire course is in one slide deck. However, it is not all PowerPoint-based.<br />
Place-holder slides for interactive and hands-on activities are included <strong>with</strong><br />
instructions. There are also “test your knowledge” question slides at the end<br />
of certain topics. Please note that correct answers for all “test your knowledge”<br />
slides are in the Speaker’s Notes. All trainers/presenters should plan to review<br />
the correct answers before presenting the test questions to audiences. Should<br />
6 ·UTERINE EVACUATION WITH MANUAL VACUUM ASPIRATION (MVA): A TRAINING MANUAL FOR CONDUCTING SHORT COURSES
the trainer/presenter not wish to include the “test your knowledge” slides<br />
in the educational session, the slides can be hidden or deleted. All slides can<br />
be re-ordered, and the interactive slides can be interspersed throughout the<br />
presentation, rather than reviewing them at the end of a topic. Ipas wants to<br />
ensure maximum flexibility for each individual presenter’s preferred style and<br />
comfort level, while maintaining standard content.<br />
Additional resources that can be used in a blended learning<br />
approach<br />
With the goal of maximizing the time of learners and trainers,<br />
Ipas recommends the following tools that can be used as distance<br />
learning, job aids or supplemental learning for participants and<br />
trainers. Specifically, documented completion of selected courses from<br />
IpasUniversity can serve as a prerequisite to Course 201.<br />
IpasUniversity (www.IpasU.org)<br />
IpasU is a self-paced Internet learning site for reproductive health-care<br />
providers <strong>with</strong> a focus on safe abortion care and postabortion care. IpasU<br />
offers free courses for both clinicians (already in practice and those still<br />
in-training) as well as those who work <strong>with</strong> developing world clinicians.<br />
At present, IpasU courses are available in English only.<br />
Other Ipas curricula (online and in print)<br />
Ipas is a global leader in reproductive health training. Our<br />
performance-based Woman-Centered Abortion Care and Woman-<br />
Centered Postabortion Care courses are known for their participatory,<br />
experiential learning methods, based on principles of adult learning and<br />
empowerment education. These courses are normally offered as part<br />
of a larger in-service training program. Trainers and reference <strong>manual</strong>s<br />
are available on www.ipas.org/publications (use search term “womancentered”).<br />
Access to the Global Trainers’ Network (GTN)<br />
Participants who successfully complete any of the three courses outlined<br />
in this <strong>manual</strong> may be interested in working <strong>with</strong> an experienced Ipas<br />
trainer from the Global Trainers’ Network to build and strengthen their<br />
skills in providing MVA care, or expand their knowledge of the Woman-<br />
Centered approach. For more information please send an email to:<br />
training@ipas.org<br />
MVA Calculator (www.mvacalculator.org)<br />
Use the free online MVA Calculator to estimate facility supply needs for<br />
MVA at www.mvacalculator.org<br />
UTERINE EVACUATION WITH MANUAL VACUUM ASPIRATION (MVA): A TRAINING MANUAL FOR CONDUCTING SHORT COURSES · 7
References<br />
Center for Reproductive Policy and Law. 2007. The World’s Abortion Laws. New<br />
York: CRR.(http://reproductiverights.org)<br />
Dalton, Vanessa, Lisa Harris, Carol Weisman, Ken Guire, Laura Castleman, Dan<br />
Lebovic. 2006. Patient Preferences, Satisfaction, and Resource Use in Office<br />
Evacuation of Early Pregnancy Failure. Obstetric Gynecology 108(1): 103-10.<br />
World Health Organization. 2007. Unsafe abortion: Global and regional estimates of<br />
the incidence of unsafe abortion and associated mortality in 2003. Geneva: WHO.<br />
World Health Organization and UNFPA. 2003. Essential drugs and other<br />
commodities for reproductive health services. Draft discussion document. Geneva:<br />
WHO.<br />
World Health Organization. 2003. Safe abortion: technical and policy guidance for<br />
health systems. Geneva: WHO.<br />
Tools<br />
Course 101: Introduction to MVA<br />
1. Course overview for trainers/presenters<br />
2. Sample participant agenda<br />
3. Recommended materials checklist (<strong>with</strong> pdfs or links to all materials)<br />
4. Sample planning checklist<br />
5. Sample course evaluation tool<br />
6. Sample certificate for course completion<br />
7. Information on MVA instruments and local availability (sample template)<br />
Course 201: Pelvic Model Practice <strong>with</strong> MVA<br />
1. Course overview for trainers/presenters<br />
2. Sample participant agenda<br />
3. Recommended materials checklist (<strong>with</strong> pdfs or links to all materials)<br />
4. Sample planning checklist<br />
5. Guidance on set up and training <strong>with</strong> pelvic models<br />
6. MVA Procedures Checklist<br />
7. Sample learning assessment tool (tests & answer keys)<br />
8. Sample course evaluation tool<br />
9. Sample certificate for course completion<br />
10. Information on MVA instruments and local availability (sample template)<br />
8 ·UTERINE EVACUATION WITH MANUAL VACUUM ASPIRATION (MVA): A TRAINING MANUAL FOR CONDUCTING SHORT COURSES
MVA Course 301: Supervised Clinical Practice <strong>with</strong> MVA<br />
1. Course overviews for trainers/presenters<br />
2. Sample participant agenda<br />
3. Recommended materials checklist (<strong>with</strong> pdfs or links to all materials)<br />
4. Sample planning checklist<br />
5. Guidance on setting up and running clinical practicum<br />
6. MVA Procedures Checklist<br />
7. Sample learning assessment tool<br />
8. Sample course evaluation tool<br />
9. Sample certificate for course completion<br />
10. Information on MVA instruments and local availability (sample template)<br />
UTERINE EVACUATION WITH MANUAL VACUUM ASPIRATION (MVA): A TRAINING MANUAL FOR CONDUCTING SHORT COURSES · 9
10 ·UTERINE EVACUATION WITH MANUAL VACUUM ASPIRATION (MVA): A TRAINING MANUAL FOR CONDUCTING SHORT COURSES
Tools
Tools<br />
1) The materials printed in this <strong>manual</strong> are for the uterine <strong>evacuation</strong> practice environment of incomplete and/ or<br />
missed abortion. The accompanying CD-ROM contains the materials for all indications and both regulatory<br />
settings (single use and multiple use of cannulae).<br />
2) These tools and accompanying PowerPoint slides may be adapted for specific training circumstances, only to<br />
the extent that the content is NOT altered. For example, if the same group of participants takes all three<br />
courses, certain review sections and accompanying slides in MVA 201 and MVA 301 can be deleted to avoid<br />
redundancy, and the timeframes on the agenda can be altered, as necessary. Additional location-specific<br />
information may be inserted, as well.<br />
A) MVA Course 101<br />
1. Course overview for trainers/presenters<br />
2. Sample participant agenda<br />
3. Recommended materials checklist (<strong>with</strong> pdfs or links to all materials)<br />
4. Sample planning checklist<br />
5. Sample course evaluation tool<br />
6. Sample certificate for course completion<br />
7. Information on MVA instruments and local availability (sample template)<br />
B) MVA Course 201<br />
1. Course overview for trainers/presenters<br />
2. Sample participant agenda<br />
3. Recommended materials checklist (<strong>with</strong> pdfs or links to all materials)<br />
4. Sample planning checklist<br />
5. Guidance on set up and training <strong>with</strong> pelvic models<br />
6. MVA Procedures Checklist<br />
7. Sample learning assessment tool (tests & answer keys)<br />
8. Sample course evaluation tool<br />
9. Sample certificate for course completion<br />
10. Information on MVA instruments and local availability (sample template)<br />
C) MVA Course 301<br />
1. Course overviews for trainers/presenters<br />
2. Sample participant agenda<br />
3. Recommended materials checklist (<strong>with</strong> pdfs or links to all materials)<br />
4. Sample planning checklist<br />
5. Guidance on setting up and running clinical practicum<br />
6. MVA Procedures Checklist<br />
7. Sample learning assessment tool (tests & answer keys)<br />
8. Sample course evaluation tool<br />
9. Sample certificate for course completion<br />
10. Information on MVA instruments and local availability (sample template)<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 1
Tool A-1:<br />
MVA 101 Course Overview (Context: Incomplete/Missed Abortion) --<br />
Approximately Three Hours<br />
INSTRUCTIONS: Use this Course Overview tool to study the topics, suggested timeframes and supporting<br />
slides/materials/activities for the course. Plan and adjust the agenda (separate tool) accordingly.<br />
Presentation Topic ~ # Slides Suggested Materials Suggested<br />
Length<br />
Welcome & Introductions 8 slides Informational Flyers (Ipas MVA 10 minutes<br />
Plus®, Ipas EasyGrip®, 3mm<br />
cannula, Ipas mission)<br />
Statistics 5 slides 10 minutes<br />
UE Methodologies Review<br />
and Comparison<br />
INCOMPLETE/MISSED:<br />
17 slides<br />
30 minutes<br />
Ipas Product Overview<br />
9 slides<br />
30 minutes<br />
10 slides <strong>with</strong> test<br />
questions<br />
MVA Procedure<br />
44 slides<br />
6 slides <strong>with</strong> test<br />
questions to use<br />
interactively <strong>with</strong> course<br />
participants (correct<br />
answers are in speaker<br />
notes).<br />
MVA steps wall chart<br />
Performing MVA + Processing<br />
Bifold<br />
Performing UE spiral notebook<br />
CD-ROMS: 6 min MVA<br />
technique using the Ipas MVA<br />
Plus or Performing UE <strong>with</strong> MVA<br />
Plus<br />
45 minutes<br />
Stocking and Resupply of<br />
Instruments<br />
18 slides mvacalculator.org<br />
JSI Table<br />
Local Distributor contact<br />
information<br />
Course Close 1 slide Course Evaluation<br />
Certificates<br />
15 minutes<br />
15 minutes<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 2
Tool A-2:<br />
MVA 101 Sample Agenda for Participants<br />
INSTRUCTIONS: Adjust this Agenda accordingly and provide one for each participant at beginning of course.<br />
Time<br />
(adapt as necessary for<br />
local setting)<br />
(10 minutes)<br />
9:00 am – 9:10 am<br />
Topic<br />
Introduction<br />
Lead Presenter<br />
(include names, rather than roles, once<br />
presenters confirmed)<br />
Representative from Local Distributor &<br />
Clinical Trainer<br />
(10 minutes)<br />
9:10 am – 9:20 am<br />
Global and local context for MVA<br />
Clinical Trainer<br />
(30 minutes<br />
9:20 am – 9:50 am)<br />
(30 minutes)<br />
9:50 am – 10:20 am<br />
(15 minutes)<br />
10:20 am – 10:35 am<br />
(45 minutes)<br />
10:35 am – 11:20 am<br />
Review and comparison of uterine<br />
<strong>evacuation</strong> technologies<br />
Overview of MVA instrument<br />
Coffee/tea break<br />
MVA procedure overview<br />
Clinical Trainer<br />
Clinical Trainer<br />
Clinical Trainer<br />
(15 minutes)<br />
11:20 am – 11:35 am<br />
MVA stocking and resupply<br />
Local Distributor<br />
(15 minutes)<br />
11:35 am – 11:50 am<br />
Course close and evaluation<br />
Clinical Trainer & Local distributor<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 3
Tool A-3:<br />
MVA 101 Recommended Materials Checklist <strong>with</strong> Link to PDF:<br />
Course Context: Incomplete/Missed Abortion INSTRUCTIONS: Use this Materials Checklist as guidance to ensure<br />
all audiovisual equipment and printed materials are in place for training event.<br />
Recommended<br />
Quantity<br />
Quantity<br />
Ordered<br />
Status Item Link to pdf, where applicable<br />
1 Computer and LCD projector for<br />
powerpoint presentations<br />
1 per participant<br />
plus extras<br />
1 per participant<br />
plus extras<br />
1 per participant<br />
plus extras<br />
1 per participant<br />
plus extras<br />
1 per participant<br />
plus extras<br />
1 per participant<br />
plus extras<br />
1 per participant<br />
plus extras<br />
1 per participant<br />
plus extras<br />
1 per participant<br />
plus extras<br />
Participant Agenda<br />
Informational flyers (MVA Plus,<br />
EasyGrip, 3mm, mission)<br />
Contact information from local<br />
supplier/vendor of MVA, including JSI<br />
Table and link to<br />
www.mvacalculator.org<br />
Peforming <strong>Uterine</strong> Evacuation <strong>with</strong> the<br />
Ipas MVA Plus Aspirator and Ipas<br />
EasyGrip® Cannulae: Instructional<br />
booklet<br />
Performing <strong>Uterine</strong> Evacuation <strong>with</strong> Ipas<br />
MVA Plus and Ipas EasyGrip®<br />
Cannulae: Instructional CD-ROM OR<br />
CD-Rom of 6 minute video<br />
MVA steps wall chart<br />
Performing MVA + Processing Bifold<br />
List of on-line resources<br />
Certificates of participation and<br />
completion<br />
Plus Flyer 2007<br />
Easy Grip Flyer<br />
3 mm Flyer 2007<br />
Performing UE <strong>with</strong> Ipas MVA<br />
Plus<br />
MVA Procedure Steps Wallchart<br />
PAC MVA Steps and Processing<br />
www.IpasU.org<br />
www.mvacalculator.org<br />
www.ipas.org<br />
www.womancareglobal.com<br />
Tool A-9<br />
1 per participant<br />
plus extras<br />
Course evaluation tool Tool A-8<br />
1 per participant Ipas MVA Plus® aspirators and Ipas<br />
EasyGrip® cannulae<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 4
Tool A-4:<br />
MVA 101 Sample Planning Checklist<br />
INSTRUCTIONS: Use this Planning Checklist as guidance to ensure all necessary steps and planning details for<br />
setting up the training event are followed <strong>with</strong> enough time for completion.<br />
Target date Action Person<br />
responsible<br />
5-6 weeks prior to Secure venue for course<br />
course<br />
(training room <strong>with</strong> space for the number of participants and<br />
adequate seating arrangements for participatory learning and<br />
appropriate viewing of audiovisual materials)<br />
Status<br />
Ensure computer, projector, screen, audio will be available at<br />
venue<br />
Contract appropriate clinical trainer and product<br />
representative for course<br />
For full series of three courses: Ensure trainer has required<br />
credentials for clinical training/patient care<br />
Ensure participants will have MVA instruments for use<br />
during and after course and ensure resupply mechanism<br />
Ensure required learning aids and printed materials are<br />
ordered in appropriate numbers (see materials list for items<br />
and quantities)<br />
5 weeks prior Advertise, invite participants<br />
4 weeks prior Make any necessary travel arrangements and ensure travelers<br />
are aware of all details (including potential airport pick-up<br />
and hotel) and requirements for reimbursement for any<br />
expenses<br />
Monitoring plan: Plan for follow-up <strong>with</strong> each course<br />
participant<br />
2 weeks prior Finalize slidesets, have file and back-up file for projection;<br />
print any handouts for participants; check ordered learning<br />
aids and printed materials<br />
Reconfirm venue arrangements<br />
Reconfirm arrangements <strong>with</strong> clinical trainer and product<br />
representative (Local Distributor)<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 5
Tool A-5:<br />
MVA 101 Course Evaluation<br />
INSTRUCTIONS: Insert date and location at top of evaluation and delete instructions. Provide Course Evaluation to<br />
all participants at the end of the course and ask them to complete and turn in before leaving. Study the responses<br />
after the course, <strong>with</strong> the goal of using responses to improve and adapt the course for future offerings.<br />
MVA 101: Introduction to MVA Course Evaluation<br />
DATE:______________________________LOCATION:_________________________<br />
Course Objective:<br />
Be familiar <strong>with</strong> the Ipas MVA product line and know how to re-supply<br />
4 = strongly agree 3 = agree 2 = disagree 1 = strongly disagree<br />
Rating<br />
1. The course fulfilled its goal and objective (see above). ______<br />
Comments:<br />
2. The trainers were responsive to participants’ needs. ______<br />
Comments:<br />
3. Because of this course, I have a better understanding of the importance of MVA and how to use it.<br />
Comments:<br />
_______<br />
4. Now that I have completed this course, I feel (please circle the appropriate response):<br />
a. Ready to take the next two courses before offering care <strong>with</strong> MVA to women<br />
b. That this procedure is not one I would choose to provide<br />
c. Prepared to promote (but not provide) MVA services<br />
d. Other [please describe]<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 6
5. What suggestions can you offer to improve this course in the future?<br />
6. I came to this course <strong>with</strong> (please circle the appropriate response):<br />
a. No experience providing transvaginal procedures<br />
b. Less than three years clinical experience including transvaginal procedures<br />
c. Between three and five years of clinical experience including transvaginal procedures<br />
d. More than five years of clinical experience including transvaginal procedures<br />
7. My clinical background is:<br />
a. Professional midwife or nurse-midwife<br />
b. Other advance practice or midlevel clinician (physician’s assistant, clinical officer, professional<br />
nurse, etc)<br />
c. Medical doctor (non specialist)<br />
d. Ob-Gyn specialist<br />
e. Public Health (non practicing clinician)<br />
f. Other (please describe)<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 7
Tool A-6:<br />
MVA 101 Certificate Template<br />
(full page version on CD-ROM)<br />
INSTRUCTIONS: Add logos of sponsoring organizations, include names of trainers and date and print one copy of<br />
Certificate Template for each participant, customized <strong>with</strong> each individual participant name, and distribute to<br />
participants at the close of course.<br />
Insert logo of<br />
sponsor/host<br />
organization<br />
Introduction to<br />
Manual Vacuum Aspiration<br />
Course 101<br />
Add Logo of<br />
sponsoring<br />
Organization<br />
CERTIFICATE OF COMPLETION<br />
Awarded to<br />
____________________________________<br />
NAME<br />
________________________________<br />
PLACE<br />
________________________<br />
DATE<br />
Insert name of Clinical Trainer<br />
Insert name of Course Sponsor<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 8
Tool A-7:<br />
Information on Instruments and Availability<br />
INSTRUCTIONS: Insert specific contact information of local MVA instruments supplier in template, delete<br />
instructions and print one copy for each course participant.<br />
[Name and contact information for MVA instruments supplier(s):]<br />
For information on planning and calculating instruments supply,<br />
see www.mvacalculator.org and/or use the following table:<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 9
B) MVA Course 201<br />
The materials printed in this <strong>manual</strong> are for the uterine <strong>evacuation</strong> practice environment of incomplete<br />
and/ or missed abortion. The accompanying CD-ROM contains the materials for all indications and<br />
both regulatory settings (single use and multiple use of cannulae).<br />
Tool B-1:<br />
MVA 201 Course Overview (Contexts for samples for course 201:<br />
Incomplete/Missed Abortion; Multiple use) – Approximately Four Hours<br />
INSTRUCTIONS: Use this Course Overview tool to study the topics, suggested timeframes and supporting<br />
slides/materials/activities for the course. Plan and adjust the agenda (separate tool) accordingly. This<br />
Overview can be adapted depending on whether this course is offered immediately after course 101 or<br />
offered on its own <strong>with</strong>out 101 as an immediate precursor.<br />
Presentation Topic ~ # Slides Suggested<br />
Materials/Activities<br />
Suggested<br />
Length<br />
Welcome & Introductions<br />
Review of Content from MVA<br />
101<br />
14 slides Informational flyers (Ipas MVA<br />
Plus®, Ipas EasyGrip®, 3mm<br />
cannula, Ipas mission<br />
30 minutes<br />
Hands-on Practice<br />
18 slides<br />
44 slides<br />
MVA Procedures Checklist<br />
Practice <strong>with</strong> instrument<br />
disassembly and re-assembly<br />
Procedure demonstration and<br />
practice <strong>with</strong> pelvic model<br />
2-4 hours<br />
Instruments Processing<br />
33 slides<br />
Processing wall chart<br />
30 minutes<br />
16 slides <strong>with</strong> test<br />
questions<br />
Resupply of Instruments 39 slides mvacalculator.org<br />
JSI Table<br />
Local Distributor contact<br />
information<br />
30 minutes<br />
Learning Assessment 1 slide Administer learning assessment 15 minutes<br />
Course close (same as above) Administer course evaluation<br />
Give out certificates<br />
15 minutes<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 10
Tool B-2:<br />
MVA 201 Sample Agenda for Participants:<br />
INSTRUCTIONS: Adjust this agenda accordingly and provide one for each participant at beginning of course. This<br />
Agenda can be adapted depending on whether this course is offered immediately after course 101 or offered on its<br />
own <strong>with</strong>out 101 as an immediate precursor.<br />
Time<br />
(adapt as necessary<br />
for local setting)<br />
(30 minutes)<br />
1:00 – 1:30<br />
(120 minutes)<br />
1:30 pm – 3:30 pm<br />
(15 minutes)<br />
3:30 pm – 3:45 pm<br />
Topic<br />
Welcome, introductions, review of content<br />
from 101 (or IpasU equivalent)<br />
Demonstration and practice on pelvic model<br />
(Use skills assessment from procedure<br />
checklist)<br />
Coffee/Tea break<br />
Lead Presenter<br />
(include names, rather than roles, once<br />
presenters confirmed)<br />
Clinical Trainer and Representative from<br />
Local Product Distributor<br />
Clinical Trainer<br />
(30 minutes)<br />
3:45 pm – 4:15 pm<br />
MVA instruments processing<br />
Representative from Local Product<br />
Distributor<br />
(30 minutes)<br />
4:15 pm – 4:45 pm<br />
MVA stocking and resupply<br />
Representative from Local Product<br />
Distributor<br />
(15 minutes)<br />
4:45pm – 5:00 pm<br />
Learning assessment<br />
Clinical Trainer & Representative from Local<br />
Product Distributor<br />
(15 minutes)<br />
5:00 pm – 5:15 pm<br />
Course close<br />
Clinical Trainer & Representative from Local<br />
Product Distributor<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 11
Tool B-3:<br />
MVA 201 Sample Materials Checklist <strong>with</strong> Link to PDF<br />
INSTRUCTIONS: Use this Materials Checklist as guidance to ensure all audiovisual equipment, training aids,<br />
medical supplies and printed materials are in place for training event. This checklist should be adjusted, depending<br />
on whether this course is offered immediately after MVA 101 or offered on its own <strong>with</strong>out 101 beforehand<br />
(participants who just took MVA 101 will already have most of these materials).<br />
Recommended<br />
Quantity<br />
Quantity<br />
Ordered<br />
Status Item (Link to pdf)<br />
1 Computer and LCD projector for<br />
powerpoint presentations<br />
1 TRAINER TIPS FOR USE OF PELVIC<br />
MODELS FOR MVA CLINICAL<br />
TRAINING<br />
1 per participant<br />
Participant agenda<br />
plus extras<br />
Pelvic Model<br />
1 per participant<br />
plus extras<br />
1 per participant<br />
plus extras<br />
1 per participant<br />
plus extras<br />
1 per participant<br />
plus extras<br />
1 per participant<br />
plus extras<br />
Informational flyers (Ipas MVA<br />
Plus®, Ipas EasyGrip®, 3mm<br />
cannula, Ipas mission)<br />
Contact information from local<br />
supplier/vendor of MVA, including<br />
JSI Table and link to<br />
www.mvacalculator.org<br />
Peforming <strong>Uterine</strong> Evacuation <strong>with</strong><br />
the Ipas MVA Plus Aspirator and<br />
Ipas EasyGrip® Cannulae:<br />
Instructional booklet<br />
Performing <strong>Uterine</strong> Evacuation <strong>with</strong><br />
Ipas MVA Plus and Ipas<br />
EasyGrip® Cannulae: Instructional<br />
CD-ROM OR<br />
CD-Rom of 6 minute video<br />
MVA steps wall chart<br />
Plus Flyer 2007<br />
Easy Grip Flyer<br />
3 mm Flyer 2007<br />
Performing UE <strong>with</strong> Ipas<br />
MVA Plus<br />
MVA Procedure Steps<br />
Wallchart<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 12
1 per participant<br />
plus extras<br />
1 per participant<br />
plus extras<br />
1 per participant<br />
plus extras<br />
1 per participant<br />
plus extras<br />
Performing MVA + Processing<br />
Bifold<br />
Processing wall chart<br />
UE for incomplete and<br />
missed abortion :<br />
PAC MVA Steps and<br />
Processing<br />
MVA Processing Wallchart<br />
List of online resources:<br />
www.IpasU.org<br />
www.mvacalculator.org<br />
www.ipas.org<br />
www.womancareglobal.com<br />
Procedure checklists Tool B-6<br />
1 per participant<br />
plus extras<br />
Certificates of participation and<br />
completion<br />
Tool B-9<br />
1 per participant<br />
plus extras<br />
1 per participant<br />
plus extras<br />
1 for every 2<br />
participants<br />
Learning assessment tool Tool B-7<br />
Course evaluation tool Tool B-8<br />
Pelvic models<br />
1 for each<br />
participant or for<br />
each pelvic model<br />
1 for each pelvic<br />
model<br />
Ipas MVA Plus® aspirators and<br />
Ipas EasyGrip® cannulae (for each<br />
participant or for each pelvic<br />
model)<br />
One speculum, tenaculum and<br />
injection syringe per pelvic model<br />
Drape for each pelvic model (when<br />
not in use)<br />
1 for each pelvic<br />
model<br />
Buckets and supplies for<br />
demonstrating instrument<br />
processing (include solution for<br />
decontamination soak, locally<br />
available products for high-level<br />
disinfection (HLD) or sterilization,<br />
including wrappers for autoclave.)<br />
1 set Samples of locally available<br />
contraceptives and pain medications<br />
(optional)<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 13
Tool B-4<br />
MVA 201 Sample Planning Checklist<br />
INSTRUCTIONS: Use this Planning Checklist as guidance to ensure all necessary steps and planning details for<br />
setting up training event are followed <strong>with</strong> enough time for completion.<br />
Target date Action Person<br />
responsible<br />
5-6 weeks prior to Secure venue for course<br />
course<br />
(training room <strong>with</strong> space for the number of participants and<br />
adequate seating arrangements for participatory learning and<br />
appropriate viewing of audiovisual materials)<br />
Status<br />
Ensure computer, projector, screen, audio will be available at<br />
venue<br />
Contract appropriate clinical trainer and product<br />
representative for course<br />
Ensure participants will have MVA instruments for use<br />
during and after course and ensure resupply mechanism<br />
Ensure required learning aids and printed materials are<br />
ordered in appropriate numbers (see materials checklist for<br />
items and quantities)<br />
NOTE: Be sure to include pelvic models, procedural supplies<br />
and instruments processing supplies, as shown on materials<br />
checklist<br />
5 weeks prior Advertise, invite participants<br />
4 weeks prior Make any necessary travel arrangements and ensure travelers<br />
are aware of all details (including potential airport pick-up<br />
and hotel) and requirements for reimbursement for any<br />
expenses<br />
Monitoring plan: Plan for follow-up <strong>with</strong> each course<br />
participant<br />
2 weeks prior Finalize slidesets, have file and back-up file for projection;<br />
print any handouts for participants; check ordered learning<br />
aids and printed materials<br />
Reconfirm venue arrangements<br />
Reconfirm arrangements <strong>with</strong> clinical trainer and product<br />
representative<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 14
Tool B-5:<br />
MVA 201: Guidance for Setting Up and Training <strong>with</strong> Pelvic Models<br />
INSTRUCTIONS: The enclosed CD-ROM includes a 4-page guide on preparing for and training <strong>with</strong> pelvic<br />
models. Facilitators should use the guide to ensure that all components of pelvic model training are in place prior to<br />
a course. Trainers and presenters should review it in advance of course for specific suggestions on pelvic model<br />
training.<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 15
Tool B-6:<br />
MVA Procedure Checklist: Incomplete/Missed Abortion<br />
INSTRUCTIONS: Provide a copy to each participant for use during training on pelvic models.<br />
Skills Yes No Comments<br />
Creates pain management plan<br />
Tailors pain management plan <strong>with</strong> woman according to her needs<br />
Discusses sources of pain, options, potential side effects<br />
Includes combination of support and pharmacological measures<br />
Takes into account woman’s medical and psychological status, dilatation<br />
necessary, staff skill, nature of procedure and availability of supplies<br />
Prepares the instruments<br />
Checks <strong>vacuum</strong> retention of aspirator<br />
Has more than one instrument available<br />
Prepares the woman<br />
Administers pain medication in timely fashion<br />
Asks woman to empty her bladder<br />
Asks what supportive measures she would like and provides them<br />
Asks for permission to start<br />
Puts on barriers and washes hands<br />
Performs pelvic exam to confirm assessment findings<br />
Warms and inserts speculum gently<br />
Removes foreign bodies in os; refers if bowel present<br />
Performs cervical antiseptic prep<br />
Follows No-Touch Technique<br />
Uses antiseptic sponges to clean os and, if desired, vagina<br />
Administers paracervical block<br />
Uses less than 200mg lidocaine<br />
Aspirates before injecting 1–2mL at tenaculum site<br />
Places tenaculum<br />
Applies slight traction to expose tissue transition<br />
Slowly injects 2–5mL lidocaine to 1–1.5 inches at 3,5,7 and 9 o’clock<br />
Dilates cervix if needed<br />
Inserts cannula<br />
Applies gentle traction to cervix<br />
Rotates cannula while gently applying pressure<br />
Inserts cannula to just past internal os OR to fundus and pulls back<br />
Suctions uterine contents<br />
Holds tenaculum and end of cannula in one hand<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 16
Attaches charged aspirator<br />
Releases buttons to start <strong>vacuum</strong><br />
Rotates cannula 180 degrees each direction<br />
Uses an ―in and out‖ motion<br />
Does not <strong>with</strong>draw aperture beyond os<br />
Uses gentle operative technique<br />
Uses positive, respectful, supportive reassurance<br />
Stops when pink foam <strong>with</strong>out tissue passes, gritty sensation is felt, uterus<br />
contracts around cannula and uterine cramping increases<br />
Removes the instrument<br />
Is ready to evacuate again after inspecting tissue if needed<br />
Inspects tissue<br />
Empties aspirator into container<br />
Looks for products of conception (POC)<br />
Evaluates amount based on estimated gestation<br />
Determines all POC have been removed<br />
Completes remaining steps:<br />
Wipes cervix to assess bleeding<br />
Considers if pelvic exam is advisable<br />
Reassures woman that procedure is finished<br />
Performs post-procedure care<br />
Processes instruments<br />
Removes barriers and washes hands<br />
Ensures woman is escorted to recovery area<br />
Resolves technical problems that arise<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 17
Tool B-7:<br />
MVA 201 Sample Learning Assessment Tool (test & answer key)<br />
(Note that the CD-ROM contains a version for participants, that does not indicate correct answers)<br />
INSTRUCTIONS: Select the appropriate learning assessment and make one copy for each participant and<br />
administer at end of course to all participants. Review answers <strong>with</strong> all participants after they have completed test.<br />
This test is appropriate for all four course versions (<strong>with</strong> answer on #10 different for Multiple Use versus Re-Use)<br />
Learning Assessment: MVA 201 (Pelvic Model Practice <strong>with</strong> MVA)<br />
Name: ____________________________________ Date: ______________________<br />
1. The steps of processing include which of the following?<br />
a) Decontamination soak<br />
b) Cleaning<br />
c) High-level disinfection (HLD) or sterilization<br />
d) Storage<br />
e) All of the above [correct]<br />
2. Following an MVA procedure, all instruments that will be reused should be<br />
a) Kept wet until they can be cleaned [correct]<br />
b) Kept dry until they can be cleaned<br />
c) Kept in an air-tight storage device<br />
d) Immediately sterilized<br />
3. Which of the following methods is NOT acceptable for processing Ipas MVA Plus® aspirators?<br />
b) Sterrad Processor<br />
c) HLD <strong>with</strong> chemicals<br />
d) Dry heat [correct]<br />
e) Steam Sterilization<br />
4. Active Stock of MVA is<br />
a. New devices, in original packaging, in the facility store room<br />
b. The devices kept in the procedure room to serve women needing MVA in any given day or shift<br />
[correct]<br />
c. The devices in the central warehouse to send to facilities when requisitioned<br />
d. The devices the chief health practicioner keeps at her private practice to serve her patients<br />
5. The primary goal of forecasting MVA needs for health-care facilities is:<br />
a) To reduce the length of time between ordering and receiving new MVA aspirators<br />
b) To reduce the number of women whose health and lives are at risk when providers lack MVA<br />
when needed [correct]<br />
c) To increase the number of providers trained and equipped to offer care <strong>with</strong> MVA<br />
d) To help provide program information for potential donors<br />
6. When a clinic storeroom reaches the reorder point quantity for MVA devices, how many should be<br />
reordered?<br />
a. The Total Initial Stock<br />
b. The Reserve Maximum minus the reorder point quantity [correct]<br />
c. The Active Stock plus the Reserve Stock quantities<br />
d. The Reserve Maximum<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 18
7. You are planning MVA needs for a small hospital, open 24 hours per day. Based on your facility’s past<br />
experience, you project that you will provide MVA care to an average of 70 women each month. Use the<br />
MVA Initial Supply and Resupply table to determine how many aspirators should be available in the active<br />
inventory:<br />
a) 2<br />
b) 4<br />
c) 6 [correct]<br />
d) 8<br />
8. For that same facility that serves 70 women per month <strong>with</strong> MVA, what is the maximum number of<br />
aspirators that should be held in reserve, unused in the facility storeroom?<br />
a) 2<br />
b) 7 [correct]<br />
c) 13<br />
d) 29<br />
9. The steps for preparing the instrument and checking <strong>vacuum</strong> retention are out of order below. Please order<br />
the steps correctly by numbering them 1-5.<br />
a) Pull the plunger straight back until the plunger arms snap outward and catch on the cylinder base<br />
[2]<br />
b) Let the aspirator sit for several minutes [3]<br />
c) Push the valve buttons to release the <strong>vacuum</strong> [4]<br />
d) Listen for a rush of air into the <strong>vacuum</strong>, indicating that the <strong>vacuum</strong> has been retained [5]<br />
e) Push both valve buttons down and forward at the same time until they lock into place [1]<br />
10. Ipas EasyGrip® cannulae (select all that apply)<br />
[ANSWER CHANGES DEPENDING ON REGULATORY CONTEXT: C FOR REUSE, C and D FOR<br />
SINGLE USE]<br />
a) Can be used after cleaning<br />
b) Cannot be autoclaved or boiled<br />
c) Must be HLD or sterile before entering the sterile uterus [correct]<br />
d) Cannot be reused [correct for SINGLE USE regulatory context)<br />
11. Put the 10 steps of the procedure in order :<br />
a) Process instruments [10]<br />
b) Aspirate tissue [7]<br />
c) Prepare instruments [1]<br />
d) Prepare the woman [2]<br />
e) Prepare the cervix [3]<br />
f) Insert Cannula [6]<br />
g) Dilate cervix [5]<br />
h) Perform any concurrent procedures [9]<br />
i) Perform paracervical block [4]<br />
j) Inspect tissue [8]<br />
12. The recommended cannula sizes for a woman seeking uterine <strong>evacuation</strong> for an 8 week LMP procedure,<br />
<strong>with</strong> a closed cervix is<br />
a) 4 mm-5mm<br />
b) 6 mm-8mm<br />
c) 7mm – 9 mm [correct]<br />
d) 10mm or 12 mm<br />
e) TBD<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 19
13. Paracervical block by itself is necessary and sufficient pain management for most women undergoing<br />
MVA:<br />
a) True<br />
b) False [correct]<br />
14. Pain management for an MVA procedure can include<br />
a) Conscious sedation<br />
b) Paracervical block<br />
c) Anxiolitics<br />
d) Analgesics<br />
e) Any one or more of the above [correct]<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 20
Tool B-8:<br />
MVA 201 Course Evaluation<br />
INSTRUCTIONS: Insert date and location at top of evaluation and delete these instructions. Provide<br />
Course Evaluation for each participant at the end of the course and ask them to complete and turn in<br />
before leaving. Study the responses after the course, <strong>with</strong> the goal of using responses to improve and<br />
adapt the course for future offerings.<br />
MVA 201 Course Evaluation<br />
DATE:_____________________________ LOCATION:_________________________<br />
Course Objectives:<br />
• Be able to simulate procedure on a pelvic model.<br />
• Be able to process MVA instruments in accordance <strong>with</strong> local regulations and <strong>with</strong> locally available<br />
products/systems<br />
4 = strongly agree 3 = agree 2 = disagree 1 = strongly disagree<br />
Rating<br />
1. The course fulfilled its goal and objectives (see above). ______<br />
Comments:<br />
2. The trainers were responsive to participants’ needs. ______<br />
Comments:<br />
3. Because of this course, I have a better understanding of how to use MVA. ______<br />
Comments:<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 21
4. Now that I have completed this course, I feel<br />
a. Ready to offer care to women <strong>with</strong> MVA<br />
b. Ready to take the next course, before offering care <strong>with</strong> MVA to women<br />
c. That this procedure is not one I would choose to provide<br />
d. Prepared to promote (but not provide) MVA services<br />
e. Other [please describe]<br />
5. What suggestions can you offer to improve this course in the future?<br />
6. I came to this course <strong>with</strong><br />
a. No experience providing transvaginal procedures<br />
b. Less than three years clinical experience including transvaginal procedures<br />
c. Between three and five years of clinical experience including transvaginal procedures<br />
d. More than five years of clinical experience including transvaginal procedures<br />
7. My clinical background is as:<br />
a. Professional midwife or nurse-midwife<br />
b. Other advance practice or midlevel clinician (physician’s assistant, clinical officer, professional<br />
nurse, etc)<br />
c. Medical doctor (non specialist)<br />
d. Ob-Gyn specialists<br />
e. Public Health (non practicing clinician)<br />
f. Other (please describe)<br />
8. As a pre-requisite for this course, I took:<br />
a) MVA 101<br />
b) Equivalent IpasUniversity courses<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 22
Tool B-9:<br />
MVA 201 Certificate Template<br />
(full page version on CD-ROM)<br />
INSTRUCTIONS: Insert logos and names of trainer and sponsor. Print one copy of Certificate Template<br />
for each participant, customized <strong>with</strong> each individual participant name, and distribute at the close of<br />
course.<br />
Insert logo of<br />
sponsor/host<br />
organization<br />
Pelvic Model Practice <strong>with</strong><br />
Manual Vacuum Aspiration<br />
Course 201<br />
Add Logo of<br />
sponsoring<br />
Organization<br />
CERTIFICATE OF COMPLETION<br />
Awarded to<br />
____________________________________<br />
NAME<br />
________________________________<br />
PLACE<br />
___________________________<br />
DATE<br />
Insert name of Clinical Trainer<br />
Insert name of Course Sponsor<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 23
Tool B-10:<br />
Information on Instruments and Availability<br />
INSTRUCTIONS: Insert specific contact information of local MVA instruments supplier in template, delete<br />
instructions and print one copy for each participant in course. There is only one version of this template.<br />
Contact information for MVA instruments supplier(s):<br />
For information on planning and calculating instruments supply,<br />
see www.mvacalculator.org and/or use the following table:<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 24
MVA Course 301<br />
Tool C-1:<br />
MVA 301 Course Overview – Approximately six to eight hours<br />
(context: incomplete/missed abortion; reuse)<br />
INSTRUCTIONS: Use this Course Overview tool to study the topics, suggested timeframes and supporting<br />
slides/materials/activities for the course. Plan and adjust the agenda (separate tool) accordingly. This Overview<br />
can be adapted depending on whether this course is offered immediately after MVA 101 and 201 or offered<br />
separately.<br />
Presentation Topic ~ # Slides Suggested<br />
Materials/Activities<br />
Suggested Length<br />
Welcome & Introduction<br />
Review MVA 101 201 content<br />
20 slides Highlight procedure, including<br />
pain management and postprocedure<br />
care<br />
30 minutes<br />
Follow-Up Care 9 slides 10 minutes<br />
Orientation to clinical practicum and<br />
other rotations<br />
1 slide Discussion and orientation to<br />
practicum and rotation to other<br />
topics<br />
20 minutes<br />
Clinical practicum rotation<br />
Monitoring to Improve Services<br />
rotation<br />
Management of Complications<br />
rotation<br />
Procedure checklist<br />
Clinical skill evaluation<br />
checklist<br />
60 - 90 minutes (concurrent<br />
<strong>with</strong> two other rotations)<br />
15 slides 60 - 90 minutes (concurrent<br />
<strong>with</strong> practicum)<br />
38 slides 60- 90 minutes (concurrent<br />
<strong>with</strong> practicum)<br />
Resupply of Instruments 18 slides Mvacalculator.org<br />
JSI Table<br />
Local Distributor contact<br />
information<br />
Learning assessment 1 slide Administer learning assessment<br />
Review clinical skill evaluation<br />
<strong>with</strong> individual participants (if<br />
not completed during clinical<br />
practicum)<br />
Course Close (same as above) Administer course evaluation<br />
Distribute certificates<br />
15 minutes<br />
30 minutes<br />
15 minutes<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 25
Tool C-2:<br />
MVA 301 Sample Agenda for Participants<br />
INSTRUCTIONS: Adjust this Agenda and provide one for each participant at beginning<br />
of course. This agenda can be adapted depending on whether this course is offered<br />
immediately after MVA 101 and 201 or offered separately.<br />
Time<br />
(adapt as necessary for<br />
local setting)<br />
(30 minutes)<br />
8:30 – 9:00<br />
(10 minutes)<br />
9:00 – 9:10<br />
(20 minutes)<br />
9:10 – 9:30<br />
(180 – 270 minutes)<br />
9:30 – 1:00<br />
Topic<br />
Welcome, introductions, review of content<br />
from MVA 101 and 201<br />
Follow-up care<br />
Orientation to clinical practicum and rotations<br />
through classroom topics<br />
Three Concurrent Sessions, <strong>with</strong> rotations<br />
through each:<br />
Lead Presenter<br />
(include names, rather than roles)<br />
Clinical Trainer & Representative local<br />
Distributor<br />
Clinical Trainer<br />
Clinical Trainer<br />
1. Clinical practicum Clinical Trainer<br />
2. Monitoring of services Clinical Trainer B<br />
3. Management of complications Clinical Trainer C<br />
(60 minutes)<br />
1:00 – 2:00<br />
(15 minutes)<br />
2:00 – 2:15<br />
(30 minutes)<br />
2:15 – 2:45<br />
(15 minutes)<br />
2:45 – 3:00<br />
Meal break<br />
MVA stocking and resupply<br />
Learning assessment<br />
Course close<br />
Representative from Local Distributor &<br />
Clinical Trainer<br />
Clinical Trainer<br />
Clinical Trainer & Representative from<br />
Local Distributor<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 26
Tool C-3:<br />
MVA 301 Recommended Materials Checklist <strong>with</strong> Link to PDF<br />
INSTRUCTIONS: Use this Materials Checklist as guidance to ensure all audiovisual equipment, training aids,<br />
medical supplies and printed materials are in place for training event. The Materials Checklist should be adjusted,<br />
depending on whether this course is offered immediately after MVA 101 and 201 (participants who just took 101<br />
and 102 will already have most of these materials).<br />
Recommended<br />
Quantity<br />
Quantity<br />
Ordered<br />
Status Item (link to pdf)<br />
2 Computer and LCD projector for<br />
powerpoint presentations (need two<br />
for concurrent rotation modules)<br />
1 per participant<br />
plus extras<br />
1 per participant<br />
plus extras<br />
1 per participant<br />
plus extras<br />
1 per participant<br />
plus extras<br />
1 per participant<br />
plus extras<br />
1 per participant<br />
plus extras<br />
1 per participant<br />
plus extras<br />
1 per participant<br />
plus extras<br />
1 per participant<br />
plus extras<br />
1 per participant<br />
plus extras<br />
Participant agenda<br />
Informational flyers (Ipas MVA<br />
Plus, Ipas EasyGrip, 3mm cannula,<br />
mission)<br />
Contact information from local<br />
supplier/vendor of MVA, including<br />
JSI Table and link to<br />
www.mvacalculator.org<br />
Peforming <strong>Uterine</strong> Evacuation <strong>with</strong><br />
the Ipas MVA Plus Aspirator and<br />
Ipas EasyGrip® Cannulae:<br />
Instructional booklet<br />
Performing <strong>Uterine</strong> Evacuation <strong>with</strong><br />
Ipas MVA Plus and Ipas<br />
EasyGrip® Cannulae: Instructional<br />
CD-ROM OR<br />
CD-Rom of 6 minute video<br />
MVA steps wall chart<br />
Performing MVA + Processing<br />
Bifold<br />
Processing wall chart<br />
Article: ―Manual <strong>vacuum</strong> <strong>aspiration</strong><br />
for uterine <strong>evacuation</strong>: Pain<br />
management‖<br />
List of on-line resources<br />
Plus Flyer 2007<br />
EasyGrip Flyer<br />
3mm Flyer 2007<br />
Performing UE <strong>with</strong> Ipas<br />
MVA Plus<br />
MVA Procedure Steps<br />
Wallchart<br />
PAC MVA Steps and<br />
Processing<br />
MVA Processing Wallchart<br />
Pain Management MVA-<br />
2009<br />
www.IpasU.org<br />
www.mvacalculator.org<br />
www.ipas.org<br />
www.womancareglobal.com<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 27
1 per participant<br />
plus extras<br />
Procedure Checklists Tool C-6<br />
1 per participant<br />
plus extras<br />
Learning assessment tool (includes<br />
clinical skill evaluation)<br />
Tool C-7<br />
1 per participant<br />
plus extras<br />
Course evaluation tool Tool C-8<br />
1 per participant<br />
plus extras<br />
1 for each<br />
participant<br />
Certificates of participation and<br />
completion<br />
Ipas MVA Plus® aspirators and<br />
Ipas EasyGrip® cannulae<br />
Tool C-9<br />
1 set Samples of locally available<br />
contraceptives and pain medications<br />
(optional)<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 28
Tool C-4<br />
MVA 301 Sample Planning Checklist<br />
INSTRUCTIONS: Use this Planning Checklist as guidance to ensure all necessary steps and planning details for<br />
setting up training event are followed <strong>with</strong> enough time for completion.<br />
Target date Action Person<br />
responsible<br />
5-6 weeks prior to Secure venue for course<br />
course<br />
(Training room <strong>with</strong> space for the number of participants and<br />
adequate seating arrangements for participatory learning and<br />
appropriate viewing of audiovisual materials.)<br />
NOTE: During course rotations, two training rooms are<br />
required for concurrent sessions, in addition to the separate<br />
clinical training venue.<br />
Status<br />
Ensure computers, projectors, screens, audio will be available<br />
at venue<br />
Secure venue for clinical training where:<br />
Trainer can provide clinical care, and<br />
Participants from outside the facility are able to provide<br />
patient care in training context.<br />
Coordinate <strong>with</strong> facility staff to ensure that both: Women<br />
are cared for in a timely way<br />
Clinical training needs for participants are met. (Course<br />
participants should demonstrate knowledge and skills on<br />
pelvic model before offering clinical care.)<br />
Contract appropriate clinical trainers and representative from<br />
Local Distributor for course<br />
There is a 3-to-4 hour block of time <strong>with</strong> concurrent sessions<br />
that requires three clinical trainers:<br />
Supervised Clinical Practicum<br />
Management of Complications<br />
Monitoring Services (could be a monitoring expert<br />
who is very familiar <strong>with</strong> MVA services, but not a<br />
clinician)<br />
Ensure clinical trainer has all required credentials for clinical<br />
training/patient care at the facility where clinical practicum<br />
will take place.<br />
Ensure participants will have MVA instruments for use<br />
during and after course and ensure resupply mechanism<br />
Ensure required learning aids and printed materials are<br />
ordered in appropriate numbers (see materials checklist for<br />
items and quantities)<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 29
5 weeks prior Advertise, invite participants<br />
4 weeks prior Make any necessary travel arrangements and ensure travelers<br />
are aware of all details (including potential airport pick-up<br />
and hotel) and requirements for reimbursement for any<br />
expenses<br />
Monitoring plan: Plan for follow-up <strong>with</strong> each course<br />
participant<br />
2 weeks prior Finalize slidesets, have file and back-up file for projection;<br />
print any handouts for participants; check ordered learning<br />
aids and printed materials<br />
Reconfirm venue arrangements, including reconfirmation<br />
<strong>with</strong> clinical facility<br />
Reconfirm arrangements <strong>with</strong> clinical trainers and<br />
representative from Local Distributor<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 30
Tool C-5:<br />
MVA 301: Guidance on Setting Up and Running Clinical Practicum<br />
INSTRUCTIONS: Use this guide for facilitators to ensure that all components of running a clinical practicum are in<br />
place and for trainers/presenters to study in advance of practicum for specific guidance and suggestions on planning<br />
and conducting a clinical practicum. There is only one version of this guidance tool.<br />
Advance Preparation<br />
❑ Ensure that all learners have reached competency in simulated skills practice prior to<br />
partaking in the clinical practicum.<br />
❑ Obtain approval for site(s) used for training.<br />
❑ Plan the design of the practicum.<br />
❑ Organize trainers and discuss their roles, emphasizing teamwork.<br />
❑ Determine how to involve practicum-site staff in the practicum.<br />
Clinical Practicum<br />
Note to trainer:<br />
This document may need to be adapted for your setting. Consider the length of time needed and available for<br />
practice, the order of topics, the need for additional trainers, the amount of review required at the start of each topic<br />
and other logistics when adapting the module.<br />
❑ Determine what each learners’ role will be during the practicum.<br />
❑ Determine how to configure teams of learners and trainers.<br />
❑ Arrange for learners to observe or assist <strong>with</strong> care for women <strong>with</strong> complications.<br />
❑ Prepare and duplicate materials (flipcharts, checklists, evaluation forms).<br />
❑ Ensure readiness of equipment and supplies needed for the practicum.<br />
❑ Have alternative activities ready for learners to do when client caseload is slow.<br />
❑ Review the Clinical Training Approaches and Coaching Skills session of the Effective Training<br />
in Reproductive Health: Course Design and Delivery Trainer’s Manual.<br />
❑ Review Conducting This Clinical Practicum (below).<br />
Conducting This Clinical Practicum<br />
Time required<br />
The time required for this clinical practicum can vary significantly depending on the practicum design, the needs<br />
and skills of learners, the amount of time available, and many other factors.<br />
Format<br />
This practicum module is divided into practicum sessions by skill set. The content of each session reflects the<br />
module of the same name in the didactic part of this training. Each session of the practicum should begin <strong>with</strong> a<br />
short content review—a mini-lecture using flipcharts and a review of the checklist(s) for that skill. After completing<br />
the content and checklist review, brief learners on the details of the session and then release them to their<br />
assignments. At the end of each practice session, have learners regroup to debrief and discuss.<br />
Designing the Practicum<br />
❑ The design of the practicum depends on the needs of the learners and realities of the practicum site. Determine<br />
whether the practicum can be held <strong>with</strong> several learners and several trainers at one time at the same site or at several<br />
sites at the same time. A modular or other adapted approach can be used, staggering place, times, learners,<br />
trainers and/or skills.<br />
• Consider designing the practicum so that learners practice skills that logically go together during clinical<br />
care.<br />
• Utilize the time well.<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 31
❑ If the learners will be divided into groups or will practice at different sites, arrange for additional trainers,<br />
because each learner must be directly supervised by a trainer.<br />
❑ Employ principles of adult learning and maintain a positive learning environment.<br />
Before the Practicum<br />
❑ Identify when caseload at the practicum site is highest. To build caseload, consider asking local facilities to refer<br />
women coming for abortion services to the practicum site during the training period. Alternatively, schedule women<br />
for endometrial biopsy during the practicum and allow learners to perform the procedure, as the skill is similar to<br />
uterine <strong>evacuation</strong>.<br />
❑ Ensure that practicum-site protocols, equipment and supplies are consistent <strong>with</strong> skills to be taught; decide how<br />
to handle any noted discrepancies.<br />
• If necessary, adapt training activities to more closely reflect practicum-site practices, or create additional<br />
activities.<br />
❑ Determine where review and debrief discussions can take place before and after practice. This may be a private<br />
room on- or off-site.<br />
❑ Determine how to keep track of learners who have successfully achieved competency and those who need more<br />
practice, as well as how the latter will receive that additional practice.<br />
During the Practicum<br />
❑ Refer to the Reference Manual frequently during review, debriefing and other discussions <strong>with</strong> learners.<br />
❑ Assign learners to practice procedures according to their skill level.<br />
❑ Assign a few learners and a trainer to work together in ―practice groups.‖ Pair strong learners <strong>with</strong> weaker ones<br />
and ask them to help each other. Once some learners have reached competency, they can help those who have not.<br />
Ensure learners understand what their roles are, what the other learners’ roles are and how to assist other learners.<br />
❑ Limit the number of learners and observers for each procedure.<br />
❑ Obtain the client’s permission for learners to perform the procedure, ensuring she understands that the trainer will<br />
be present and that she has the right to refuse <strong>with</strong>out being denied care.<br />
❑ Always respect the woman’s right to confidentiality and privacy, not only in direct care but also when discussing<br />
her care <strong>with</strong> learners.<br />
❑ Only give corrective feedback to learners in the presence of a client when the mistake could endanger her or<br />
cause her discomfort, in order to limit the anxiety of the client as well as the learner.<br />
❑ Carefully monitor the practicum to ensure that other trainers are following agreed-upon protocols and using the<br />
checklists; to problem-solve issues that arise; to ensure that practice groups are working well; and to make certain<br />
that every learner is getting opportunities to participate.<br />
❑ In addition to leading a debrief discussion, consider seeking feedback from learners after each session.<br />
❑ Use the Clinical Skills Evaluation form in this module for evaluating learners to determine if they can be<br />
considered competent in abortion-care skills.<br />
After the Practicum<br />
❑ Provide the evaluation for learners to complete<br />
❑ Debrief <strong>with</strong> site staff and other trainers about what worked well and how the clinical practicum could be<br />
improved, and thank everyone for their participation.<br />
❑ Provide each learner <strong>with</strong> specific recommendations for implementing and improving their skills when they<br />
return to their sites.<br />
❑ Provide feedback on each learner’s skills to their site supervisor, if appropriate.<br />
❑ Provide opportunities for refresher courses and site-visit exchanges between learners.<br />
❑ Ask the learners what they see as their most important next steps and how you might assist them.<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 32
Tool C-6: MVA Procedure Checklist: Incomplete/Missed Abortion<br />
INSTRUCTIONS: Provide a copy to each participant for use during training on pelvic models. Only one version<br />
of this tool is printed below, but the CD-ROM contains both versions.<br />
MVA Procedure Checklist: Incomplete/Missed Abortion<br />
Skills Yes No Comments<br />
Creates pain management plan<br />
Tailors pain management plan <strong>with</strong> woman according to her needs<br />
Discusses sources of pain, options, potential side effects<br />
Includes combination of support and pharmacological measures<br />
Takes into account woman’s medical and psychological status, dilatation<br />
necessary, staff skill, nature of procedure and availability of supplies<br />
Prepares the instruments<br />
Checks <strong>vacuum</strong> retention of aspirator<br />
Has more than one instrument available<br />
Prepares the woman<br />
Administers pain medication in timely fashion<br />
Asks woman to empty her bladder<br />
Asks what supportive measures she would like and provides them<br />
Asks for permission to start<br />
Puts on barriers and washes hands<br />
Performs pelvic exam to confirm assessment findings<br />
Warms and inserts speculum gently<br />
Removes foreign bodies in os; refers if bowel present<br />
Performs cervical antiseptic prep<br />
Follows No-Touch Technique<br />
Uses antiseptic sponges to clean os and, if desired, vagina<br />
Administers paracervical block<br />
Uses less than 200mg lidocaine<br />
Aspirates before injecting 1–2mL at tenaculum site<br />
Places tenaculum<br />
Applies slight traction to expose tissue transition<br />
Slowly injects 2–5mL lidocaine to 1–1.5 inches at 3,5,7 and 9 o’clock<br />
Dilates cervix if needed<br />
Inserts cannula<br />
Applies gentle traction to cervix<br />
Rotates cannula while gently applying pressure<br />
Inserts cannula to just past internal os OR to fundus and pulls back<br />
Suctions uterine contents<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 33
Holds tenaculum and end of cannula in one hand<br />
Attaches charged aspirator<br />
Releases buttons to start <strong>vacuum</strong><br />
Rotates cannula 180 degrees each direction<br />
Uses an ―in and out‖ motion<br />
Does not <strong>with</strong>draw aperture beyond os<br />
Uses gentle operative technique<br />
Uses positive, respectful, supportive reassurance<br />
Stops when pink foam <strong>with</strong>out tissue passes, gritty sensation is felt, uterus<br />
contracts around cannula and uterine cramping increases<br />
Removes the instrument<br />
Is ready to evacuate again after inspecting tissue if needed<br />
Inspects tissue<br />
Empties aspirator into container<br />
Looks for products of conception (POC)<br />
Evaluates amount based on estimated gestation<br />
Determines all POC have been removed<br />
Completes remaining steps:<br />
Wipes cervix to assess bleeding<br />
Considers if pelvic exam is advisable<br />
Reassures woman that procedure is finished<br />
Performs post-procedure care<br />
Processes instruments<br />
Removes barriers and washes hands<br />
Ensures woman is escorted to recovery area<br />
Resolves technical problems that arise<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 34
Tool C-7:<br />
MVA 301 Sample Learning Assessment Tools<br />
(Contexts: incomplete/missed abortion; multiple use for cannulae)<br />
INSTRUCTIONS: There are two parts of Learning Assessments for MVA 301: (1) Clinical Skills Evaluation, and<br />
(2) Learning Assessment for Managing Complications and Monitoring.<br />
For Clinical Skills Evaluation: Provide one copy per participant for the Clinical Trainer who is conducting the<br />
Clinical Practicum portion of this course. The Clinical Trainer will complete an evaluation for each participant and<br />
review it <strong>with</strong> personally <strong>with</strong> the participant, either immediately after the practicum (if time allows) or during the<br />
Learning Assessment module of the course.<br />
For the Learning Assessment for Managing Complications and Monitoring, keep one copy of test <strong>with</strong> highlighted<br />
answers for presenter/trainer. Select the participant version from the CD-ROM (correct answers not noted) make<br />
one copy for each participant and administer at end of course to all participants. Review answers <strong>with</strong> all<br />
participants after they have completed test.<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 35
Clinical Skills Evaluation<br />
UTERINE EVACUATION FOR INCOMPLETE/MISSED ABORTION:<br />
Instructions: The trainer should use one form to evaluate the ability of each learner based on direct observation of<br />
the learner’s management of an incomplete abortion case, including performance of <strong>manual</strong> <strong>vacuum</strong> <strong>aspiration</strong><br />
(MVA). Proficiency in MVA service delivery requires demonstrating competency on all items in Part I. If a learner<br />
does not demonstrate competency or cannot be observed, refer to Part II where recommendations can be made as to<br />
how performance might be improved to achieve competency. After completing the form, the trainer should discuss<br />
the results <strong>with</strong> the learner.<br />
Mark an X in the box next to each step that is competently demonstrated by the learner.<br />
I. Clinical Skills<br />
❑ 1. Establishes rapport <strong>with</strong> the woman, helping her feel comfortable<br />
❑ 2. Assesses the woman’s status: medical history, presenting conditions, date of LMP, emotional state<br />
❑ 3. Provides or confirms that the woman received counseling: privately explores her decisions<br />
❑ 4. Discusses the procedure <strong>with</strong> the woman and obtains consent<br />
❑ 5. Evaluates need for and administers pain management based on the woman’s condition and her desires<br />
❑ 6. Uses infection-prevention practices: handwashing, gloves<br />
❑ 7. Assesses uterus: size, position, trauma<br />
❑ 8. Identifies cervical laceration or trauma<br />
❑ 9. Identifies possible reproductive tract infection<br />
❑ 10. Ensures that the cannulae are HLD or sterile and rinsed of caustic solutions<br />
❑ 11. Prepares aspirator and checks <strong>vacuum</strong><br />
❑ 12. Selects cannula based on uterine size and dilatation; inspects cannula and aspirator for wear<br />
❑ 13. Swabs cervix, and vagina if desired, <strong>with</strong> antiseptic solution<br />
❑ 14. Administers paracervical block and any other medications; allows time for medications to take effect<br />
❑ 15. Dilates the cervix, if needed<br />
❑ 16. Inserts cannula and attaches aspirator<br />
❑ 17. Uses no-touch technique; does not contaminate the cannula<br />
❑ 18. Moves cannula effectively to empty the uterus<br />
❑ 19. Stops <strong>evacuation</strong> when signs of completion are present<br />
❑ 20. Examines the aspirate to assure it is consistent <strong>with</strong> the woman’s condition<br />
❑ 21. Assures post-procedure care is provided to monitor and discuss her recovery<br />
❑ 22. Assures contraceptive counseling and a method are provided if the woman desires<br />
❑ 23. Assures follow-up care is scheduled <strong>with</strong> referrals made where needed<br />
II. Recommendations.<br />
For skills that were not performed to competency or were not observed, suggest recommendations to be followed,<br />
for example: “needs to continue practice under supervision” or “repeat clinical training.”<br />
Item<br />
Recommendation<br />
____________________ __________________________________________________________<br />
____________________ __________________________________________________________<br />
____________________ __________________________________________________________<br />
____________________ __________________________________________________________<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 36
III. Comments<br />
Please add any comments you may have about the learner’s ability to perform MVA.<br />
__________________________________________________________________________________<br />
__________________________________________________________________________________<br />
__________________________________________________________________________________<br />
__________________________________________________________________________________<br />
__________________________________________________________________________________<br />
PLEASE PRINT<br />
Evaluator ____________________________ Learner ____________________________________<br />
Name<br />
Name<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 37
Sample Learning Assessment Tool for Managing Complications and<br />
Monitoring (test & answer key) (Trainer version)<br />
Circle the correct response<br />
1. MVA procedures result in immediate and long-term complications when performed by<br />
trained providers:<br />
a. Rarely, but complications can include infection and/or retained POC [correct]<br />
b. Quite often<br />
c. Such as breast cancer and infertility<br />
d. b & c<br />
2. Managing complications does not entail:<br />
a. Staff knowing how to recognize a complication<br />
b. Staff knowing how to treat a complication<br />
c. Referral for conditions that cannot be fully treated onsite [correct]<br />
d. Fully treating onsite all complications that occur<br />
3. Retained products of conception (POC):<br />
a. Is indicated by vaginal bleeding and pain<br />
b. Can lead to infection<br />
c. Is treatable by <strong>vacuum</strong> <strong>aspiration</strong><br />
d. All of the above [correct]<br />
4. Continuing pregnancy:<br />
a. Is the same as failed abortion<br />
b. Requires uterine <strong>evacuation</strong><br />
c. Both a & b [correct]<br />
d. Is caused by dilatation and curettage (D&C)<br />
5. A condition that occurs when the uterus cannot contract to stop bleeding is:<br />
a. Disseminated intravascular coagulopathy (DIC)<br />
b. Ashermans Syndrome<br />
c. <strong>Uterine</strong> atony [correct]<br />
d. Hematometra<br />
6. The causes of medication-related complications can include:<br />
a. Overdosage<br />
b. Incorrect injection into a vessel<br />
c. Hypersensitivity<br />
d. All of the above [correct]<br />
7. Medical-abortion complications include:<br />
a. Severe and prolonged bleeding, continuing pregnancy [correct]<br />
b. Severe headaches, dizziness<br />
c. Brief fainting spells<br />
d. a & c<br />
8. A vasovagal reaction:<br />
a. Is the same as physiological shock<br />
b. Usually resolves itself and is not life-threatening [correct]<br />
c. Indicates uterine perforation<br />
d. Must be treated surgically<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 38
9. Sites should refer women <strong>with</strong> complications to another facility if:<br />
a. They cannot fully treat her onsite [correct]<br />
b. She cannot pay at the current site<br />
c. She has a high fever<br />
d. She has injury to the uterus, vagina or bowel<br />
10. After-care for women <strong>with</strong> complications includes providing:<br />
a. Close monitoring<br />
b. Information about follow-up<br />
c. Counseling on medical and emotional consequences<br />
d. All of the above [correct]<br />
11. Circle True or False:<br />
1. True or False Monitoring is a random tracking of services conducted once in a while. [false]<br />
2. True or False Monitoring does not need to be expensive or complex.[true]<br />
3. True or False It is possible to use existing sources of information for monitoring.[true]<br />
4. True or False To measure changes in one type of service, different information should be<br />
collected each time. [false]<br />
5. True or False An example of an indicator is the number and type of complications. [true]<br />
12. Put the steps of monitoring in correct order: [b,a,d,c]<br />
___ a. Information gathering<br />
___ b. Planning<br />
___ c. Developing an action plan<br />
___ d. Analysis<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 39
Tool C-8:<br />
MVA 301 Course Evaluation<br />
INSTRUCTIONS: Insert date and location of course at top of evaluation. Provide Course Evaluation for each<br />
participant at the end of the course and ask them to complete and turn in before leaving. Study the responses after<br />
the course, <strong>with</strong> the goal of using responses to improve and adapt the course for future offerings.<br />
MVA 301 Course Evaluation<br />
DATE:_________________________ LOCATION:_______________________<br />
Course Objectives:<br />
Perform a supervised MVA procedure in a local clinical facility<br />
Be familiar <strong>with</strong> key tools for monitoring services <strong>with</strong> a goal toward quality improvement<br />
Be able to manage potential complications<br />
4 = strongly agree 3 = agree 2 = disagree 1 = strongly disagree<br />
Rating<br />
1. The course fulfilled its goal and objectives (see above). ______<br />
Comments:<br />
2. The trainers were responsive to participants’ needs. ______<br />
Comments:<br />
3. Because of this course, I have a better understanding of how to use MVA. _______<br />
Comments:<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 40
4. Now that I have completed this course, I feel<br />
a. Ready to offer care to women <strong>with</strong> MVA<br />
b. That I need more training before offering care <strong>with</strong> MVA to women<br />
c. That this procedure is not one I would choose to provide<br />
d. Prepared to promote (but not provide) MVA services<br />
e. Other [please describe]<br />
5. What suggestions can you offer to improve this course in the future?<br />
6. I came to this course <strong>with</strong><br />
a) No experience providing transvaginal procedures<br />
b) Less than three years clinical experience including transvaginal procedures<br />
c) Between three and five years of clinical experience including transvaginal procedures<br />
d) More than five years of clinical experience including transvaginal procedures<br />
7. My clinical background is as:<br />
a) Professional midwife or nurse-midwife<br />
b) Other advance practice or midlevel clinician (physician’s assistant, clinical officer, professional<br />
nurse, etc)<br />
c) Medical doctor (non specialist)<br />
d) Ob-Gyn specialists<br />
e) Public Health (non practicing clinician)<br />
f) Other (please describe)<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 41
Tool C-9:<br />
MVA 301 Certificate Template<br />
(full page version on CD-ROM)<br />
INSTRUCTIONS: Print one copy of Certificate Template for each participant, customized <strong>with</strong> each individual<br />
participant name, and distribute at the close of course.<br />
Insert logo of<br />
sponsor/host<br />
organization<br />
SUPERVISED CLINICAL PRACTICE WITH<br />
Manual Vacuum Aspiration<br />
Course 301<br />
Add Logo of<br />
sponsoring<br />
Organization<br />
CERTIFICATE OF COMPLETION<br />
Awarded to<br />
____________________________________<br />
NAME<br />
________________________________<br />
PLACE<br />
_________________________<br />
DATE<br />
Insert name of Clinical Trainer<br />
Insert name of Course Sponsor<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 42
Tool C-10: Information on Instruments and Availability<br />
INSTRUCTIONS: Insert specific contact information of local MVA instruments supplier in template,<br />
delete instructions and print one copy for each participant in course.<br />
Contact information for MVA instruments supplier(s):<br />
For information on planning and calculating instruments supply,<br />
see www.mvacalculator.org and/or use the following table:<br />
UTERINE EVACUATION WITH MVA: A TRAINING MANUAL FOR CONDUCTING SHORT COURSES Page 43
E-09-MVA-008<br />
Rev. 0 12/2009<br />
MVASRTC-E09