Clogging of Drainage Catheters: Quantitative and Longitudinal ...
Clogging of Drainage Catheters: Quantitative and Longitudinal ...
Clogging of Drainage Catheters: Quantitative and Longitudinal ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Radiology<br />
Kyoung Ho Lee, MD<br />
Joon Koo Han, MD<br />
Kwang Gi Kim, PhD<br />
Youngro Byun, PhD<br />
Chang Jin Yoon, MD<br />
Seung Ja Kim, MD<br />
Byung Ihn Choi, MD<br />
Index terms:<br />
Abscess, percutaneous drainage,<br />
70.21<br />
Animals<br />
<strong>Catheters</strong> <strong>and</strong> catheterization,<br />
technology, 70.21<br />
Experimental study, 70.21<br />
Published online before print<br />
10.1148/radiol.2281020245<br />
Radiology 2003; 227:833–838<br />
Abbreviation:<br />
ID internal diameter<br />
1 From the Department <strong>of</strong> Radiology,<br />
Institute <strong>of</strong> Radiation Medicine, Clinical<br />
Research Institute (K.H.L., J.K.H., C.J.Y.,<br />
S.J.K., B.I.C.) <strong>and</strong> Interdisciplinary Program<br />
in Medical <strong>and</strong> Biological Engineering,<br />
Clinical Research Institute<br />
(K.G.K.), Seoul National University College<br />
<strong>of</strong> Medicine, Seoul National University<br />
Hospital, 28 Yongon-dong,<br />
Chongno-gu, Seoul 110-744, Korea;<br />
<strong>and</strong> Department <strong>of</strong> Materials Science<br />
<strong>and</strong> Engineering, Kwangju Institute <strong>of</strong><br />
Science <strong>and</strong> Technology, Gwangju,<br />
Korea (Y.B.). Received March 29,<br />
2002; revision requested June 11; final<br />
revision received November 5; accepted<br />
November 19. Supported in<br />
part by Korean Ministry <strong>of</strong> Health<br />
<strong>and</strong> Welfare grant HMP-98-G-2-034.<br />
Address correspondence to J.K.H.<br />
(e-mail: hanjk@radcom.snu.ac.kr).<br />
<strong>Clogging</strong> <strong>of</strong> <strong>Drainage</strong> <strong>Catheters</strong>:<br />
<strong>Quantitative</strong> <strong>and</strong> <strong>Longitudinal</strong><br />
Assessment by Monitoring<br />
Intracatheter Pressure in<br />
<strong>Catheters</strong> <strong>and</strong> Rabbits 1<br />
PURPOSE: To develop a method for the quantitative <strong>and</strong> longitudinal assessment <strong>of</strong><br />
clogging in drainage catheters <strong>and</strong> to confirm the validity <strong>of</strong> the method.<br />
MATERIALS AND METHODS: Intracatheter pressure was measured during the<br />
infusion <strong>of</strong> saline at a rate <strong>of</strong> 0.1–3.0 mL/sec in nine catheters with different internal<br />
diameters. With the data obtained, a fitting equation between the intracatheter<br />
pressure <strong>and</strong> internal diameter was derived on the basis <strong>of</strong> the Poiseuille law. To<br />
confirm the validity <strong>of</strong> this measurement method, four drainage catheters were<br />
inserted into the peritoneal cavity in each <strong>of</strong> 15 rabbits. Intracatheter pressures at<br />
infusion rates <strong>of</strong> 0.1 <strong>and</strong> 0.5 mL/sec were monitored for 14 days, while the degrees<br />
<strong>of</strong> catheter clogging were graded on the basis <strong>of</strong> the different frequencies <strong>of</strong> manual<br />
irrigation: one, two, or three times per day. Repeated measures analysis <strong>of</strong> variance<br />
was used to determine the statistical significance <strong>of</strong> differences in pressure between<br />
different irrigation frequencies.<br />
RESULTS: Pressure was measured successfully throughout the experiment except in<br />
three rabbits with dislodged catheters. Three to 14 days after catheter insertion, the<br />
pressures were significantly lower in catheters with higher irrigation frequencies<br />
than in those with lower irrigation frequencies (P .05). The effective internal<br />
diameter <strong>of</strong> each catheter could be monitored by means <strong>of</strong> the derived fitting<br />
equation.<br />
CONCLUSION: This method can be used to quantitatively measure the degree <strong>of</strong><br />
clogging <strong>of</strong> a drainage catheter. It can also be used for comparative or longitudinal<br />
in vivo studies concerning the effectiveness <strong>of</strong> drainage procedures or catheter<br />
development.<br />
©<br />
RSNA, 2003<br />
Author contributions:<br />
Guarantor <strong>of</strong> integrity <strong>of</strong> entire study,<br />
B.I.C.; study concepts, K.H.L., Y.B.;<br />
study design, K.H.L., J.K.H., K.G.K.,<br />
C.J.Y.; literature research, S.J.K.; experimental<br />
studies, C.T.Y., S.J.K., K.H.L.;<br />
data acquisition, K.H.L., C.J.Y., S.J.K.;<br />
data analysis/interpretation, C.J.Y.,<br />
S.J.K.; manuscript preparation, K.H.L.,<br />
J.K.H., S.J.K.; manuscript definition <strong>of</strong><br />
intellectual content, C.J.Y., K.G.K.,<br />
Y.B.; manuscript editing, B.I.C.; manuscript<br />
revision/review <strong>and</strong> final version<br />
approval, B.I.C., J.K.H.<br />
©<br />
RSNA, 2003<br />
In the past decade, computed tomography– <strong>and</strong> sonography-guided percutaneous drainage<br />
<strong>of</strong> abscesses <strong>and</strong> fluid collections has become a widely used, safe, <strong>and</strong> effective<br />
technique. Various factors can hinder or delay the successful drainage <strong>of</strong> abscesses, such as<br />
the location <strong>and</strong> configuration <strong>of</strong> the abscess (1–3), the nature <strong>of</strong> the infecting organism,<br />
host resistance (4), fistulous connections, <strong>and</strong> viscosity <strong>of</strong> the abscess contents (5). Several<br />
procedure-related factors can also influence the patency <strong>of</strong> the drainage tube. A number <strong>of</strong><br />
methods for preventing catheter clogging have been proposed, including the use <strong>of</strong><br />
irrigations <strong>and</strong> large-lumen or sump-type catheters (6). However, catheter clogging is still<br />
encountered frequently during various drainage procedures.<br />
We have been working on the development <strong>of</strong> anticlogging drainage catheters with new<br />
biomaterials <strong>and</strong> drug-delivery technologies in recent years. During this work, we found<br />
that no recognized method has been reported for objective evaluation <strong>of</strong> the effectiveness<br />
<strong>of</strong> catheter drainage. The purpose <strong>of</strong> this study was to develop a method for the quantitative<br />
<strong>and</strong> longitudinal assessment <strong>of</strong> clogging in drainage catheters <strong>and</strong> to confirm the<br />
validity <strong>of</strong> the method.<br />
833
Radiology<br />
MATERIALS AND METHODS<br />
Principle<br />
The flow <strong>of</strong> fluids, including pus (5),<br />
through a drainage catheter is governed<br />
by the Poiseuille law (7), which describes<br />
the rate <strong>of</strong> laminar flow <strong>of</strong> fluid (or gas)<br />
through a cylindric structure. For drainage<br />
catheters, the Poiseuille law is expressed<br />
by the following equation:<br />
Q Prr4<br />
8L , (1)<br />
where Q is the flow rate, Pr is the pressure<br />
gradient between the two ends <strong>of</strong> the<br />
catheter, r is the radius <strong>of</strong> the catheter, L<br />
is the length <strong>of</strong> the catheter, <strong>and</strong> is the<br />
viscosity <strong>of</strong> the fluid. If the fluid is infused<br />
at a constant rate by using an infusion<br />
pump, the resistance <strong>of</strong> a given catheter<br />
can be expressed as a function <strong>of</strong> the<br />
intracatheter pressure (Pr) because all<br />
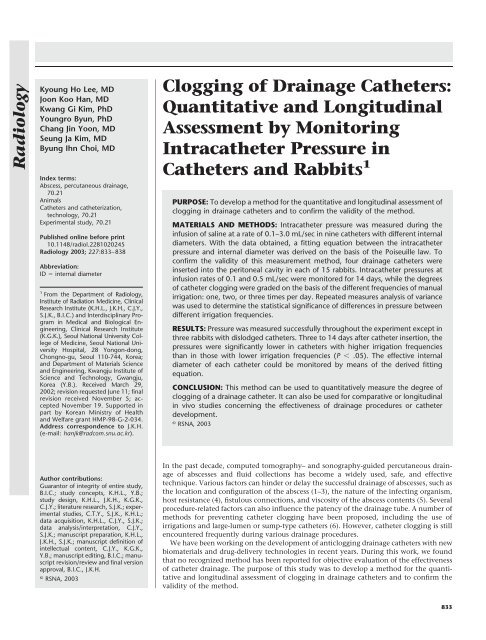
other variables remain constant (Fig 1).<br />
Furthermore, the effective internal diameter<br />
(ID) <strong>of</strong> a drainage catheter, which is<br />
influenced by the clogging effect in vivo,<br />
can be calculated if other variables are<br />
known.<br />
With the method used in this study, a<br />
prerequisite is that the infusion pump<br />
(A-50 B-1; Nemoto Kyorindo, Tokyo, Japan)<br />
must maintain a constant infusion<br />
rate when the intracatheter pressure is<br />
high. We confirmed the constant rate in<br />
a separate experiment. The cumulative<br />
volume infused was increased linearly at<br />
a preset infusion rate from 0.1 to 3.0 mL/<br />
sec until the intracatheter pressure exceeded<br />
the measurable limit (350 mm<br />
Hg) <strong>of</strong> the pressure-monitoring device<br />
(Siredoc 60; Siemens Medical Systems, Erlangen,<br />
Germany), which was a st<strong>and</strong>ard<br />
patient monitor. In the present study,<br />
laminar flow was presumed for all measurements,<br />
<strong>and</strong> every precaution was<br />
taken to ensure that catheters were<br />
aligned to avoid kinking or distortion <strong>of</strong><br />
the lumen.<br />
In Vitro Experiment<br />
A series <strong>of</strong> unused angiographic <strong>and</strong><br />
drainage catheters with different IDs<br />
were connected to the measurement system,<br />
as illustrated in Figure 1, <strong>and</strong> the<br />
intracatheter pressure was measured during<br />
the infusion <strong>of</strong> saline at a rate from<br />
0.1 to 3.0 mL/sec (C.J.Y., S.J.K.). This in<br />
vitro experiment was performed (a) to<br />
verify that the measurement system discriminated<br />
adequately between catheters<br />
with different IDs, (b) to allow the derivation<br />
<strong>of</strong> a st<strong>and</strong>ard curve (or equation)<br />
between the intracatheter pressure <strong>and</strong><br />
the effective ID, <strong>and</strong> (c) to determine the<br />
infusion rate to be used in the animal<br />
experiment. The 48 combinations <strong>of</strong> IDs<br />
<strong>and</strong> infusion rates are summarized in Table<br />
1. If the ID <strong>of</strong> each catheter was not<br />
provided by the manufacturers, it was<br />
measured with image analysis s<strong>of</strong>tware<br />
(UTHSCSA ImageTool, version 2.03; University<br />
<strong>of</strong> Texas Health Science Center,<br />
San Antonio, Tex), <strong>and</strong> digitally captured<br />
images <strong>of</strong> a magnified cut surface were<br />
obtained by using a stereomicroscope (SZ<br />
11; Olympus Optical, Tokyo, Japan).<br />
We measured the ID <strong>of</strong> each catheter<br />
five times <strong>and</strong> calculated the mean after<br />
discarding the highest <strong>and</strong> lowest values.<br />
All catheters were carefully cut at the<br />
shaft to a fixed length <strong>of</strong> 30 cm. After<br />
infusion was initiated, the intracatheter<br />
pressure gradually increased until it<br />
reached a plateau (determined with consensus<br />
between the two observers) in<br />
5–15 seconds; this plateau indicated that<br />
a steady state had been reached between<br />
inflow from the infusion pump <strong>and</strong> outflow<br />
from the catheter tip. To minimize<br />
measurement error, intracatheter pressure<br />
was measured five times for each<br />
combination. The mean value was calculated<br />
after the highest <strong>and</strong> lowest values<br />
had been discarded. The pressure-monitoring<br />
device was set to zero by opening<br />
the system to air before each measurement.<br />
St<strong>and</strong>ard Equation<br />
For the measurement system used in<br />
this study, the Poiseuille law equation<br />
can be written as follows:<br />
Pr 5.628 1012 Q<br />
<br />
6,000<br />
D 4 , (2)<br />
where Pr (in millimeters <strong>of</strong> mercury) is<br />
intracatheter pressure, Q (in milliliters<br />
per second) is infusion rate, <strong>and</strong> D (in<br />
French) is ID <strong>of</strong> catheter because the<br />
length was fixed to 30 cm <strong>and</strong> the viscosity<br />
<strong>of</strong> water is 1.002 10 3 Ns/m 2 at<br />
20°C (8).<br />
On the basis <strong>of</strong> Equation (2), a fitting<br />
equation was derived to describe the intracatheter<br />
pressure as a function <strong>of</strong> the<br />
infusion rate <strong>and</strong> ID. This process included<br />
empirical modification <strong>of</strong> Equation<br />
(2) by trial <strong>and</strong> error (K.G.K.) <strong>and</strong><br />
iterative nonlinear curve fitting (Origin,<br />
version 6.1; OriginLab, Northampton,<br />
Mass) with the in vitro experimental data<br />
for 48 combinations.<br />
The fitting equation was modified as<br />
follows:<br />
Figure 1. Diagram <strong>of</strong> pressure measurement<br />
system. A catheter, a pressure-monitoring device,<br />
<strong>and</strong> an infusion pump are connected<br />
with a three-way stopcock. If the fluid is infused<br />
at a constant mean rate (Q) <strong>of</strong> the infusion<br />
pump, the resistance (R) <strong>of</strong> a given catheter<br />
can be expressed as a function <strong>of</strong> the<br />
intracatheter pressure (P).<br />
Pr k 1 Q 2 10 10 k 2 e Q/k3 k 4 <br />
<br />
6,000<br />
D 4 ,<br />
k 5<br />
(3)<br />
where k 1 , k 2 , k 3 , k 4 , <strong>and</strong> k 5 are coefficients.<br />
The error range <strong>of</strong> this fitting<br />
equation was represented by k 1 . With<br />
this equation, the relationship between<br />
the ID <strong>and</strong> the intracatheter pressure was<br />
plotted at each infusion rate. These<br />
curves were compared with the ideal<br />
curves generated by the Poiseuille equation<br />
(Eq [2]). The fitting equation was<br />
also used to calculate the theoretic effective<br />
IDs <strong>of</strong> catheters in the animal experiment.<br />
Animal Experiment<br />
All animal experimental protocols<br />
were approved by the animal research<br />
committee at our institution <strong>and</strong> were<br />
performed at the Clinical Research Institute.<br />
Fifteen New Zeal<strong>and</strong> White rabbits<br />
(body weight, 2.5–3.0 kg) were used for<br />
the experiment. Animals were sedated<br />
with an intramuscular injection <strong>of</strong> 12-15<br />
mg per kilogram <strong>of</strong> body weight <strong>of</strong> ketamine<br />
hydrochloride (Ketalar; Yuhan<br />
Yanghang, Seoul, Korea) <strong>and</strong> 2 mg/kg <strong>of</strong><br />
xylazine hydrochloride (Rompun 2%;<br />
Bayer Korea, Seoul, Korea). After the abdominal<br />
wall was shaved <strong>and</strong> prepared,<br />
four st<strong>and</strong>ard 8-F drainage catheters<br />
(Jungsung) with length <strong>of</strong> 30 cm <strong>and</strong> ID<br />
<strong>of</strong> 5.07 F were inserted into the peritoneal<br />
cavity <strong>of</strong> each rabbit, with the<br />
Seldinger method <strong>and</strong> fluoroscopic guidance<br />
(C.J.Y.). Efforts were made to place<br />
the tips <strong>of</strong> the four catheters in the same<br />
region <strong>of</strong> the peritoneal cavity. During<br />
834 Radiology June 2003 Lee et al
TABLE 1<br />
Catheter <strong>and</strong> Infusion Rates Tested in in Vitro Experiment<br />
Radiology<br />
Catheter Name<br />
Manufacturer<br />
Outer<br />
Diameter<br />
(F)<br />
ID (F)<br />
Infusion Rate (mL/sec)<br />
0.1 0.5 1.0 1.5 2.0 2.5 3.0<br />
Micr<strong>of</strong>erret-18 infusion<br />
catheter Cook, Bloomington, Ind 3 1.58 Yes No No No No No No<br />
Tempo angiographic<br />
catheter Cordis, Miami, Fla 4 2.86 Yes Yes Yes Yes No No No<br />
Torcon NB Advantage<br />
angiographic catheter Cook 5 3.12 Yes Yes Yes Yes Yes Yes Yes<br />
<strong>Drainage</strong> catheter Jungsung, Seongnam, Korea 7 3.88 Yes Yes Yes Yes Yes Yes Yes<br />
Envoy guiding catheter Cordis 6 4.35 No Yes Yes Yes Yes Yes Yes<br />
<strong>Drainage</strong> catheter Jungsung 8 5.07 No Yes Yes Yes Yes Yes Yes<br />
<strong>Drainage</strong> catheter Jungsung 9 5.38 No Yes Yes Yes Yes Yes Yes<br />
<strong>Drainage</strong> catheter Jungsung 10 6.74 No Yes Yes Yes Yes Yes Yes<br />
Simple-Loc Locking<br />
Loop (MSL) Cook 12 7.33 No No Yes Yes Yes Yes Yes<br />
the follow-up period, the catheters were<br />
left in place, <strong>and</strong> animals were kept in a<br />
specially designed restraint cage in the<br />
laboratory to prevent the catheters from<br />
being dislodged accidentally. Each day,<br />
200 mg <strong>of</strong> cefazolin sodium (Cefamezin;<br />
Dong-a Pharmacy, Seoul, Korea) <strong>and</strong> 15<br />
mg <strong>of</strong> gentamicin sulfate (Gentamicin;<br />
Korea United Pharmacy, Seoul, Korea)<br />
was administered intramuscularly to prevent<br />
peritonitis.<br />
To grade the degrees <strong>of</strong> catheter clogging,<br />
each <strong>of</strong> the four catheters inserted<br />
into an animal was irrigated manually<br />
with 10 mL <strong>of</strong> sterile saline at a different<br />
frequency (zero, one, two, or three times<br />
per day). With the method described in<br />
the in vitro experiment, intracatheter<br />
pressure was measured for each catheter<br />
at baseline <strong>and</strong> 3, 7, 10, <strong>and</strong> 14 days after<br />
insertion by infusing sterile saline at rates<br />
<strong>of</strong> 0.1 <strong>and</strong> 0.5 mL/sec, consecutively.<br />
These infusion rates were predetermined<br />
on the basis <strong>of</strong> results in the in vitro<br />
experiment to ensure that the maximum<br />
intracatheter pressure was within the<br />
measurable range <strong>of</strong> the pressure-monitoring<br />
device. Measurement procedures<br />
were conducted together by two radiologists<br />
(C.J.Y., S.J.K.), who were blinded to<br />
the irrigation frequency. Measurements<br />
were obtained from the four catheters in<br />
each animal in r<strong>and</strong>om order. From the<br />
intracatheter pressure, we were able to<br />
calculate the effective ID by using the<br />
fitting equation derived on the basis <strong>of</strong><br />
results in the in vitro experiment.<br />
Changes in effective ID during the 14-<br />
day follow-up period were plotted for<br />
each irrigation frequency.<br />
Microscopic Analysis<br />
After the study was completed, the<br />
catheters were removed, <strong>and</strong> the animals<br />
were returned to laboratory cages; there<br />
were no complications. The surface<br />
morphology <strong>of</strong> the catheters after withdrawal<br />
was examined with stereomicroscopy<br />
<strong>and</strong> scanning electron microscopy<br />
(DS130-C; Akashi, Tokyo, Japan)<br />
at an accelerating voltage <strong>of</strong> 20 kV<br />
(K.H.L., C.J.Y.), after the catheters were<br />
prepared in a st<strong>and</strong>ard manner (9). Two<br />
catheters were selected r<strong>and</strong>omly for<br />
each irrigation frequency, <strong>and</strong> representative<br />
segments were prepared for<br />
stereomicroscopic <strong>and</strong> scanning electron<br />
microscopic examinations <strong>of</strong> their<br />
internal surfaces.<br />
Statistical Analysis<br />
The data obtained in the animal experiment<br />
were analyzed to determine<br />
whether the intracatheter pressure was<br />
related to the irrigation frequency by<br />
means <strong>of</strong> repeated measures analysis <strong>of</strong><br />
variance. A P value <strong>of</strong> less than .05 was<br />
considered to indicate a statistically significant<br />
difference. Statistical analysis<br />
was not performed with the stereomicroscopic<br />
or scanning electron microscopic<br />
data.<br />
RESULTS<br />
In Vitro Experiment<br />
Intracatheter pressures at each combination<br />
<strong>of</strong> infusion rate <strong>and</strong> ID are summarized<br />
in Figure 2.<br />
St<strong>and</strong>ard Equation<br />
The coefficients k 2 , k 3 , k 4 , <strong>and</strong> k 5 were<br />
determined to be 152.089, 0.1799, 5.372,<br />
<strong>and</strong> 136, respectively, by means <strong>of</strong> iterative<br />
nonlinear curve fitting. The error<br />
range <strong>of</strong> fitting Equation (3), which is<br />
represented by k 1 , was 1.000 0.014<br />
(SD), 0.987 0.061, 1.217 0.045,<br />
1.102 0.034, 1.029 0.022, 0.931 <br />
0.029, <strong>and</strong> 0.730 0.063 at infusion<br />
rates <strong>of</strong> 0.1, 0.5, 1.0, 1.5, 2.0, 2.5, <strong>and</strong> 3.0<br />
mL/sec, respectively. By taking k 1 to be 1,<br />
the fitting equation can be written thus:<br />
Q 2 10 10<br />
152.089 e Q/0.1799 5.372<br />
Pr <br />
6,000<br />
D 4<br />
.<br />
136<br />
(4)<br />
Figure 2 illustrates the theoretic curves<br />
that describe the relationship between ID<br />
<strong>and</strong> intracatheter pressure, according to<br />
fitting Equation (4) <strong>and</strong> the Poiseuille<br />
equation (Eq [2]).<br />
Animal Experiment<br />
In three <strong>of</strong> the 15 rabbits, one or more<br />
catheters became dislodged within 4 days<br />
<strong>of</strong> follow-up, <strong>and</strong> these three rabbits were<br />
excluded from the analysis. When the<br />
infusion rate was 0.5 mL/sec, the absolute<br />
intracatheter pressure could not be<br />
measured in all combinations because it<br />
sometimes exceeded the measurable<br />
limit (350 mm Hg) <strong>of</strong> the pressure-monitoring<br />
device. In these cases, the intracatheter<br />
pressure was regarded as 350<br />
mm Hg for statistical analysis. This out<strong>of</strong>-range<br />
inaccuracy occurred in 16 catheters<br />
from day 7 after insertion: 10 catheters<br />
with an irrigation frequency <strong>of</strong> zero<br />
times per day (four catheters from day 7,<br />
five from day 10, <strong>and</strong> one from day 14),<br />
five catheters with an irrigation frequency<br />
<strong>of</strong> one time per day (three catheters<br />
from day 10 <strong>and</strong> two from day 14),<br />
<strong>and</strong> one with an irrigation frequency <strong>of</strong><br />
two times per day (from day 14).<br />
Figures 3 <strong>and</strong> 4 illustrate changes in<br />
the intracatheter pressure <strong>and</strong> the effec-<br />
Volume 227 Number 3 <strong>Clogging</strong> <strong>of</strong> <strong>Drainage</strong> <strong>Catheters</strong>: Assessment <strong>of</strong> Intracatheter Pressure 835
Radiology<br />
tive ID, respectively, during the 14-day<br />
follow-up for each irrigation frequency.<br />
Three to 14 days after catheter insertion,<br />
the intracatheter pressure was significantly<br />
lower in catheters with higher irrigation<br />
frequencies than in those with<br />
lower irrigation frequencies. Table 2 summarizes<br />
the results <strong>of</strong> statistical analysis<br />
<strong>of</strong> intracatheter pressure differences at<br />
each irrigation frequency for each observation<br />
during 14-day follow-up.<br />
Microscopic examination <strong>of</strong> the catheters<br />
after they were withdrawn showed<br />
multifocal plugging <strong>of</strong> the side holes <strong>and</strong><br />
catheter lumen with white jellylike<br />
pieces <strong>of</strong> tissue debris <strong>of</strong> various sizes <strong>and</strong><br />
frequencies. Results <strong>of</strong> histopathologic<br />
examination revealed that this tissue debris<br />
was inflammatory exudate that consisted<br />
<strong>of</strong> lymphocytes, plasma cells, neutrophils,<br />
<strong>and</strong> some eosinophils among a<br />
background <strong>of</strong> delicate fibrillary collagenous<br />
material. Results <strong>of</strong> scanning electron<br />
microscopic examination revealed<br />
that this tissue debris had irregular surfaces<br />
(Fig 5), but the catheter surfaces<br />
remained smooth in other areas without<br />
debris.<br />
Figure 2. Graphs show results <strong>of</strong> the in vitro experiment <strong>and</strong> theoretic curves. (a, b) Relationship<br />
between ID <strong>of</strong> a catheter <strong>and</strong> intracatheter pressure (P). Colors <strong>of</strong> the plots <strong>and</strong> curves<br />
indicate a specific preset infusion rate. In a, red 0.1 mL/sec, blue 1.0 mL/sec, orange 2.0<br />
mL/sec, <strong>and</strong> black 3.0 mL/sec. In b, red 0.5 mL/sec, blue 1.5 mL/sec, <strong>and</strong> black 2.5<br />
mL/sec. Data are plotted separately in a <strong>and</strong> b to avoid crowding. Plots indicate the pressures<br />
measured in 48 combinations <strong>of</strong> catheter IDs <strong>and</strong> infusion rates. Solid curves were generated by<br />
fitting Equation (4) derived from the data (plots), <strong>and</strong> the dotted curves represent the ideal curves<br />
generated by the Poiseuille equation (Eq [2]). Note agreement between the data, fitting curves,<br />
<strong>and</strong> ideal curves. A log 10 scale was used to plot P on the y axis.<br />
DISCUSSION<br />
In this study, we evaluated a method<br />
with application <strong>of</strong> the Poiseuille law for<br />
the quantitative <strong>and</strong> longitudinal assessment<br />
<strong>of</strong> catheter clogging during percutaneous<br />
drainage procedures. We verified<br />
the validity <strong>of</strong> this method in two ways:<br />
(a) by performing an in vitro experiment,<br />
in which a series <strong>of</strong> catheters with different<br />
IDs were used to simulate various degrees<br />
<strong>of</strong> obstruction <strong>and</strong> (b) by observing<br />
the results in an in vivo experiment, in<br />
which the degree <strong>of</strong> clogging was graded<br />
according to the irrigation frequency.<br />
Furthermore, our results show that the<br />
effective ID <strong>of</strong> a drainage catheter can be<br />
estimated in vivo by means <strong>of</strong> the mathematically<br />
based approach used in our<br />
study.<br />
To our knowledge, no method has<br />
been reported for evaluating the effectiveness<br />
<strong>of</strong> drainage procedures <strong>and</strong> the<br />
catheters used in such procedures. Our<br />
efforts to develop anticlogging drainage<br />
catheters in recent years have demonstrated<br />
to us that there is a need for an<br />
objective method <strong>of</strong> quantifying catheter<br />
clogging.<br />
We previously determined the degree<br />
<strong>of</strong> catheter clogging in animal models by<br />
means <strong>of</strong> measurement <strong>of</strong> catheter<br />
weight changes, microscopic morphologic<br />
analysis <strong>of</strong> side holes <strong>and</strong> luminal<br />
Figure 3. Graphs show intracatheter pressure changes in 12 rabbits during the 14-day follow-up.<br />
Pressure was measured during the infusion <strong>of</strong> sterile saline at rates <strong>of</strong> (a) 0.1 <strong>and</strong> (b) 0.5 mL/sec.<br />
The degree <strong>of</strong> catheter clogging was graded on the basis <strong>of</strong> the different frequencies <strong>of</strong> manual<br />
irrigation: zero, Πone, two, <strong>and</strong> three times per day. Plots indicate means, <strong>and</strong><br />
error bars represent the st<strong>and</strong>ard errors <strong>of</strong> means. In b, pressures exceeding the measurable limit<br />
(350 mm Hg) <strong>of</strong> the pressure-monitoring device were regarded as 350 mm Hg. Note that degrees<br />
<strong>of</strong> catheter clogging were discriminated by means <strong>of</strong> the pressure measurement system illustrated<br />
in Figure 1. A log 10 scale was used to plot pressure on the y axis.<br />
surfaces, scanning electron microscopy,<br />
or measurement <strong>of</strong> the infusion rate<br />
through a catheter after it was withdrawn.<br />
In our experience, morphologic<br />
analysis is not an effective method because<br />
it is labor intensive <strong>and</strong> tends to<br />
836 Radiology June 2003 Lee et al
Radiology<br />
Figure 4. Graphs show changes in the effective ID <strong>of</strong> drainage catheters in 12 rabbits during the<br />
14-day follow-up. Data were calculated from the pressure measurement (Fig 3) at infusion rates <strong>of</strong><br />
(a) 0.1 <strong>and</strong> (b) 0.5 mL/sec by means <strong>of</strong> fitting Equation (4). Degrees <strong>of</strong> catheter clogging were<br />
graded on the basis <strong>of</strong> the different frequencies <strong>of</strong> manual irrigation: zero, Πone, two,<br />
<strong>and</strong> three times per day. Plots indicate means, <strong>and</strong> error bars represent the st<strong>and</strong>ard errors<br />
<strong>of</strong> means. Note that the degree <strong>of</strong> catheter clogging (effective IDs) is monitored comparatively.<br />
TABLE 2<br />
Results <strong>of</strong> Statistical Analysis <strong>of</strong> Differences in Pressures at Each Irrigation<br />
Frequency in 12 Rabbits during 14-day Follow-up<br />
Irrigation<br />
Frequency<br />
(no. <strong>of</strong> times daily)<br />
result in sampling error <strong>and</strong> because it is<br />
practically impossible to prepare the<br />
catheters without losing debris. For these<br />
reasons, we did not statistically analyze<br />
stereomicroscopic <strong>and</strong> scanning electron<br />
No. <strong>of</strong> Days after Catheter Insertion<br />
0 3 7 10 14<br />
Saline infusion rate,<br />
0.1 mL/sec<br />
0 vs 1 .964 .101 .011* .001* .001*<br />
0 vs 2 .995 .076 .001* .001* .001*<br />
0 vs 3 .965 .028* .001* .001* .001*<br />
1 vs 2 .960 .894 .392 .103 .042*<br />
1 vs 3 .929 .573 .059 .001* .001*<br />
2 vs 3 .970 .666 .299 .036* .019*<br />
Saline infusion rate,<br />
0.5 mL/sec<br />
0 vs 1 .987 .029* .001* .001* .001*<br />
0 vs 2 .746 .008* .001* .001* .001*<br />
0 vs 3 .813 .002* .001* .001* .001*<br />
1 vs 2 .734 .644 .084 .013* .001*<br />
1 vs 3 .800 .332 .008* .001* .001*<br />
2 vs 3 .931 .611 .340 .013* .001*<br />
Note.—Data are P values obtained by means <strong>of</strong> repeated measures analysis <strong>of</strong> variance.<br />
* P .05.<br />
microscopic data in this study. These<br />
methods to determine the degree <strong>of</strong> catheter<br />
clogging necessitated prolonged experimental<br />
cycles <strong>and</strong> required the use <strong>of</strong><br />
many animals for multiple observation<br />
times; these factors resulted in the unavoidable<br />
loss <strong>of</strong> animals <strong>and</strong> catheters.<br />
With the method we developed for the<br />
current study, however, several catheters<br />
could be followed over time in one animal,<br />
which provided quantitative <strong>and</strong><br />
comparative information about temporal<br />
characteristics <strong>of</strong> the obstruction process<br />
or anticlogging effect. This feature is critical<br />
for the evaluation <strong>of</strong> drainage procedures<br />
or for the development <strong>of</strong> new<br />
drainage catheters with anticlogging effects<br />
(ie, those involving novel biomaterials<br />
or drug-delivery systems). Furthermore,<br />
the method used in this study does<br />
not preclude analyses <strong>of</strong> weight or morphologic<br />
changes after catheter withdrawal.<br />
This method might also be used<br />
in clinical studies because the amount <strong>of</strong><br />
saline injected is small (less than 10 mL<br />
per catheter in this study); that amount is<br />
not enough to significantly increase the<br />
pressure inside the abscess cavity.<br />
However, the method used in this<br />
study has several limitations. (a) Despite<br />
the advantage <strong>of</strong> allowing direct assessment<br />
<strong>of</strong> flow through a catheter in vivo,<br />
the direction <strong>of</strong> the infused flow during<br />
the measurement is opposed to the direction<br />
<strong>of</strong> natural drainage. This might be a<br />
substantial limitation because debris inside<br />
a drainage system can act as a oneway<br />
check valve. (b) The Poiseuille law<br />
can be applied only if an assumption is<br />
made that narrowing <strong>of</strong> the lumen is diffuse<br />
(7), but this assumption does not<br />
reflect the real situation. In cases <strong>of</strong> multifocal<br />
severe obstruction, the flow dynamics<br />
become more complex.<br />
With the Poiseuille law, we derived a<br />
fitting equation from the in vitro experimental<br />
data <strong>and</strong> used the equation to<br />
calculate the effective ID <strong>of</strong> catheters in<br />
the animal experiment. However, this<br />
method also has several limitations. For<br />
example, in the animal experiment, the<br />
ID <strong>of</strong> catheters was 5.07 F, but the ID <strong>of</strong><br />
the same catheters calculated from the<br />
baseline measurement was approximately<br />
3.5 F. This discrepancy might be attributed<br />
to multiple factors. (a) Intracatheter pressure<br />
for a given catheter in vivo can be<br />
variable since it is influenced by many<br />
factors, including the respiratory cycle,<br />
abdominal pressure, <strong>and</strong> locations <strong>of</strong> side<br />
holes relative to adjacent anatomic structures.<br />
(b) <strong>Catheters</strong> used in the in vitro<br />
experiment had only one end hole. (c)<br />
Mechanical properties, such as the compliance<br />
materials, were not considered in<br />
this study. We believe, however, that<br />
these limitations are not important if the<br />
method is used for comparing the de-<br />
Volume 227 Number 3 <strong>Clogging</strong> <strong>of</strong> <strong>Drainage</strong> <strong>Catheters</strong>: Assessment <strong>of</strong> Intracatheter Pressure 837
Radiology<br />
grees <strong>of</strong> catheter clogging between different<br />
catheters.<br />
We found a discrepancy between the<br />
curves generated by the fitting Equation<br />
(4) <strong>and</strong> those generated by the Poiseuille<br />
equation (Eq [2]). Furthermore, intracatheter<br />
pressure was found to be proportional<br />
to the square <strong>of</strong> the infusion rate<br />
<strong>and</strong> not to the infusion rate, as indicated<br />
by fitting Equation (4). This discrepancy<br />
might be attributed to technical factors<br />
or to the fact that the system is not modeled<br />
perfectly by the Poiseuille law. The<br />
reasons for these differences remain unknown,<br />
<strong>and</strong> further study is required.<br />
In summary, we propose a method for<br />
in vivo evaluation <strong>of</strong> the effectiveness <strong>of</strong><br />
a drainage catheter, which is based on<br />
the application <strong>of</strong> the Poiseuille law.<br />
With this method, the flow resistance <strong>of</strong><br />
a catheter can be determined quantitatively;<br />
thus, it <strong>of</strong>fers a means <strong>of</strong> quantifying<br />
the degree <strong>of</strong> clogging or the anticlogging<br />
effect <strong>of</strong> drainage catheters. This<br />
method can be used for comparative <strong>and</strong><br />
longitudinal studies concerning the evaluation<br />
<strong>of</strong> drainage procedures or the development<br />
<strong>of</strong> new catheters.<br />
Practical application: By applying the<br />
noninvasive method used in this study,<br />
flow resistance through multiple drainage<br />
catheters can be compared over time<br />
in one animal, which provides quantitative<br />
information about the gradual obstruction<br />
<strong>of</strong> catheters. This information<br />
is critical for the evaluation <strong>of</strong> drainage<br />
procedures or development <strong>of</strong> new catheters<br />
with anticlogging effects, such as<br />
those made with novel biomaterials <strong>and</strong><br />
drug-delivery systems. Furthermore, this<br />
method does not preclude analyses based<br />
Figure 5. Images show internal surfaces <strong>of</strong> drainage catheters after the catheters were withdrawn.<br />
(a) Stereomicroscopic image shows debris that plugs the catheter side holes <strong>and</strong> lumen,<br />
which were irrigated one time per day. (b) Scanning electron microscopic image shows a catheter<br />
that was irrigated two times per day. Note the irregular surface caused by the debris (D). (Original<br />
magnification, 170.)<br />
on weight or morphologic changes after<br />
the catheter is withdrawn.<br />
Acknowledgments: We thank Hyuk Jae<br />
Choi, Myoung Soo Kim, RT, <strong>and</strong> Hyun Jung<br />
Lee, RT, for their technical assistance in animal<br />
preparation. We are grateful to Myoung Jin<br />
Jang, PhD, for her help with the statistical<br />
analysis.<br />
References<br />
1. Haaga JR, Weinstein AJ. CT-guided percutaneous<br />
aspiration <strong>and</strong> drainage <strong>of</strong> abscesses.<br />
Am J Roentgenol 1980; 135:1187–<br />
1194.<br />
2. vanSonnenberg E, Mueller PR, Ferrucci JT<br />
Jr. Percutaneous drainage <strong>of</strong> 250 abdominal<br />
abscesses <strong>and</strong> fluid collections. I. Results,<br />
failures, <strong>and</strong> complications. Radiology<br />
1984; 151:337–341.<br />
3. Mueller PR, vanSonnenberg E, Ferrucci JT<br />
Jr. Percutaneous drainage <strong>of</strong> 250 abdominal<br />
abscesses <strong>and</strong> fluid collections. II. Current<br />
procedural concepts. Radiology 1984;<br />
151:343–347.<br />
4. Dawson SL, Mueller PR, Ferrucci JT Jr. Mucomyst<br />
for abscesses: a clinical comment.<br />
Radiology 1984; 151:342.<br />
5. Park JK, Kraus FC, Haaga JR. Fluid flow<br />
during percutaneous drainage procedures:<br />
an in vitro study <strong>of</strong> the effects <strong>of</strong> fluid<br />
viscosity, catheter size, <strong>and</strong> adjunctive<br />
urokinase. Am J Roentgenol 1993; 160:165–<br />
169.<br />
6. Han JK. Percutaneous abdominal abscess<br />
drainage. In: Han MC, Park JH, eds. Interventional<br />
radiology. Seoul, Korea: Ilchokak,<br />
1999; 707–714.<br />
7. Pfitzner J. Poiseuille <strong>and</strong> his law. Anaesthesia<br />
1976; 31:273–275.<br />
8. Frazini JB, Finnemore EJ, eds. Fluid mechanics<br />
with engineering applications. Appendix<br />
A. 9th ed. Boston, Mass: McGraw-<br />
Hill, 1997; 764–765.<br />
9. Moon HT, Lee YK, Han JK, Byun Y. A novel<br />
formulation for controlled release <strong>of</strong> heparin-DOCA<br />
conjugate dispersed as nanoparticles<br />
in polyurethane film. Biomaterials<br />
2001; 22:281–289.<br />
838 Radiology June 2003 Lee et al