Use of Transdermal Fentanyl - St Elizabeth Hospice
Use of Transdermal Fentanyl - St Elizabeth Hospice
Use of Transdermal Fentanyl - St Elizabeth Hospice
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
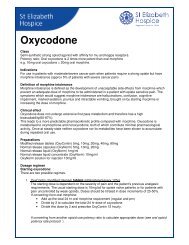
<strong>Use</strong> <strong>of</strong> <strong>Transdermal</strong> <strong>Fentanyl</strong><br />
Introduction<br />
<strong>Fentanyl</strong> is an alternative strong opioid for stable moderate to severe opioid responsive pain.<br />
It is available as a transdermal patch with duration <strong>of</strong> action <strong>of</strong> 72 hours. Due to its long half life<br />
<strong>Transdermal</strong> fentanyl takes 12-24 hours to reach therapeutic drug levels following application therefore it<br />
is not appropriate to use fentanyl in patients who need rapid titration <strong>of</strong> their medication for severe<br />
uncontrolled pain.<br />
Indications<br />
• Where oral or subcutaneous routes are inappropriate or unacceptable<br />
• Poor absorption(e.g. inflammatory bowel disease, intractable nausea and vomiting)<br />
• Dysphagia<br />
• Intractable morphine induced constipation or other unacceptable side effects with morphine<br />
• Compliance is poor but supervised patch application is possible<br />
• Mild to Moderate Renal failure<br />
Cautions<br />
• In treatment <strong>of</strong> unstable pain<br />
• Avoid exposure to external heat sources e.g. hot water bottles, hot baths as these may cause<br />
increased delivery rate, resulting in toxicity<br />
• Elderly and debilitated patients: toxicity more likely<br />
• <strong>Fentanyl</strong>, as with all other strong opioids should be used with caution in severe liver and renal<br />
disease.<br />
GENERAL POINTS<br />
• Prescribe generically stating which type <strong>of</strong> patch is being used, either matrix or reservoir. Patients<br />
should remain on same type/brand <strong>of</strong> patch to avoid potential differences in bioavailability.<br />
• Apply to intact normal, non-hairy skin avoiding irradiated areas, scar tissue or oedematous skin.<br />
• Patches should be changed every 3 days applying each new patch to a different skin site.<br />
• In a small proportion <strong>of</strong> patients the patch appears to lose efficacy after 48 hours. Usually this is<br />
because the dose needs to be increased but a small percentage <strong>of</strong> patients do better if the patch<br />
is changed every 2 days.<br />
• <strong>St</strong>eady-state plasma concentrations <strong>of</strong> fentanyl are achieved after 36-48h; the patient should<br />
therefore use prn doses <strong>of</strong> immediate release opiate during the first 3 days<br />
• A normal release opioid e.g. oral morphine or diamorphine SC must be available prn for<br />
breakthrough pain or to counteract any opioid withdrawal syndrome which can occur during the<br />
fentanyl initiation period. The correct 4 hourly equivalent dose should be used (see fentanyl dose<br />
conversion chart)<br />
• Avoid direct contact with heat which increases drug absorption e.g. hot water bottle, electric<br />
blanket<br />
• Showering is possible as patches are waterpro<strong>of</strong> but avoid soaking in a hot bath.<br />
• If patch adherence is poor, use micropore tape or an adhesive dressing such as Tegaderm.<br />
DriClor antiperspirant roll-on can be applied prior to patch application to improve adhesiveness
• <strong>Fentanyl</strong> is unsuitable for patients with marked sweating or persistent fever. Allergy to the silicone<br />
medical adhesive may occur and necessitate change to alternative opioid.<br />
• After removal patches should be folded firmly in half so that the adhesive is not exposed and<br />
disposed <strong>of</strong> safely as they may contain significant residues <strong>of</strong> fentanyl.<br />
• <strong>Fentanyl</strong> is less constipating than morphine and it may be necessary to reduce the dose <strong>of</strong><br />
laxatives.<br />
• Some patients experience opioid withdrawal symptoms when changed from morphine to TD<br />
<strong>Fentanyl</strong> despite satisfactory pain relief. These manifest with symptoms <strong>of</strong> colic, diarrhoea,<br />
nausea, sweating and restlessness and may last for a few days; prn doses <strong>of</strong> immediate release<br />
morphine can be used to relieve troublesome symptoms.<br />
NB Durogesic D-Trans is superior to other fentanyl patches in terms <strong>of</strong> adhesion. It is important<br />
to note that changing from one brand <strong>of</strong> patch to another may not be exactly equivalent in dose.<br />
INITIATION OF FENTANYL<br />
• Patient should be on a stable dose <strong>of</strong> strong opioid equivalent to about 30-60mg oral morphine /<br />
24 hours before a fentanyl patch is initiated.<br />
• Calculate the dose <strong>of</strong> fentanyl from the data sheet conversion chart below or seek advice.<br />
FENTANYL PATCH CONVERSION CHART<br />
4 hrly, immediate release oral morphine<br />
dose (mg)<br />
<strong>Fentanyl</strong><br />
patch dose<br />
(micrograms/hour)<br />
24 hour oral morphine<br />
dose(mg)<br />
2.5 -10 12 < 60<br />
5 - 20 25 < 135<br />
25 – 35 50 135 – 224<br />
40 – 50 75 225 – 314<br />
55 – 65 100 315 – 404<br />
70 – 80 125 405 – 494<br />
85 – 95 150 495 – 584<br />
100 – 110 175 585 – 674<br />
115 – 125 200 675 – 764<br />
130 – 140 225 765 – 854<br />
145 – 155 250 855 – 944<br />
160 – 170 275 945 – 1034<br />
175 – 185 300 1035 - 1125<br />
• Five patch sizes are available 12, 25, 50, 75, 100 micrograms/hour.<br />
• Patches can be combined to achieve desired dose.<br />
• Systemic analgesic concentrations are generally reached within 12hr; so if converting from:<br />
a. 4hrly oral morphine, give regular doses for the first 12 hr after applying the patch.<br />
b. 12hrly m/r morphine, apply the patch and give the final m/r dose at the same time.<br />
c. A syringe driver, continue the syringe driver for about 12hr after applying the patch.<br />
ADJUSTING FENTANYL PATCH DOSE<br />
• If patient shows signs <strong>of</strong> opiate toxicity e.g. drowsiness, confusion, myoclonic jerks, pinpoint<br />
pupils, reduce the dose and reassess the pain.<br />
• After 48 hrs, if a patient continues to need 2 or more rescue doses <strong>of</strong> morphine a day, the patch<br />
strength should be increased by 25microgram/h. Remember it will take 12-24 hrs for the<br />
increased dose to take effect.
USE OF TRANSDERMAL FENTANYL IN THE TERMINAL STAGES<br />
• In moribund patients, it is best to continue the transdermal fentanyl and give rescue doses <strong>of</strong><br />
morphine or diamorphine calculated according to the fentanyl conversion chart.<br />
• If >2 prn doses/24h are required consider giving morphine or diamorphine via CSCI<br />
• In an unstable pain situation it may be necessary to remove the patch and start a syringe driver.<br />
PLEASE SEEK SPECIALIST ADVICE<br />
CONVERTING FROM TRANSDERMAL FENTANYL TO ORAL OPIATES<br />
o <strong>Fentanyl</strong> is mainly excreted by hepatic metabolism to inactive metabolites but a reservoir <strong>of</strong><br />
fentanyl accumulates in the skin under the patch. Significant blood levels can persist for 12-24<br />
hours after the patch is removed.<br />
o Remove fentanyl patch but do not start the patient on regular oral morphine until 12 hours after<br />
the patch has been removed because there will be an existing subcutaneous reservoir <strong>of</strong><br />
fentanyl.<br />
o When converting from fentanyl to immediate release oral morphine use the lower dose<br />
indicated in the range on the conversion chart to calculate the equivalent 4 hrly dose <strong>of</strong> oral<br />
morphine. If an alternative strong opiate is being prescribed calculate the equivalent dose from<br />
the oral opiate potency ratios guideline<br />
o Ensure that an immediate release oral opiate e.g. morphine is prescribed prn for the first 12<br />
hours after removing the fentanyl patch.<br />
o 12 hours after removing the patch prescribe a regular dose oral opiate either q4hrly immediate<br />
release morphine or modified release preparation every q12hrly.This dose can be calculated from<br />
the fentanyl conversion chart.<br />
CONVERTING FROM TRANSDERMAL FENTANYL TO SUBCUTANEOUS MORPHINE<br />
1. Calculate the equivalent 24 hour oral morphine dose from the fentanyl conversion chart.<br />
2. <strong>Use</strong> the mid dose <strong>of</strong> the range given<br />
3. Divide this dose by 2 to calculate the dose <strong>of</strong> morphine/24 hours SC.<br />
4. Commence CSCI 12 hours after removal <strong>of</strong> fentanyl patch<br />
CONVERTING FROM TRANSDERMAL FENTANYL TO SUBCUTANEOUS DIAMORPHINE<br />
1. Calculate the equivalent 24 hour oral morphine dose from the fentanyl conversion chart.<br />
2. <strong>Use</strong> the mid-dose <strong>of</strong> the range given<br />
3. Divide this dose by 3 to calculate the 24hour dose <strong>of</strong> diamorphine SC<br />
4. Commence CSCI 12 hours after removal <strong>of</strong> fentanyl patch<br />
References<br />
1. <strong>Fentanyl</strong> TTS data sheet. Summary <strong>of</strong> product characteristics. http://www.medicines.org.uk/ Jan<br />
2008<br />
2. British National formulary No 54. September 2007. http://bnf.org<br />
3. Palliative Care Formulary .third edition 2008. Twycross R + Wilcock A<br />
4. Ahmedzai S, Brooks D. <strong>Transdermal</strong> fentanyl versus sustained release oral morphine in cancer pain;<br />
preference, efficacy and quality <strong>of</strong> life. Journal <strong>of</strong> Pain and Symptom Management 1997;13:254-261<br />
5. Portenoy RK, et al.<strong>Transdermal</strong> <strong>Fentanyl</strong> for cancer pain. Anaesthesiology 1993;78: 36-43<br />
6. Fine PG. <strong>Fentanyl</strong> in the treatment <strong>of</strong> cancer pain. Seminars in Oncology .1997; 24: 20-27<br />
7. Donner B et al. Long term treatment <strong>of</strong> cancer pain with transdermal fentanyl. Journal <strong>of</strong> Pain and<br />
Symptom Management 1998;15: 168-175