Annual Report - Central Manchester University Hospitals - NHS ...
Annual Report - Central Manchester University Hospitals - NHS ...
Annual Report - Central Manchester University Hospitals - NHS ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
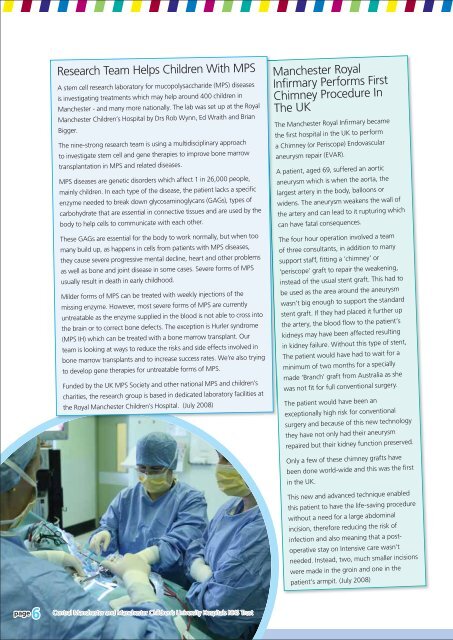
Research Team Helps Children With MPS<br />
A stem cell research laboratory for mucopolysaccharide (MPS) diseases<br />
is investigating treatments which may help around 400 children in<br />
<strong>Manchester</strong> - and many more nationally. The lab was set up at the Royal<br />
<strong>Manchester</strong> Children’s Hospital by Drs Rob Wynn, Ed Wraith and Brian<br />
Bigger.<br />
The nine-strong research team is using a multidisciplinary approach<br />
to investigate stem cell and gene therapies to improve bone marrow<br />
transplantation in MPS and related diseases.<br />
MPS diseases are genetic disorders which affect 1 in 26,000 people,<br />
mainly children. In each type of the disease, the patient lacks a specific<br />
enzyme needed to break down glycosaminoglycans (GAGs), types of<br />
carbohydrate that are essential in connective tissues and are used by the<br />
body to help cells to communicate with each other.<br />
These GAGs are essential for the body to work normally, but when too<br />
many build up, as happens in cells from patients with MPS diseases,<br />
they cause severe progressive mental decline, heart and other problems<br />
as well as bone and joint disease in some cases. Severe forms of MPS<br />
usually result in death in early childhood.<br />
Milder forms of MPS can be treated with weekly injections of the<br />
missing enzyme. However, most severe forms of MPS are currently<br />
untreatable as the enzyme supplied in the blood is not able to cross into<br />
the brain or to correct bone defects. The exception is Hurler syndrome<br />
(MPS IH) which can be treated with a bone marrow transplant. Our<br />
team is looking at ways to reduce the risks and side effects involved in<br />
bone marrow transplants and to increase success rates. We’re also trying<br />
to develop gene therapies for untreatable forms of MPS.<br />
Funded by the UK MPS Society and other national MPS and children’s<br />
charities, the research group is based in dedicated laboratory facilities at<br />
the Royal <strong>Manchester</strong> Children’s Hospital. (July 2008)<br />
<strong>Manchester</strong> Royal<br />
Infirmary Performs First<br />
Chimney Procedure In<br />
The UK<br />
T<br />
The <strong>Manchester</strong> Royal Infirmary became<br />
the first hospital in the UK to perform<br />
a Chimney (or Periscope) Endovascular<br />
aneurysm repair (EVAR).<br />
A patient, aged 69, suffered an aortic<br />
aneurysm which is when the aorta, the<br />
largest artery in the body, balloons or<br />
widens. The aneurysm weakens the wall of<br />
the artery and can lead to it rupturing which<br />
can have fatal consequences.<br />
The four hour operation involved a team<br />
of three consultants, in addition to many<br />
support staff, fitting a ‘chimney’ or<br />
‘periscope’ graft to repair the weakening,<br />
instead of the usual stent graft. This had to<br />
be used as the area around the aneurysm<br />
wasn’t big enough to support the standard<br />
stent graft. If they had placed it further up<br />
the artery, the blood flow to the patient’s<br />
kidneys may have been affected resulting<br />
in kidney failure. Without this type of stent,<br />
The patient would have had to wait for a<br />
minimum of two months for a specially<br />
made ‘Branch’ graft from Australia as she<br />
was not fit for full conventional surgery.<br />
The patient would have been an<br />
exceptionally high risk for conventional<br />
surgery and because of this new technology<br />
they have not only had their aneurysm<br />
repaired but their kidney function preserved.<br />
Only a few of these chimney grafts have<br />
been done world-wide and this was the first<br />
in the UK.<br />
This new and advanced technique enabled<br />
this patient to have the life-saving procedure<br />
without a need for a large abdominal<br />
incision, therefore reducing the risk of<br />
infection and also meaning that a postoperative<br />
stay on Intensive care wasn’t<br />
needed. Instead, two, much smaller incisions<br />
were made in the groin and one in the<br />
patient’s armpit. (July 2008)<br />
page 6<br />
<strong>Central</strong> <strong>Manchester</strong> and <strong>Manchester</strong> Children’s <strong>University</strong> <strong>Hospitals</strong> <strong>NHS</strong> Trust