CONNECTIVE TISSUES I. Introduction A ... - Faculty.rmc.edu
CONNECTIVE TISSUES I. Introduction A ... - Faculty.rmc.edu
CONNECTIVE TISSUES I. Introduction A ... - Faculty.rmc.edu
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
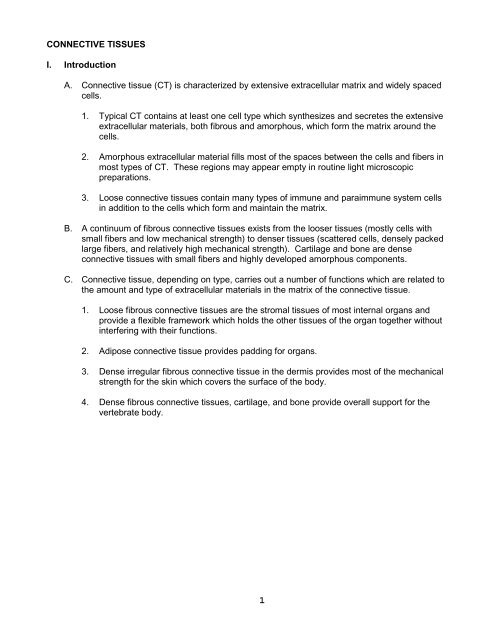
<strong>CONNECTIVE</strong> <strong>TISSUES</strong><br />
I. <strong>Introduction</strong><br />
A. Connective tissue (CT) is characterized by extensive extracellular matrix and widely spaced<br />
cells.<br />
1. Typical CT contains at least one cell type which synthesizes and secretes the extensive<br />
extracellular materials, both fibrous and amorphous, which form the matrix around the<br />
cells.<br />
2. Amorphous extracellular material fills most of the spaces between the cells and fibers in<br />
most types of CT. These regions may appear empty in routine light microscopic<br />
preparations.<br />
3. Loose connective tissues contain many types of immune and paraimmune system cells<br />
in addition to the cells which form and maintain the matrix.<br />
B. A continuum of fibrous connective tissues exists from the looser tissues (mostly cells with<br />
small fibers and low mechanical strength) to denser tissues (scattered cells, densely packed<br />
large fibers, and relatively high mechanical strength). Cartilage and bone are dense<br />
connective tissues with small fibers and highly developed amorphous components.<br />
C. Connective tissue, depending on type, carries out a number of functions which are related to<br />
the amount and type of extracellular materials in the matrix of the connective tissue.<br />
1. Loose fibrous connective tissues are the stromal tissues of most internal organs and<br />
provide a flexible framework which holds the other tissues of the organ together without<br />
interfering with their functions.<br />
2. Adipose connective tissue provides padding for organs.<br />
3. Dense irregular fibrous connective tissue in the dermis provides most of the mechanical<br />
strength for the skin which covers the surface of the body.<br />
4. Dense fibrous connective tissues, cartilage, and bone provide overall support for the<br />
vertebrate body.<br />
1
II.<br />
Components of Connective Tissue<br />
A. Extracellular matrix (ECM) may include fibers and amorphous materials.<br />
1. Fibrous Components<br />
a. Collagenous Fibers (Table 6.2 and Figs. 6.5 - 6.8)<br />
(1) Collagen fibers in fibrous connective tissue and bone are primarily Type I<br />
collagen. Collagen fibers in cartilage are Type II collagen.<br />
(a) Typical fibrous connective tissue collagen fibers consist of bundles of Type<br />
I collagen fibrils. The fibrils measure 20 to 200 nanometers in diameter<br />
and are cross-banded in a complex pattern which repeats every 68 nm<br />
(see Fig. 6.7).<br />
(b) Typical collagen fibers are clearly recognizable in TEM preparations<br />
because of the cross-banding pattern. Collagen fibers are acidophilic in<br />
routine LM preparations and can be specifically stained by a variety of<br />
techniques.<br />
(c) Collagen fibers are "bendable" but not "stretchable" (steel cable-like<br />
properties) and therefore limit stretching of a tissue in the direction in which<br />
the fibers run. The larger the bundles of fibrils, the more restricted the<br />
stretch of the tissue.<br />
(2) Reticular fibers (usually Type III collagen) (Fig. 6.12)<br />
(a) Reticular fibers are small intertwining bundles or single collagen fibrils<br />
(usually about 20 nanometers in diameter) which form a meshwork.<br />
(b) Reticular fibers can be recognized in TEM by the small bundles, the more<br />
uniform diameter of the fibrils, and the relative lack of cross-banding.<br />
Reticular fibers are not visible in routine LM preparations, but are easily<br />
visible by LM following silver staining.<br />
(c) Reticular fibers form the reticular layer in basement membranes and are<br />
important in the stroma of many glands.<br />
b. Elastic Fibers (Fig. 6.13 - 6.15)<br />
(1) Elastic fibers are a combination of amorphous elastin plus a microfibrillar<br />
component. In the absence of the microfibrillar component, elastin sheets or<br />
laminae are formed.<br />
(2) Elastic fibers can be recognized by TEM because of their structure. Elastic<br />
fibers are frequently slightly more acidophilic than collagen fibers in routine LM<br />
preparations and can be identified by specific staining (resorcin-fuchsin, etc.).<br />
(3) Elastic fibers are highly elastic (stretchable, return to original length when<br />
released).<br />
2
2. Amorphous Components lack recognizable structure in either TEM or LM. Amorphous<br />
components were referred to in the past as "ground substance". Various amorphous<br />
components may be complexed with each other and with fibrous components. This<br />
material may complex with minerals to form the rigid ECM found in bony tissue.<br />
a. Amorphous components of ECM may include many types of chemicals.<br />
(1) Proteins of many types occur in ECM.<br />
(2) Glycoproteins (proteins with added oligosaccharide groups)(Table 6.5, Fig.<br />
6.18) which occur in relatively large amounts as amorphous components in<br />
ECM include fibronectin, laminin, some types of collagen, etc. Fibronectin links<br />
different ECM components and allows attachment of cells to extracellular<br />
matrix. Laminin serves similar functions in basal lamina.<br />
(3) Glycosaminoglycans (GAGs) (Table 6.3, Fig. 6.16) are polysaccharides<br />
consisting of disaccharide units, at least one of which is sulfated or contains a<br />
carboxylic acid side chain. The acidic groups result in highly acidic<br />
characteristics for the entire GAG, making them highly basophilic. Most GAGs<br />
have a molecular weight of about 10,000-50,000, but hyaluronic acid may have<br />
a molecular weight of 1 million.<br />
(4) Proteoglycans (Figs. 6.16, 6.17) consist of GAGs assembled on a core protein<br />
to form a very large molecule (about 2 million Dalton in some cases).<br />
(5) Proteoglycan Aggregates (Fig. 6.16, 6.17) usually consists of proteoglycans<br />
assembled onto a hyaluronic acid molecule to form a complex "supermolecule"<br />
which may have a volume larger than a mitochondrion.<br />
3. Tissue Fluid is the extracellular fluid in connective tissue as well as in other tissues.<br />
Since tissue fluid is formed by exchange with blood plasma across endothelial layers,<br />
tissue fluid is approximately equal to blood plasma minus most of the plasma proteins.<br />
3
B. Cells in connective tissues<br />
1. Resident or permanent cells<br />
a. Matrix-forming and maintaining cells are responsible for the synthesis and<br />
secretion of the fibrous and amorphous components of the ECM of the different<br />
types of CT.<br />
(1) Mesenchyme cells<br />
(a) True mesenchyme cells occur only in embryos and are derived from<br />
mesoderm or from neural crest. Mesenchyme cells can differentiate into all<br />
types of adult matrix forming cells.<br />
(b) Mesenchyme cells are spindle-shaped or stellate with a large nucleus<br />
(usually with distinct nucleolus) and relatively little cytoplasm, often forming<br />
thin processes.<br />
(c) Mesenchyme cells produce primarily GAGs and proteoglycans, especially<br />
hyaluronic acid.<br />
(d) Cells with similar properties found in adult CT are called mesenchymal<br />
stem cells and appear to function in tissue repair.<br />
(2) Fibroblasts (and fibrocytes)(Figs. 6.19, 6.20, 6.8)<br />
(a) Fibroblasts occur in all adult fibrous connective tissues.<br />
(b) Fibroblasts are large, flattened (spindle-shaped in sections) cells with oval<br />
or elongated nuclei containing both euchromatin and heterochromatin and<br />
usually containing an obvious nucleolus. Fibrocytes have flattened<br />
heterochromatic nuclei. Fibroblast cytoplasm is slightly basophilic (due to<br />
extensive rER) if the cell is very active and slightly acidophilic if the cell is<br />
inactive. Fibroblasts typically have long thin cytoplasmic processes which<br />
are visible with TEM.<br />
(c) Fibroblasts secrete collagen fiber bundles, reticular fibers, elastics fibers,<br />
GAGs, and glycoproteins.<br />
(d) Myofibroblasts are fibroblastic cells which contain elaborated actin filament<br />
bundles and are therefore contractile. Myofibroblasts appear to be<br />
important in wound closure.<br />
(3) Reticular cells (Plate 34)<br />
(a) Reticular cells occur only in reticular connective tissue. Reticular<br />
connective tissue is usually the stromal component of lymphoid tissue.<br />
(b) Reticular cells are stellate cells with long cellular processes which make<br />
contact with other cells. The processes of reticular cells surround the<br />
reticular fibers in the ECM of reticular CT. Reticular cells have large nuclei<br />
with distinct nucleoli.<br />
4
(c) Reticular cells secrete reticular fibers and GAGs. Some reticular cells are<br />
probably also phagocytic.<br />
(4) Chondroblasts and chondrocytes (Figs. 7.4 - 7.7, Plate 7)<br />
(a) Chondroblasts and chondrocytes occur only in cartilage.<br />
(b) Chondroblasts and healthy chondrocytes are large spherical to oval cells<br />
with basophilic cytoplasm and oval nuclei containing distinct nucleoli.<br />
Degenerating or poorly preserved chondrocytes frequently appear<br />
shrunken and contain small predominately heterochromatic nuclei.<br />
(c) Chondroblasts and chondrocytes may synthesize and secrete collagen<br />
(which forms small reticular fiber-like arrays in most cartilage or collagen<br />
fiber bundles in fibrocartilage), elastin (which forms visible elastic fibers in<br />
elastic cartilage), GAGs, and proteoglycans.<br />
(5) Osteoblasts (Figs. 8.7 - 8.9)<br />
(a) Osteoblasts are found only on or near growing surfaces of bone tissue.<br />
(b) Osteoblasts are roughly cuboidal cells with spherical to oval nuclei (often<br />
with visible nucleoli) and basophilic cytoplasm. Osteoblasts become<br />
stellate with fine processes when they are surrounded by bone matrix.<br />
(c) Osteoblasts synthesize and secrete the organic components of bone<br />
matrix, consisting of collagen (which forms fine collagen fiber bundles),<br />
GAGs, glycoproteins, and proteoglycans. Osteoblasts also pinch off from<br />
their surfaces the alkaline phosphatase-rich matrix vesicles which initiate<br />
mineralization of immature bone.<br />
(6) Osteocytes (Fig. 8.10)<br />
(a) Osteocytes are found only in formed bone matrix.<br />
(b) Osteocytes are stellate (with thin processes) cells with spherical to oval<br />
nuclei and weakly basophilic or unstained cytoplasm. Osteocytes are very<br />
poorly preserved in most preparations.<br />
(c) Osteocytes normally "maintain" bone matrix, but they are capable of small<br />
amounts of net synthesis or net resorption of bone matrix.<br />
5
. Matrix-removing cells<br />
(1) Osteoclasts (Figs. 8.12 - 8.15)<br />
(a) Osteoclasts occur on and near surfaces where bone matrix is being resorbed.<br />
(b) Osteoclasts are large multinucleate cells with acidophilic cytoplasm containing<br />
numerous acid phosphatase- rich lysosomes. The surface of the osteoclast<br />
next to the bone matrix has numerous infoldings in the plasma membrane<br />
which form a ruffled border.<br />
(c) Osteoclasts resorb bone matrix by releasing lysosomes and organic acids onto<br />
the bone matrix surface. Osteoclasts can also break down cartilage matrix<br />
trapped in bone matrix during endochondrial bone formation. Osteoclasts can<br />
be formed from monocytes and are therefore related to macrophages.<br />
c. Storage cells<br />
(1) White fat cells (white adipocytes) (Figs 9.1 - 9.3)<br />
(a) White adipocytes occur in loose connective tissues and are the dominant cells<br />
in white adipose connective tissue.<br />
(b) White adipocytes are large spherical cells with a flattened eccentric nucleus in a<br />
thin rim of cytoplasm surrounding a single large central fat droplet.<br />
(c) White adipocytes are the major fat storage cells in adult humans.<br />
(d) White adipocytes develop from the same precursor cells that give rise to<br />
fibroblasts, but the control of their development is unclear.<br />
(2) Brown fat cells (brown adipocytes) (Figs 9.1, 9.4)<br />
(a) Brown adipocytes occur in brown fat deposits in embryonic and neonatal<br />
humans but are rare in adult humans.<br />
(b) Brown adipocytes are spherical cells (smaller than white fat cells) containing<br />
spherical eccentric nuclei, multiple small fat droplets, and numerous<br />
mitochondria.<br />
(c) Brown adipocytes are capable of rapid heat generation.<br />
6
2. Transient or migratory cells<br />
a. Macrophages (Fig. 6.22)<br />
(1) Macrophages occur in most loose and moderately dense fibrous connective<br />
tissues. Some macrophages may be relatively long-term residents of<br />
connective tissues while other macrophages are clearly migratory.<br />
(2) Two types of macrophages are frequently described, but the relationships<br />
between these morphological categories and functional categories are unclear.<br />
Most macrophages are probably quite variable in morphology and are capable<br />
of rapid changes in function in response to chemical signals.<br />
(a) "Fixed" macrophages are associated with CT fibers and therefore tend to<br />
have a more elongated shape.<br />
(b) Free macrophages are not associated with CT fibers and tend to be more<br />
oval in shape.<br />
(3) Macrophages usually appear in routine LM preparations as flattened cells<br />
(slightly smaller than fibroblasts) with football- shaped to kidney bean-shaped<br />
nuclei containing both euchromatin and heterochromatin.<br />
Macrophage nuclei are usually slightly smaller and slightly darker staining<br />
than fibroblast nuclei in the same preparation. Macrophages are difficult to<br />
distinguish from fibroblasts, so positive identification depends on detection of<br />
specific cell surface markers which are unique to macrophages.<br />
Newly developed macrophages have weakly acidophilic cytoplasm containing<br />
lysosomal granules (acid phosphatase positive). Activated macrophages<br />
contain cytoplasm filled with obvious granules of undigested material. Most<br />
macrophages have elongated processes which are not obvious by LM but<br />
which are seen with TEM and SEM.<br />
(4) Macrophages are phagocytic cells derived from monocytes. Macrophages are<br />
important in removal of debris from connective tissues, in stimulating immune<br />
responses, and in defense against some types of bacteria and some types of<br />
tumor cells.<br />
7
. Lymphocytes (Fig. 10.11, Plate 4, Fig. 4)<br />
(1) Lymphocytes occur in loose connective tissues and are the most abundant cell<br />
type in lymphoid tissue.<br />
(2) Lymphocytes have small, heterochromatic, spherical nuclei surrounded by very<br />
thin rims of cytoplasm.<br />
(3) Lymphocytes include several functional categories of immune response and<br />
regulatory cells which cannot be distinguished by routine LM.<br />
(a) T lymphocytes are responsible for cell-mediated immunity.<br />
(b) B lymphocytes develop into plasma cells which secrete antibodies.<br />
(c) Natural killer cells kill virus-infected cells and some types of cancer cells.<br />
c. Plasma cells (Fig. 6.25, Plate 4, Fig. 4)<br />
(1) Plasma cells occur in lymphoid tissues and in loose connective tissues.<br />
Plasma cells are especially numerous in loose connective tissue below the<br />
luminal epithelium in the digestive, respiratory, and reproductive tracts.<br />
(2) Plasma cells are large lymphocytes with eccentric spherical or oval nuclei<br />
containing central euchromatin and peripheral heterochromatin ("clock face<br />
nucleus"). The cytoplasm is strongly basophilic due to abundant rough<br />
endoplasmic reticulum and contains a prominent Golgi apparatus near the<br />
center of the cell.<br />
(3) Plasma cells are active antibody synthesizing and secreting cells derived from<br />
B lymphocytes.<br />
d. Neutrophils (Figs. 10.6 - 10.8)<br />
(1) Neutrophils occur in most loose connective tissues.<br />
(2) Neutrophils contain heavily heterochromatic nuclei divided into 3 to 5 lobes.<br />
Their cytoplasm contains numerous secretory granules which are usually very<br />
weakly acidophilic.<br />
(3) Neutrophils are antibacterial cells and accumulate in sites of bacterial<br />
infections.<br />
8
e. Eosinophils (Fig. 10.9)<br />
3. Other cells<br />
(1) Eosinophils occur in small numbers in most loose connective tissues.<br />
(2) Eosinophils have heterochromatic bilobed nuclei and cytoplasm packed with<br />
acidophilic granules which are modified lysosomes.<br />
(3) Eosinophils accumulate around parasitic infections and in areas of allergic<br />
reactions. Eosinophils damage large parasites (like nematodes) by secreting<br />
their modified lysosomes onto the surface of the parasite. Eosinophils<br />
phagocytize antigen-antibody complexes and inactivate several types of<br />
inflammatory molecules released by mast cells.<br />
a. Mast cells (Fig. 6.23)<br />
(1) Mast cells occur in most loose and moderately dense connective tissues and<br />
are most numerous near small blood vessels.<br />
(2) Mast cells are large spherical to oval cells with a spherical nucleus containing<br />
mixed euchromatin and heterochromatin. Mast cell cytoplasm is filled with<br />
numerous basophilic granules.<br />
(3) Mast cell cytoplasmic granules contain approximately 30 different components,<br />
including histamine and heparin (and serotonin in rodents), which increase<br />
permeability of blood vessel walls. Mast cell granules are released in response<br />
to antigen binding to antibodies in receptors on the mast cell surface.<br />
b. Pericytes or perivascular cells (Fig. 6.24)<br />
(1) Pericytes are observed outside the endothelium of capillaries, venules, and<br />
small veins, primarily in loose connective tissues. Pericytes typically share a<br />
continuous basal lamina with adjacent endothelial cells. The basal lamina runs<br />
between the pericyte and the endothelium but also separates the pericyte from<br />
the surrounding connective tissue.<br />
(2) Pericytes are flattened cells with oval nuclei and little cytoplasm.<br />
(3) The functions of pericytes are unclear, but they may be mesenchyme-like cells<br />
which can differentiate into other types of CT cells or they may be muscle-like<br />
cells which alter capillary permeability. Perivascular cells may be one source of<br />
new capillary smooth muscle cells during outgrowth of blood vessels.<br />
9
III. COMPOSITION OF DIFFERENT TYPES OF <strong>CONNECTIVE</strong> TISSUE<br />
Type Cellular Extracellular<br />
Components<br />
Components<br />
Loose Connective Tissues<br />
Mesenchymal Mesenchyme GAGs (e.g.,<br />
CT Cells hyaluronic acid)<br />
Mucous Fibroblasts Very Fine Collagen fibers<br />
CT<br />
GAGs<br />
Loose FECT Fibroblasts Small Collagen fibers<br />
(FibroElastic Macrophages Small Elastic fibers<br />
Connective Adipocytes Reticular fibers<br />
Tissue) Mast Cells GAGs<br />
Neutrophils<br />
proteoglycans<br />
Eosinophils<br />
Lymphocytes<br />
Plasma cells<br />
Perivascular cells<br />
Adipose Adipocytes Reticular fibers<br />
CT (white and/or GAGs<br />
brown)<br />
proteoglycans<br />
Reticular Reticular cells Reticular fibers<br />
CT Lymphocytes GAGs<br />
Plasma cells<br />
proteoglycans<br />
Macrophages<br />
10
Type Cellular Extracellular<br />
Components<br />
Components<br />
Moderately Dense or Intermediate Connective Tissues<br />
Moderately Fibroblasts Collagen fibers<br />
Dense or Macrophages Elastic fibers<br />
Intermediate<br />
Reticular Fibers<br />
FECT<br />
GAGs<br />
Dense Fibrous Connective Tissues<br />
Dense Fibroblasts Very Large Collagen fibers<br />
Irregular Macrophages Elastic fibers<br />
FECT<br />
Reticular fibers<br />
GAGs<br />
Dense Fibroblasts Collagen fibers<br />
Regular<br />
Elastic fibers<br />
FECT<br />
GAGs<br />
Dense Fibroblasts Collagen fibers<br />
Regular Fibrocytes GAGs<br />
Collagenous<br />
CT<br />
Dense Fibroblasts Elastic fibers<br />
Regular<br />
GAGs<br />
Elastic<br />
CT<br />
11
Type Cellular Extracellular<br />
Components<br />
Components<br />
Cartilage<br />
Hyaline Chondroblasts Very Fine Collagen fibers<br />
Cartilage Chondrocytes GAGs<br />
Proteoglycans<br />
Elastic Chondroblasts Fine Elastic fibers<br />
Cartilage Chondrocytes Very Fine Collagen fibers<br />
GAGs<br />
Proteoglycans<br />
Fibro- Chondrocytes Large Collagen fibers<br />
Cartilage<br />
GAGs<br />
Bone<br />
Woven Osteoblasts Collagen fibers<br />
Bone Osteocytes GAGs<br />
(Immature Osteoclasts Proteoglycans<br />
Bone)<br />
Glycoproteins<br />
Hydroxyapatite<br />
Ca 2+ 10(PO 3- 3 ) 6 (OH - ) 2<br />
Spongy Osteoblasts Collagen fibers<br />
Bone Osteocytes GAGs<br />
(Cancellous Osteoclasts Proteoglycans<br />
Bone)<br />
Glycoproteins<br />
Hydroxyapatite<br />
Ca 2+ 10(PO 3- 3 ) 6 (OH - ) 2<br />
Compact Osteoblasts Collagen fibers<br />
Bone Osteocytes GAGs<br />
Osteoclasts<br />
Proteoglycans<br />
Glycoproteins<br />
Hydroxyapatite<br />
Ca 2+ 10(PO 3- 3 ) 6 (OH - ) 2<br />
12
IV. Classifying Fibroelastic Connective Tissue<br />
A. Loose fibroelastic connective tissue (FECT)<br />
1. The ECM usually contains relatively small diameter collagen fibers. Abundant<br />
amorphous extracellular material frequently keeps the fibers separated. The diameter of<br />
collagen fiber bundles is typically smaller than the diameter of the nuclei of the<br />
fibroblasts in the tissue.<br />
2. A wide diversity of cell types occur in the tissue.<br />
a. Fibroblasts are usually present and responsible for production and maintenance of<br />
ECM<br />
b. Blood and immune system cells (granulocytes, lymphocytes, plasma cells), and<br />
macrophages are common in most loose FECTs.<br />
c. White adipose cells are frequently present.<br />
3. Cells are more numerous than in more dense FECT. In very loose FECT the cells may<br />
occupy more volume than the fibers.<br />
B. Moderately dense FECT<br />
1. Fibers are intermediate in size, arrangement and packing relative to loose and dense<br />
FECT.<br />
2. Cells are intermediate in diversity and number relative to loose and dense FECT.<br />
Fibroblasts and macrophages are usually the only abundant cell types.<br />
C. Dense FECT<br />
1. Extensive arrays of large collagen fibers fill most of the volume of the tissue. Collagen<br />
fiber bundle diameters are typically much larger than the diameter of the cells.<br />
2. Fibroblasts are usually the most frequently encountered cell type.<br />
3. Fewer cells per unit volume are present (relative to moderately dense FECT).<br />
13