Interesting Case Series Acquired Absence of the Penis - ePlasty
Interesting Case Series Acquired Absence of the Penis - ePlasty
Interesting Case Series Acquired Absence of the Penis - ePlasty
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
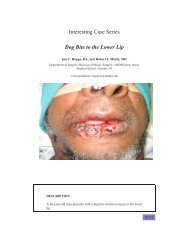
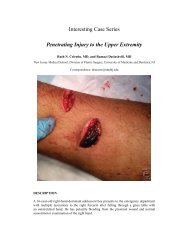
<strong>Interesting</strong> <strong>Case</strong> <strong>Series</strong><strong>Acquired</strong> <strong>Absence</strong> <strong>of</strong> <strong>the</strong> <strong>Penis</strong>Ian C. Hoppe, BA, and Mat<strong>the</strong>w J. Trovato, MDDepartment <strong>of</strong> Surgery, Division <strong>of</strong> Plastic Surgery, New Jersey Medical School–UMDNJ, NewarkCorrespondence: hoppeic@umdnj.eduDESCRIPTIONA 45-year-old man presents with an acquired absence <strong>of</strong> <strong>the</strong> penissecondary to penile resection due to squamous cell carcinoma.NEXT
QUESTIONS1. What are <strong>the</strong> goals for phallic reconstruction?2. What options are available for reconstruction?3. What surgical repair is most appropriate?4. What is <strong>the</strong> long-term course for phallic reconstruction?BACKNEXT
DISCUSSIONSeveral goals should be kept in mind during phallic reconstruction.(1) A new urethra must be constructed that allows for functional voiding.(2) There must be enough tissue to allow for <strong>the</strong> insertion <strong>of</strong> apros<strong>the</strong>tic device to permit sexual intercourse. (3) The final result mustbe aes<strong>the</strong>tically acceptable to <strong>the</strong> patient with (4) minimal loss <strong>of</strong> functionfrom donor sites. If possible, it is also desirable to (5) provideboth erogenous and protective sensation. From a surgeon’s perspective,(6) <strong>the</strong> reconstruction should be a single-step procedure.Many flaps are available for <strong>the</strong> reconstruction <strong>of</strong> <strong>the</strong> phallus. Pedicledoptions include abdominal, infraumbilical, groin, thigh, superficialinferior epigastric artery, and gracilis flaps. Microsurgical advanceshave made free flaps increasingly effective, including <strong>the</strong> radial forearmand lateral arm flaps. Osteocutaneous flaps have also been popularizedas <strong>of</strong> late, including <strong>the</strong> fibular and radial forearm osteocutaneous freeflaps. The radial forearm cutaneous flap is most desirable because <strong>of</strong> itsgood arterial supply and <strong>the</strong> abundance <strong>of</strong> skin available to create aneourethra and neophallus. The lateral border <strong>of</strong> this flap can be wrappedaround a Foley ca<strong>the</strong>ter using a tube-within-a-tube roll technique to allowfor an epi<strong>the</strong>lialized urethra. The donor site can be easily coveredwith a split-thickness skin graft.BACKNEXT
Postoperatively, <strong>the</strong> Foley ca<strong>the</strong>ter should remain in place for up to 4weeks to allow for <strong>the</strong> neourethra to heal and to facilitate micturition.To monitor <strong>the</strong> patency <strong>of</strong> <strong>the</strong> microsurgical anastomoses, implantableDopplers may be placed on <strong>the</strong> anastomosed artery and vein. PencilDopplers can also be routinely used to monitor <strong>the</strong> perfusion <strong>of</strong> <strong>the</strong> flap.After <strong>the</strong> microsurgical anastomosis has taken, return <strong>of</strong> sexual functionshould become a priority. Several options for pros<strong>the</strong>tic implantsare available including rod-like implants and inflatable balloon-like implants.The long-term viability <strong>of</strong> <strong>the</strong>se implants is dependent on <strong>the</strong>presence <strong>of</strong> enough tissue and intact protective sensation.REFERENCES1. Selvaggi G, Elander A. Penile reconstruction/formation. Curr Opin Urol. 2008;18(6):589–97.2. Kim SK, Lee KC, Kwon YS, Cha BH. Phalloplasty using radial forearm osteocutaneous free flaps infemale-to-male transsexuals. J Plast Reconstr Aes<strong>the</strong>t Surg. 2009;62(3):309–17.3. Dabernig J, Shelley OP, Cuccia G, Schaff J, Haferkamp A, Djakovic N. Urethral reconstruction using<strong>the</strong> radial forearm free flap: experience in oncologic cases and gender reassignment. Eur Urol.2007;52(2):547–53.4. Monstrey S, Hoebeke P, Selvaggi G, et al. Penile reconstruction: is <strong>the</strong> radial forearm flap really <strong>the</strong>standard technique? Plast Reconstr Surg. 2009;124(2):510–18.BACK