Primary Epithelioid Sarcoma of the Scalp Complicated by ... - ePlasty
Primary Epithelioid Sarcoma of the Scalp Complicated by ... - ePlasty
Primary Epithelioid Sarcoma of the Scalp Complicated by ... - ePlasty
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
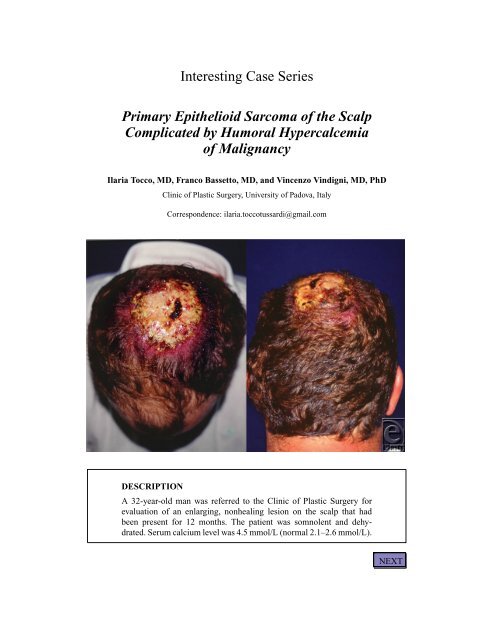
Incisional biopsies from 4 quadrants demonstrated an epi<strong>the</strong>lioid sarcomacomprising epi<strong>the</strong>lioid cells and discrete areas <strong>of</strong> central necrosis.Plain skull radiographs showed bony erosion. Full-body computed tomographicscans confirmed a s<strong>of</strong>t-tissue mass fixed to <strong>the</strong> skull andmultiple metastatic nodules in <strong>the</strong> cervical lymph nodes and both lungs.BACKNEXT
QUESTIONS1. What are <strong>the</strong> characteristics <strong>of</strong> epi<strong>the</strong>lioid sarcoma?2. What is <strong>the</strong> treatment plan for an epi<strong>the</strong>lioid sarcoma <strong>of</strong> <strong>the</strong> scalp?3. What are <strong>the</strong> pathogenesis and treatment <strong>of</strong> humoral hypercalcemia <strong>of</strong>malignancy?BACKNEXT
DISCUSSION<strong>Epi<strong>the</strong>lioid</strong> sarcoma is a mesenchymal malignancy that has been mostly reportedas affecting <strong>the</strong> distal extremities. It is exceptionally rare as a primaryneoplasm in <strong>the</strong> head and neck. Early diagnosis poses a challenge. The firstappearance <strong>of</strong> <strong>the</strong> tumor can be very ambiguous, most frequently as slowgrowingsubcutaneous nodules and ulcers that are easily misdiagnosed asbenign lesions for long times, as was <strong>the</strong> reported case. Moreover, even <strong>the</strong>histological diagnosis may pose some difficulties. Specific enzymatic, histochemical,and ultrastructural tests are required for accurate diagnosis.A treatment plan for this neoplasm has not been well defined in <strong>the</strong> literaturebecause <strong>of</strong> <strong>the</strong> rarity <strong>of</strong> sarcomas in general and <strong>of</strong> epi<strong>the</strong>lioid sarcomas locatedin <strong>the</strong> head and neck in particular. The tumor may be localized in <strong>the</strong> dermisand subcutaneous tissue, but it has a propensity for extension through deeperstructures, even <strong>the</strong> cortical bone. Thus, it is imperative that antitumor <strong>the</strong>rapybe implemented promptly. Early intervention is important. For epi<strong>the</strong>lioidsarcoma, aggressive surgical management and radical lymphadenectomy seemto be <strong>the</strong> treatments <strong>of</strong> choice. Reconstruction <strong>of</strong> <strong>the</strong> tumor excision defectcan be challenging. Chemo<strong>the</strong>rapy may play a limited role in advanced stages.Radiation <strong>the</strong>rapy, although usually performed, needs fur<strong>the</strong>r research onefficacy.The osteolytic process <strong>of</strong> bone invasion and several factors generated <strong>by</strong>disseminated tumor (such as parathyroid hormone–related peptide) can resultin an increase in serum calcium concentration, a condition known as humoralhypercalcemia <strong>of</strong> malignancy. Hypercalcemia can potentially threaten <strong>the</strong> life<strong>of</strong> <strong>the</strong> patient, and this previously unreported association with epi<strong>the</strong>lioidsarcoma stresses <strong>the</strong> importance <strong>of</strong> a high index <strong>of</strong> suspicion for early diagnosis.Treatment <strong>of</strong> tumor-related hypercalcemia consists <strong>of</strong> normal salineadministered intravenously at a rate <strong>of</strong> 200 to 500 mL per hour, followed <strong>by</strong>intravenous bisphosphonate. If normocalcemia is not achieved, <strong>the</strong> prognosisis very poor, and approximately 50% <strong>of</strong> such patients die within 30 days.BACKNEXT
REFERENCES1. Varela JM, Valencia J, Jimenez F, Torres A. <strong>Epi<strong>the</strong>lioid</strong> sarcoma. Eur J Plast Surg. 1989;12:138-42.2. Tran LM, Mark RM, Meier R, Calcaterra CT, Parker RG. <strong>Sarcoma</strong>s <strong>of</strong> <strong>the</strong> head and neck. Cancer.1992;70:169-77.3. Suwantemee C. <strong>Primary</strong> epi<strong>the</strong>lioid sarcoma <strong>of</strong> <strong>the</strong> scalp. Plast Reconstr Surg. 1999;104:785-8.4. Bos GD, Pritchard DJ, Reiman HM, Do<strong>by</strong>ns JH, Ilstrup DM, Landon GC. <strong>Epi<strong>the</strong>lioid</strong> sarcoma: ananalysis <strong>of</strong> fifty-one cases. J Bone Joint Surg Am. 1988;70:862-70.5. Phillips T, Pollock D, Sommerland B, Baker H. <strong>Epi<strong>the</strong>lioid</strong> sarcoma—a case report. Clin Exp Dermatol.1986;11:169.6. Body JJ, Dumon JC. Treatment <strong>of</strong> tumor-induced hypercalcaemia with <strong>the</strong> bisphosphonate pamidronate:dose-response relationship and influence <strong>of</strong> <strong>the</strong> tumor type. Ann Oncol. 1994;5:359-63.7. Stewart AF. Hypercalcemia associated with cancer. N Engl J Med. 2005;352:373-9.8. Chase DR, Enzinger FM. <strong>Epi<strong>the</strong>lioid</strong> sarcoma: diagnosis, prognostic indicators and treatment. Am J SurgPathol. 1985;9:241-63.Tocco et al. <strong>Primary</strong> <strong>Epi<strong>the</strong>lioid</strong> <strong>Sarcoma</strong> <strong>of</strong> <strong>the</strong> <strong>Scalp</strong> <strong>Complicated</strong> <strong>by</strong> Humoral Hypercalcemia<strong>of</strong> Malignancy. www.<strong>ePlasty</strong>.com, Interesting Case, December 10, 2012BACK