Winter 2009/2010 - SSM Cardinal Glennon Children's Medical Center
Winter 2009/2010 - SSM Cardinal Glennon Children's Medical Center
Winter 2009/2010 - SSM Cardinal Glennon Children's Medical Center
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
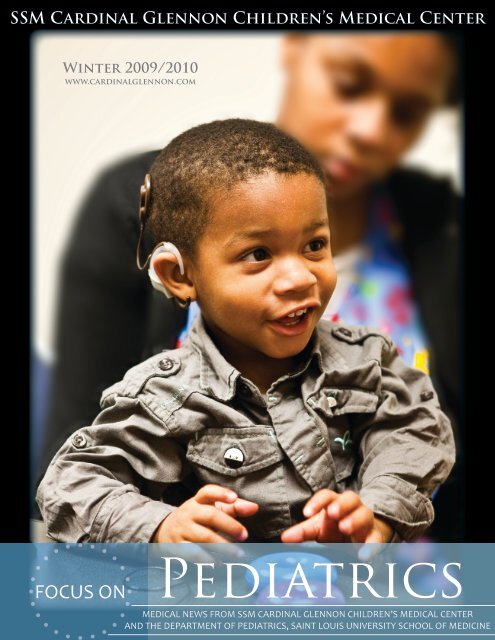
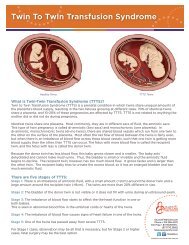
<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> Children’s <strong>Medical</strong> <strong>Center</strong><strong>Winter</strong> <strong>2009</strong>/<strong>2010</strong>www.cardinalglennon.comPediatricsFOCUS ONMEDICAL NEWS FROM <strong>SSM</strong> CARDINAL GLENNON CHILDREN’S MEDICAL CENTERAND THE DEPARTMENT OF PEDIATRICS, SAINT LOUIS UNIVERSITY SCHOOL OF MEDICINE
making a Difference<strong>Cardinal</strong> <strong>Glennon</strong> Division of OtolaryngologyAnita Jeyakumar, M.D., examines Isaiah Little, 1, during his follow up visit on Oct. 16 at <strong>Cardinal</strong> <strong>Glennon</strong>’s clinic. Dr. Jeyakumar performed Isaiah’s bilateral implant on Sept. 30.4The <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> Children’s <strong>Medical</strong> <strong>Center</strong>Division of Otolaryngology is a comprehensive ENTprogram, treating a full spectrum of conditionsincluding ear disease and sinus, sleep, neck and airwaydisorders.In three short years at <strong>Cardinal</strong> <strong>Glennon</strong>, Division DirectorRon Mitchell, M.D., has recruited numerous faculty and staffwhose shared goal is to care compassionately for patients andgrow the program to reach more children in need.The Division currently staffs eight faculty, two nursepractitioners and two clinic nurses. Anita Jeyakumar, M.D.,and Alan Wild, M.D., are the most recent faculty additions.Dr. Jeyakumar is expanding <strong>Cardinal</strong> <strong>Glennon</strong>’s CochlearImplant <strong>Center</strong>, while Dr. Wild is seeing patients several timesa month at St. Anthony’s <strong>Medical</strong> <strong>Center</strong> in South St. LouisCounty 1 .Yet, even with the new faculty, Dr. Mitchell says he owesmuch of the Division’s growth to the nurse practioners, TaraAlbert, CPNP, and Alicia McGlaughlin, CPNP.“They are the reason we have been able to grow the division,”Dr. Mitchell says. “They keep us all on track and the trainmoving forward.”Albert says her role is about convenience. The Divisioncurrently holds slots open for urgent clinic appointments,so Albert can bring patients in at the request of communityphysicians 2 .To provide the services needed for each of its unique patients,the Division also works extremely closely with audiologists,speech and language therapists, the Division of Sleep Services,and the Division of Allergy and Immunology.“We make an efficient game plan for the parents and providethe best care for the child,” Albert says. “We understand thecost of getting here, so we coordinate from the beginning.”This teamwork has also allowed the Division to expand itsresearch. Dr. Mitchell is the Principal Investigator on a largeNIH-sponsored grant to study children with sleep apnea. Thestudy, known as CHAT, is a joint project with <strong>Cardinal</strong><strong>Glennon</strong>’s Sleep Services.Thomas Donovan, M.D., is also working with <strong>Cardinal</strong><strong>Glennon</strong> Dermatologist Elaine Siegfried on a studyexamining the relationship between sinusitis and eczema.“Pediatric ENT involves a number of subspecialties withinspecialties, and we are only as good as this interaction,” Dr.Mitchell says. “In order to provide optimal care for each child,we must work together. Our relationships are something thatis unique to <strong>Cardinal</strong> <strong>Glennon</strong>.”1For the South County schedule, please visitwww.cardinalglennon.com, For Professionals, Close to Home Schedules.2 To make an appointment, please call (314) 268-4020.
Ear Disease & Cochlear ImplantsFor SoundSitting on his mother’s lap, Isaiah Little, 1, hears his first sound on Oct. 26. Saint LouisUniversity audiologist Sarah Borton, AuD., CCC-A, and <strong>Cardinal</strong> <strong>Glennon</strong>audiologist Sarah Duncan, M.S., CCC-A, turned on Isaiah’s right implant and taughthis mother,Tabatha Little, how to use them.Isaiah Little, 1, is not afraid to smile at his audience thismorning. He flashes a wide grin at audiologists, SarahBorton, AuD., CCC-A, and Sarah Duncan, M.S.,CCC-A, as they offer him brightly colored blocks. Maybe heknows what’s coming — today Isaiah will hear his first sound.With the recent addition of Anita Jeyakumar, M.D., theDivision of Otolaryngology has launched the CochlearImplant <strong>Center</strong>. Dr. Jeyakumar leads an experienced team ofprofessionals and, with a wide range of resources, the <strong>Center</strong>is able to address issues unique to each child with profoundhearing loss.The <strong>Center</strong>’s team includes:• Surgeons• Audiologists• Speech and languagepathologists• Nurses• Social worker• Implant coordinatorParents and children meet individually with these specialiststo determine the best possible care plan.When a child is diagnosed with profound hearing loss,options to address fundamental communication needsinclude:• Strictly oral/aural communication• American Sign Language (ASL)• Manually coded English (MCE)• Total Communication, which is a combination of signOn Nov. 11, Anthony Mikulec, M.D., places a cochlear implant behind two-yearoldBryson May’s right ear. The procedure was completed in three hours.and spoken/auditory communication• Auditory options include: hearing aids and cochlearimplantsAny child with profound hearing loss should seek a specialtyevaluation, Dr. Jeyakumar says. For some children withsevere-to-profound hearing loss, hearing aids may not provideadequate benefit, even after extensive auditory training.Cochlear implantation may be an option for a portion ofthese patients, and research shows a better outcome withimplants if children receive them earlier in life.The two-to-four-hour cochlear implant procedure is donebehind the ear. Dr. Jeyakumar - or fellow otolaryngologistAnthony Mikulec, M.D. - drills through the mastoid bone toaccess the cochlea where the electrodes are placed. The bodyof the device is secured under the skin on the skull, and theexternal piece attaches to this once the implant is activated.Factors that can affect the benefit of implants include:• Duration of deafness• Length of hearing aid use• Family and educational support“Pediatric otolaryngology allows me to make a realdifference in the lives of my patients, and often enables meto cure a problem,” Dr. Jeyakumar says. “The children wetreat are often victims of circumstance, so we feel we can beanother advocate for a child in need.”5
Sinus DisordersFor ComfortWorking closely with the Division of Allergy and Immunology, <strong>Cardinal</strong><strong>Glennon</strong>’s Otolaryngologists treat various levels of sinusitis.Concerning symptoms of sinusitis occur frequently or last longer than threemonths. They include nasal congestion, fever, facial pain, foul breath and cough.Initial treatment with antibiotics and topical nasal steroid sprays are an option,but if they do not relieve symptoms, Thomas Donovan, M.D., suggests referringpatients to an ENT specialist. <strong>Cardinal</strong> <strong>Glennon</strong> specialists are also available forconsultations during early stages of sinusitis.Upon referral, Dr. Donovan and his team work to avoid adenoidectomies.However, if an adenoidectomy is necessary, 50 percent of children improvesignificantly after the procedure.Thomas Donovan, M.D., examines Austin Smith’s nasal cavity.Austin, 16, fractured his nose when he was in a car accident atage 3. As his bones remodeled over time, they created asignificant nasal obstruction that made it difficult for Austinto breathe. Dr. Donovan will reset Austin’s nose in the next fewmonths.Since 1980, John Stith, M.D., hasworked with adults and childrenwith ENT conditions. Dr. Stithspent his first nine years with the AirForce, but as of 1989, he has devotedhimself to solving the airway problems ofhis pediatric patients at <strong>Cardinal</strong> <strong>Glennon</strong>.“The airway is the biggest challenge inpediatric ENT, so being able to help achild with any sort of airway condition isvery satisfying,” Dr. Stith says. “We’ve hada lot of success here.”Fellow otolaryngologist John Eisenbeis,M.D., works with the Division of PulmonaryMedicine to provide comprehensivecare to children with cystic fibrosis. Usingstate-of-the-art endoscopes, Dr. Eisenbeismonitors sinus disease and promotesrespiratory health during office visits.Airway ManagementFor Breath“Kids are fun, and we can getthem better. Even when it issomething permanent, we havethe chance to fix it and improvetheir life.”- Thomas Donovan, M.D.6The spectrum of airway obstructionproblems in children include benign causessuch as:• Adenotonsillar enlargement• Allergic rhinitis• Upper respiratory infections.However, there are congenital and acquiredproblems as well. These can be more severeand include:• Choanal atresia• Laryngomalacia• Vocal cord paralysis• Subglottic and tracheal stenosisSpeech therapist Christy Meyer, M.A., CCC-SLP, works with Evie Hale, 9 months, after placing a Passy-Muir Valveon Evie’s trachea. As Evie sits on her mother, Veronica Hale’s, lap, otolaryngologist John Stith, M.D., watches Evie’sreaction. The valve will help move air up through Evie’s vocal cords and allow her to make her first sounds. Evie wasborn premature and suffered from bronchial pulmonary dysplasia, lung disease and subglottic stenosis. After failinga cricoid split, Dr. Stith inserted a tracheostomy. He will reassess Evie in the spring in hopes of someday removing thetrach.<strong>Cardinal</strong> <strong>Glennon</strong>’s Division of Otolaryngology has all the necessary resourcesand professionals available to evaluate and treat any of these problems.While affected patients are usually babies with a history of prematurity, it isimportant that parents seek medical attention for any acute airway distress,cyanosis, or apneas as neglecting these symptoms in an affected child may haveserious adverse consequences.
Like his counterparts, DivisionDirector Ron Mitchell, M.D.,can treat the full spectrum ofENT problems. However, his clinicaland research interest lies in pediatricsleep disorders.Working with several specialtiesincluding sleep medicine, pulmonology,psychology and weight management,Dr. Mitchell helps manage sleep apneapatients. These children usually presentwith:• Snoring• Mouth-breathing• Restless sleep• Daytime behavioral problemsincluding hyperactivity, aggressionand reduced school performanceChildren with these symptoms as wellas large tonsils should be referred foran ENT evaluation. Some children willneed a sleep study while others mayproceed directly to adenotonsillectomies(T&A).Currently, Dr. Mitchell is performingmore T&As for sleep-disorderedbreathing than for recurrent throatinfections. T&As are the first line oftreatment and are known to cure 80 to90 percent of sleep apnea in normalweightchildren. In overweight children,Sleep ServicesFor RestAmber Nichols, 17, lies in one of the three beds in <strong>Cardinal</strong> <strong>Glennon</strong>’s sleep lab - the largest pediatric sleep lab inMissouri. Amber underwent an adenotonsillectomy on Nov. 9 in hopes of helping with her sleep apnea. Dr. Mitchellperformed the procedure and will follow up with Amber in January.T&A is curative in 25 percent of cases.The remaining patients may needfurther evaluation and treatmentincluding weight management, CPAPor further airway procedures.Important quality of life issues can beaddressed by managing sleep problemsearly, but often the problems areoverlooked. Dr. Mitchell suggestsincorporating questions in regard tosleep during wellness visits.“I’ve noticed in my 10 years sincefellowship that there is more of aninterest and more children are comingin for sleep-related issues,” Dr. Mitchellsays. “It’s a growing specialty, and thepotential impact on the child - sociallyand in school - as well as the benefits forthe whole family, is much wider thanthe sleep problem itself.”Sinusitis & EczemaA joint study between ENT,Allergy and Dermatology.Exploring the association betweenrespiratory infections and flares ofeczema, particularly in extremelysevere cases.Thomas Donovan, M.D.Elaine Siegfried, M.D.Manoj Warrier, M.D.Faculty ResearchFor the Futurechat“A Randomized ControlledStudy of Adenotonsillectomyfor Childhood Sleep Apnea”This five-year, multi-institutional studysponsored by the NIH is looking atoutcomes of T&A for sleep apnea inchildren.Ron Mitchell, M.D.Shalini Paruthi, M.D.Pediatrics on DemandDecember 7“Pediatric Sleep-DisorderedBreathing (SDB),”Ron Mitchell, M.D.December 14“Complications of Otitis Media,”Thomas Donovan, M.D.December 21“Sensorineural Hearing Loss andRehabilitation in Pediatric Patients,”Anita Jeyakumar, M.D.www.pediatricsondemand.comUsername: ds\r010-onlinePassword: webcme7