Spring 2011 - SSM Cardinal Glennon Children's Medical Center
Spring 2011 - SSM Cardinal Glennon Children's Medical Center
Spring 2011 - SSM Cardinal Glennon Children's Medical Center
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
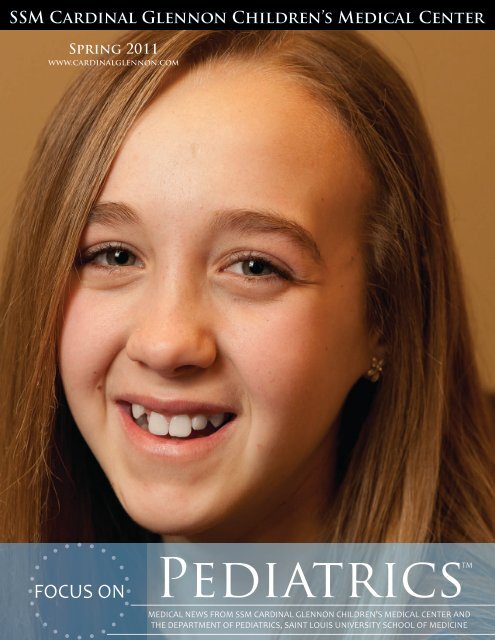
ON THE COVERLauren LeeLauren, 11, who was diagnosed with Hodgkin’s Lymphomain December 2010, begins a chemotherapy treatment atthe Bob Costas Cancer <strong>Center</strong> at <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong>.“The kids never cease to amaze me,” says Abby Sharamitaro,CPNP. “No matter how sick, kids will be kids. They’reresilient.” With the knowledge that she has another 7straight days of treatment ahead, and more after that,Lauren still lights up in front of the camera.FOCUS ONPediatricsTMEditor In ChiefSherlyn HailstonePresident<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong>Children’s <strong>Medical</strong> <strong>Center</strong><strong>Medical</strong> EditorKenneth Haller, MDAssociate Professor of PediatricsSaint Louis UniversitySchool of MedicineEditorAndrew SuttonPhysician Services Manager<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong>Children’s <strong>Medical</strong> <strong>Center</strong>WriterJessica HedgesPhysician Services Communications Specialist<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong>Children’s <strong>Medical</strong> <strong>Center</strong>For comments and suggestions, please email FocusOnPeds@ssmhc.com.
“The Ultimate Recycling Project”The St. Louis Cord Blood Bankat <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong>Children’s <strong>Medical</strong> <strong>Center</strong>The St. Louis Cord Blood Bank at <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong>Children’s <strong>Medical</strong> <strong>Center</strong> offers hope for anyone aroundthe world in need of a stem cell transplant. For childrenbeing treated for cancer and life-threatening blood andimmune disorders at <strong>Cardinal</strong> <strong>Glennon</strong>, this invaluableresource is right next door.Founded in 1996, the St. Louis Cord Blood Bank(SLCBB) was formed to create an inventory of stem cellproducts for transplant, with a focus to treat more patientsof all racial and ethnic backgrounds – and that it did.One of the largest public cord blood banks in the world,the SLCBB has received more than 100,000 cord blooddonations and holds a repository of 23,000 units, of which20 percent come from minority donors.<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> Division Director of Hematology-Oncology William Ferguson, MD, serves as the St. LouisCord Blood Bank Director, and Pediatric Hematologist-Oncologists Deepika Bhatla, MD, and Shermini Saini,MD, specialize in bone marrow transplantation at<strong>Cardinal</strong> <strong>Glennon</strong>. The Hem-Onc Division’s close workingrelationship with the St. Louis Cord Blood Bank supportsthe leading role its physicians have taken in developing theuse of stem cell transplants.“<strong>Cardinal</strong> <strong>Glennon</strong> and the St. Louis Cord Blood Bankhave a great symbiotic relationship. Together we cantreat more patients and work to find cures for diseaseslike Sickle Cell Anemia,” says Donna Regan, ExecutiveDirector of the St. Louis Cord Blood Bank. Usuallydiscarded as medical waste, cord blood has been usedto treat more than 70 different diseases. Donation isfree, safe and painless for the mother and baby, and thecollection process is facilitated on a voluntary basis bydelivering physicians, midwives, and the delivery staffs atparticipating hospitals. “The cord blood that gave life oncehas the potential to save another life. We like to call it the‘ultimate recycling project,’” Donna says.Cord blood saved the life of now 22-year-old Jessica Hahn.“I was 8 years old when I learned I had cancer,” Jessicasays. “I had never heard of cancer before, but the doctorsand nurses at <strong>Cardinal</strong> <strong>Glennon</strong> helped me understandwhat was going on in my body and what was going tohappen during treatment. We watched a Charlie Brownvideo that explained things on an 8-year-old level.”As a result of Jessica’s chemotherapy treatments forosteosarcoma, her cancer went into remission, but shedeveloped myelodysplastic syndrome, a disease of the bonemarrow. In order to repopulate her blood-forming cells,Jessica would need a bone marrow transplant. Her parentsand siblings were not matches, but before they couldworry, Jessica’s doctor told the Hahn’s about cord blood.In 2001, she received a transplant at <strong>Cardinal</strong> <strong>Glennon</strong>with cord blood stem cells provided by the St. Louis CordBlood Bank.“<strong>Cardinal</strong> <strong>Glennon</strong> became my home away from home. Istill look forward to checking in with my former nursesand doctors; they have become not only friends of minebut extended family,” Jessica says.On a follow up appointment to the Costas <strong>Center</strong>, Jessicaexpressed her interest in the medical field and learningmore about potential job opportunities at <strong>Glennon</strong>.One of the Hem-Onc nurses initiated a meet-and-greetwith Donna Regan and in the summer of 2009, Jessicacompleted an internship at the St. Louis Cord Blood Bank.“It was so exciting to learn more about the procedure andto give back to the same bank that my cord blood camefrom,” she says.Jessica now works as the Bank’s Operations Assistant. “Thebest part about my job is knowing that with each exportedcord a patient’s life could be saved, just like it saved mine.”5
Forming Bonds, Forging Hope<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong>Division of Hematology-OncologyIt’s apparent that patient and family care are the mainconcerns within the Hematology-Oncology Divisionat <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> Children’s <strong>Medical</strong> <strong>Center</strong>.While the reason behind an appointment with aHem-Onc specialist may be unpleasant, the Hem-Oncteam works together to make their young patients’experiences the very best.Outpatient services are provided within the BobCostas Cancer <strong>Center</strong> at <strong>Cardinal</strong> <strong>Glennon</strong>. Smilingfaces greet visitors, colorful butterflies paint theceilings and a large play area decorated withpatient artwork welcomes childrenof all ages. After a couple ofappointments at the Costas<strong>Center</strong>, John Mossman, Hem-Onc Information Specialist,is one of those happy facesthat becomes familiar toparents and children alike.On a cold Fridaymorning in January, Johnwarmly checks patients inand answers phone calls.“No problem, I’ll get thatappointment rescheduledfor you,” John tells a caller.“Hopefully the roads will be clearof snow by next week.”It wouldn’t be unusual to find a small patientsitting with John at the front desk while he multitasks.I“My favorite part about my job is interacting with thekids. t’s apparent They come that to patient know and us as family the people care are they the can goto main when concerns they’re scared,” within the John Hematology-Oncologysays.Division at <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> Children’s<strong>Medical</strong> Like John, <strong>Center</strong>. the kids While are the what reason Clinical behind Nurse an Ashleyappointment Hite looks forward with a Hem-Onc to everyday. specialist “We develop may be specialunpleasant, relationships the with Hem-Onc our patients,” team works she says. together “We to alsomake help their to facilitate young patients’ relationships experiences between the patients very best. as theyfind comfort in each other. The Costas <strong>Center</strong> is kidfriendlyand provides a lot of space and openness toencourage interaction.”Ashley’s professional connection to <strong>Cardinal</strong> <strong>Glennon</strong>stemmed from a personal one. “My cousin was treatedat <strong>Cardinal</strong> <strong>Glennon</strong> for leukemia,” Ashley says. “Hebecame close to all the doctors and though it wasdifficult, it was also an amazing experience for myentire family.” Since joining the Hem-Onc team inJuly 2010, Ashley says her connection to <strong>Cardinal</strong><strong>Glennon</strong> and the Hem-Onc Division hasonly become stronger.From appointment setting tonursing and physician care,team work and collaborationare essential componentsof the Hem-Onc Division.Abby Sharamitaro, CPNP,is one of the Hem-Oncteam’s Nurse Practitioners,serving as a support andadvocate for the Divisionand bridging the gapbetween nurses and doctors.“As a multidisciplinaryteam, we utilize our resourceswith Child Life, Psychology andSocial Work, and meet regularly todiscuss new and existing patients andtheir families,” Abby explains. “We always takethe patient and their family’s emotional and financialconcerns into account and work to make things betterfor them.”The emotional aspect of treating children andadolescents with serious and sometimes lifethreateningillnesses is one the team must address withnearly every patient encounter. “I get down on theirlevel and try to take the ‘medical’ out of it,” Abby6
says. “I’ll sit next to the patient on the exam table andinitiate age- and personality-appropriate educationalactivities. Depending on the situation, I may ask theparents about the best way to approach their child.”Each faculty and staff member has their own approach,and personal contact is key at <strong>Cardinal</strong> <strong>Glennon</strong>.“<strong>Glennon</strong> has a small hospital feel. The attendingphysicians take care of their patients here; they knowtheir patients and their medical conditions and are oncall nights and weekends in case they’re needed,” Abbysays.David Greenberg, MD, is the Orthopaedic Oncologistwho works with the Hem-Onc Division. He says, “Thecare of cancer patients today truly requires a multidisciplinaryapproach. Cancer patients often requiremultiple methods of treatment, including surgery,medicine and radiation therapy. One of the advantagesof <strong>Cardinal</strong> <strong>Glennon</strong> and Saint Louis University isthat we approach cancer as a team, with frequentcommunication among the physicians.”Despite his full clinic schedule today, Dr. Greenbergarrives early to discuss one of his inpatient cases withDivision Director Dr. William Ferguson. After somecollaboration, they decide that Dr. Ferguson will see thepatient the following day, and then he’s off to his firstappointment of the morning.“How’s our little girl doing?” Dr. Greenberg greets hispatient, a 2 ½-year-old with a benign tumor in herfemur that is causing inflammation and discomfort.“Her leg is hurting her,” the little girl’s father answers.With that, Dr. Greenberg outlines the surgery plan,cast options for the rambunctious toddler, and offersto show his patient’s great-grandmother – who hasn’tseen the x-ray – the study of her granddaughter’s bone.After explaining the x-ray to the family, Dr. Greenbergassures them that he will schedule the surgery as soon aspossible.“My patients are often sent to me with unknown lesionsand fearing the worst. Going over the imaging studiesand allowing them to visualize what we are dealing withhelps,” Dr. Greenberg says. “Regardless of the outcome,patients generally have added comfort when theyunderstand their disease. An important part of my job isto provide that understanding.”The little girl waves goodbye over her daddy’s shoulder,and before they are out the door, Dr. Greenberg is onthe phone making arrangements to remove the tumor.The Division ofHematology-OncologyProvides six clinical services tochildren and adolescents withblood disorders and cancer:1. Hematopoietic Stem Cell Transplantation – fourpatienttransplantation unit2. Neuro-Oncology Program – Neuro-Oncologylong-term follow-up clinic recently added3. Hemostasis Program – only federally-designatedpediatric Hemophilia Treatment <strong>Center</strong> in theSt. Louis area and includes an expanding 340Bprogram that facilitates distribution of clottingfactor concentrates to patients4. Sickle Cell Anemia/Hemoglobinopathies Program– includes a monthly clinic in Centreville, Ill.,at the Southern Illinois Healthcare FoundationMother & Child <strong>Center</strong>5. Apheresis Program – team of nurses andphysicians trained in apheresis on infants toadolescents6. Long-term Follow-upIs committed to advancing the careof children through collaborationwith basic science research andclinical research programs:• Active participant in the National Institute’s ofHealth-sponsored Children’s Oncology Group• Active participant in the <strong>Center</strong> for InternationalBlood and Marrow Transplant Research• One of the founding institutions of the newlyformedNeuroblastoma and MedulloblastomaTranslational Research Consortium7
The Port of Dr. Ferguson-YangLauren Lee“You look awfully good,what are you doing at thedoctor’s office?” Dr. Fergusonteases Lauren during acheckup and chemotherapytreatment at the Bob CostasCancer <strong>Center</strong> at <strong>SSM</strong><strong>Cardinal</strong> <strong>Glennon</strong> Children’s<strong>Medical</strong> <strong>Center</strong>.8It was December 22, 2010. Christmas was just around thecorner. At the top of 11-year-old Lauren Lee’s Christmaswish-list was an iPod Touch. She also wished to feel better.That day, Lauren and her family viewed an x-ray of herchest with <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong>’s Division Director ofHematology-Oncology, William Ferguson, MD. The imagerevealed a large mass and Lauren’s diagnosis – Hodgkin’sLymphoma.“She looked pale, anemic,” says Tim Lee, Lauren’s father.“That was the clue something was wrong.” Rachel Tarr,Physician Assistant, of Family Medicine Associate’s inCollinsville, Ill., examined Lauren in December after she hadbeen running a fever, vomiting and experiencing night sweats.A blood test indicated that Lauren was severely anemic.Rachel called <strong>Cardinal</strong> <strong>Glennon</strong> immediately to schedule anappointment for Lauren to see a Hematologist-Oncologistspecialist.“I refer my patients to <strong>Cardinal</strong> <strong>Glennon</strong> because I’ve had agreat personal and professional experience with the hospital,”Rachel, who is a graduate of Saint Louis University Schoolof Medicine, says. “<strong>Cardinal</strong> <strong>Glennon</strong> also offers a nonintimidatingenvironment for children.”When you’re looking for a combination of advancedresearch and technology, expert faculty and resources andcompassionate care, there is no better place than <strong>Cardinal</strong><strong>Glennon</strong>. “We have access to all the latest information andnewest medications, including many new investigational
drugs,” Dr. Ferguson says. “As part of theNIH-sponsored Children’s Oncology Group,we are not only provided with the latestresearch and protocols, but have access tophysicians and researchers throughout theworld with the most up-to-date informationfor any given disease. At the same time,we strive to provide a friendly, comfortingand accommodating environment wherepatients and families are not only treatedas individuals, but as partners in workingtowards a cure.”Within a day of Rachel’s phone call to<strong>Glennon</strong>, Lauren had her initial visit withDr. Ferguson. Within an hour of Lauren’sappointment, Dr. Ferguson was on the phonewith Rachel to discuss the results. “I’ve beenreceiving regular, thorough updates fromDr. Ferguson on Lauren’s status; usually thesame day he sees her,” Rachel says. “The notesindicate that he’s discussed Lauren’s treatmentplan and possible outcomes with the Lees. It’sobvious they are spending a lot of time withthe family.”On December 27, 2010, Lauren begantreatment at <strong>Cardinal</strong> <strong>Glennon</strong>. For any pre-teen, thethought of needles and doctors can be scary. For Lauren,those fears were real. “She’s always been scared of needlesand doctors,” says Angie, Lauren’s mother. “But Dr.Ferguson was great at explaining the treatment process toLauren in a way that made her feel comfortable. You don’tget that with every doctor.”“I try to explain things using ‘plain English,’” Dr. Fergusonsays. “Since successful treatment depends as much uponthe family as it does upon what we do in the hospital, itis very important to work extra hard to educate patientsand families. I also try to emphasize that our entire team isavailable to answer questions; sometimes another doctor ornurse will explain things a little different, but in a way thatjust ‘clicks’ better.”In order to receive her medication, <strong>SSM</strong> <strong>Cardinal</strong><strong>Glennon</strong> Pediatric Surgeon, Edmund Yang, implanteda Portacath under Lauren’s skin in her chest. Before thesurgery, Dr. Yang visited with the Lee’s. “He came in andexplained every step of the way,” says Tim of Dr. Yang.Lauren may not like her port – “It’s disgusting,” she says –but she’s affectionately coined it “Dr. Ferguson-Yang.”After a series of questions and examination, Dr. Ferguson addresses the entire family - Lauren, mom, dadand sister - to go over Lauren’s progress and medication. In regard to the steroid medication Lauren has beentaking, Tim, Lauren’s father, mentions that her appetite has increased. A side-effect the Lees are aware of, Dr.Ferguson jokingly assures them, “I do not get kick-backs from Dierberg’s or Schnuck’s.” Laughing, Tim says,“Maybe you should!” Before leaving, Dr. Ferguson checks with Lauren - “Anything else I can do for you?”to David Ish, Director of Child Life. “I met the toy guy. Hebrought me ceramics to paint and stuffed animals,” Laurensays. Child Life Services provides activities and opportunitiesfor patients to help reduce stress and anxiety and gain a senseof control over their hospital experience.Another big support has been Lauren’s older sister Morgan,22. Both Tim and Angie agree, “Morgan is the rock.” Inregard to <strong>Cardinal</strong> <strong>Glennon</strong> faculty and staff, Morgan says,“They’re all really nice and try to make everything as painlessas possible.”Recently, Lauren confided in her mom – “After all of this, Ijust may like doctors.”To pass the time during her inpatient and outpatient visitsto <strong>Glennon</strong>, Lauren listens to her new iPod Touch that sheunwrapped this past Christmas. She also was introduced(From left to right) Lauren, Morgan, Tim and Angie Lee9
whose primary clinical and researchfocuses are bleeding and clottingdisorders, and a nurse coordinator,physical therapist and social worker,all of whom are dedicated to the<strong>Center</strong> and its patients.“Members of our team are requiredto attend an annual regional meetingwith other hemophilia treatmentcenters to ensure that we are up-todatewith leading edge care,” saysDr. Puetz. “Our patients have theopportunity to participate in researchstudies and various bleeding disorderdatabases, and our facility at theCostas <strong>Center</strong> allows us to provide care in one place, even ifthe patient needs an infusion.”Brent Miller, MD, Grayson’s father, is a nephrologist. Bothhe and Shelley have had many personal and professionalexperiences at health care institutions, and they agree thatthe care Grayson has received at <strong>Glennon</strong> is unmatched. “Inmy healthcare experiences, I always ask the question: ‘Arethese people here to benefit themselves or their patients?’ Ican truthfully answer that the faculty and staff at <strong>Cardinal</strong><strong>Glennon</strong> are here for the patients. From the people makingthe food to the doctors, the feeling that everyone at <strong>Glennon</strong>is concerned for the well-being of your child is palpable andcomforting,” Dr. Miller says, adding, “Even the parking iseasy, and times when we’ve had to come to the ER, we arealways taken care of right away. ”“You wouldn’t understand until you’ve had a child treated at<strong>Glennon</strong>,” Shelley says. “One of the biggest differences is thatwe can always get in touch with an attending hematologist,“Hi Grayson! You remember me. We go way back.” Dr. Puetzsays. “I haven’t heard from you lately, so that’s good news.”no matter what time. I called everyday for the first year of Grayson’s lifeand they were always helpful.”When Grayson was 7 monthsold, he had a spontaneous brainhemorrhage and was rushed to<strong>Cardinal</strong> <strong>Glennon</strong> in the middle ofthe night. Hematologist ChristopherHugge, MD, was on-call and arrivedat <strong>Glennon</strong> at 4 a.m. to attend to hispatient. “That’s when we found outGrayson was a severe hemophiliac,”Shelley remembers. Grayson haddeveloped an inhibitor that makesit difficult to obtain enough clottingfactor to control bleeding. Concerned for their baby’s life, theMillers say they were “extremely grateful” Grayson was beingcared for at <strong>Cardinal</strong> <strong>Glennon</strong>.“When we first met Dr. Puetz, he told us his goal was to turnGrayson’s hemophilia from a tragedy to an annoyance,” Dr.Miller says. “In the beginning, we always thought it would bea tragedy. But three years later, it’s just an annoyance we haveto deal with everyday.”Grayson is seen by Dr. Puetz on an as-needed basis, andannually for a comprehensive evaluation. Shelley administersGrayson’s daily medications through a portacath and draws alab once per month that she takes to <strong>Glennon</strong> for testing.Just the other day, the Millers received Grayson’s lab results forthe month. “Dr. Puetz called and was so excited. Grayson’s levelwas at 15, which is the highest it’s ever been. We celebrated.”Shelley says. “Those are the things you hold on to.”Dr. Puetz asks Grayson if he can take a look at his port, but Grayson is lessthan willing. “Let me tell you a secret,” Shelley, Grayson’s mother, says to him.After a quick whispered exchange, Grayson willingly reveals his port and talksabout the pirate bed his daddy is building him.“Everything looks good,” Dr. Puetz says. But before Dr. Puetz can consultwith the family, Grayson makes a request – “Can I have my tootsie roll now?”11
Q&AWilliam Ferguson, M.D.Division Director of Hematology-Oncology12Q: Why did you choose to specialize in Hematology-Oncology? What do you like best about your job?A: Part of what attracted me to Hematology-Oncologywas the challenge of skillfully providing very intensive andcomplex medical care to children with life-threateningdiseases. However, unlike certain other specialties where thisis also true (such as critical care or neonatology), we also getto have the same sort of close, long-term relationship thatprimary care physicians value so much. There’s nothing quitelike a visit from a former patient who is not only cured ofwhat was once incurable cancer, but who is now showing offtheir own child!Q: How does the Division of Hematology-Oncology workas a team to provide the best possible care for patients?A: The entire team of physicians, nurse practitioners, andoutpatient nurses meet every day to discuss all of the patientsseen that day either in the hospital or in the Costas <strong>Center</strong>.This allows us to regularly stay informed on our entire patientpopulation and get everybody’s input on how to best care forour patients. We also meet very frequently with our affiliatedspecialists – social workers, psychologists, child life specialists,etc. – in order to get their perspective and to identify patientsand families who would benefit from their special skills.In addition, we have several multi-disciplinary clinics thatincorporate other medical specialists, with the same goalof providing timely and cooperative care for these complexpatients.Q: How does your Division keep in contact with yourpatients’ primary care physicians?A: For efficiency, we stay in contact by routinely e-mailingor faxing our own documentation. This keeps the primaryphysician up to date, but avoids the delay of regular mail. Weused to rely more on phone calls; but as practices have gottenbusier, we try to avoid taking busy doctors away from theirpatients, unless it is an urgent manner.Q: Do you have a particular patient care philosophy thathas guided you throughout your career?A: Very simple – we should strive to treat our patients andfamilies the same way we would want ourselves and our ownchildren to be treated.To reach Dr. Ferguson,please call: 314-577-5638To reach the Bob CostasCancer <strong>Center</strong>, please call:314-268-4000
Hematology-OncologyFacultyWilliam Ferguson, MDDivision Director, Hematology-Oncology<strong>Medical</strong> Director, Bob Costas Cancer <strong>Center</strong>Professor of Pediatrics, Saint Louis University School of MedicineMD: New York University School of MedicineResidency: Massachusetts General HospitalFellowships: Massachusetts General Hospital, Massachusetts Institute ofTechnologyDeepika Bhatla, MDAssistant Director, Stem Cell Transplantation ProgramAssociate Professor of Pediatrics, Saint Louis University School of MedicineMD: Lady Hardinge <strong>Medical</strong> College and Smt Sucheta Kripalini Hospital,New Delhi; University College of <strong>Medical</strong> Sciences and Guru Tag BahadurHospital, New DelhiResidency: University of Kentucky Chandler <strong>Medical</strong> <strong>Center</strong>Fellowship: Cincinnati Children’s Hospital <strong>Medical</strong> <strong>Center</strong>Gordon B. Gale, MDProfessor of Pediatrics, Saint Louis University School of MedicineMD: Saint Louis University School of MedicineResidency: Saint Louis University/<strong>Cardinal</strong> <strong>Glennon</strong> Children’s <strong>Medical</strong><strong>Center</strong>Fellowship: Children’s Hospital of PhiladelphiaKaren Gauvain, MDDirector, Neuro-Oncology ProgramAssistant Professor of Pediatrics, Saint Louis University School of MedicineMD: Saint Louis University School of MedicineResidency: Washington University/St. Louis Children’s HospitalFellowship: Washington University/St. Louis Children’s HospitalDavid Greenberg, MDAssistant Professor of Orthopaedic Surgery, Saint Louis University School ofMedicineMD: Georgetown University School of MedicineResidency in Orthopaedic Surgery: University of Missouri – ColumbiaFellowship in Musculoskeletal Oncology: University of ChicagoChristopher Hugge, MDAdministrative Director, Hemostasis ProgramDirector, Apherisis ProgramAssistant Professor of Pediatrics, Saint Louis University School of MedicineMD: St. Louis University School of MedicineResidency: Saint Louis University/<strong>Cardinal</strong> <strong>Glennon</strong> Children’s <strong>Medical</strong><strong>Center</strong>Fellowship: Washington University/St. Louis Children’s HospitalDennis M. O’Connor, MDProfessor of Pediatrics, Saint Louis University School of MedicineMD: Saint Louis University School of MedicineResidency: Saint Louis University/<strong>Cardinal</strong> <strong>Glennon</strong> Children’s <strong>Medical</strong><strong>Center</strong>John Puetz, MD<strong>Medical</strong> Director, Oncology Long-term Follow-up ClinicClinical Director, Hemostasis ProgramClinical Associate Professor of Pediatrics, Saint Louis University School of MedicineMD: Washington UniversityResidency: Washington University/St. Louis Children’s HospitalFellowship: University of UtahShermini Saini, MDAssistant Professor of Pediatrics, Saint Louis University School of MedicineMD: University of Wisconsin-MadisonResidency: Tulane UniversityFellowship: Duke UniversityHematology-OncologyProfessional StaffJeanne Harvey, APRN, PNP-CPediatric Nurse PractitionerAbby Sharamitaro, RN, MSN, CPNP, CPONPediatric Nurse Practitioner13
Physician Services Department1465 South Grand Blvd.Saint Louis, Missouri 63104-1095Non Profit OrgU.S. PostagePAIDSt. Louis, MOPermit No. 2412