Pediatrics - SSM Cardinal Glennon Children's Medical Center
Pediatrics - SSM Cardinal Glennon Children's Medical Center
Pediatrics - SSM Cardinal Glennon Children's Medical Center
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
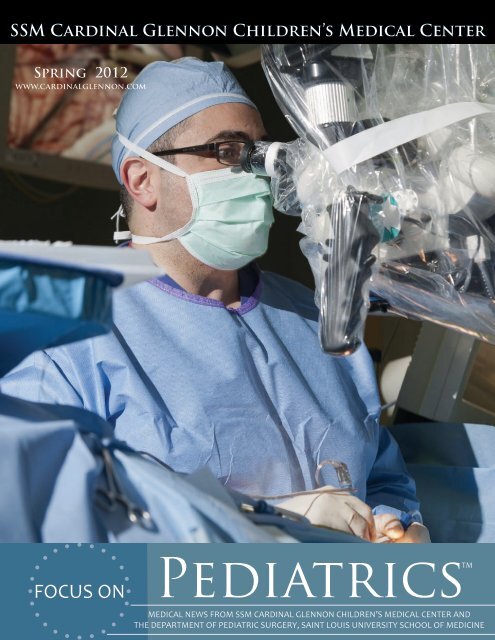
ON THE COVERDr. Samer K. ElbabaaNeurosurgery Division Director Dr. Samer K. Elbabaaremoves a tumor from a pediatric patient’s brain. Since Dr.Elbabaa’s arrival in July 2011, the Division of Neurosurgery at<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> Children’s <strong>Medical</strong> <strong>Center</strong> hasincreased its neurosurgical clinic times and expanded its staffto see more patients, and added state-of-the-art endoscopicand microsurgical equipment for innovative procedures.FOCUS ON<strong>Pediatrics</strong>TMEditor In ChiefSherlyn HailstonePresident<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong>Children’s <strong>Medical</strong> <strong>Center</strong><strong>Medical</strong> EditorKenneth Haller, MDAssociate Professor of <strong>Pediatrics</strong>Saint Louis UniversitySchool of MedicineEditorAndrew SuttonPhysician Services Team Leader<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong>Children’s <strong>Medical</strong> <strong>Center</strong>WriterJessica HedgesPhysician Services Communications Specialist<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong>Children’s <strong>Medical</strong> <strong>Center</strong>For comments and suggestions, please email FocusOnPeds@ssmhc.com.
Announcements2012 <strong>Glennon</strong>Express GuidesMailed in January<strong>Glennon</strong>ExpressGuide2012Each physicianoffice receivedtwo 2012<strong>Glennon</strong> ExpressGuides and anorder form foradditional guidesin January. If youdid not receive your guides or would likeextras, please e-mailJessica_Hedges@ssmhc.com.To view a printable PDF of the2012 <strong>Glennon</strong> Express Guide, go towww.cardinalglennon.com,For Physicians, Office Resources,2012 <strong>Glennon</strong> Express Guide.One-Stop-Shoppingfor ContinuingEducationOpportunities2012EducationConnections - anew CME/CEU guide with<strong>SSM</strong> <strong>Cardinal</strong><strong>Glennon</strong>, <strong>SSM</strong>Maternity Careand Saint LouisUniversity Schoolof Medicine educational opportunities- was mailed to physician offices inFebruary. If you did not receive yourguide or would like extras, please e-mailJessica_Hedges@ssmhc.com.To view a printable PDF ofEducation Connections, go towww.cardinalglennon.com,For Physicians, Education,Education Connections.AppointmentsKoenig, Joyce, MDAppointed to serve as 2012-2013 President for the Midwest Society for Pediatric ResearchAwardsDanis <strong>Pediatrics</strong> at <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> Children’s <strong>Medical</strong> <strong>Center</strong>The Danis <strong>Pediatrics</strong> office staff and the General Academic <strong>Pediatrics</strong> faculty received the 2011 Bright FuturesPreventive Services Improvement Project award from the American Academy of <strong>Pediatrics</strong> (AAP) QualityImprovement Innovation Network on Nov. 11, 2011 in Chicago. The mission of the improvement project isto improve health supervision care of children from birth to age 3 as outlined by Bright Futures: Guidelines forHealth Supervision of Infants, Children, and Adolescents.InvitationsKoenig, Joyce, MDInvited grant reviewer: National Institutes of Health and National Institute of Child Health and HumanDevelopment. 21 February 2012.Invited grant reviewer, special emphasis panel: National Institutes of Health and National Institute of Allergyand Infectious Diseases. 2-3 February 2012.Invited platform session chair: 2012 Pediatric Academic Societies meeting – Chorioamnionitis, Inflammationand the Developing Fetus. 2012. (upcoming meeting)Zand, Debra, PhDInvited Membership: Association for Psychologists in Academic Health <strong>Center</strong>s. December 2011.PresentationsAbraham, Elizabeth, MD“Steroid-Based Versus Steroid-Free Immunosuppression in Children.” American Transplant Congress. Boston.June 2012. (upcoming presentation)Elbabaa, Samer MD“Pediatric Traumatic Brain Injury.” Midwest Pediatric Trauma Conference. St. Louis. 18 November 2011.“Revisiting the Endoscopic Ventricular Shunt Catheter Insertion and Revision: Risk Factors for Failure.” 39thAnnual Meeting of the International Society for Pediatric Neurosurgery. Goa, India. 16-20 October 2011.Koenig, Joyce, MD“Leukocytes, Platelets and Coagulation Disorders in Neonates.” American Academy of <strong>Pediatrics</strong> NeoPrepReview Course. New Orleans. 21 January 2012.Research abstract accepted for platform presentation. Pediatric Academic Societies meeting. Boston. 30 April2012. (upcoming presentation)PublicationsBabusis, Elizabeth, MD“Live and Inactive Influenza Vaccines Induce Similar Humoral Responses, but Only Live Vaccines InduceDiverse T-Cell Responses in Young Children.” The Journal of Infectious Diseases. September 2011.Elbabaa, Samer, MD“Code the Complexities of Intracranial Endoscopies in Pediatric Neurosurgery.” AAPC Coding Edge. January2012.“Myelomeningocele and Associated Anomalies” (Chapter 117). Benzel, Edward (2012). Spine Surgery:Techniques, Complication Avoidance and Management (3rd Edition). Elsevier.Haller, Kenneth, MD and Scalzo, Tony, MD“I’ve Heard Some Things That Scare Me: Responding with Empathy to Parents’ Fears of Vaccinations.” MissouriMedicine. January/February 2012.Jain, Ajay, MD“Enteral Bile Acid Treatment Improves Parenteral Nutrition Related Liver Disease and Intestinal MucosalAtrophy in Neonatal Pigs.” American Journal of Physiology – GI. November 2011.ResearchAbraham, Elizabeth, MDCompleted an M.S. in Clinical Research from the University of CincinnatiKoenig, Joyce, MDAwarded a two-year grant (Feb. 2012-Jan. 2014) totaling $412,000 by the National Institutes of Health andNational Institute of Allergy and Infectious Diseases to study neonatal immunity and inflammatory mechanismsResignationsKumar, Tarun, MD - Department of SurgeryWalsh, David, MD - Department of Child Neurology1
Free Epic Care Link Service for Real-TimeAccess to Patient InformationEpic Care Link Features Include:Epic Care Link is an easy, web-based tool for communityphysicians, nurses and office managers to receive and accessreal-time information regarding their patients.• Read-only access to your patient’s entire chart from your desktop or laptop computer• E-mail notifications available for set up so you know any time one of your patients visits the EmergencyDepartment, is admitted or discharged, or has lab/imaging results available for review• Lab/Imaging results, OP notes, admission H&P, consults and outpatient clinic notes available as soon assigned by a <strong>Cardinal</strong> <strong>Glennon</strong> specialistTo see how Epic Care Link works, go to www.cardinalglennon.com, For Physicians, Epic Care Link.If you would like to sign up for the free Epic Care Link service, please contact Jane Beckman, ConnectivityCoordinator, at Jane_Beckman@ssmhc.com.Earn FREE CME Credit Online, On Your Timewith <strong>Pediatrics</strong> on DemandNew lectures available:“Minimally-Invasive Endoscopic Neurosurgery” – Samer Elbabaa, MD“Eating Disorders in Teens: <strong>Medical</strong> Aspects” – Dianne Elfenbein, MD“Cystic Fibrosis” – Robert Wilmott, MD“Neonatology: Homeward Bound” – Connie Anderson, MD“Neonatology: Cyanotic Heart Disease” – Catherine Cibulskis, MD“Neonatology: An Infant with a Cleft Palate and Dysmorphic Features” – Thomas Bender, MDTo view a presentation:Logon to www.pediatricsondemand.comUsername: ds\r010-onlinePassword: webcmeTo earn 1 CME Credit from St. Louis University School of Medicine:Choose the link icon above the presenter’s window. Click TEST LINK. Register (if you haven’t already), take thequiz and finish the evaluation. Certificates are sent to your e-mail address within 48 hours.Sign-Up to Receive <strong>Cardinal</strong> <strong>Glennon</strong> Newson Demand for Pediatric Updates<strong>Cardinal</strong> <strong>Glennon</strong> News on Demand provides community physicians, nurses and office staff withregular pediatric updates that help you and your patients. The electronic newsletter is e-mailedmonthly. To receive the newsletter, send your e-mail address to Jessica_Hedges@ssmhc.com.2
Primary Care Physician Communication ProcessImproves at <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong>Dear Physician Partners,Over the past year, you have provided us valuable feedback regarding our primary carephysician communications process. Because consistent communication remains a top priorityat <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong>, we have made many changes that are reflective of yourfeedback. From patient admission to discharge, take a look at how we’veimproved our communication with you:Patient AdmissionHuman ProcessTechnical ProcessEmergencydepartmentsecretary calls/pagesprimary care physicianat time of admissionto inform of inpatientadmissionEmergencydepartment residentnote is auto-faxed toprimary care physicianupon signatureFor any*admissionbetween 5 p.m. and4 a.m., Access <strong>Center</strong>calls primary carephysician exchange at5 a.m. to notify** ofadmissionFloorresident H&P isauto-faxed to primarycare physician uponsignatureFor any*admissionbetween 4 a.m. and5 p.m., the Floor TeamUnit Secretary callsprimary care physicianoffice to notify ofadmissionFloorattending H&P isauto-faxed to primarycare physician uponsignature, and includesattending pagernumber*Medicine, Surgical,PICU and NeurologyAdmissions**Notification messagewill include patientname, admittingdiagnosis, room number,unit and telephonenumber for unit to whichpatient is admitted.Patient DischargeWe continue to make strides in communication, and we vow to make every effort to get it right. Since modifyingthe communications process in November, we’ve already heard from some of you. Dr. George Anderson of Preferred<strong>Pediatrics</strong> said, “I’ve had multiple patients admitted since <strong>Cardinal</strong> <strong>Glennon</strong>’s new communication process tookeffect, and I was notified promptly with each admission.”Our commitment as a hospital is to provide the best medical care for our patients, and we know that notifying andinforming you of patient admissions, discharges and changes in care are integral parts of fulfilling that responsibility.Your input regarding our communication is greatly appreciated and a significant factor in our continuedimprovement. Please contact any of us directly with your comments.Sincerely,Sherlyn Hailstone, President (Sherlyn_Hailstone@ssmhc.com)John Peter, MD, Vice President of <strong>Medical</strong> Affairs (peterjr@slu.edu)Robert Wilmott, MD, Chief of <strong>Pediatrics</strong> (wilmottr@slu.edu)Dennis Vane, MD, Chief of Surgery (dvane@slu.edu)3
DiversionsAndrew Sutton Physician Services Manager2008 Nalle Winery Reserve ChardonnayThe weather is warming up, and it’s time for long evenings on the patio with a group of good friends. One of thefriends you should bring to the party is the 2008 Nalle Reserve Chardonnay.Nalle Winery is a tiny, family-owned operation in the Dry Creek Valley in Sonoma’s wine country. So tiny in fact,that it’s literally a mother, father and son that run the winery and make the wine. I had a chance to visit them this pastsummer and fell in love with their laid-back attitude, and their simply outstanding Burgundy style wines.The grapes are sourced from the Hopkins Ranch in Russian River Valley, where cool temperatures and fog allow thegrapes to develop slowly with just the right amount of acidity, and elegance. This wine shows fantastic nose of ripefruit, with a touch of vanilla, and a little bit of apple. Its mouth feel sways a little toward medium than light, showingthe kiss of oak from a short barrel fermentation, balanced by a touch of crispness and acidity. This is a very wellbalancedwine that is an absolute joy to consume. Available through the Nalle website for $42.00, I would put thiswine up against a Premier Cru Burgundy any day of the week. YUM! www.nallewinery.comPediatric Brains More Vulnerable to Injury,Concussion Clinic Opens at <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong>An increased amount of research over the years proves that pediatric brains are more vulnerable toinjury and pediatric patients experience more severe symptoms and require more time to recover froma concussion. The Missouri Interscholastic Youth Sports Brain Injury Act (“A youth athlete suspectedof sustaining a concussion or brain injury must be removed from competition at that time andfor at least 24 hours. He or she must not return to competition until being evaluated by alicensed health care provider trained in the evaluation and management of concussions.”)is a Missouri state law that requires children and adolescents to be seen immediately byconcussion experts.Research findings across multiple disciplines on pediatric concussions prompted theopening of <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong>’s new multidisciplinary concussion clinic. NeurologistRaman Malhotra, MD, and Neuro-Psychologist Stacey Woodrome, PhD, are the clinic’smain providers.Appointments are available every Wednesday from 8 a.m.-noon.Please call 314-577-5338 for an appointment.Practice Points:Managing Headaches in ChildrenSean Goretzke, MDDepartment Director of Child Neurology, <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> Children’s <strong>Medical</strong> <strong>Center</strong>Assistant Professor of Neurology, Saint Louis University School of Medicine4Headaches are not a rare occurrence in the pediatric population. Up to 60 percent of children will havea headache severe enough to seek medical care by the age of 18. Headache is consistently among the top10 reasons children visit the emergency room. As such a common occurrence, the most important initial job for the managingphysician is to sort out which children have headaches due to a dangerous cause and which are symptoms of what are termed“primary headache disorders.” It is important to remember that very basic things can cause headache such as viral or bacterialrhinosinusitis, eye strain, skipping meals and not getting enough sleep.
Acute HeadacheWith an acute headache, especially if referred to as “the worstheadache of my life”, we drift back to our medical school trainingand worry that a subarachnoid hemorrhage from a rupturedaneurysm may be the cause. Additionally, whether they tellyou or not, just about every parent of a child with recurrentheadaches is concerned that their child may have a brain tumor.Luckily, these are incredibly rare causes of headache in kids,though sometimes parental anxiety makes it difficult to keep anobjective eye on the facts at hand regarding the headache, andleads to a prompt emergency room or neurologic referral. Weare, of course, more than happy to help, though this article willtry to present some suggestions to help navigate these waters.MigraineThe “worst headache” scenario can be especially worrisome if itis the child’s first headache. In reality, most of these children turnout to have migraine, and this is, in fact, their first migraine.Younger children who are not used to severe degrees of pain maybe screaming for minutes to hours from a migraine headache.Often the patient’s family calls in to the office or after-hourspager, and you don’t have the luxury of examining the child. Ingeneral, if this headache occurs during exertion, or if it is associatedwith fainting, they should be taken to the emergency roomimmediately. Even then, it is most likely a migraine headache,though prompt medical attention is recommended. If the childhas had similar headaches in the past, though not as severe asthe current headache, and the child can tolerate oral medication,an appropriate dose of non-steroidal anti-inflammatory can berecommended. If there is not improvement within an hour ortwo, the child can be directed to the office for other medicationoptions.For the child with acute, intermittent, severe headaches, itis important to ask for other symptoms of migraine. Theseare similar to adults and include a throbbing quality, nauseaand/or vomiting, photo- and phonophobia and aggravationwith exercise. These headaches typically last 1-72 hours, andcontrary to adult criteria, can be bilateral in location. Thoughmost migraines occur in the fronto-temporal region of thehead, they can also occur in the posterior region in isolation.If the child meets criteria for migraine, it becomes appropriateto find an abortive agent. This can be as simple as a dose ofacetaminophen or ibuprofen (which are surprisingly effectivein children with migraine). There are many other options(both over the counter and prescription) that can be tried. Thefamily of triptan medications can safely be used in childrenwith migraine. These were initially not approved for children(though gaining acceptance over the years), not due to concernsover safety, rather because of the high rate of placebo effect inpediatric studies. Although as a child neurologist, I have usedthese medications down to age 6, effectively and safely, it isprobably reasonable for a primary care physician to limit the useto children ages 10-12 and up.Even if migraines are responsive to abortive agents, they canstill be quite interfering with the child’s life. If the patient isexperiencing more than 4-8 days per month where the headacheis affecting their ability to function normally, considerationshould be given to using a preventer (prophylactic) medication.These medications are taken daily (in addition to their abortiveagent as needed), with the goal of decreasing headaches down to1-3 days per month, or less. It is important to let families knowthat this will not eliminate all headaches, but should certainlymake them a more manageable and less frequent occurrence.Chronic Daily HeadacheThe last scenario is that of the child with “chronic dailyheadaches (CDH).” This refers to headache occurring morethan 15 days out of the month, and can often be an “all day,every day” phenomenon. This is a challenging condition, andcan take quite a lengthy office visit (or visits) to sort out. Theyare often multi-factorial in nature, and the patient may have afew different types of headaches involved in the process. Thisis probably the most common patient referred to our childneurology group, not only for the lengthy nature needed forthe visit, but also for ongoing parental frustration that “nothinghas worked.”It is important to identify any poor “headache hygiene” habitsthat may be a contributing factor in children with CDHs. Thisincludes amount and quality of sleep, eating habits, caffeineintake, overuse of pain relieving medication, prior or currentconcussive head injuries (often overlooked) and stress levels athome or school. Addressing these can often lead to a significantimprovement. For headaches that persist, especially if severe,features of migraine should continue to be sought out, andpreventative treatment of migraine may be of great benefit.“Red flags” for children with chronic headaches that shouldprompt consideration for imaging studies and/or pediatricneurology referral include:• Associated chronic illness (such as inflammatory orautoimmune disorders, an immune compromisedstate, history of systemic or CNS malignancy andneurofibromatosis)• Progressive severe worsening of the headache or newheadache type in someone with prior headaches• Headaches waking the child from sleep consistently• Associated systemic signs such as fever or weight loss• Young age (under 3 y/o)• Duration of headaches less than three months• Progressive neurologic complaints to include progressiveloss of vision (not simply visual aura’s of migraine),personality changes, new speech deficits, cognitivedecline and balance difficultiesAt <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong>, we are happy to provide expertmanagement of children with chronic headaches that areaffecting their ability to lead a happy and productive life. Tomake an appointment with one of our neurologists, please call314-577-5338 or 314-678-5444.5
of years. Recently, they got really bad. “I was sick all weekwith migraines, double vision and vomiting,” Marissasays. By the weekend she was worse, and on Sunday, Dec.18, 2011, Nancy called Marissa’s pediatrician’s physicianexchange. They were referred to <strong>SSM</strong> St. Joseph HospitalWest near their home where Marissa had a CT scan. Thescan revealed a mass in her head and she was transferred to<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> by ambulance the same evening.“We were met by a neurosurgery resident in the ER whenwe arrived,” Nancy says. “He was very good at explainingto us what was going on and the next steps that would betaken.”On Monday morning, the Deerings met Dr. Elbabaa whoordered an MRI of Marissa’s head. It showed that Marissahad a large meningioma brain tumor that arose from thesac at the mid-line and was compressing her brain. Atthis point, it was unclear if the tumor was cancerous. Dr.Elbabaa performed surgery the same day, and after fivehours the Deerings received the best news of their lives.“It was 3:31 p.m. on the nose, and we got a call sayingthat Dr. Elbabaa was closing and coming to talk with us,”Nancy remembers. “He said, ‘I have wonderful news. It’snot cancer,’” Nancy adds, “It was a Christmas miracle.”While in the hospital, Marissa slept a lot and noticedsome dizziness and short term memory loss. Dr. Elbabaaexplains that recovery time, as well as outcome andprognosis, depends on the location and pathology of thetumor. For example, if a tumor is near the brain stem,a prolonged period of rehabilitation may be required,whereas removal of a tumor closer to the brain’s surfacerequires less recovery time and causes fewer neurologicalimpairments. No matter the situation, Dr. Elbabaa makesthe patient and their family aware of the expected andpossible impairments prior to surgery.The Deerings made it home before Christmas, havingonly spent 4 days in the hospital. “Marissa’s recoveringunbelievably,” Nancy says.“Neurosurgery is a fascinating field where we can seeimmediate improvement,” Dr. Elbabaa says. “An excellentoutcome is dependent on surgical planning, coordinationand collaboration, and we spend a tremendous amountof time on all of this.”The average time it takes to remove a brain tumor isbetween 4-10 hours. Fortunately for Ryleigh and Marissa,their surgeries were completed in 4-6 hours and recoverytime was rather short. In other neurological cases, surgeryand recovery time is even quicker.8
Dr. Elbabaa removes a posterior fossa cerebellar tumor from a pediatric patient. A successfulneurosurgical outcome requires the collaboration of multiple specialties in the operating room,including neurosurgery, anesthesia, neurophysiology and technical support.9
EndoscopyIn the last 10-15 years, the practice of minimally-invasive neurosurgery has grown and become standard of care for themanagement of certain conditions at institutions with proper surgical expertise and technology. In contrast to an openneurosurgical procedure, minimally-invasive neurosurgery requires just a few small incisions, shortens recovery time andreduces pain, blood loss and scarring. The surgery, which typically lasts only 30-60 minutes, requires a tiny endoscope,small pump, video camera and a special light source. Dr. Elbabaa’s clinical and research specialties involve the practice ofminimally-invasive neurosurgery, most notably the minimallyinvasiveendoscopic treatment of hydrocephalus.As 14-month-old Lydia Garstang grew, her pediatrician, Dr.Douglas Barton of the St. Charles Clinic <strong>Medical</strong> Group,became increasingly concerned about the size of Lydia’s head.After ordering an ultrasound and CT scan, he referred theGarstangs to a geneticist at <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> whereLydia had an MRI. The MRI results prompted furthercollaboration among specialties, and that’s when the Garstangsmet Dr. Elbabaa. “Dr. Elbabaa was concerned with the resultsfrom Lydia’s MRI. He showed us that her ventricles wereenlarged and that the passage [aqueduct] was restricted,” RogerGarstang, Lydia’s father, says.Lydia was diagnosed with obstructive hydrocephalus, which iscaused by cerebrospinal fluid flow obstruction due to idiopathicaqueductal stenosis. Most commonly, hydrocephalus is treatedby the placement of a permanent shunt, but Dr. Elbabaa feltthat there was potential to treat Lydia’s case with the minimallyinvasiveprocedure endoscopic third ventriculostomy (ETV).“While we were worried about any condition or surgery thatdealt with the brain, Dr. Elbabaa explained the potentialbenefits and risks of ETV and we liked the idea of it versus theshunt procedure that is a life-long ordeal,” Roger says.10Exactly one monthago, Lydia Garstang(now 15 months old)had minimally-invasiveneurosurgery at <strong>SSM</strong><strong>Cardinal</strong> <strong>Glennon</strong>. Now,her small scars are hardlyvisible and she’s all smilesas she flies high on thepark swing.According to Dr. Elbabaa, multiple studies looking atcomplications, long term ETV success and riskfactors for failure in both adult and pediatricpopulations suggest outcomes comparableto or better than shunting. In selectpatients with obstructive hydrocephalus,ETV as an alternative to permanentshunting can avoid the high risk ofcomplications related to shunting.Ventricular shunts have up to 80%lifetime risk of complications and10% infection rate, mostly in the firstyear after implantation. The averagelife of a shunt is about 6-8 years.Lydia had her surgery on Jan. 16, 2012.Just a day after surgery, the Garstangs sayLydia was “feeling great and wanted to go homeand play.” During her hospital stay, Roger said the careDr. Elbabaa and his team had for their family was apparent.
“They kept us well informed, explaining every detail.They never just came in to our room, got to the point,and left. They stayed with us until all of our questionswere answered. I don’t think some of them ever sleep; Idon’t know how they do it,” he says.Lydia’s pediatrician, Dr. Barton, is also impressed withthe care and communication at <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong>.“I have found <strong>Cardinal</strong> <strong>Glennon</strong> to be increasinglyresponsive to patient/family and primary physicianneeds, and the addition of Dr. Elbabaa has markedlyelevated the quality and continuity of care provided topatients and their families, as well as the communicationlevel with the primary physician,” Dr. Barton says,adding, “Communication has largely been throughEPIC, and because of this I receive nearly immediateupdates regarding my patients’ experiences at <strong>Cardinal</strong><strong>Glennon</strong>. This was no different with Lydia. I receivedthe excellent level of communication that I have cometo expect from <strong>Cardinal</strong> <strong>Glennon</strong> specialists.” (See page2 to learn more about Epic Care Link.)When a child undergoes a serious operation, the parent’sand primary care physician’s expectations of everyoneinvolved in the child’s care are high, and rightfully so.For Marissa’s mother, Nancy, her expectations were met– “Everyone at <strong>Cardinal</strong> <strong>Glennon</strong> walks on water in mybook,” she says.1 2Endoscopic Applications inNeurosurgeryEndoscopic third ventriculostomy (ETV) for obstructivehydrocephalusEndoscopic tumor biopsy and removal for intraventriculartumorsEndoscopic fenestration of arachnoid cystsEndoscopic resection of colloid cystsEndoscopic simplification of multi-loculated hydrocephalusEndoscopic placement of ventricular catheters in shuntsEndoscopic trans-sphenoidal surgery for sellar and supra-sellartumorsEndoscope-assisted microsurgeryEndoscopic strip craniectomy for craniosynostosisEndoscopic choroid plexectomyEndoscopic aqueductoplastyEndoscopic spinal surgeryDr. Elbabaa’s Publications onMinimally-Invasive NeurosurgeryJournal publications:Elbabaa SK, Steinmetz M, Ross J, Moon D, LucianoM. “Endoscopic Third Ventriculostomy for ObstructiveHydrocephalus in the Pediatric Population: Evaluation ofOutcome.” European Journal of Pediatric Surgery. 2001.Endoscopic view of rightforamen of Monro is themost common approachview during an ETVprocedure.BEFOREA tiny balloon is usedto dilate the hole madeat the floor of the thirdventricle during anETV procedure.AFTERBedaiwy MA, Fathalla MM, Shaaban OM, RagabMH, Elbabaa SK, Luciano M, El-Nashar SA, FalconeT. “Reproductive Implications of Endoscopic ThirdVentriculostomy for the Treatment of Hydrocephalus.”European Journal of Obstetrics & Gynecology and reproductiveBiology. September 2008.Elbabaa SK and Luciano MG. “Endoscopic ThirdVentriculostomy.” Contemporary Neurosurgery. 1 June 2009.Simon JW and Elbabaa SK. “Revisiting EndoscopicVentricular Shunt Catheter Insertion and Revision in thePediatric Hydrocephalus Population: Risk Factors for Failure.”(Submitted to Child’s Nervous System)Sher E, Hanzlink E, Woodrome S, Luo QJ and ElbabaaSK. “A Neuropsychological Prospective on DifferentNeuro-Endoscopic Procedures in the Pediatric Population.”(In preparation for submission)Endoscopic view of asuprasellar arachnoid cystresulting in obstructivehydrocephalus.Endoscopic viewafter coagulationand fenestration.Textbook Chapters:Najjar J and Elbabaa SK. “Endoscopic Resection of ThirdVentricular Colloid Cyst.” Al-Mefty , O (2012). Controversies inNeurosurgery. Thieme. (In press)11
Q&ASamer K. Elbabaa,MD, FAANSDivision Director of Pediatric Neurosurgery at<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> Children’s <strong>Medical</strong> <strong>Center</strong>Assistant Professor, Department of Neurological Surgeryat Saint Louis University School of MedicineQ: Why did you specialize in neurosurgery?A: There are still so many unknowns in neurosurgery and a great potential to improve the field. I chose pediatricsbecause I like children. Their honesty and desire to get better and back on the playground makes my job evenmore gratifying and fulfilling.Q: What do you like best about your job?A: I like that there are multiple ways to do the same surgery and the outcomes are immediate. My background andmentorship have given me a balanced approach to various neurosurgical conditions and procedures, ranging fromcomplex microsurgical procedures to minimally-invasive endoscopic techniques.Q: How have the neurosurgical services at <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> grown in the past year?A: Since my arrival less than a year ago, we’ve expanded the neurosurgical clinic timeframe to absorb all referralsin a timely manner, added a separate clinic where our neurosurgical nurse practitioner sees patients and recruiteda neurosurgery clinical nurse. In the near future, my goal is to recruit another pediatric neurosurgeon. We’ve alsoadded state-of-the-art minimally-invasive endoscopy equipment for minimally-invasive neurosurgical procedures,as well as a state-of-the-art operating microscope for complex microsurgical procedures.Q: Is there a particular patient care philosophy that guides you?A: I pay respect to the fine details of every patient and treat all children the way I’d want my own children to betreated. I also remember to never lose hope for an improvement, even when the chances are slim.To reach Dr. Elbabaa, please call 314-577-5306 or e-mail selbabaa@slu.edu.To schedule an appointment with the neurosurgery team at <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong>, please call 314-678-2182.12
NeurosurgeryFacultySamer K. Elbabaa, MD, FAANSDivision Director of Pediatric Neurosurgery, <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> Children’s <strong>Medical</strong> <strong>Center</strong>Assistant Professor, Department of Neurological Surgery at Saint Louis University School of MedicineMD: University of JordanInternship, General Surgery: University of North Carolina at Chapel HillResidency, Neurosurgery: University of North Carolina at Chapel HillChief Residency, Neurosurgery: University of North Carolina at Chapel HillClinical Fellowship, Pediatric Neurosurgery: The Cleveland ClinicMicrosurgery: University Hospital Zurich, Zurich, SwitzerlandNeurosurgeryClinical StaffCathy Gross, RN, MSN, CPNPNeurosurgery Advanced Practice Nurse, <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> Children’s <strong>Medical</strong> <strong>Center</strong>BSN: Jewish Hospital College of NursingMSN: Saint Louis UniversityRachel Elledge, RNNeurosurgery Clinical Nurse, <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> Children’s <strong>Medical</strong> <strong>Center</strong>ASN: Jewish Hospital College of Nursing(From left to right) Rachel Elledge, RN; Samer K. Elbabaa, MD, FAANS; Cathy Gross, RN, MSN, CPNP13
Non Profit OrgU.S. PostagePAIDSt. Louis, MOPermit No. 2412Physician Services Department1465 South Grand Blvd.Saint Louis, Missouri 63104-1095Get into the Swing of it!Every home run the <strong>Cardinal</strong>s hittallies a win for our kids!Make your pledge today! glennon.orgThanks to our sponsors:Presented by:Powered by:Grand Slam:On Deck: