Pediatrics - SSM Cardinal Glennon Children's Medical Center
Pediatrics - SSM Cardinal Glennon Children's Medical Center
Pediatrics - SSM Cardinal Glennon Children's Medical Center
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
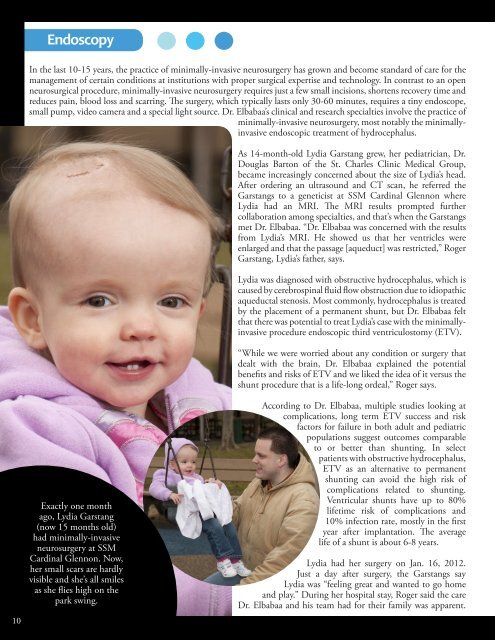
EndoscopyIn the last 10-15 years, the practice of minimally-invasive neurosurgery has grown and become standard of care for themanagement of certain conditions at institutions with proper surgical expertise and technology. In contrast to an openneurosurgical procedure, minimally-invasive neurosurgery requires just a few small incisions, shortens recovery time andreduces pain, blood loss and scarring. The surgery, which typically lasts only 30-60 minutes, requires a tiny endoscope,small pump, video camera and a special light source. Dr. Elbabaa’s clinical and research specialties involve the practice ofminimally-invasive neurosurgery, most notably the minimallyinvasiveendoscopic treatment of hydrocephalus.As 14-month-old Lydia Garstang grew, her pediatrician, Dr.Douglas Barton of the St. Charles Clinic <strong>Medical</strong> Group,became increasingly concerned about the size of Lydia’s head.After ordering an ultrasound and CT scan, he referred theGarstangs to a geneticist at <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> whereLydia had an MRI. The MRI results prompted furthercollaboration among specialties, and that’s when the Garstangsmet Dr. Elbabaa. “Dr. Elbabaa was concerned with the resultsfrom Lydia’s MRI. He showed us that her ventricles wereenlarged and that the passage [aqueduct] was restricted,” RogerGarstang, Lydia’s father, says.Lydia was diagnosed with obstructive hydrocephalus, which iscaused by cerebrospinal fluid flow obstruction due to idiopathicaqueductal stenosis. Most commonly, hydrocephalus is treatedby the placement of a permanent shunt, but Dr. Elbabaa feltthat there was potential to treat Lydia’s case with the minimallyinvasiveprocedure endoscopic third ventriculostomy (ETV).“While we were worried about any condition or surgery thatdealt with the brain, Dr. Elbabaa explained the potentialbenefits and risks of ETV and we liked the idea of it versus theshunt procedure that is a life-long ordeal,” Roger says.10Exactly one monthago, Lydia Garstang(now 15 months old)had minimally-invasiveneurosurgery at <strong>SSM</strong><strong>Cardinal</strong> <strong>Glennon</strong>. Now,her small scars are hardlyvisible and she’s all smilesas she flies high on thepark swing.According to Dr. Elbabaa, multiple studies looking atcomplications, long term ETV success and riskfactors for failure in both adult and pediatricpopulations suggest outcomes comparableto or better than shunting. In selectpatients with obstructive hydrocephalus,ETV as an alternative to permanentshunting can avoid the high risk ofcomplications related to shunting.Ventricular shunts have up to 80%lifetime risk of complications and10% infection rate, mostly in the firstyear after implantation. The averagelife of a shunt is about 6-8 years.Lydia had her surgery on Jan. 16, 2012.Just a day after surgery, the Garstangs sayLydia was “feeling great and wanted to go homeand play.” During her hospital stay, Roger said the careDr. Elbabaa and his team had for their family was apparent.