Major Salivary Gland Imaging1
Major Salivary Gland Imaging1
Major Salivary Gland Imaging1
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
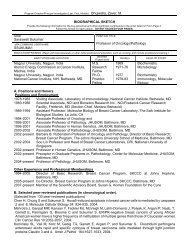
State of the ArtDavid M. Yousem, MDMichael A. Kraut, MD, PhDAra A. Chalian, MDIndex terms:<strong>Salivary</strong> glands, calculi, 264.818<strong>Salivary</strong> glands, CT, 264.12111,264.12112<strong>Salivary</strong> glands, diseases, 264.247<strong>Salivary</strong> glands, MR, 264.12141,264.12143<strong>Salivary</strong> glands, neoplasms, 264.363,264.37<strong>Major</strong> <strong>Salivary</strong> <strong>Gland</strong> Imaging 1The algorithm for imaging the salivary glands depends on the clinical scenario withwhich the patient presents to the clinician. Because of the importance of identifyingsmall calculi in the gland or salivary duct as the cause of the symptom complex,nonenhanced computed tomography is often the best initial study for the evaluationof the painful gland. If an infiltrative neoplasm is highly suspected, nonenhanced andenhanced magnetic resonance (MR) imaging may be superior in demonstratingperineural, meningeal, and skull base invasion. Sialography is reserved for theevaluation of chronic sialadenitides unrelated to sialolithiasis. Thin-section MRtechniques for MR sialography may soon replace conventional sialography.Radiology 2000; 216:19–29Abbreviations:HIV human immunodeficiency virusSE spin echo1From the Department of Radiology,Johns Hopkins Hospital, 600 N WolfeSt, Houck B-112, Baltimore, MD 21287(D.M.Y., M.A.K.), and the Departmentof Otorhinolaryngology: Head andNeck Surgery, University of PennsylvaniaMedical Center, Philadelphia(A.A.C.). Received January 22, 1999;revision requested March 30; finalrevision received August 6; acceptedAugust 18. Address correspondenceto D.M.Y. (e-mail: yousem@rad.jhu.edu). RSNA, 2000While neoplasms of the major salivary glands constitute less than 3% of all tumors in thebody, many people have an illness related to the salivary glands at some time in their lives.The process may be self-limited, such as with viral parotitis or mumps, but in others it maybe a relapsing and remitting illness, such as chronic sialadenitis secondary to sialolithiasis.Still others may be evaluated for what is thought to be a salivary gland mass but is actually amass peripheral to the glands, such as a lymph node. Very rarely, a nonnodal extraglandularlesion such as a schwannoma, masseteric hypertrophy, or other pseudomass may be mistakenfor a glandular process, even by experienced otorhinolaryngologists (1). The purpose of thisreview is to illustrate the role of imaging in evaluating diseases of the major salivary glands.The range of studies needed to assess salivary gland lesions spans a wide gamut. Many ofthe disease processes described above may not require imaging of any kind. Still others maybe readily evaluated with palpation and direct visualization either endoscopically ortransorally. At the other end of the spectrum are infiltrative deep lobe parotid masses suchas adenoid cystic carcinomas, which may require computed tomography (CT), magneticresonance (MR) imaging, and/or conventional angiography as part of a preoperativeevaluation for perineural, vascular, or skull base infiltration. Ultrasonography (US),underutilized in most North American sites, may supplant the role of CT and MR imagingfor superficial salivary gland lesions when experienced sonographers use the technique.Patients with major salivary gland lesions may present to the otorhinolaryngologist ororal and maxillofacial surgeon with a suspected mass, with a suspected obstruction orinflammation, or with diffuse glandular enlargement (2). Although there are overlappingentities in this simple stratification, the imaging studies ordered may change with eachpresentation. For the purposes of this review, major salivary gland imaging will be dividedinto neoplastic lesions, obstructive or inflammatory lesions, and systemic diseases.NEOPLASTIC LESIONSThe usual clinical manifestation of a salivary gland neoplasm is that of an enlarging mass.The first critical step in evaluating a mass is to determine whether or not it is painful. Whilepainful masses may be produced by obstructive or inflammatory disease, the classicpainless mass in the salivary glands is usually due to a neoplasm, cyst, or lymph node. Adull, gnawing pain may be produced by some neoplasms in the glands. Other signs that aparotid neoplasm is malignant are infiltration of the overlying skin, regional adenopathy,or facial nerve palsy. Regional lymph node spread is relatively infrequent with salivarygland primary malignancies.There are some general rules that apply to salivary gland neoplasms. The smaller thesalivary gland, the higher the rate of malignancy. Thus, the rate of malignancy increasesfrom 20%–25% in the parotid gland to 40%–50% in the submandibular gland and to50%–81% in the sublingual glands and minor salivary glands (3–6). Nearly 80% of benignparotid neoplasms are pleomorphic adenomas (3,4). Pleomorphic adenomas, also known19
Figure 1. Bilateral Warthin tumors. Bilateralparotid masses (arrows) are seen on this transverse,contrast material–enhanced, fat-saturatedT1-weighted spin-echo (SE) (750/30 [repetitiontime msec/echo time msec]) MR image.The multiplicity and location at the tail of theparotid gland (near the lower mandible) aretypical features of this tumor.a. c.Figure 3. Pleomorphic adenomas. (a) TransverseT1-weighted SE (600/11) MR image showsthe mass (P) to be well highlighted against thenormal hyperintensity of the parotid gland.The margination is not particularly sharp, yetthe diagnosis was pleomorphic adenoma.(b) The mass (P) is hyperintense on this transverse,long repetition time (4,000 msec), T2-weighted fast SE MR image. (c) The mass (P )enhances on this contrast-enhanced, T1-weighted SE (600/30) MR image, though it hasa central nonenhancing component.Figure 2. Submandibular pleomorphic adenoma.Transverse, contrast-enhanced CT scanshows that the pleomorphic adenoma (A) arisesin the right submandibular gland. The attenuationcharacteristics leave little indication as towhether the lesion is benign or malignant.as benign mixed tumors, occur most commonlyin middle-aged women. Monomorphicadenomas and myoepitheliomas arethe other common benign tumors andmay arise in both parotid and submandibularglands. Oncocytomas and Warthin tumorsare rare outside the parotid region.Multiple parotid masses are usually dueto lymphadenopathy or Warthin tumors,the latter appearing almost exclusively inthe parotid gland, usually in the tail ofthe gland in older men (Fig 1). The mostcommon malignancy of the parotid glandis mucoepidermoid carcinoma (2,3). Inthe submandibular gland, pleomorphicadenomas remain the most common benigntumor (Fig 2), but adenoid cysticcarcinoma is the most common malignanthistologic diagnosis (5). The samediagnoses prevail in the sublingual andminor salivary glands (7), where malignanciesoutnumber benign tumors.Lymph nodes may manifest as intraparotidmasses. Since the parotid gland encapsulateslate in the 2nd trimester, itincorporates lymphatic tissue, whereasb.the other salivary glands do not. Thisaccounts for the potential for malignantadenopathy involving the parotid glands.This is usually seen in the setting of adermatologic malignancy (basal cell carcinoma,squamous cell carcinoma, andmelanoma), but occasionally an upper aerodigestivesystem squamous cell carcinomamay result in malignant parotid adenopathy.The lymph nodes must be determinedto be intraparotid or extraparotidat imaging. By the same token, lymphomamay occur primarily in the parotidgland as an infiltrative process oradenopathy, or as a manifestation of systemicdisease.Some would advocate the use of MRimaging as the first (and only) techniqueto evaluate a neoplasm of the major salivaryglands. Implicit in such a decision isthat the clinicians are highly confidentthat the process in the gland is neoplasticand not obstructive or inflammatory. Ifthere is even a slight chance that the massmay in some way be related to sialolithiasis,CT should be recommended first,since MR imaging is not as reliable indetecting small calculi, and ‘‘pseudomasses’’may accompany sialolithiasis (seeObstructive or Inflammatory Lesions).If there is very strong suspicion that alesion is neoplastic, there are some compellingreasons why MR imaging may bepreferred over other modalities. Virtuallyall parotid lesions are well visualized onT1-weighted MR images because of thehyperintense (fatty) background of thegland (Fig 3) (8). The T1-weighted imagegives an excellent assessment of the marginof the tumor, its deep extent, and itspattern of infiltration. This sequence,coupled with fat-saturated, contrast material–enhancedT1-weighted imaging, usedprimarily to address perineural spread(9,10), bone invasion, or meningeal infiltration,is the best means for ‘‘mapping’’the tumor. If there is a superimposeddiffuse inflammatory process, a focal masscould possibly be obscured with this sequence.On fat-saturated images, boththe bone marrow and cortex of the mandible,maxilla, and skull base will behypointense. Enhancing (hyperintense)tissue extending into this hypointensebackground is indicative of bone invasion.At the skull base, where the abundantfat and bony foramina will also havesuppressed signal (low signal intensity),the fat-saturated, contrast-enhanced imagewill show spread of hyperintenseenhancing tumors up the stylomastoidforamen (cranial nerve VII) (Fig 4), foramenovale (cranial nerve V-3), or foramenrotundum (cranial nerve V-2). Therefore,if a facial or trigeminal nerve palsy accom-20 • Radiology • July 2000 Yousem et al
a.b.Figure 4. Perineural infiltration of cranialnerve VII by adenoid cystic carcinoma. (a) TransverseT1-weighted SE (600/11, two signals acquired)MR image shows that the right parotidmass (m) enters the notch of the stylomastoidforamen (arrow). (b) Coronal, gadoliniumenhancedT1-weighted SE (600/17, one signalacquired) MR image shows vertical extensionof the enhancing tumor (arrows) through thestylomastoid foramen (line is at the plane oftransverse image in a).panies a mass, MR imaging is usually thestudy of choice. If meningeal symptomscoexist, MR imaging may also be preferredsince the leptomeninges are betterassessed with MR than with CT (11).On nonenhanced and enhanced T1-weighted series, no histologic discriminationis possible since almost all masses arelower in intensity than the parent glandand almost all salivary gland neoplasmsenhance. Deep infiltration into the parapharyngealspace, muscles, and bone, wellseen on T1-weighted images, will stronglysuggest malignancy (4) or, less frequently,rupture of the capsule of a pleomorphicadenoma (Fig 5). While benign and malignantmasses exhibit considerable overlapFigure 5. Seeding of pleomorphic adenoma.Parotid (arrow) and deep lobe or parapharyngeal(arrowheads) masses are present on the leftside on this transverse T1-weighted SE (500/11)MR image. The patient underwent prior attemptedresection of a deep lobe pleomorphicadenoma, but the capsule of the tumor wasviolated. Months later she presented with thispicture of tumor infiltrating the operative bedand the surrounding tissue.with regard to geographic properties suchas margins, shapes, and borders (Fig 6)(12,13), T2-weighted MR imaging hasbeen shown to be a reasonably reliable(73%) predictor of whether a salivarygland tumor is benign (Fig 7) or malignant(14,15). The conventional wisdomis that a hyperintense mass on T2-weighted images is benign and a mass oflow to intermediate signal intensity ismalignant. Others have implied that signalintensity on T2-weighted images is oflittle help (4,13). In general, however, themost common benign tumor of the salivaryglands, the pleomorphic adenoma,has very high signal intensity on T2-weighted images (Fig 7) (13). Benign cysts(mucous retention cyst, lymphoepithelialcyst, first branchial cleft cyst, ranula,sialocele, and pseudocysts) may also behyperintense on T2-weighted images,and, depending on the presence of hemorrhage,infection, or hyperproteinaceousfluid, the T1-weighted image may showintermediate (solid-appearing) intensity.For this reason, administration of contrastmaterial is helpful because cystsusually enhance on their periphery,whereas pleomorphic adenomas enhancesolidly (Figs 3c, 7b). The value of contrastenhancement applies also to CT becausethe attenuation of the cyst may not bethat of pure fluid, particularly when traumatized,infected, or hyperproteinaceous.Most high-grade mucoepidermoid carcinomas,undifferentiated carcinomas, adenocarcinomas,and squamous cell carcinomasof the major salivary glands havelow to intermediate signal intensity onlong repetition time images (Fig 8). Somemalignancies, however, exhibit elevatedsignal intensity on T2-weighted images.Most commonly, this is seen in low-grademucoepidermoid carcinomas (14), insome adenoid cystic carcinomas (15), andrarely in adenocarcinomas. Among benignmasses that are not hyperintense onlong repetition time images, Warthin tumor,the second most common benignmass in the adult parotid gland, is oftenof intermediate, low, or mixed signal intensityon T2-weighted images (8). Thechronic sialadenitides, such as Sjögrendisease, Mikulicz disease (also known asSjögren type 1 or sicca syndrome withouta connective tissue disorder), and radiationsialadenitis, may also appear hypointenseon T2-weighted images (14). Inmost series, these exceptions account forthe 25% error rate that occurs if one reliessolely on signal intensity on T2-weightedimages to predict histologic diagnosis.The CT attenuation of masses, otherthan for differentiating benign cysts fromsolid masses, and lipomas from otherneoplasms (Fig 9), does not help in predictinghistologic diagnosis since mostmalignant and nonmalignant solidmasses have similar CT attenuation (Fig10). Although high-grade malignanciestend to have irregular infiltration into theglandular parenchyma (13,16), which canbe detected with both MR imaging andCT, there are enough exceptions to thisrule that CT has only fair accuracy (60%–70%) in predicting the histologic diagnosisof a lesion (17). Because CT appearanceis not a good predictor of histologicdiagnosis and since CT is less accuratethan MR imaging for determining theextent of disease (16), there is little reasonto advocate CT over MR imaging in thesetting of a suspected salivary gland mass.However, neither study can be relied uponwholly to predict histologic diagnosis;hence, fine-needle aspiration or biopsy isusually required to establish the diagnosisin the major salivary glands.Nuclear scintigraphy may help diagnoseWarthin tumors (cystadenoma lymphomatosum)and oncocytomas. Thesetumors are unique in that they showincreased radiotracer uptake at technetiumpertechnetate imaging. Since neitherof these lesions has substantial malignantpotential, a course of observationmay be advocated in the elderly patientwith surgical contraindications. This is incontrast to the treatment of pleomorphicadenomas. Since pleomorphic adenomashave the potential for malignant degenerationand/or coexistent adenocarcinoma,they are treated more aggressivelyVolume 216 • Number 1 <strong>Major</strong> <strong>Salivary</strong> <strong>Gland</strong> Imaging • 21
Figure 6. Right submandibular gland adenocarcinoma.Transverse CT scan shows anexophytic, well-defined mass (M) in the rightsubmandibular region that proved to be an adenocarcinoma.First and foremost, one should attemptto determine whether this lesion is asubmandibular lymph node metastasis or aprimary lesion from the submandibular gland(as in Fig 2). The anterior facial vein, whichusually lies between submandibular and extraglandularmasses (1), was not conspicuous inthis case. The gland and mass were resectedtogether, and the origin from the submandibulargland was uncovered. Although this lesionwas well defined, it was malignant (comparewith Fig 2).a. b.Figure 7. Pleomorphic adenoma. (a) Transverse T2-weighted SE (3,000/80, one signal acquired)MR image shows that the lesion ( * ) is hyperintense. This may raise the question of a cyst versus apleomorphic adenoma. (b) With administration of a gadolinium-containing contrast agent andfat saturation, the mass ( * ) is seen to enhance avidly on this coronal T1-weighted SE (600/17, onesignal acquired) MR image, compatible with a solid mass.a. b.Figure 8. Mucoepidermoid carcinoma of the parotid gland. (a) Transverse T2-weighted SE(3,000/90) MR image shows an intermediate-signal-intensity mass (arrow) slightly lower inintensity than that of the native parotid tissue. (b) The ill-defined nature of the mass (arrow) wasexemplified by the fuzzy margins on this transverse, contrast-enhanced, fat-saturated, T1-weighted SE (600/30) MR image. The diagnosis was high-grade mucoepidermoid carcinoma.with surgical extirpation (18). Positronemission tomography (PET) has beenstudied to see if it can reliably predicthistologic diagnosis (19). At an accuracyrate of 69%, PET compared unfavorablywith accuracy rates reported for MR imaging(14,15,19). Therefore, the role of scintigraphyis usually limited to confirmingthe clinical diagnosis of Warthin tumorsin those patients with multiple parotidmasses.US is a useful technique to assess superficialparotid, submandibular, and sublingualmasses (20,21). US is not as readilyused in North America, and the expertisein interpreting sonograms of the headand neck is not as widespread in theUnited States as it is in Europe and Japan.In appropriate hands, however, US canhelp analyze superficial salivary glandlesions with the same precision as CT andMR imaging. Gritzmann (22) demonstratedin a blinded retrospective review that 287(95%) of 302 space-occupying lesions ofthe major salivary glands (285 in theparotid, 13 in the submandibular, andfour in the sublingual glands) could becompletely delineated at US. All 302 neoplasmswere hypoechoic to normal glandulartissue. US enabled correct assessmentof whether a lesion was benign or malignantin 272 cases (90%) on the basis ofdefinition of the margins of the tumor,but 28% of malignant lesions (16 of 58lesions) were misinterpreted as being benign(22). US differentiated extraglandularfrom intraglandular lesions with anaccuracy of 98% (all mistakes were periparotidlymph nodes). Other reports haveconfirmed that US also does an excellentjob in enabling distinction of glandularfrom extraglandular masses (23). This differentiationis helpful to the otorhinolaryngologistwho may not be able to discernthe planes as well by means of palpation.Malignant salivary tumors show a highergrade of vascularity at color Doppler USthan do benign tumors (24). Peripheralvascularity with a hypovascular centerimplies a pleomorphic adenoma (24). Theechotexture of lymphoma is finer thanthat in benign adenopathy (25).The limitations of US (even in the bestof hands) include its inability to evaluatedeep parotid masses, lesions obscured bythe mandible, parapharyngeal extension,retropharyngeal and deep neck adenopathy,and the intracranial or skull baseextent of a mass (22). US shows a lack ofspecificity for cystic lesions, and the relationshipof a tumor to the facial nerve ishard for surgeons to appreciate on USimages.22 • Radiology • July 2000 Yousem et al
a.Figure 10. Mucoepidermoid carcinoma of theparotid gland. Transverse CT scan shows anill-defined mass (C) that has less attenuationthan that of enhancing parotid tissue in theright parotid gland. The attenuation of thismass is the same as that of the pleomorphicadenoma in Figure 2 and less than that of thecarcinoma in Figure 6.Figure 11. Markers for the seventh cranialnerve. Transverse T1-weighted SE (500/11) MRimage shows that the seventh cranial nerveemerges from the stylomastoid foramen tocourse through the fat (straight arrow) immediatelybelow this exit. In its course through theparotid gland (p), it runs lateral to the retromandibularvein (curved arrow). This is the bestsequence for defining anatomic landmarks.b.Figure 9. Lipomas. (a) Although the attenuationof this patient’s parotid glands is low dueto fatty infiltration on this transverse CT scan,a palpable (see marker superficially) lipoma (L)in the left parotid gland was appreciated.(b) This lipoma (arrow), hyperintense on thistransverse T1-weighted SE (600/11) MR image,was extraglandular but still contained by thedeep cervical fascia surrounding the gland.To the surgeon, it is the facial nervethat is the critical structure when operatingon the parotid gland. By contrast,submandibular and sublingual glandulartumors are removed with relative impunity.While submandibular and sublingualgland resections can injure the lingualnerve or hypoglossal nerve andpossibly the marginal branch of the facialnerve, these deficits are easily compensatedfor by the patient. However, theconsequences of facial nerve injury are sosubstantial functionally and cosmeticallythat much effort is directed toward teasingout the trunk and peripheral branchesof the facial nerve before even addressingthe mass. Though some parotid malignanciesmay manifest with facial nerve impairment(24%) (2), a new postoperativefacial paralysis is the bane of the surgeonand the patient.Even with thin-section MR imaging,there is controversy as to the reliableidentification of the facial nerve belowthe skull base (26–29). Its course is surmisedby its egress from the stylomastoidforamen; its passage anterior to the posteriorbelly of the digastric muscle, lateralto the plane of the stylomandibular tunnel,and around the retromandibular vein;and its branching pattern to the musclesof facial expression (30–32) (Fig 11). Theline connecting the lateral surface of theposterior belly of the digastric muscle andthe lateral surface of the mandibular ascendingramus has also been used toseparate superficial (lateral to the facialnerve) and deep (medial to the facialnerve) parotid masses (33). The differentiationof deep or superficial parotidmasses is critical from the standpoint ofthe extent of dissection needed to separatethe nerve from the tumor or to gainaccess to the tumor, the attendant risk tothe facial nerve, and, in the case of tumorsextending into the parapharyngealspace, the need for a cervical approachwith or without mandibulotomy (6).Demonstration or suspicion of direct invasionof the nerve at the stylomastoidforamen (or above) prods the surgeon toplan for transmastoid identification ofthe facial nerve to control disease andprevent tumor spillage. The superficialparotidectomy thereby becomes skull basesurgery with its attendant risks (to theother cranial nerves, venous sinuses, carotidartery, and temporomandibular jointfunction) and morbidity. If the nerve atthe skull base is invaded, the cartilaginousauditory canal may have to be addressedand possibly resected. A radicalmastoidectomy is contemplated and eventhe ascending ramus of the mandiblemay be removed (6). MR imaging doeswell in demonstrating the perineural, vascular,and dural invasion that may bepresent with parotid malignancies (34).Adenoid cystic carcinoma has a veryhigh rate of perineural spread (50%–60%)(35). It is the most common malignancyto affect the minor salivary glands andthe sublingual gland, and it is one of thethree most common tumors of the parotidand submandibular glands. Visualizationof the cranial nerves and tumoralinfiltration around these nerves to andthrough the skull base is probably bestevaluated by using nonenhanced andgadolinium-enhanced, fat-saturated, T1-weighted MR sequences (9,10,34).Multiple painless masses in the parotidVolume 216 • Number 1 <strong>Major</strong> <strong>Salivary</strong> <strong>Gland</strong> Imaging • 23
a. b.Figure 12. CT-guided aspiration of deep lobeparotid mass. Via a transbuccal approach, theneedle passed between the ascending ramus ofthe mandible and the maxilla, with its tip(arrow) at the edge of the deep lobe parotidmass (P). Several 2-cm thrusts into the massunder syringe suction and transverse CT guidanceyielded cells compatible with mucoepidermoidcarcinoma. The well-defined margins beliedthe malignant nature of the mass.c. d.Figure 13. (a–d) Transverse CT scans of ductal and glandular calcifications. (a) There is a largesolitary sialolith (arrow) in the right submandibular duct. (b) These glandular calcifications(arrows) could easily be mistaken for vessels on this contrast-enhanced CT scan. (c) Are thesevessels or calcifications (arrows) along this ill-defined monomorphic adenoma of the submandibulargland? (d) Image obtained with bone window settings is equivocal due to the small size of theopacities (arrows), but the nonenhanced scans showed that the posterolateral one was acalcification and the anteromedial structure was a vessel, hence the value of a nonenhanced scan.gland invoke a differential diagnosis ofWarthin tumors (Fig 1) (36), multiplepleomorphic adenomas (18), oncocytomas,lymph nodes, lymphoma, acinic cellcarcinoma, metastases (37), human immunodeficiencyvirus (HIV)–related cystsand nodules (38), and Sjögren syndrome(39,40). Lymphoma, associated with Sjögrensyndrome or not, may infiltrate theentire parotid gland or present as multiplelymph nodes in the gland. Cysticdegeneration of a benign-appearing neoplasmsuggests a Warthin tumor or pleomorphicadenoma (41).Perhaps the most useful study that onecan perform to ascertain the nature of apainless mass in the salivary glands isimage-guided aspiration or biopsy (Fig12). The request for image-guided aspirationsmost often arises when a deep lobeparotid mass or parapharyngeal space ectopicminor salivary gland lesion is incidentallydiscovered. Since the lesions arenonpalpable and difficult to approachendoscopically, the radiologist may becalled on to obtain a tissue sample.Whether or not one chooses to puncturethe lesion from the anterior face via aretromaxillary (transbuccal) or a transparotidapproach depends on the comfortlevel of the radiologist and the course ofthe carotid vessels with respect to themass. Cytologic aspirates with 22-gaugespinal needles are usually sufficient, butoccasionally core biopsies of the glandwith 18–20-gauge needles may be requiredfor a definitive diagnosis. Becauseof the precarious position of the facialnerve, a core biopsy is generally shunnedin sampling parotid masses. It should benoted that inflammatory masses of thesalivary glands may mimic epithelial neoplasmsat cytology because desquamatedcells frequently populate the former. Thisis a known potential pitfall of head andneck cytology and accounts for manyinaccurate aspiration results (42,43).In those cases in which the diagnosis isknown from a biopsy or aspiration performedunder palpation guidance, theemphasis in imaging should shift towarddelineation of the size and extent of themass rather than histologic discrimination.Once again, symptoms may suggestone modality over another since the presenceof cranial nerve palsies, meningealsigns, venous obstruction, and fixation ofthe mass to vital structures such as thecarotid artery may lead to a preference forMR imaging, but bone pain and adenopathymight suggest that CT is the favoredmodality.Some head and neck surgeons do notperform any imaging or aspirations priorto operating on a salivary gland mass.This is usually in the setting of a superficialpainless mobile parotid mass withnormal facial nerve function (presumedto be a pleomorphic adenoma).OBSTRUCTIVE ORINFLAMMATORY LESIONSMost patients with sialolithiasis (salivarygland calculi) will have the cardinal signsof pain and swelling of the gland (44–47).Sialolithiasis is the second most commondisease of the salivary glands after mumps(44). The gland may be diffusely or focally24 • Radiology • July 2000 Yousem et al
sialoliths, the surgeon may decide to treatthe patient with resection of the gland.This is often the preferred treatment forpatients with recurrent bouts of sialolithiasiswith sialadenitis, since this regionof the duct is not well accessed transorally.A cervical (submandibular) surgicalapproach may be taken with sialolithsthat extend beyond the mylohyoid (inthe proximal duct).Most of the imaging modalities that aresensitive to calculi, such as conventionalradiography, CT (48), and US (49,50), candemonstrate sialoliths with high accuracy.Of 185 patients with major salivarygland calculi, calculi were identified andlocalized correctly (intraductal vs intraglandular)with US in 174 patients (94%)reported in Gritzmann’s review (22). Fourteenof the 174 cases detected at US werenot evident at conventional radiography.However, US is less accurate than CT indistinguishing multiple clusters of stonesfrom single large stones (48,50). Generally,CT in this setting is best performedwithout administration of contrast material,since small opacified blood vesselsmay simulate small sialoliths (Fig 13). Ifan abscess or inflammatory process issuspected, adding enhanced scans afteridentifying stones on nonenhanced scansmay be useful.Recently, some investigators have advocatedfast T2-weighted MR imaging withthin sections to noninvasively evaluatethe ductal architecture of the salivaryglands and to identify stones (Fig 14).Although beautiful images of the salivaryductal system can be generated with thinsection,T2-weighted MR imaging (51–53), tiny calculi within the gland andeven in the larger ductal system can beoverlooked on MR images because of thesignal void associated with the calcifiedstone. Clearly, CT, US, and simple conventionalradiography will enable identificationof the calculi, but MR imaging affordsthe opportunity to visualize the effectthe sialolith has on the ductal system. Isthis necessary? In most instances, theanswer is no. However, in those cases of apainful gland associated with chronic sialadenitiswithout a sialolith seen at CTor conventional radiography, the irregularityof the ductal system may give a clueas to the cause of the painful gland.Strictures may be present where a sialolithhas resided. The poor outflow of salivaleads to chronic sialadenitis. In other cases,the sialadenitis may not be from calculibut may be due to autoimmune inflammatoryconditions that have a signaturesialographic appearance—pruned, truncatedmain ducts with punctate or globua.c.b. d.Figure 14. Submandibular calculi visualized at MR imaging. (a) Transverse T1-weighted SE(500/11) MR image shows two areas of low signal intensity (arrows) in the floor of the mouth onthe left. (b) These calculi (arrows) are confirmed on this transverse T2-weighted SE (4,000/80) MRimage, and the obstructed duct (arrowhead) is evident. Inflammation around the stones accountsfor some peripheral high signal intensity. (c) The duct (arrowhead) can also be seen on thiscontrast-enhanced, T1-weighted, fat-saturated, spoiled gradient-echo (35/2.1, 30° flip angle) MRimage. The walls enhanced, presumably due to inflammation (sialodochitis). (d) There wascoincidental sialadenitis of the left submandibular gland seen as enlargement and high signalintensity on this transverse, fat-saturated, T2-weighted fast SE (4,000/80) MR image. Noteintraglandular ductal dilatation (arrows).enlarged with a sialolith in the proximalduct.Sialolithiasis is predominantly a diseaseof the submandibular gland since80%–82% (143 of 174) of sialoliths occurhere (22,44). Sialoliths form more frequentlyin the submandibular gland becauseof the more alkaline, thicker, andviscous saliva the submandibular gland produces.Other factors that predispose to stasisin the Wharton duct (eg, an uphillcourse, a dependent gland, a wider lumen,and a tighter orifice) may play a roleas well. Calculi may be multiple (25%)and may occur within intraglandular ductaltributaries or within the main ducts.When in the gland itself, the symptomsmay be relatively minor, whereas ductalsialoliths usually have a more precipitouspresentation (44).Ductal calculi may initially be treatedwith secretagogues and/or dilation of theduct. Transoral resection of sialoliths andsialodochoplasty can be performed forisolated distal duct (close to the ampulla)sialoliths. Imaging may help define thelocation of isolated nonpalpable or multiplesialoliths. For proximal or glandularVolume 216 • Number 1 <strong>Major</strong> <strong>Salivary</strong> <strong>Gland</strong> Imaging • 25
Figure 15. MR sialography in a healthy volunteer.The main submandibular duct (arrows)and some of its tributaries (arrowheads) can beseen on this transverse, maximum intensityprojection reformatted image from a threedimensional,T2-weighted fast SE (5,000/102,one signal acquired) data set.a. b.Figure 17. Simple ranula. (a) In the rightsublingual gland, the hyperintense lesion (arrow)on this transverse T2-weighted SE (3,000/102) MR image could represent a pleomorphicadenoma or a cyst. (b) The absence of enhancementon this fat-saturated, T1-weighted SE(600/17) MR image suggests a cystic lesion, inthis case a simple ranula of the sublingualgland. (c) The nonenhancing ranula (curvedarrow) lies superior to the geniohyoid muscles(g) and has not perforated through the mylohyoidmusculature on this coronal T1-weighted SE (600/17) MR image with fat saturation.Figure 16. Acute right-sided parotitis. Transverse,contrast-enhanced, fat-saturated, T1-weighted SE (600/30) MR image shows markedenhancement of the right parotid gland (thickand thin arrows) compared with the left. Thesuperficial subcutaneous tissue is also inflamed.lar collections peripherally in the glandularparenchyma (54). The larger ducts arespared as the disease affects the peripheryfirst and spares the central ductal system.Tiny abscesses in the glands will showsimilar punctate cystic regions.Sialography is contraindicated in theacute setting of sialadenitis because of thepossibility of exacerbating the symptomsassociated with the infection. The retrogradeinjection of contrast agents can forceinflammatory products into the more peripheralparenchyma of the gland. Furthermore,the act of instrumenting theduct may irritate it, cause narrowing fromposttraumatic edema or stricture formation,and lead to reduced drainage of theinfected saliva. MR sialography has theadvantage of not requiring cannulationof the duct and a heightened sensitivityto edema in the salivary gland, whichmay not be evident at CT.c.Can MR sialography replace conventionalsialography, a cumbersome procedurethat is contraindicated in patientswith acute sialadenitis and may result inirritation and injury to the duct if notperformed properly? The answer appearsto be yes, if not now then very soon (Fig15). The caveat is that the need to performsialography should be restrictedto a very few number of cases whenclinical assessment, serology (especiallyfor the autoimmune causes), conventionalradiography, and/or CT cannot facilitatediagnose of the cause of thechronic sialadenitis.Sialolithiasis often causes sialadenitis(44). The inflamed gland will be large andpainful, and the cardinal signs of warmthand redness may be present over the gland.Secondary involvement of the glands byodontogenic abscesses may also lead toinfection of the gland. Purulent materialmay be expressed from the ductal orificein most bacterial infections and is the bestclinical sign of an infected gland.Figure 18. HIV-related lesions. Transverse,contrast-enhanced CT scan depicts a rightsidedparotid cyst (straight arrow) and multiplesmall nodules in the left parotid gland (curvedarrow) in this patient who was HIV positive buthad not fulfilled criteria for acquired immunodeficiencysyndrome.Other causes of acute parotitis includeviral (mumps), bacterial (staphylococcusand streptococcus), granulomatous (tuberculosis,candida, cat-scratch fever), andpostpartum parotitis. Poor dental hygienemay contribute to the developmentof infections affecting the submandibular,sublingual, and parotid glands. Theminor salivary glands rarely show inflammatorychange other than mucous retentioncysts from local obstruction.If the patient is experiencing his or her26 • Radiology • July 2000 Yousem et al
Figure 19. Sjögren disease. While both parotidglands (arrowheads) show cystic changes inand enlargement of the gland on this coronalT2-weighted SE (4,000/80) MR image, the leftside also shows periparotid adenopathy (arrow).This pattern may be seen with Sjögrendisease or HIV-related lymphoepithelial cystsand nodules.Figure 20. Conventional sialography. The extentof the ductal system and its tributaries iswell seen on this conventional sialogram in apatient who has Sjögren disease. Note the tinyareas of cavitation (arrows) in the periphery.Figure 21. <strong>Gland</strong>ular calcifications in a patientwith sarcoidosis. Transverse nonenhancedCT scan shows the presence of multiple smallcalcifications in the parotid glands bilaterally.first episode of acute sialadenitis in thesetting of dehydration or a palpable sialolith,the otorhinolaryngologist may electto forego imaging and treat empirically.Surgeons are loath to operate in the settingof acute parotitis. Surgical planes areobliterated, and the dissection of the facialnerve is very cumbersome when thesurrounding gland is edematous and inflamed.Medical management is indicated.Even when an abscess is present,most head and neck surgeons prefer towait until antibiotics have reduced thediffuse inflammation in the gland beforetackling the focal mass.On CT or MR images, one may see theinflamed gland as enlarged, of abnormalattenuation or intensity, and enhancingavidly (Fig 16). There is usually inflammatorystranding into the overlying subcutaneoustissue and thickening of the investingdeep cervical fascia with acuteparotitis. This is seen equally well at MRimaging and CT. The gland will have highsignal intensity at T2-weighted MR imaging.The presence of adjacent lymphnodes or intraglandular lymph nodes maysuggest the inflammatory nature of thelesion but can also be seen, in anotherclinical setting, with neoplasms.CT and MR imaging in the coronalplane for inflammatory conditions of theparotid and submandibular glands maybe helpful for evaluating the extent of thelesion. The relationship of the inflammatorymass to the floor of the mouth (aswith a ranula) for submandibular lesionsand the skull base for parotid gland masseshas importance with respect to the surgicalapproach. A ranula has been termed amucous escape cyst, a mucous retentioncyst, and a mucocele of the sublingualgland or neighboring minor salivary glandulartissue (Fig 17). A ranula that issuperficial to the mylohyoid muscle (asimple ranula, epithelial lined) is usuallyaddressed transorally. It may be treatedwith resection or, in some cases, marsupialization.The lingual and hypoglossalnerves must be carefully identified duringthe operation. A ranula that plungesthrough the muscular floor (a plungingranula or pseudocyst, not epithelial lined)may be excised through a transcervicalsubmandibular incision with a neck dissection.This allows complete resection ofthe cyst and will help spare the lingualand hypoglossal nerve. Alternatively, thesurgeon may excise the sublingual glandtransorally and pack the cyst or place adrain in it. By treating the gland, somebelieve the plunging cyst will resolve onits own.Occasionally, one will identify an abscessin the gland that is associated withinfiltration of the subcutaneous tissueand/or the glandular tissue. As always,one should exclude a sialolith as thecause for the abscess on a nonenhancedCT scan, US scan, or conventional radiograph.Contrast-enhanced CT and MRimaging are currently the best ways todemonstrate a glandular abscess. Becauseof the fatty attenuation and intensitythat is intrinsic to the parotid glands,particularly as one ages, abscesses areparticularly well seen on enhanced CTscans and fat-saturated, T1-weighted MRimages. CT has been shown to be of benefitin evaluating the inflammatory masseswhen compared to MR imaging (55).One should include superinfected HIVrelatedcysts, suppurative parotid lymphnodes, and cystic degeneration of neoplasmswith or without superimposedinfection in the differential diagnosis ofabscesses of the gland.There are a number of manifestationsof chronic sialadenitis, both clinicallyand radiographically. Most important, thechanges from chronic sialolithiasis mayresult in a small atrophic gland with focalintraglandular calcifications. Rarely, onemay see a large ductal stone still remainingwith no evidence of acute inflammationand inducing no pain. This occursmost frequently in the submandibulargland.A mucous plug in the duct may alsocause a painful, swollen gland (Kussmauldisease). One pseudomass associated withcalcifications in the gland is termed the‘‘Kuttner tumor,’’ a focal, masslike firmnessof the submandibular gland due tochronic sialadenitis from sialolithiasis.SYSTEMIC DISORDERS OF THEMAJOR SALIVARY GLANDSIn the category of systemic disorders thataffect the major salivary glands, there area number of autoimmune diseases. HIVrelatedcysts and nodules (Fig 18), Sjögrentype 1 (previously known as Mikuliczdisease) and Sjögren type 2 (Fig 19), andsarcoidosis fall within the general rubricof autoimmune disorders with salivarygland manifestations (56). CT is probablythe best way to image patients with systemicdisorders since calculi may be at theroot of or a byproduct of the acute symptomsrelated to the systemic disorder.Sjögren syndrome and sarcoidosis predisposeto stone formation. The attenuationof the gland may be increased with bothSjögren disease and sarcoidosis. Focalmasses may be present with cysts, nodules,and lymph nodes in all of the diseaseslisted above.Sialography may be useful in stagingSjögren syndrome, since patients’ symptomsmay not correlate well with severityVolume 216 • Number 1 <strong>Major</strong> <strong>Salivary</strong> <strong>Gland</strong> Imaging • 27
of the disease (Fig 20). The results of aprospective study comparing MR sialography(6,000/115; flip angle, 60°; pixel size,0.29 0.31 3 mm) with the standard ofreference conventional sialography showedan agreement rate of 89% (P .001) instaging the disease (57). For identifyingstage I or greater disease and stage II orgreater disease, MR sialography was 100%and 91% accurate, respectively (57). Punctate,globular, and destructive patternsmay be discerned with MR sialography(58).In most cases, the diagnosis of Sjögrendisease is made clinically based on thesicca syndrome and the connective tissuedisorder (eg, rheumatoid arthritis) combinedwith serology of antinuclear antibodies.Sialography, be it MR or conventional,is used primarily to stage disease(see previous section). For those cases inwhich the diagnosis is in question, somewould favor performing a lip biopsy ofthe minor salivary gland tissue over sialography.Still others have suggested that abiopsy of the parotid gland has a higheryield than a labial biopsy since the sensitivityfor Sjögren disease with labial minorsalivary gland biopsy is 58% (21 of 36patients) compared to 100% (36 of 36patients) for parotid biopsy (59).Sjögren syndrome increases the risk ofparotid lymphoma by more than 4,400%(60). Therefore, any dominant mass in aSjögren-affected parotid gland must beconsidered lymphoma and requires aspirationor biopsy with assessment of cellularclonality. MR imaging has been particularlyhelpful with identifying dominantmasses within glands affected by Sjögrendisease (60).Som et al (39) have coined the term‘‘acquired immunodeficiency syndrome–related parotid cysts’’ to describe the cystsassociated with HIV infection and notethat they are hard to distinguish fromSjögren-related benign lymphoepitheliallesions. In patients who are HIV positive,one can see both cysts or lymphoid nodulesin the parotid glands. Complementaryfindings of cervical adenopathy,adenoidal hypertrophy, and tonsillar enlargementmay also be present (61).In addition to the autoimmune disordersin the preceding paragraphs, thesalivary glands may be affected by othersystemic disorders. Sialosis refers to abilateral, painless enlargement of the salivaryglands that may be caused by systemicdisorders such as diabetes mellitus,alcoholism, hypothyroidism, and malnutrition.Some medications may provokesialosis (including some antibiotics, diuretics,and psychotropic medications).The disorder is rarely imaged but usuallyshows enlarged parotid glands of increasedattenuation and slightly increasedT2 intensity.Granulomatous diseases, including fungalinfections, Wegener disease, tuberculosis,syphilis, and cat-scratch fever, mayproduce painless focal or generalizedmasses in the salivary glands. If there arecalcifications within a painless mass inthe parotid gland, granulomatous diseasesand pleomorphic adenoma becomethe most likely diagnoses. Sarcoidosis predisposesto glandular calcifications (Fig21) with or without nodes.Unusual disorders such as Kimura disease(eosinophilia, lymphoid proliferationin neck nodes and salivary glands,usually occurring in Asian patients), amyloidosis,toxoplasmosis, actinomycosis,and hematogenous metastases (usuallyfrom thyroid or renal cell carcinoma)rarely will affect the parotid gland.The clinical history will usually offerthe best means for establishing that theparotid gland is affected by systemic disorders.Imaging, if required, is used primarilyto assess an atypical dominant mass.In this scenario, MR imaging is probablythe most effective study.SUMMARYMost disorders of the salivary glands willmanifest a few discrete clinical scenarios.Because sialolithiasis may have a varietyof manifestations, CT should be the mainstayof imaging. Optimal imaging evaluationof the salivary glands may requirenonenhanced (to visualize sialoliths), enhanced(to identify abscesses, cysts, andneoplasms), or both nonenhanced andenhanced (for painful masses for whichone cannot exclude sialolithiasis) CTscans. On the other hand, with a subacutemanifestation of a nonpainful, noninflammatorymass, where there is a highdegree of suspicion for neoplasm, contrast-enhanced,fat-saturated MR imagingwill best demonstrate the extent of diseaseand the presence of perineural seeding.Sialography, if indicated at all, maybe performed with heavily T2-weightedMR techniques.Acknowledgment: The authors would like toacknowledge the kind support provided byLaurie A. Loevner, MD, in the analysis andcollection of the images and material presentedherein.References1. Weissman JL, Carrau RL. Anterior facialvein and submandibular gland together:predicting the histology of submandibularmasses with CT or MR imaging. Radiology1998; 208:441–446.2. Kane WJ, McCaffrey TV, Olsen KD, LewisJE. Primary parotid malignancies: a clinicaland pathologic review. Arch OtolaryngolHead Neck Surg 1991; 117:307–315.3. Batsakis JG. Tumors of the head and neck:clinical and pathological considerations.Baltimore, Md: Williams & Wilkins, 1979.4. Freling NJ, Molenaar WM, Vermey A, etal. Malignant parotid tumors: clinical useof MR imaging and histologic correlation.Radiology 1992; 185:691–696.5. Weber RS, Byers RM, Petit B, Wolf P, AngK, Luna M. Submandibular gland tumors:adverse histologic factors and therapeuticimplications. Arch Otolaryngol Head NeckSurg 1990; 116:1055–1060.6. Shah JP. Head and neck surgery. 2nd ed.London, United Kingdom: Mosby-Wolfe,1996; 431–460.7. Weber RS, Palmer JM, el-Naggar A, Mc-Neese MD, Guillamondegui OM, ByersRM. Minor salivary gland tumors of thelip and buccal mucosa. Laryngoscope1989; 99:6–9.8. Schlakman BN, Yousem DM. MR of intraparotidmasses. AJNR Am J Neuroradiol1993; 14:1173–1180.9. Parker GD, Harnsberger HR. Clinicalradiologicissues in perineural tumorspread of malignant diseases of the extracranialhead and neck. RadioGraphics1991; 11:383–399.10. Barakos JA, Dillon WP, Chew WM. Orbit,skull base, and pharynx: contrast-enhancedfat suppression MR imaging. Radiology1991; 179:191–198.11. Dillon WP. Imaging of central nervoussystem tumors. Curr Opin Radiol 1991;3:46–50.12. Teresi LM, Lufkin RB, Wortham DG, AbemayorE, Hanafee WN. Parotid masses:MR imaging. Radiology 1987; 163:405–409.13. Swartz JD, Rothman MI, Marlowe FI,Berger AS. MR imaging of parotid masslesions: attempts at histopathologic differentiation.J Comput Assist Tomogr 1989;13:789–796.14. Som PM, Biller HF. High-grade malignanciesof the parotid gland: identificationwith MR imaging. Radiology 1989; 173:823–826.15. Sigal R, Monnet O, de Baere T, et al.Adenoid cystic carcinoma of the head andneck: evaluation with MR imaging andclinical-pathologic correlation in 27 patients.Radiology 1992; 184:95–101.16. Kaneda T, Minami M, Ozawa K, et al.Imaging tumors of the minor salivaryglands. Oral Surg Oral Med Oral PatholOral Radiol Endod 1994; 78:385–390.17. Berg HM, Jacobs JB, Kaufman D, ReedeDL. Correlation of fine needle aspirationbiopsy and CT scanning of parotid masses.Laryngoscope 1986; 96:1357–1362.18. Som PM, Shugar JM, Sacher M, StollmanAL, Biller HF. Benign and malignant parotidpleomorphic adenomas: CT and MRstudies. J Comput Assist Tomogr 1988;12:65–69.19. Keyes JW Jr, Harkness BA, Greven KM,Williams DW, Watson NE Jr, McGuirt WF.<strong>Salivary</strong> gland tumors: pretherapy evaluationwith PET. Radiology 1994; 192:99–102.20. Kress E, Schulz HG, Neumann T. Diagno-28 • Radiology • July 2000 Yousem et al
sis of diseases of the large salivary glandsof the head by ultrasound, sialographyand CT-sialography: a comparison ofmethods. HNO 1993; 41:345–351. [German]21. Wittich GR, Scheible WF, Hajek PC. Ultrasonographyof the salivary glands. RadiolClin North Am 1985; 23:29–37.22. Gritzmann N. Sonography of the salivaryglands. AJR Am J Roentgenol 1989; 153:161–166.23. Schroeder HG, Schwerk WB, Eichhorn T.High-resolution real-time sonography insalivary gland diseases. II. <strong>Salivary</strong> glandtumors. HNO 1985; 33:511–516. [German]24. Martinoli C, Derchi LE, Solbiati L, RizzattoG, Silvestri E, Giannoni M. ColorDoppler sonography of salivary glands.AJR Am J Roentgenol 1994; 163:933–941.25. Yoshiura K, Miwa K, Yuasa K, et al. Ultrasonographictexture characterization ofsalivary and neck masses using twodimensionalgray-scale clustering. DentomaxillofacRadiol 1997; 26:332–336.26. Dailiana T, Chakeres D, Schmalbrock P,Williams P, Aletras A. High-resolution MRof the intraparotid facial nerve and parotidduct. AJNR Am J Neuroradiol 1997;18:165–172.27. Lufkin R, Teresi L, Wortham D, et al.Magnetic resonance imaging of the facialnerve: normal anatomy and pathology.Acta Radiol Suppl 1986; 369:212–214.28. Wortham DG, Teresi LM, Lufkin RB, HanafeeWN, Ward PH. Magnetic resonanceimaging of the facial nerve. OtolaryngolHead Neck Surg 1989; 101:295–301.29. McGhee RB Jr, Chakeres DW, SchmalbrockP, Brogan MA, Negulesco JA. Theextracranial facial nerve: high resolutionthree-dimensional Fourier transform MRimaging. AJNR Am J Neuroradiol 1993;14:465–472.30. Eracleous E, Kallis S, Tziakouri C, Blease S,Gourtsoyiannis N. Sonography, CT, CTsialography, MRI and MRI sialography ininvestigation of the facial nerve and thedifferentiation between deep and superficialparotid lesions. Neuroradiology 1997;39:506–511.31. Thibault F, Halimi P, Bely N, et al. Internalarchitecture of the parotid gland at MRimaging: facial nerve or ductal system?Radiology 1993; 188:701–705.32. Thibault F, Bonfils P, Halimi P, et al. Is thefacial nerve visible on magnetic resonanceimaging?. Ann Otolaryngol ChirCervicofac 1992; 109:365–368. [French]33. Ariyoshi Y, Shimahara M. Determiningwhether a parotid tumor is in the superficialor deep lobe using magnetic resonanceimaging. J Oral Maxillofac Surg1998; 56:23–27.34. Eisen MD, Yousem DM, Montone KT, etal. Use of preoperative MR to predictdural, perineural, and venous sinus invasionof skull base tumors. AJNR Am JNeuroradiol 1996; 17:1937–1945.35. Seaver PR Jr, Kuehn PG. Adenoid cysticcarcinoma of the salivary glands: a studyof ninety-three cases. Am J Surg 1979;137:449–455.36. Shugar JM, Som PM, Biller HF. Warthin’stumor, a multifocal disease. Ann OtolRhinol Laryngol 1982; 91:246–249.37. Silvers AR, Som PM. <strong>Salivary</strong> glands. RadiolClin North Am 1998; 36:941–966.38. Shugar JM, Som PM, Jacobson AL, RyanJR, Bernard PJ, Dickman SH. Multicentricparotid cysts and cervical adenopathy inAIDS patients: a newly recognized entity—CTand MR manifestations. Laryngoscope1988; 98:772–775.39. Som PM, Brandwein MS, Silvers A. Nodalinclusion cysts of the parotid gland andparapharyngeal space: a discussion of lymphoepithelial,AIDS-related parotid andbranchial cysts, cystic Warthin’s tumors,and cysts in Sjögren’s syndrome. Laryngoscope1995; 105:1122–1128.40. Vogl TJ, Dresel SH, Grevers G, et al.Sjoegren’s syndrome: MR imaging of theparotid gland. Eur Radiol 1996; 6:46–51.41. Som PM, Curtin HD. Head and neck imaging.3rd ed. St Louis, Mo: Mosby, 1996.42. Sack MJ, Weber RS, Weinstein GS, ChalianAA, Nissenbaum HL, Yousem DM. Imageguidedfine-needle aspiration of the headand neck: five years’ experience. ArchOtolaryngol Head Neck Surg 1998; 124:1155–1161.43. Yousem DM, Sack MJ, Weinstein GS, HaydenRE. Computed tomography–guided aspirationsof parapharyngeal and skull basemasses. Skull Base Surg 1995; 5:131–136.44. Levy DM, ReMine WH, Devine KD. <strong>Salivary</strong>gland calculi. JAMA 1962; 181:1115–1119.45. Laudenbach P. <strong>Salivary</strong> calculi. Rev Prat1992; 42:989–995. [French]46. Haring JI. Diagnosing salivary stones. JAm Dent Assoc 1991; 122:75–76.47. Antoniadis D, Mendonidou L, PapanayotouP, Trigonidis G. Clinical study ofsialolithiasis: findings from 100 cases. HellStomatol Chron 1989; 33:245–251.[Greek]48. Avrahami E, Englender M, Chen E,Shabtay D, Katz R, Harell M. CT of submandibulargland sialolithiasis. Neuroradiology1996; 38:287–290.49. Murray ME, Buckenham TM, Joseph AE.The role of ultrasound in screening patientsreferred for sialography: a possibleprotocol. Clin Otolaryngol Appl Science1996; 21:21–23.50. Yoshimura Y, Inoue Y, Odagawa T. Sonographicexamination of sialolithiasis. JOral Maxillofac Surg 1989; 47:907–912.51. Fischbach R, Kugel H, Ernst S, et al. MRsialography: initial experience using a T2-weighted fast SE sequence. J Comput AssistTomogr 1997; 21:826–830.52. Murakami R, Baba Y, Nishimura R, et al.MR sialography using half-Fourier acquisitionsingle-shot turbo spin-echo (HASTE)sequences. AJNR Am J Neuroradiol 1998;19:959–961.53. Lomas DJ, Carroll NR, Johnson G, AntounNM, Freer CE. MR sialography: work inprogress. Radiology 1996; 200:129–133.54. Som PM, Shugar JM, Train JS, Biller HF.Manifestations of parotid gland enlargement:radiographic, pathologic, and clinicalcorrelations. I. The autoimmune pseudosialectasias.Radiology 1981; 141:415–419.55. Casselman JW, Mancuso AA. <strong>Major</strong> salivarygland masses: comparison of MR imagingand CT. Radiology 1987; 165:183–189.56. Holliday RA, Cohen WA, Schinella RA, etal. Benign lymphoepithelial parotid cystsand hyperplastic cervical adenopathy inAIDS-risk patients: a new CT appearance.Radiology 1988; 168:439–441.57. Ohbayashi N, Yamada I, Yoshino N, SasakiT. Sjögren syndrome: comparison of assessmentswith MR sialography and conventionalsialography. Radiology 1998;209:683–688.58. Tonami H, Ogawa Y, Matoba M, et al. MRsialography in patients with Sjögren’s syndrome.AJNR Am J Neuroradiol 1998;19:1199–1203.59. Marx RE, Hartman KS, Rethman KV. Aprospective study comparing incisionallabial to incisional parotid biopsies in thedetection and confirmation of sarcoidosis,Sjögren’s disease, sialosis and lymphoma.J Rheumatol 1988; 15:621–629.60. Grevers G, Ihrler S, Vogl TJ, Weiss M. Acomparison of clinical, pathological andradiological findings with magnetic resonanceimaging studies of lymphomas inpatients with Sjögren’s syndrome. EurArch Otorhinolaryngol 1994; 251:214–217.61. Yousem DM, Loevner LA, Tobey JD, GeckleRJ, Bilker WB, Chalian AA. Adenoidalwidth and HIV factors. AJNR Am J Neuroradiol1997; 18:1721–1725.Volume 216 • Number 1 <strong>Major</strong> <strong>Salivary</strong> <strong>Gland</strong> Imaging • 29