John Ulatowski, MD, PhD - Roswell Park Cancer Institute
John Ulatowski, MD, PhD - Roswell Park Cancer Institute
John Ulatowski, MD, PhD - Roswell Park Cancer Institute
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
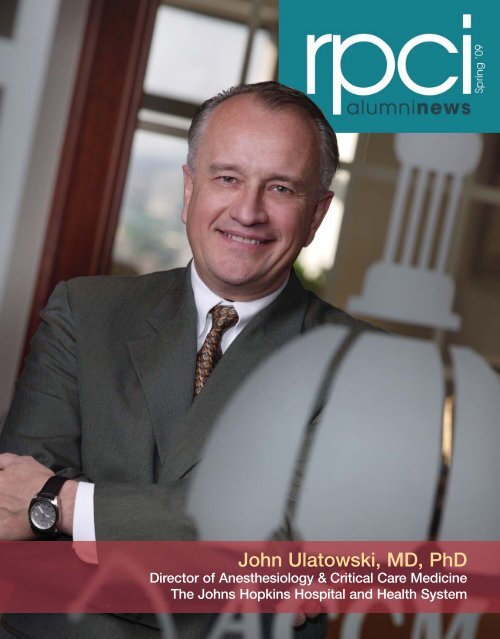
<strong>John</strong> <strong>Ulatowski</strong>, <strong>MD</strong>, <strong>PhD</strong>Director of Anesthesiology & Critical Care MedicineThe <strong>John</strong>s Hopkins Hospital and Health System
greetings from the parktable ofcontentsCREATIVE STAFFAs I pen this note, the snow outside my window rushes by in torrents of white. Hopefully,by the time you read this letter, the snows will have been replaced by warm spring rainsand the emergence of new life in the garden. So, too, is it at <strong>Roswell</strong> <strong>Park</strong>, where new lifeemerges in the form of new programs and new trainees. You'll read in this issue of newprograms and our continued efforts to recruit new trainees, of former trainees who havegone on to greater glory, and of new recruits with unlimited potential.Dr. <strong>John</strong> <strong>Ulatowski</strong>’s story highlights the role that RPCI played in the germination of hiscareer in translational research. Just as a gardener plants seeds in the spring, the <strong>Roswell</strong><strong>Park</strong> faculty works to germinate the seeds of curiosity within our trainees. <strong>John</strong> reminiscesabout these events, commencing with his humble beginnings in our master’s degreeprogram, where the seeds of research curiosity were sown, through his <strong>PhD</strong> program, wherehe became enamored with the idea of pursuing a career in translational research. His storyexemplifies what we do best at <strong>Roswell</strong> <strong>Park</strong>: training translational scientists. I look forwardto meeting more inspired and inspiring trainees like <strong>John</strong> in the years to come.Don't forget to do your part by recommending <strong>Roswell</strong> <strong>Park</strong> as a first choice for clinical andbasic scientific training…and keeping us informed of your professional and personalmilestones.6241014222324faculty interviewalumni spotlightrpci headlinersresearch & technologyit’s academicforum and functionclass notesManaging EditorColleen M. KaruzaSenior Copywriter & EditorSue BanchichCreative Services DirectorBenjamin RicheyGraphic Production ManagerHillary BanasPhotographyBill SheffBenjamin RicheyADMINISTRATIONPresident & CEODonald L. Trump, <strong>MD</strong>, FACPSenior Vice PresidentEducational AffairsDean, <strong>Roswell</strong> <strong>Park</strong> GraduateDivision, University at BuffaloArthur M. Michalek, <strong>PhD</strong>, FACEVice President Emeritus,Educational AffairsEdwin A. Mirand, <strong>PhD</strong>, DScVice President, Marketing,Planning & Public AffairsLaurel A. DiBrogArthur M. Michalek, <strong>PhD</strong>, FACESenior Vice President, Educational AffairsDean, <strong>Roswell</strong> <strong>Park</strong> Graduate Division, University at BuffaloextracurricularsVice President, DevelopmentCindy A. EllerPublished three times a year. All rights reserved. Noportion of this magazine may be reproduced withoutwritten permission. To receive a free subscription,please email Colleen.Karuza@roswellpark.org. Tolearn more about giving opportunities, please call theDevelopment Office at 716-845-4444.
FACULTY INTERVIEW: WILLIAM CANCE, <strong>MD</strong>, SURGEON-IN-CHIEFWhat attracted you to <strong>Roswell</strong> <strong>Park</strong>?<strong>Roswell</strong> <strong>Park</strong> is on a stellar trajectory across the board in oncology,and it offers the opportunity to do clinical work and to translatebasic research into clinical trials. I’m really excited about new typesof clinical trials, particularly with small-molecule inhibitors. We’reuniquely positioned at <strong>Roswell</strong> <strong>Park</strong> to be able to take thoseabilities into the clinic—and a lot of those new therapies will beless toxic, because they’re more selective.Dr. William G. CanceCAREER HIGHLIGHTS✯ <strong>MD</strong>, Duke University School of Medicine – 1982✯ Fellow of the American College of Surgeons“There’s suchpride in, andsuch a love of,<strong>Roswell</strong> <strong>Park</strong> inthe community.It’s a terrificplace to be.facultyinterview:William Cance, <strong>MD</strong>“FFrom the time he was a fourth-grader, William Cance knew he wanted to be asurgeon. In high school, he found a mentor in surgical oncologist Dr. WarrenCole, Past President of the American <strong>Cancer</strong> Society. Dr. Cance’s decision tospecialize in surgical oncology intensified after his roommate at Duke Universitydied of sarcoma. “I saw firsthand the devastation of cancer,” he reflects.Recently appointed Chair of Surgical Oncology and Surgeon-in-Chief at <strong>Roswell</strong><strong>Park</strong>, Dr. Cance directs the Department of Surgical Oncology, oversees operatingroom and surgical services, and serves as principal investigator of a surgicaloncology training grant. He served previously as Chair of the Department ofSurgery and Associate Director of Shands <strong>Cancer</strong> Center at the University ofFlorida. Here he answers questions about his hopes for <strong>Roswell</strong> <strong>Park</strong>.I am also developing a natural collaboration with Dr. AndreiGudkov [The Garman Family Chair in Cell Stress Biology andSenior Vice President of Basic Science]. He was kind enough to letme locate my lab next to his and has kindly shared his resourceswith our group. He’s one of the most brilliant people I’ve ever met.How do you foresee the medical communitycoping with the ongoing shortage ofphysicians, including surgeons?The shortage of surgeons is already being felt in rural areas, and itwill be felt all over as Baby Boomers retire and the need increases.Not enough surgeons are being trained; there are nowhere nearenough surgical oncologists to do all the cancer surgery in thecountry, so most cancer surgery will continue to be done bygeneral surgeons who were trained during their residency.This has increased the importance of <strong>Roswell</strong> <strong>Park</strong>’s educationalmission. The leaders in surgical oncology will be fellowship-trainedsurgical oncologists, who will lead the other surgeons who will bedoing cancer surgery. We have a tremendous fellowship programat <strong>Roswell</strong> <strong>Park</strong>, led by Dr. Stephen Edge, that provides thisspecial expertise in surgical oncology. We have great faculty insurgery; for example, Dr. <strong>John</strong> Kane is on the training committeeof the Society of Surgical Oncology. So we have the traininginfrastructure—and as we train fellows, we will be recruiting someof them to join us at <strong>Roswell</strong> <strong>Park</strong>.You brought several colleagues to<strong>Roswell</strong> <strong>Park</strong> with you. Please give anexample of their potential contributionsto the <strong>Institute</strong>’s mission.Drs. Vita Golubovskaya and Elena Kurenova are AssociateProfessors of Oncology and will be the nucleus of our lab efforts.Both are accomplished scientists with expertise in cell andmolecular biology. They will be leaders of our departmentaltranslational research efforts.✯ President, Society of Surgical Oncology✯ Clinical Interests: surgical oncology, endocrine surgery✯ Research Interest: the biology of focal adhesionkinase (FAK), which plays a key role in protectingcancer cells from programmed death (apoptosis)✯ Chief Fellow, Surgical Oncology, MemorialSloan-Kettering <strong>Cancer</strong> Center, 1989-90✯ Hector MacLean Distinguished Professor of <strong>Cancer</strong>Research, University of North Carolina LinebergerComprehensive <strong>Cancer</strong> Center – 2002Dr. Sergei Kurenov is an engineer who did simulation for theMIG-29 aircraft in the former Soviet Union. Now he does surgicalsimulations. He’s bringing with him a postdoctoral computerprogrammer, and they will collaborate with Dr. James Mohler,Dr. Khurshid Guru and members of <strong>Roswell</strong> <strong>Park</strong>’s robotic surgerysimulation group to make it even stronger. Dr. Kurenov will alsobe working with the minimally invasive surgery program, whichDr. Mohler has done a great job of getting off the ground.What are your principal goals as youassume your new role?I look forward to coordinating and enhancing <strong>Roswell</strong> <strong>Park</strong>’s surgicalservices and translational research efforts across all the disciplines.Surgery remains a mainstay of oncologic practice, and we need tocontinue to keep abreast of advances in surgery, patient safety andpatient outcomes. I’m also anxious to strengthen our academicmission through clinical trials while delivering the highest-qualitycancer care.There’s such pride in, and such a love of, <strong>Roswell</strong> <strong>Park</strong> in thecommunity. It’s a terrific place to be.2| facultyinterview3
<strong>John</strong> <strong>Ulatowski</strong>’sFantastic VoyageR<strong>Roswell</strong> <strong>Park</strong> <strong>Cancer</strong> <strong>Institute</strong> was the launching point for<strong>John</strong> <strong>Ulatowski</strong>’s first voyage into the bloodstream.From those early days of graduate school when heexplored the development of blood cells, he journeyedon into anesthesiology and neurology. Along the way,he earned worldwide recognition for advancing ourunderstanding of the physiological processes that affectrecovery after a stroke or brain injury. Today Dr. <strong>Ulatowski</strong>is Director of Anesthesiology and Critical Care Medicine(ACCM) of The <strong>John</strong>s Hopkins Medical Institutions,overseeing a department with 115 faculty, 75 residents,and 24 CRNAs, who serve more than 70 anesthetizinglocations in two major hospitals and surgicenters every day.When he came to <strong>Roswell</strong> <strong>Park</strong> in 1975 to earn a master’sdegree in natural sciences, he planned to apply to medicalschool the following year. “But my experience at <strong>Roswell</strong><strong>Park</strong> was extremely stimulating, and convinced me that acareer in research would be as rewarding as a career inmedicine,” he says, “so I stayed for a <strong>PhD</strong> in cellphysiology.”That decision led to two important connections, first withMichael McGarry, <strong>PhD</strong>—then Director of the Departmentof Laboratory Animal Resources, now Vice President ofPreclinical Studies at Medelis. Dr. McGarry “had aninterest in experimental hematology, particularly in thePhoto courtesy The <strong>John</strong>s Hopkins Medical Institutionsimmune response as it pertained to the development of ablood cell called the eosinophil,” recalls Dr. <strong>Ulatowski</strong>.His working relationship with Dr. McGarry, coupled with his experiences as a part-time labtechnician in Buffalo General Hospital’s hematology laboratory, “got me interested instudying how blood cells develop.”The second connection, with James Zucali, <strong>PhD</strong>, his thesis advisor, led him to reconsider acareer in medicine. Dr. Zucali, he says, “saw the value of having an <strong>MD</strong> in addition to being abasic science researcher, for ease of translational work—taking science from the bench to thebedside.”Heeding Dr. Zucali’s advice, Dr. <strong>Ulatowski</strong> completed medical school at the University at Buffalo,setting his sights on a relatively unexplored area of inquiry—the brain. “I found that verychallenging,” he explains, “so I trained as a neurologist at the University of Maryland.“I was then attracted to <strong>John</strong>s Hopkins by an opportunity to train asan intensive-care physician focused on brain injury and spinal cordinjury. <strong>John</strong>s Hopkins had a nationally leading program in that area,and it was administered through the Department of Anesthesiology.”At the suggestion of Dr. Mark Rogers, then department chair,Dr. <strong>Ulatowski</strong> pursued a second fellowship in anesthesiology.The fusion of neurology and anesthesiology has given him an unusualperspective in addressing yet-unanswered questions about the brain:“How do we preserve brain under stressful conditions, such as whena patient undergoes anesthesia or has a direct trauma to the body?We are finding that there are many secondary effects of generalizedinjury to the body that affect brain function, and that’s an extremelyimportant area of research.“Now I’m studying the endpoint of what a red cell produces—hemoglobin—in a state that is free to float in the bloodstream.I’m excited about the possibility that those kinds of plasma-based,oxygen-carrying compounds might be able to deliver oxygen toischemic or injured brain better than blood cells themselves, becausemany times a fluid-based protein can get through the small channelsof the bloodstream to critical areas of the brain better than bloodcells themselves can.”It’s interesting, he reflects, that many of the questions he seeks toanswer today, 30 years after graduate school, have led him toconcentrate once again on the development of red blood cells—thevery work that first commanded his attention at <strong>Roswell</strong> <strong>Park</strong>.In the hot seatDr. <strong>Ulatowski</strong> answers questions about the challengesof modern medicine and the keys to success.How can the United States cope with theongoing critical shortage ofanesthesiologists?Given the demands of the healthcare system now and in the future,I think it’s wise to create a healthcare workforce matrix to meetdemand. The anesthesiologist should be at the top of the informationpyramid. However, nowadays we’re working more and more withmid-level providers, such as nurse-anesthetists and anesthesiologistassistants. The way to counteract the shortage of anesthesia providersis to consider, in some way or another, training all three.Will we see more physicians earning both an<strong>MD</strong> and a <strong>PhD</strong> to narrow the gap betweenbasic and clinical research?It’s extremely difficult for someone to study in the basic sciences andthen progress through clinical medicine to obtain an <strong>MD</strong> whilestaying fresh and competitive. Only a few people who do that canremain at the top of their field.I think a better model for the future is to have a combination ofdedicated basic scientists and clinician-scientists who work closelytogether in the translational, bench-to-bedside component. Thatmakes much more sense for the future, by allowing individuals tofocus their time and expertise on one element of the healthcareparadigm that ultimately brings new discovery to the clinical forefront.The key element is to have professionals who communicate andwork together in a community of scientists rather than having thoseindividuals represented in one person.What laid the foundation for yourprofessional achievement?The tremendous dedication of those who allowed me the opportunityto do this, starting with my parents, and then all the individuals whohave been my mentors throughout my career. And being affiliated inmy career with organizations that allowed me to grow. My success isreally the success of institutions that focus on developing people totheir fullest. <strong>Roswell</strong> <strong>Park</strong> and <strong>John</strong>s Hopkins have been two of those.4| alumnispotlight5
Faculty NotesFaculty Notes❶❷ ❸ ❹ ❺ ❻ ❼ ❽ ❾10❶ Anubha Bharthuar, <strong>MD</strong>, Clinical Fellow, Department of Medicine,discussed “Quality of Life in Patients with Advanced Pancreatic<strong>Cancer</strong> Receiving Gemcitabine, Capecitabine, and Bevacizumab:Results from a Prospective Multicenter Phase II Trial,” at the FifthAnnual Meeting of the International Society of GastrointestinalOncology, held in Virginia.❷ Shousong Cao, <strong>MD</strong>, <strong>Cancer</strong> Biology, has been appointed a VisitingProfessor at Forth Military Medical University in Xi’an, ShaanxiProvince, China, and has also been named to the editorial board ofThe Open Colorectal <strong>Cancer</strong> Journal, published by Bentham SciencePublishers, Ltd.❸ K. Michael Cummings, <strong>PhD</strong>, Chair of the Department of HealthBehavior, was recognized in March 2009 as a leader in globaltobacco control when he received the American <strong>Cancer</strong> Society’sLuther L. Terry Award for Outstanding Research at the 14th WorldConference on Tobacco and Health in Mumbai, India. The Award isnamed for the late U.S. Surgeon General who led the landmark 1964Surgeon General’s Report connecting tobacco use to lung cancerand other illnesses.❹Luqman Dad, <strong>MD</strong>, Radiation Medicine, is one of three people whowere elected recently to two-year terms on the Executive Committeeof the Association of Residents in Radiation Oncology (ARRO). ARROis the resident organization within ASTRO, the American Society forRadiation Oncology, and represents nearly 600 radiation oncologyresidents in the U.S.❺ Michelle Detwiler, MS, Project Coordinator, Cell Stress Biology, hasbeen elected President of the Association of Biomolecular ResourceFacilities, an organization with a membership of more than 1,000scientists.❻Kelli Bullard Dunn, <strong>MD</strong>, FACS, FASCRS, Department of Surgery,has been awarded the Victor W. Fazio, <strong>MD</strong>, MS, Award for EditorialExcellence by the editors of Diseases of the Colon & Rectum.Editor-in-Chief Robert Madoff, <strong>MD</strong>, commended Dr. Bullard Dunnfor “her astute clinical acumen, scientific expertise and superbeditorial judgment.”❼ Theresa Hahn, <strong>PhD</strong>, Assistant Member, Department of Medicine,presented “Clinical and Genetic Factors Underlying Acute BoneMineral Density Loss by 100 Days after Blood and MarrowTransplantation: A Potential Early Regimen-Related Complication,”for a session on Clinical Transplantation – Transplantation Regimen,at the 2008 annual meeting of the American Society of Hematology,held in December in San Francisco.❽Wen Wee Ma, MBBS, Assistant Professor of Oncology, was quotedrecently in HemOnc Today about lack of progress in the treatmentof pancreatic cancer. He pointed out that since the approval ofgemcitabine a decade ago, “the field has been trying to meshdifferent combinations [of drugs] with gemcitabine. The most recentresults presented by Kindler and colleagues at 2008 ASCO showedthat gemcitabine and bevacizumab with erlotinib or cetuximabdoesn’t have sufficient activity in advanced diseases.” Dr. Ma addedthat he sees a need for greater attention to the potential ofindividualized therapies.❾Enrico Mihich, <strong>MD</strong>, Distinguished Member of <strong>Roswell</strong> <strong>Park</strong>’sDepartment of Pharmacology and Therapeutics, has been nameda Fellow of the American Association for Advancement of Science.A member of the <strong>Roswell</strong> <strong>Park</strong> faculty since 1957, Dr. Mihich is anationally recognized expert in the development of therapeutics,Past President of the American Association of <strong>Cancer</strong> Researchand a member of the US National <strong>Cancer</strong> Advisory Board.10 Kena Miller, RN, MSN, FNP, Department of Medicine, discussed“An Update on Myeloma: The Latest in Research and Treatment,”a Continuing Education program for community practice nurses,presented in November 2008 by the Leukemia and LymphomaSociety. She is also a co-author of “Management of Side Effects ofNovel Therapies for Multiple Myeloma: Consensus StatementsDeveloped by the International Myeloma Foundation’s NurseLeadership Board,” published in the Clinical Journal of OncologyNursing, Supplement to Vol. 12, No. 3.Renal function may be compromised in some patients as a result of radiation treatment to the abdomen—butthe effects may not be noticed until a year or more after the end of radiotherapy (RT), according to a study ledby 11 Gary Yang, <strong>MD</strong>, Associate Professor of Radiation Medicine. Dr. Yang and his team tracked 129 patientswho underwent 3D conformal radiation therapy for GI cancers, finding that some experienced renal decline ayear or more after the end of RT. The results of their study, presented at the annual meeting of the AmericanSociety for Therapeutic Radiology and Oncology, represent the first quantification of the effects of RT on kidneyfunction, and underscore the need for longer patient monitoring after RT has ended. Investigators whocontributed to the study include Kilian Salerno May, <strong>MD</strong>, Radiation Medicine; Rameela Chandrasekhar,Biostatistics; Leayn Flaherty, RPA-C, Radiation Medicine; Richard Russo, C<strong>MD</strong>, RTT, Radiation Medicine; andGregory Wilding, <strong>PhD</strong>, Assistant Chair, Biostatistics.Pili heads GU SectionNationally recognized medical oncologist Roberto Pili, <strong>MD</strong>, has beenappointed Professor of Oncology, Chief of the Genitourinary Section andCo-Leader of the Genitourinary Program. He comes to RPCI from The SidneyKimmel Comprehensive <strong>Cancer</strong> Center at <strong>John</strong>s Hopkins University, where heserved as Associate Professor of Oncology and Urology.Nobel Laureate Roger Tsien topresent Dave Lecture at RPCIRoger Tsien, <strong>PhD</strong>, winner of the 2008 Nobel Prizein Chemistry, will present the annual Dave MemorialLecture at RPCI, Thursday, April 23, 2009, at 9 amin the Hohn Lecture Hall of the Research StudiesCenter. He will discuss “Optical and MR Imaging ofTumors In Vivo with Activatable Cell-PenetratingPeptides.” Dr. Tsien is an investigator with theHoward Hughes Medical <strong>Institute</strong>, Professor ofPharmacology at the University of California at SanDiego School of Medicine, and Professor ofChemistry and Biochemistry at the University ofCalifornia at San Diego.Established to honor the late Chandrakant V. Dave,<strong>PhD</strong>, who served on the Pharmacology facultyat RPCI, the Dave Lecture Series is organized bygraduate students of the Molecular Pharmacologyand <strong>Cancer</strong> Therapeutics Department.116| rpciheadliners7
RPCI: Industry Leaderin Buffalo NiagaraThe Buffalo Niagara Partnership (BNP) has recognized RPCI as an innovative leader inthe region’s life sciences industry. Donald Trump, <strong>MD</strong>, RPCI’s President & CEO, acceptedthe INNOVATE Buffalo Niagara Award for Life Sciences on behalf of the <strong>Institute</strong> at aluncheon held Jan. 28, 2009. Among other achievements, the BNP cited RPCI’s role as“a source of important new products and processes for use in the fight against cancer.”The awards singled out Buffalo Niagara’s “most groundbreaking and inventivecompanies” in five industry sectors: advanced manufacturing, agribusiness/foodprocessing, professional services, life sciences and logistics. Twenty-one finalists werechosen from among 60 companies nominated.There’s No Stopping BuffaloasPowerful MedicineMusic is powerful medicine for Marc Murray, a 25-year-old patient whocame to RPCI for a bone marrow transplant after a diagnosis of acutemyeloid leukemia. During his long recovery, he connected with StuartFuchs, a multi-talented musician, member of the gypsy jazz bandBabik, and an artist-in-residence at RPCI, and the two began playingguitar together during informal jam sessions in the hospital.It was a time of rediscovery for Mr. Murray, who had once playedguitar regularly before “letting it lapse” several years ago. Mr. Fuchsinspired him to pick it up again, and it has been both physically andspiritually therapeutic. “Some of the medicines I’m on cause shakingin my hands, and playing the guitar helps with that,” Mr. Murray says.“As a result of the chemotherapy, my hands peeled, and I lost all thecalluses I’d built up on my fingertips, so Stuart helped me with someexercises to build them up.“The guitar is soothing,” he adds, “and there’s music for every kindof emotion. You can play whatever you feel.”8Christine Sable is a powerful spokesman for RPCI’s new fundraising campaign,NEVER STOP BUFFALO. After receiving a diagnosis of advanced-stage ovariancancer, the Lancaster, PA, resident enrolled in a clinical trial of a new ovarian cancervaccine developed by Kunle Odunsi, <strong>MD</strong>, <strong>PhD</strong>, Surgeon in Gynecologic Oncologyand Co-Leader of the Tumor Immunology and Immunotherapy Program at RPCI.Community donations to RPCI were critical for initial research on the vaccine.In Ms. Sable’s case, the vaccine was administered after conventional chemotherapy,and it quickly improved her immune system’s ability to fight off recurrence of thedisease. Five years later, she’s still cancer-free and has experienced no side effects.“<strong>Roswell</strong> <strong>Park</strong> is such an incredible place,” she says. “It has given so many peoplehope, and given them their lives back.”Funding from NEVER STOP BUFFALO and similar campaigns will help fast-track thedevelopment of other new treatments at RPCI. Dollars raised by the campaign will beawarded competitively in the form of grants to fund research proposals submitted byRPCI physicians and scientists to the <strong>Institute</strong>’s Research Advisory Committee. Grantswill be awarded to projects showing the greatest potential to improve cancerprevention, diagnosis and care.“Christine Sable is just one of thousands of patients who arrive at <strong>Roswell</strong> <strong>Park</strong> eachyear looking for lifesaving treatments for the hundreds of cancers we treat,” saysDonald Trump, <strong>MD</strong>, FACP, President & CEO. “Now, more than ever, we need ourcommunity’s continued support. We will never stop searching, never stop healing,and never stop fighting until cancer is defeated.”To learn more, or to donate to NEVER STOP BUFFALO, call 716-845-4444, or makea secure online gift at www.neverstopbuffalo.com.That’s the underlying principle of the new Arts in Healthcare initiativeof the University at Buffalo’s Center for the Arts. Launched in the fall of2008, the program places artists at RPCI and Women’s and Children’sHospital of Buffalo so they can share their talents with patients andvisitors. In addition to Mr. Fuchs, RPCI’s team includes visual artistsAnn Frank, Barbara Murak and Pragna Hathi Wood; actor/storytellerJoy Scime; and dancer Sheila Dollas. Their work is funded by The<strong>John</strong> R. Oishei Foundation and gifts to the <strong>Roswell</strong> <strong>Park</strong> AllianceFoundation.Margarita Coyne, RN, BSN, Director of Patient Services, helped getthe program off the ground. She says interacting with artists providespatients with a welcome distraction, facilitating communication andreminding patients and families that “there are other things going onin life.” And studies show that cancer patients who participate in artactivities in a hospital setting report feeling less bored, sad andanxious.Debra Miga, Assistant Coordinator of Volunteer Services, notes thatpatients who have heard about the artists-in-residence program arestarting to request that the artists visit them in their rooms or specificclinics. That’s no surprise to Mr. Fuchs, who helps them explore theiremotions through many styles of music, from the tunes he plays on a10-stringed Andean churango to the deep tones he creates with anAustralian didgeridoo.Creating art or music gives patients “control over their immediateenvironment, even if just for a little while,” says Mr. Fuchs. “There is areal magic that happens when patients engage in the creativeprocess. They enter the present moment, which allows them to puttheir troubles aside while they express themselves creatively. Theactivity becomes a reflective healing process, a mirror into their soul.”Marc Murray (left) with Artist-in-Residence Stuart FuchsThe Arts Council in Buffalo & Erie County has honored RPCIPresident & CEO Donald Trump, <strong>MD</strong>, FACP, as a Trailblazerfor his contributions as “a pioneer, legacy makerand innovator in the Western New Yorkarts and cultural community.” He shared theaward in the Artist and Healthcare Initiative category withCheryl Klass, President of Women & Children’s Hospital ofBuffalo. Both institutions are partners in the Arts in HealthcareInitiative of the University at Buffalo’s Center for the Arts,which takes local artists into the healthcare setting to engagepatients in music, drama, and the visual arts.The awards were presented at the 23rd Annual Arts AwardProgram, held March 20, 2009. Other Trailblazer honoreesincluded Angelo Fatta, <strong>PhD</strong> (Philanthropist/Patron of theArts), Michael Morgulis (Artist/Entrepreneur), and Artpark &George Osborne (Programming and Leadership).| rpciheadliners feature | 9
Adjei leads NSCLC trialpdtLet There Be Light!PDT Center Receives Federal Funding in Excess of $10 MillionAlex A. Adjei, <strong>MD</strong>, <strong>PhD</strong>, Senior Vice President ofClinical Research and the Katherine Anne Gioia Chair in<strong>Cancer</strong> Medicine, is chairing a newly launched nationalclinical trial that is the first ever to focus on whetherbiomarkers can help guide therapies for lung cancer.The large National <strong>Cancer</strong> <strong>Institute</strong> (NCI) trial for nonsmallcell lung cancer, called MARVEL (MarkerValidation for Erlotinib in Lung <strong>Cancer</strong>), seeks tovalidate whether a biomarker can predict clinicalbenefit in the disease. It will establish whether abiomarker can identify a target, epidermal growthfactor receptor (EGFR), and the effectiveness of drugsin blocking the target, thus re-defining treatmentoptions for lung cancer patients.NCI Director <strong>John</strong> Niederhuber, <strong>MD</strong>, says MARVEL is“of major importance, because it could define, basedon a single test, the best therapy for this disease.”Approximately 1,200 lung cancer patients will be testedfor a high copy number of the EGFR gene byFluorescent in Situ Hybridization (FISH) status of themarker and will be randomized based on the outcomeof the test. After receiving initial standardchemotherapy, patients who are both EGFR-positiveand EGFR-negative will receive either erlotinib orpemetrexed, two approved treatments for advancedlung cancer. The study will help understand themechanisms of the drugs and identify patients who willbenefit most from these targeted therapies.Alex Adjei, <strong>MD</strong>, <strong>PhD</strong> with Sarah Burke, RN, MSN, Clinical Research Nurse“The MARVEL trial is the result of collaboration among several nationalhealthcare organizations, including the U.S. Food & Drug Administration,NCI cooperative groups, the biomarker industry and the pharmaceuticalindustry,” notes Dr. Adjei. “All are focused on the goal of providing new,Marker Validation for Erlotinib in Lung <strong>Cancer</strong> more effective treatments for lung cancer patients.”A five-year, $10.2 million grant from theNational <strong>Cancer</strong> <strong>Institute</strong> (NCI) will helpRPCI continue its pioneering studies inphotodynamic therapy (PDT). The <strong>Institute</strong>is known worldwide for the development ofPDT, which uses red laser light to trigger aphotosensitizing drug that collects in tumorcells. When activated by the laser, the drugkills the cancer cells. RPCI has receiveduninterrupted NCI funding for its PDTprogram since 1992—a remarkableachievement.Led by principal investigator BarbaraHenderson, <strong>PhD</strong>, Professor of Oncologyand Director of the PDT Center, Departmentof Cell Stress Biology, the program projectgrant explores mechanisms and strategiesfor making PDT more effective in treatingcancer. The program consists of fiveprojects, supported by four technical,statistical and administrative core units:Ravindra Pandey, <strong>PhD</strong>, DistinguishedMember, PDT Center, will continue his workin developing novel agents for optimizationof PDT and tumor imaging.Heinz Baumann, <strong>PhD</strong>,Professor of Oncology,Department ofMolecular and CellularBiology, will exploremolecular pathwaysfor optimizing PDT.Sandra Gollnick, <strong>PhD</strong>, Professor ofOncology, PDT Center, will examinehow PDT can affect mechanisms oftumor immunologyNathalie Zeitouni, <strong>MD</strong>, Interim Chair,Department of Dermatology, willinvestigate mechanisms of PDT inpatients being treated for skin cancer.“<strong>Roswell</strong> <strong>Park</strong> has a long-standing benchto-bedsideapproach to PDT that facilitatesan understanding of the underlyingmechanisms of the process while translatingthat knowledge into novel treatments,”says Dr. Henderson.Adds Donald Trump, <strong>MD</strong>, FACP,President & CEO of RPCI, “The verypositive review and awarding of fundingfor this program are a testament to theoutstanding science conducted at <strong>Roswell</strong><strong>Park</strong>. NCI program project grants are highlysought by cancer centers. Receipt of thisNCI grant demonstrates the cutting-edgescience in this pioneering <strong>Roswell</strong> <strong>Park</strong>research program. The grant continuessupport of a broad-based, multidisciplinaryteam approach to PDT cancer researchand discovery at RPCI.”It’s estimated that 215,020 people will be diagnosed with lung cancer thisyear, and 161,850 will die of the disease, making lung cancer the numberonecancer killer. Non-small cell lung cancer comprises about 85-90% ofall lung cancers diagnosed.Read more about the trial on the NCI website, atwww.cancer.gov/newscenter/pressreleases/MARVELrelease.Nestor Rigual, <strong>MD</strong>, Associate Professorof Oncology and Attending Surgeon,Department of Head & Neck Surgery,and Merrill Biel, <strong>MD</strong>, Clinical AssociateProfessor, University of Minnesota, willconduct clinical trials using PDT for thetreatment of early-stage cancers of thehead and neck.10 | researchandtechnology 11
Robotics“Patients have indicated that the overallquality of their life after cancer surgery isas important as how long they survive.”12Mounting a First-LineDefense Against InfectionsBrahm Segal, <strong>MD</strong>, right, with graduate students David Lewandowski and Nicole Rall| researchandtechnologyT“Inflammation helps the bodydefend against infections, suchas bacteria, viruses and fungi.”he National <strong>Institute</strong> of Allergy and Infectious Diseases (NIAID) has awarded a five-year,$2,176,043 research grant to RPCI to examine mechanisms of acute inflammation. BrahmSegal, <strong>MD</strong>, Chief of Infectious Diseases, is the principal investigator.“Inflammation helps the body defend against infections, such as bacteria, viruses and fungi,”explains Dr. Segal. “Just as it is important to stimulate inflammation to control infections,it is also necessary to turn off the inflammatory response to avoid tissue injury and allergy.Excessive inflammation is associated with a broad range ofdiseases, including cancer, diabetes and autoimmune diseases.”Dr. Segal and colleagues from Vanderbilt University MedicalCenter will analyze NADPH oxidase (nicotinamide adeninedinucleotide phosphate-oxidase), an enzyme complex thathelps defend against infections. The study is expected to offernew insights into chronic granulomatous disease (CGD), a rare inherited disorder of theNADPH oxidase that is characterized by recurrent infections and inflammatory complications.“Future studies supported by this grant will help us understand how NADPH oxidase controlsinflammation,” says Dr. Segal. “Knowledge gained about how the body regulates inflammationmay help us understand disorders of inflammation and develop better treatments.”PioneeringRoboticSurgeryAdds Lifeto YearsKhurshid Guru, <strong>MD</strong>Bladder cancer patients treated with state-of-the-art robot-assisted surgery at RPCIreport that their quality of life returned to normal within six months, according to astudy conducted by Khurshid Guru, <strong>MD</strong>, Director of Robotic Surgery. The study waspublished in the British Journal of Urology International.Pioneered at RPCI, robot-assisted cystectomy provides patients with a less-invasivetreatment option that has several potential advantages over traditional open surgery,including less postoperative pain and fewer days in the hospital. The prospective studyis the first to examine the quality-of-life benefits of the surgical technique.“Patients have indicated that the overall quality of their life after cancer surgery is asimportant as how long they survive,” says Dr. Guru. “This study helps us understand thepatient’s physical, social, emotional and functional well-being after surgery.”Quality of life was examined using the Functional Assessment of <strong>Cancer</strong> Therapyquestionnaire with 34 patients who underwent robot-assisted surgery between January2006 and December 2007. Patients were monitored according to National Comprehensive<strong>Cancer</strong> Center guidelines. The average age of the patients was 65 years; 88% were men.Of all patients, 13% received chemotherapy after surgery. Quality-of-life issues wereassessed at 1-, 3- and 6-month intervals.The study found that physical well-being had decreased significantly by the first follow-upvisit, due to the immediate impact of surgery. However, six months later, patients reportedthat their physical activities were comparable with their pre-surgery activities. Emotionalscores were statistically higher after surgery, indicating that feelings of sadness andanxiety appeared to be alleviated by the minimally invasive surgery and rapid recovery.Scores for social and family support remained uniformly high.Says Dr. Guru, “Robot-assisted surgery continues to demonstrate its efficacy as atreatment for bladder cancer patients and has now shown its value to patients as theyreturn to life after cancer.”13
Reinventing thepostdoc experienceA FAQ page will provide community informationfor out-of-towners. Dr. Kisailus notes that manypostdocs are married and have children, “sothey have to think about housing, daycare andschool systems.” The website will serve doubleduty as a bulletin board to identify and connectwith peers who share interests, and to showcaseachievements for prospective employers.RPCI’s postdoctoral scholars “have their fingers on the pulse ofwhat’s going on in science,” observes Adam Kisailus, <strong>PhD</strong>.“They’re on top of the literature, they have fresh ideas and afresh outlook, and they bring enthusiasm and energy into theclassroom. We rely on them for our scientific research, but at manyuniversities, they’re almost invisible.”Today RPCI’s Division of Educational Affairs is focusing more sharplyon their needs and interests with a plan informed largely by Dr.Kisailus’ own postdoctoral experience. After earning a <strong>PhD</strong> inmolecular biology from Georgetown University, he came to RPCI toinvestigate focal adhesion kinase activity in the lab of Irwin Gelman,<strong>PhD</strong>, now Interim Chair of <strong>Cancer</strong> Genetics. Dr. Kisailus says he andhis fellow postdocs “found there were things we wanted to do as acommunity.” The timing was good, too! Arthur Michalek, <strong>PhD</strong>,Dean and Senior Vice President of Educational Affairs, and Craig<strong>John</strong>son, Director of Graduate Admissions and Summer ResearchPrograms, had just determined that there was a need for greaterpostdoc support. Dr. Kisailus’ interest led to his appointment lastsummer as Assistant Dean.The new initiative will provide RPCI’s postdocs with more training insuch areas as grant writing, ethics, teaching, and career paths, tosupplement the strong research training they receive from mentors.Dr. Kisailus will oversee programs and services designed to providethem with one-stop shopping:• A Web portal (www.roswellpark.org/Site/Education/postdoc)where candidates can learn about, and apply for, postdoctoralopportunities at RPCI.14 | it’s academicAdam Kisailus, <strong>PhD</strong> (center), with postdocs Kjerstin Owens (left) and Gaia Bistulfi• A handbook outlining the responsibilities ofpostdoctoral scholars and their RPCI mentors,and apprising them of workshops and othertraining-enhancement opportunities.• The Science Teaching Experience forPostdoctoral Scholars (STEPS), a programaimed at developing teaching skills, fromcreating a syllabus to adapting coursecontent for high school or college students.Dr. Kisailus says the program might evolve intoa local certificate program that postdocs couldlist among other credentials on their CVs.• APoDS—the Association of PostDoctoral Scholars—an existingorganization that sponsors social events, presents guest speakers,and organizes poster sessions and other professional activities.• Networking opportunities within the biotech corridor of theBuffalo Niagara Medical Campus.Postdoctoral candidates and scholars can reach Dr. Kisailus at1-716-845-5944 or via email at Adam.Kisailus@roswellpark.org.Front and center:the postdoc as lecturer“Most postdoctoral scholars are expert in onefield, but they may lack experience in teachingor in presenting material at a seminar,” says Dr.Kisailus. To fill that gap, soon they’ll be able tostrengthen their teaching proficiency by presenting a lecturefor Oncology for Scientists. Required of all RPCI graduatestudents, the two-semester course typically enrolls 40-50students and is coordinated by AnneMarie W. Block, <strong>PhD</strong>,Director of the Clinical Cytogenetics Laboratory and AssociateProfessor of Oncology. Dr. Block says RPCI faculty present mostof the lectures, but Dr. Kisailus “thought we could include thepostdocs, because they’re not that far removed from thegraduate experience. They appreciate a good lecture, andthey know how to put one together.”Medical Dosimetry Program:“very competitive”– and it’s accreditedRPCI’s Chief Physicist, Matthew Podgorsak (center), with medical dosimetrist trainees (l. to r.) Mohamed Smith, Mobeen Tamimi, Barry Melancon, and Ashkan ParnianiThere’s growing demand in the U.S. for medical dosimetrists,who calculate the radiation dosage for cancer patients and use3D graphics and patient imaging to determine the best way todeliver radiation to the tumor site. RPCI’s Medical Dosimetry TrainingProgram stands out as one of only 12 in the nation accredited bythe Joint Review Committee on Education in Radiologic Technology(JRCERT). That seal of approval is important for trainees, becausecompletion of a JRCERT-accredited program is now a prerequisitefor taking the Certified Medical Dosimetrist Exam.Here Matthew Podgorsak, <strong>PhD</strong>, Chief Physicist at RPCI, discusseswhat it takes to achieve accreditation—and why it’s important.What’s the rationale behind thenew C<strong>MD</strong> Exam prerequisite?The Medical Dosimetrist Certification Board is trying to ensure thateducational programs are meeting the challenges of the moreadvanced technology that’s being used in cancer therapy today.Professional dosimetrists need to have proper practical training, butthey also need a basic understanding of the theory and principlesbehind the technology—something they can get only by attendingan accredited medical dosimetry training program.What elements of the training program cameunder review during the accreditation process?JRCERT reviewed a number of standards, from ethics issues to thenumber of didactic courses that must be offered. We also had toshow that our students are mentored by practicing medicaldosimetrists in both on-the-job and laboratory training. Our studentsinteract with not only the seven medical dosimetrists on staff, but alsophysicists, radiation oncologists, and business professionals. Thisgives students a well-rounded educational experience—and that’simportant, because when they are practicing professionally, they willhave to interact with many other people within the discipline.How many students applyto the program each year?There were 30-40 applicants for next year’s class [fall of 2009], andwe can enroll only six per year, so it’s a very competitive program.The number we can take is based in part on student access tomentors and equipment, especially the planning workstations.We have several workstations dedicated for student use, and arein the process of acquiring others, with the implied hope that wecan increase our enrollment.What’s the attraction to this field?Medical dosimetrists are scientists, but they also have to have acertain artistic flair in order to visualize the best way of using theavailable technology to deliver the radiation dose to our patients sothey get the best care. There are many degrees of freedom involved,so you need dosimetrists who are experienced, but who alsounderstand the basics of what they’re doing. That’s key, and that’swhat we have at <strong>Roswell</strong> <strong>Park</strong>.For more information about RPCI’s Medical Dosimetry TrainingProgram, visit www.roswellpark.org/Medical_Dosimetry_Training.15
The Head of the ClassTwo of the three top research projects recognized at the Jan. 22, 2009 MedicalStudent Research Forum at the University at Buffalo were based at RPCI, reportsArthur Michalek, <strong>PhD</strong>, FACE, RPCI’s Senior Vice President for Educational Affairs.The U.B. School of Medicine sponsors the annual forum as one way of “encouragingand supporting research training for medical students,” notes Dr. Michalek, whoserved as a judge for the event.Stephan Munich (2011) took second place for “Administration of ChemotherapeuticAgents Enhances the Therapeutic Effect Induced by a Survivin Molecular MimicVaccine Against Human Glioma,” which he completed under the guidance of RobertFenstermaker, <strong>MD</strong>, Clinical Chair of Neurosurgery, and Michael Ciesielski, <strong>PhD</strong>,Assistant Member in Neurosurgery.Matthew Sheldon tied with two other presenters for third place. He completed hisproject, “Apical Margins after Robot-Assisted Radical Prostatectomy: Does TechniqueMatter?” under the direction of Khurshid Guru, <strong>MD</strong>, Director of Robotic Surgery;James Mohler, <strong>MD</strong>, Chair, Urologic Oncology, and Leader of the Prostate Program;Hyung Kim, <strong>MD</strong>, Urologic Oncology; and Gregory Wilding, <strong>PhD</strong>, Assistant Chair,Biostatistics.First place was awarded to Andrew Baschnagel (2009), an applicant to RPCI’sRadiation Medicine Residency Program. His project, completed at the National<strong>Institute</strong>s of Health, addressed “Urinary c-MET and HGF Levels as an Indicator ofDisease Progression in Glioblastoma Multiforme Patients.”Low <strong>Cancer</strong>Incidence AmongSeneca NationshelfLIFECheck out these titles written or edited by RPCI faculty:Mitochondria & <strong>Cancer</strong>by Keshav Singh, <strong>PhD</strong>Member, <strong>Cancer</strong> Genetics(New York: Springer Publishing, 2008)Interferons: Current Statusby Kailash Chadha, <strong>PhD</strong>Associate Member, Molecular and CellularBiology (Kerala, India: Research Signpost, 2007)Martin Mahoney, <strong>MD</strong>, <strong>PhD</strong> and Arthur Michalek, <strong>PhD</strong>, FACEIn the most extensive review ever of cancerpatterns within an American Indian tribalgroup, RPCI researchers analyzed cancerpatterns in the Seneca Nation of Indiansfor the period from 1955-2004. Led byArthur Michalek, <strong>PhD</strong>, FACE, SeniorVice President for Educational Affairs, andMartin Mahoney, <strong>MD</strong>, <strong>PhD</strong>, AssociateProfessor of Oncology, Departments ofMedicine and Health Behavior, the studywas published in a recent issue of thejournal <strong>Cancer</strong>.The retrospective study examined patterns ofcancer incidence in 3,953 males and 4,193females who were registered tribal membersof the Seneca Nation. <strong>Cancer</strong> incidence rateswere based on data collected through acomputer match with the New York State<strong>Cancer</strong> Registry.The study found that, overall, no specifictype of cancer was significantly elevated. Infact, both male and female tribal membersdemonstrated significantly reducedincidences for all cancers combined. Inaddition, no specific age group showedsignificantly elevated incidence. A total of233 primary cancers were diagnosed amongSeneca males, with colorectal (20%) andprostate cancers (17%) the most common.Among female members, 256 cancers werediagnosed, with lung (20%) and breast cancer(16%) reported as the most commonmalignancies.“Among the unique strengths of this studywas the reliance on tribal roll books toidentify enrolled tribal members and theability to conduct a comprehensive studyover 50 years, leading to the accrual of morethan 120,000 person-years of observation,”says Dr. Michalek. “These parameters helpedovercome the issues of limited-sizepopulations, which has challenged studiesamong American Indian tribal groups in thepast. Additionally, the leaders of the SenecaNation demonstrated their trust in <strong>Roswell</strong><strong>Park</strong> researchers and a commitment tothe health of their members by allowingresearchers access to information requiredfor this comprehensive analysis.”Dr. Mahoney said cancer “remains a relativelyrare diagnosis among tribal members, whichplaces some limitation on the interpretationof these results. However, awareness of theseunique cancer patterns is of extraordinaryvalue to the Seneca Nation leaders as theydetermine healthy policy and cancerpreventionstrategies.”16 | it’s academic 17
To tap the potential of the “Y Generation” in the fight against cancer,more than a year ago RPCI unveiled its y<strong>Roswell</strong> campaign, aninitiative targeting people born between 1980-1996. The goal:encouraging young people’s interest in science and healthcarecareers and galvanizing their volunteer efforts on behalf of cancerresearch and patient care. Along the way, says Michael Wong, <strong>MD</strong>,<strong>PhD</strong>, FRCPC, Department of Medicine, “it became obvious thatone of the audiences we were tapping into was the teachers of theY Generation. Students can always point to a teacher who inspiredthem to take the next step.”That “aha!” moment, coupled with a request from local teachers forhealthcare career information they could share with their students, ledto the creation of the Touch Science program at RPCI. Geared towardscience teachers in the City of Buffalo’s public schools, Touch Sciencetook off Dec. 6, 2008, with a day-long program at RPCI, whereparticipants explored some of the latest, most exciting technology atRPCI—and tried it out for themselves. Led by RPCI faculty, the eventprovided an overview of RPCI’s educational programs as well asstrategies for giving science-oriented students a head start towardtheir dreams. Kelly Baudo, Supervisor of Science Education for theBuffalo Public Schools, was among the presenters.Thomas Dougherty, <strong>PhD</strong>, Chief Emeritus of the PhotodynamicTherapy (PDT) Center at RPCI, discussed his role in the developmentof the laser-based cancer therapy, now in use worldwide. As a chemistwho came to RPCI from industry, he’s the personification of the stronglink between chemistry and medicine. “The chemistry and physicsteachers had a blast with him,” says Catherine Donnelly, RPCI’sIntegrated Marketing Communications Manager and coordinator ofTouch Science. “They didn’t want to leave.”Dominic Smiraglia, <strong>PhD</strong>, <strong>Cancer</strong> Genetics, welcomed teachers to hislaboratory and engaged them in a description of “one type of changeGeneticist Dominic Smiraglia, <strong>PhD</strong>, demonstratesa new technique for DNA analysis.Zap! Thomas Dougherty, <strong>PhD</strong>, and Adam Sumlindemonstrate what happens to tumor cells with theright mix of laser light and chemicals.that occurs in tumor-suppressor genes, called DNA methylation,which generally leads to the silencing of tumor-suppressor genes.Then we studied one common tumor-suppressor gene in breastcancer samples to determine which samples had this methylationevent, and we found it in a few samples. Some teachers have labspace and could fairly easily be trained to do these types ofexperiments.”Ms. Donnelly says RPCI is “still inventing” Touch Science, whichcurrently focuses on three goals:• Enriching science education in the local schools• Promoting health education and a healthy lifestyleto help students reduce their cancer risk• Recruiting students into careers in healthcareand the sciences, especially in the field of oncology“My vision would be to eventually have a Touch Science program ina box,” she says. “We could include videos, a game or quiz showthey could use in the classroom, a Prevention quiz and <strong>Cancer</strong>s of theMonth quiz.” Right now she offers teachers a “Jeopardy”-style gamefeaturing questions on topics ranging from the history of RPCI tocurrent vaccine research.Steve Indalecio, a science teacher from Harriet Ross TubmanSchool #31, gave Touch Science two thumbs up:“We do a lot of these workshops throughoutthe year,” he notes. “This is my eighth yearas a teacher, and I can honestly say this isthe best workshop I’ve ever attended.”Says Dr. Wong, “We need to engage people, capture theirimagination and energy and capture their enthusiasm for teachingchildren. Great scientists and great physicians will be the end result.”Robotics Director Khurshid Guru, <strong>MD</strong>, letsteachers experience firsthand the on-targetprecision of robot-assisted surgery.RPCI patient Prudy Georgia, seated, with nurse Susan OnettoPrudy watched as I pawed through my cart of art supplies insearch of something we could try. Her hands were no longerthe swollen claws they were at my last visit, the joints of herfingers no longer purple and hurting from the effects ofchemotherapy. She waved her hands at me to show them in theirtrue form. They looked better now, just reddened. But when sheturned them over, I could see the peeling flesh on her palms andalmost feel for myself the rawness of her tender fingers. Nothing Icould offer was soft enough for her to touch comfortably, and eventhough she seemed curious to try something, we decided to forgoan art project that day to let her healing hands rest. But she invitedme to stay anyway, and we chatted about her week and her hopes togo home, maybe after the weekend.As Prudy talked, she watched through the open door the activity atthe nurses’ station. She craned to see more: “There goes my nurse.”I wondered if she needed something, but before I could ask, Prudywent on: “Her name is Susan Onetto. The day I decided I was readyto buzz my head, she helped me. I’d had enough; the hair waseverywhere, even in my eggs at breakfast. When I told her what Iwanted to do, she said, ‘Oh, I can help you with that,’ and she cameback with a buzzer and buzzed my head in the shower. Just think ofall the things she must have had to do, and she took the time to helpme with my hair! I felt so much better, and she did a good job, don’tyou think?” She patted her downy head with her sore hands. I agreed.She did look elegant with her new short hair.TellMeA Story!A transcript of a narrative recorded by RPCI Artist-in-Residence Ann Frankduring a recent visit on 5W with patient Prudence “Prudy” GeorgiaPrudy continued, “Susan has such an air of competence in everythingshe does, even the small things—and everything with a smile! Whensomeone takes such care in all they do, big things and small things,it’s a window into their spirit. It says something about who they are.“They’re all like that here. I feel very confident in their care. One day Iwas coughing, and I gagged a little. I could see them all at thenurses’ station, and six heads turned at once to check on me. ‘I’mokay!’ I told them, quick, before they all ran in.“All the nursing staff, and the aides, too—they don’t shirk anything.Two of them are even pregnant—Cassie and Roxanne. They don’t letthat slow them down.” She was impressed with how late into thepregnancy one of the nurses was working—her baby was due verysoon—and though the other nurse was not as far along, she was nowlooking pregnant. It was obviously a welcome distraction for Prudy tobe able to share in their joy and anticipation.Frowning a little, Prudy tried to think of more names, mutteringabout her ‘chemo brain.’ “Do you know Theresa? She can’t help butbe a fabulous caregiver.”And she spoke of the nurses’ good humor: “Have you met Roberto?He’s a riot!“The nurses and aides are so joyful here. They work all day, with usall so sick, and they still have fun and make us smile.”18 | yroswellfeature | 19
“In Magnet hospitals,patient outcomes are better, andtheir length of stay is shorter.”Lisa Boris, RN, BSN, likes to think of it as “the Nobel Prize for nursing” – andindeed, designation as a Magnet Hospital for Nursing Excellence is an honor earnedby fewer than 5% of all hospitals in the U.S. For the first time, RPCI is on a quest forthat distinction, given by the American Nurses Credentialing Center (ANCC), the nation’slargest nursing accrediting and credentialing organization.“It’s a rigorous process,” explains Ms. Boris, Nurse Manager of RPCI’s Upper and Lower GICenters. That’s an understatement! For starters, members of the nursing staff are hard atwork on a 3,500-page document that demonstrates how RPCI measures up in 20 differentareas of nursing quality that the ANCC calls “forces of magnetism.” Among other points,ANCC reviewers want to see evidence that RPCI nurses understand their roles in the<strong>Institute</strong>’s mission and vision; that the administration listens to their ideas and fosters acollegial, collaborative atmosphere; that the <strong>Institute</strong> provides a safe and pleasant workenvironment for its nurses; and that the care they deliver contributes directly to thehighest-quality care for patients.Patients are the primary beneficiaries of the Magnet label, because it helps them identifyhospitals where they’ll receive the best care. “In Magnet hospitals, patient outcomes arebetter, and their length of stay is shorter,” notes Maureen Kelly, RN, MS, RPCI’s VicePresident of Patient Care Services and Chief Nursing Officer. “U.S. News & World Reporthas added Magnet status as one of the indicators for measurement of the top 100 cancercenters and top 100 hospitals in the U.S.”are drawn to RPCI by the emphasis onpatient care. “Our nurse-to-patient ratiosare excellent,” she explains, “which givesnurses the opportunity to spend time notonly on quality care but also to educatepatients and families about continued careoutside the hospital. We build a partnershipwith the patient and have better outcomesas a result.”The <strong>Institute</strong> also encourages its more than600 nurses to further their education, withpay incentives for earning a master’s degreeor <strong>PhD</strong>, and strong support for nurse-ledresearch. “Some of the best ideas comefrom our frontline, bedside nurses,” saysMs. Boris. “They see firsthand the needs ofour patients, and they’re making adifference in research. The administration istelling them, ‘Your ideas matter.’” Ms. Kellyadds that the ANCC will also examinenurses’ credentials, from the degrees theyhold to the numbers of ContinuingEducation units they have earned.After the application package is deliveredFebruary 1, 2010, the ANCC will beginevaluating how well RPCI fulfills the 20“forces of magnetism.” If the documentpasses muster, an ANCC accreditation teamwill conduct a three-day site visit to askcandid questions of the nurses and otherRPCI staff about the <strong>Institute</strong>’s nursingmodel. “We have to show strongcollaboration between the Department ofNursing and the entire institution inachieving positive patient outcomes,” saysMary Ann Long. “Ultimately, that’s whatMagnet is about.”Ms. Kelly notes that data gathered for theMagnet self-evaluation document will serveas benchmarks for continued improvementin nursing at RPCI, and will form “a plan ofaction for the coming years.” Whileaccreditation is granted for a four-yearperiod, she adds, retaining Magnet statuswill require continual evaluation, bothinternally and by the ANCC.Lisa Boris is confident of the outcome.“There’s nowhere better to go for cancercare than <strong>Roswell</strong> <strong>Park</strong>, and our nursingcare reflects that,” she says proudly. “Wealready know that. We want everyone elseto know it, too.”The Magnet seal of approval is also a beacon for talented nurses who are looking for thebest places to work, and Ms. Boris notes that RPCI already has solid proof that it belongsin that category. “We have a waiting list of people who want to come here,” she says.One major attraction: the option of working three 12-hour days followed by four daysoff—an arrangement that grew from the nurses’ request for “a work-life balance.”Mary Ann Long, RN, MS, RPCI’s Director of Patient Care Services and Magnet Director,says the waiting list includes both recent grads and nurses with extensive experience, who20 | feature21
’sVisiting Professor inOncology ProgramL. to r.: Kay Seekamp, RN, Pfizer, Inc.; JamesMarshall, <strong>PhD</strong>; Peter Steffan, Pfizer; Ian Thompson,<strong>MD</strong>; and Brad Salmon Pfizer, Associate Director,Clinical Protocol Manager, Pfizer OncologyIan Thompson, <strong>MD</strong>, Professor and Endowed Chair of the Departmentof Urology at the University of Texas Medical Center, Vice Chair ofthe National <strong>Cancer</strong> <strong>Institute</strong>’s Early Detection Research <strong>Institute</strong>,and newly named Chair of the Genitourinary Committee of theSouthwest Oncology Group, visited RPCI recently as VisitingProfessor in Oncology under the auspices of Pfizer’s highlycompetitive Medical and Academic Partnerships grants program.RPCI was one of only eight institutions nationwide to win grantsupport for a three-day visit by a distinguished expert in oncology.Dr. Thompson is also Clinical Associate Professor in the Departmentof Surgery/Uniformed Services of Health Sciences, Department ofSurgery, Bethesda, <strong>MD</strong>. His RPCI visit focused on the prevention,detection and management of prostate cancer; cancer screening;and chemoprevention strategies. James R. Marshall, <strong>PhD</strong>, SeniorVice President, <strong>Cancer</strong> Prevention and Population Sciences, and James Mohler, <strong>MD</strong>, Chair ofGenitourinary Surgery at <strong>Roswell</strong> <strong>Park</strong>, were local hosts to Dr. Thompson.The Visiting Professor in Oncology program is designed to advance oncology by creatingopportunities for educational visits by prominent cancer experts to U.S. medical schools/teaching hospitals and cancer centers. Grant recipients are chosen by an independent academicadvisory board of experts in the oncology field. Dr. Thompson lectured and met with Urologyresidents and fellows and with Urology and Prevention faculty at both the University at Buffaloand <strong>Roswell</strong> <strong>Park</strong>.(FAC) Clara M. Ambrus, <strong>MD</strong>, <strong>PhD</strong>, FACP, and Julian L. Ambrus,<strong>MD</strong>, <strong>PhD</strong>, FACP, have been awarded the American College ofPhysicians (ACP) Laureate Award, given for “abiding commitment toexcellence in medical care, education, research, or service to theircommunity, chapter, and ACP. Awardees are physicians with a longhistory of excellence and peer approval in their specialty of internalmedicine.” Julian Ambrus is also President-Elect of the CatholicAcademy of the Sciences, Washington, DC.(FAC) <strong>John</strong> Cowell, <strong>PhD</strong>, Associate Director for Basic Science andProfessor of Pathology in Medical College of Georgia <strong>Cancer</strong> Center,has been named a Georgia <strong>Cancer</strong> Coalition Distinguished <strong>Cancer</strong>Scholar. He served previously as Chair of <strong>Cancer</strong> Genetics at RPCI.(<strong>PhD</strong>) Andrew Freedman, <strong>PhD</strong>, of the National <strong>Cancer</strong> <strong>Institute</strong>’sDivision of <strong>Cancer</strong> Control and Population Sciences, wasco-leader of a team that developed one of the first colorectalcancer absolute risk assessment models. Available online atwww.cancer.gov/Colorectal<strong>Cancer</strong>Risk, the tool was thesubject of a recent article in the NCI <strong>Cancer</strong> Bulletin(www.cancer.gov/ncicancerbulletin/011309/page3).Oh, the Places You’ve Gone!(FAC) Douglas E. Williams, <strong>PhD</strong>, has been promoted fromPresident to CEO of ZymoGenetics, Inc., Seattle, Washington.ZymoGenetics discovers and develops novel protein therapeuticsbased on the company’s research and biological insights into keydisease pathways.Congratulations!Nicholas Petrelli, <strong>MD</strong>, FACS, former Chair of Surgery at RPCI,congratulates <strong>Roswell</strong> <strong>Park</strong> Alliance founders Anne and Donna Gioia,who received the Society of Surgical Oncology’s James EwingLayman’s Award at the 62nd Annual <strong>Cancer</strong> Symposium. Anne andDonna, who were honored for their passionate leadership andadvocacy, join a stellar roster of awardees, including General H.Norman Schwarzkopf and the late Ann Landers.(FAC) Michael McGarry, <strong>PhD</strong>, is Vice President of Preclinical Studiesat Medelis, Inc., an oncology contract research organization based inPhoenix, AZ.Join us for the following Faculty Forum lectures, each presented from 8-9 a.m. in the Zebro Family Conference Room of RPCI’sCenter for Genetics and Pharmacology. Physician participants will be awarded AMA Category 1 credit.May 20Mihich Lecture, “Mechanisms andTherapeutic Targeting of the TumorMicroenvironment,” with Douglas Hanahan,<strong>PhD</strong>, Professor of Biochemistry, University ofCalifornia at San FranciscoMay 27“Dissecting Human Genomes to Understand‘Stemness’ and <strong>Cancer</strong>,” with Gennadi V.Glinsky, <strong>MD</strong>, <strong>PhD</strong>, Head of the Translationaland Functional Genomics Laboratory,Ordway <strong>Cancer</strong> Center, Albany, NY22 | forum&functionJune 3Director’s Conference, “Monoclonal AntibodyTherapy of <strong>Cancer</strong>: Making Better Antibodies,and Making Antibodies Better,” with GeorgeWeiner, <strong>MD</strong>, Director of the HoldenComprehensive <strong>Cancer</strong> Center at TheUniversity of IowaJune 10Weiss Memorial Lecture, “Targeting theIntrinsic Therapeutic Resistance of Breast<strong>Cancer</strong> Tumor-Initiating Cells,” withJeffrey Rosen, <strong>PhD</strong>, the C.C. Bell Professor,Department of Molecular & Cellular Biology,Baylor College of MedicineJuly 22Cori Lecture, “Translational Control of<strong>Cancer</strong>,” with Nahum Sonenberg, <strong>PhD</strong>, theJames McGill Professor of the Rosalind andMorris Goodwin <strong>Cancer</strong> Centre, McGillUniversity, Montreal, and Recipient of the2008 Canada Gairdner International Award,given for his pioneering discoveries in cellulartranslation of genetic information.(MS) Herbert Newton, <strong>MD</strong>, FAAN, is Professor of Neurologyand Oncology, and Director of the Division of Neuro-Oncology,Department of Neurology, of The Ohio State University MedicalCenter and the James <strong>Cancer</strong> Hospital. He holds the EstherDardinger Chair in Neuro-Oncology and serves as Co-Director of theDardinger Neuro-Oncology Center at the James <strong>Cancer</strong> Hospital.You can connect to your RPCI colleagues on a numberof Social Networking sites—including LinkedIn ® , Twitter,Facebook and myspace.In photo (above, l-r) are Anne Gioia; Candace <strong>John</strong>son, <strong>PhD</strong>, Deputy Director, RPCI;Dr. Petrelli, Medical Director, Helen F. Graham <strong>Cancer</strong> Center, Christiana Care HealthServices; Donna Gioia; and Cindy Eller, Vice President, Development, RPCI.KEY: SMR (Summer Reserach Program); <strong>PhD</strong> (Doctoral Program);PDoc (Postdoctoral); MS (Master’s Degree Program);STF (Staff); FAC (Faculty); FLW (Fellow); RES (Resident)I just received the RPCI alumni magazine [which featured an articleabout West Point cadets who participated in a summer studyprogram at RPCI]. Thanks so much for the positive press andcontinuing support. In late October, each cadet presented to ourfaculty about their RPCI research and experience over the summer.It inspired a few cadets to consider the option for next summer,and feedback from the faculty was great. Thanks and best wishes.Melissa R. Eslinger, MAJ, LGAssistant Professor, Course Director, GeneticsU.S. Military Academy, West Pointclassnotes | 23
Photo courtesy of Lockport Union Sun & JournalThe Road Less TraveledDr. Natalie Zeitouni in St. Lucia“I want to help thesepeople as much asI can, and I’m at apoint in my careerwhere I’ve donea lot, so now I canvolunteer in anarea that I knowwell—dermatology.”Every year, more than 300,000 vacationers flock to the Caribbean island of St. Lucia tohike through the exotic rainforest and lounge on the sunny beaches. But Dr. NathalieZeitouni, Interim Chair of Dermatology at RPCI, set her sights on a different destinationwhen she traveled to St. Lucia recently with the nonprofit group Health VolunteersOverseas (HVO).At St. Jude Hospital, near Vieux-Fort, on the island’s southern coast, she cared forpatients ranging from the very young to the very old, and shared her expertise indermatology with physicians, residents and nurses. She also delivered gifts ofmedications and certain medical supplies provided by Howard Stoll, Jr., <strong>MD</strong>, whoretired recently from RPCI’s Dermatology Department. Clothing and small gifts werepresented to children living in an orphanage near Vieux-Fort.At <strong>Roswell</strong> <strong>Park</strong>, Dr. Zeitouni specializes in Mohs surgery and leads research on unusualskin tumors, the use of photodynamic therapy for treating cutaneous carcinomas, andthe identification of risk factors and development of treatment guidelines for rare skincancers. Because her time in St. Lucia was limited, she focused partly on teaching themedical staff, “so they can take care of their own patients.”Dr. Zeitouni hopes to volunteer with HVO again in the future, perhaps in Peru or anotherarea where the program places an even greater emphasis on teaching. “I’ve alwayswanted to give back,” she says. “I want to help these people as much as I can, and I’mat a point in my career where I’ve done a lot, so now I can volunteer in an area that Iknow well—dermatology.”An <strong>MD</strong> WithHorse Sense“When you’reriding, you can’tthink about anythingelse. When I’mtaking a challenginglesson, I can’t thinkabout my kids orwhat I have to doat home or evenmy patients—andthat’s good.”Three-year-old Rory “saddles up for <strong>Roswell</strong>” with a hand fromhis mom, Tracey O’Connor, <strong>MD</strong> (right), and Jeffrey Durbin.Growing up in Indiana, Tracey O’Connor was among a group of “extremelyenthusiastic little girls” who took riding lessons at a local livery stable. “I would dothat once a week, and then every Christmas nag my parents to buy me a pony,and every Christmas night, I would cry because it didn’t happen,” recalls Dr. O’Connor,Attending Physician in RPCI’s Department of Medicine. But persistence paid off: “WhenI was 11, my mother finally nagged my father into getting me a pony of my own.”Today Dr. O’Connor rides a horse instead of a pony, and her love of riding is stronger thanever. “It’s so engrossing,” she says. “When you’re riding, you can’t think about anythingelse. When I’m taking a challenging lesson, I can’t think about my kids or what I have todo at home or even my patients—and that’s good.”Dr. O’Connor’s equestrian interests led to her friendship with Sue and Terry Williams,owners of the Chestnut Ridge Equestrian Center in Gasport, New York, where her horse,Providence, is stabled. Terry died of colon cancer not long after he and Sue foundedSaddle Up for <strong>Roswell</strong>, a riding event that has raised more than $25,000 to date for the<strong>Roswell</strong> <strong>Park</strong> Alliance Foundation. Dr. O’Connor, a sponsor, has competed in the eventevery year, along with scores of other participants who understand the dynamic betweenhorse and rider.“Horses are unpredictable animals,” says Dr. O’Connor. “They have minds and feelingsand personalities of their own. You develop relationships with them over time, and whenthey give you what you’re asking them to do, even though it may be difficult for them,that’s a great feeling.”24 | extracurriculars 25
Return Service RequestedNON-PROFIT ORG.U.S. POSTAGEPAIDBUFFALO, NEW YORKPERMIT NO. 61Doctors Rank<strong>Roswell</strong> <strong>Park</strong>Among Nation’s Top<strong>Cancer</strong> HospitalsWorld’s Largest Circulation Magazine<strong>Roswell</strong> <strong>Park</strong> <strong>Cancer</strong> <strong>Institute</strong> ranks among the nation’s topspecialty hospitals for general cancer care on a list to bepublished in the May/June 2009 issue of AARP The Magazine.The publication has the largest circulation of any magazine inthe world, with more than 34 million readers.The list also includes:• University of Texas M.D. Anderson <strong>Cancer</strong> Center,Houston, TX• Memorial Sloan-Kettering <strong>Cancer</strong> Center, New York City• Dana-Farber <strong>Cancer</strong> <strong>Institute</strong>, Boston, MA• Mayo Clinic, Rochester, MN• City of Hope, Duarte, CA• The <strong>John</strong>s Hopkins Hospital, Baltimore, <strong>MD</strong>• Duke University Hospital, Durham, NCThe list was compiled by Consumers’ Checkbook, anindependent, nonprofit consumer service organization that rateseverything from cars and appliances to veterinarians, creditcards, and pest-control firms. Recognizing that growing numbersof patients are traveling outside their communities in order toreceive the best health care, Consumers’ Checkbook polleddoctors across the nation to find out where they would be mostlikely to send patients who needed specialized care.The resulting list, called “Doctors’ Faves” on the AARP website,includes doctors’ picks for the best hospitals for general cardiaccare, general cancer care, mystery diagnoses, neurosurgery,and eye care. The list can be found online atwww.aarpmagazine.org/health/right_hospital_for_you.html