Techniques in Pediatric MRI – Tips for Imaging Children - Siemens ...
Techniques in Pediatric MRI – Tips for Imaging Children - Siemens ...
Techniques in Pediatric MRI – Tips for Imaging Children - Siemens ...
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
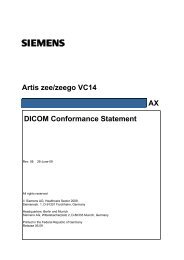
How-I-do-it1A1B1 Longer TR and TE times are generally required when imag<strong>in</strong>g very young children. The high water content <strong>in</strong> neonatal bra<strong>in</strong>s, coupled with the lackof fatty myel<strong>in</strong> results <strong>in</strong> a reduction <strong>in</strong> contrast-to-noise ratio (CNR) and grey/white matter differentiation. Restore pulses on T2w imag<strong>in</strong>g can improve CSFcontrast and allow shorter TR times to reduce scan time.<strong>Techniques</strong> <strong>in</strong> <strong>Pediatric</strong> <strong>MRI</strong> <strong>–</strong><strong>Tips</strong> <strong>for</strong> Imag<strong>in</strong>g <strong>Children</strong>Glenn CahoonRoyal <strong>Children</strong>’s Hospital, Melbourne, AustraliaMagnetic resonance imag<strong>in</strong>g (<strong>MRI</strong>) exam<strong>in</strong>ationsof children require a particularset of skills and expertise <strong>in</strong> order to successfullyobta<strong>in</strong> diagnostic images withm<strong>in</strong>imal distress to the patients and theirfamily. There have been many developments<strong>in</strong> <strong>MRI</strong> <strong>in</strong> recent years, whichhave lead to a dramatic <strong>in</strong>crease <strong>in</strong> thenumber and types of referrals we are nowsee<strong>in</strong>g <strong>for</strong> pediatric MR exam<strong>in</strong>ations.This paper provides an overview of thechallenges that pediatric patients raise<strong>in</strong> the MR sett<strong>in</strong>g, and some of thedifferent techniques that may beemployed to overcome these difficulties.While some technical modificationsare described, the focus is on practicalrecommendations that can assist youngchildren to comply with the MR procedure,and m<strong>in</strong>imize the use of anesthesiawith this vulnerable population.<strong>Pediatric</strong> MR imag<strong>in</strong>g can be considereda series of subspecialties. Each area,neurology, cardiac, MSK, oncology, allhave their own subtle nuances that alteras patients mature. In our facility we rout<strong>in</strong>elyscan patients from the early fetal*stages right through to young (and not soyoung) adults with complex congenitalconditions. Each of these fields, andstages of development requires their ownspecialized skills, knowledge, and equipmentto be per<strong>for</strong>med appropriately,however, there is a number of commonchallenges and techniques that apply toimag<strong>in</strong>g pediatric patients.6 MAGNETOM Flash · 2/2011 · www.siemens.com/magnetom-world
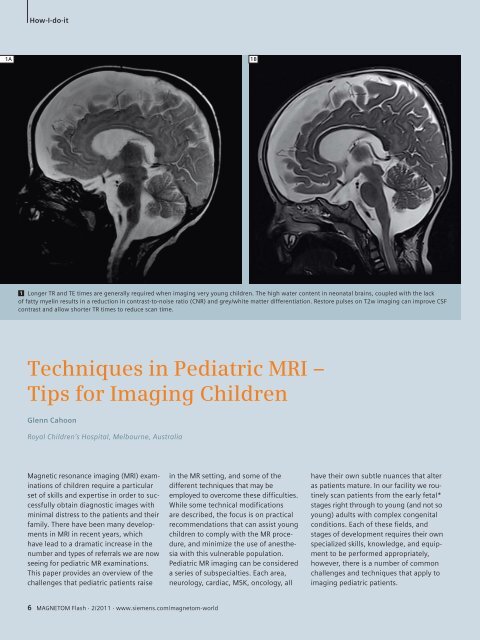
How-I-do-itChallenges ofscann<strong>in</strong>g childrenSafety<strong>MRI</strong> of children poses a number of specificsafety issues with patient heat<strong>in</strong>gbe<strong>in</strong>g the primary concern. Neonatesand <strong>in</strong>fants <strong>in</strong> particular have immaturethermoregulation mechanisms, andhigher core body temperatures mak<strong>in</strong>gthem particularly sensitive to RF heat<strong>in</strong>geffects [1]. These mechanisms are furtheraffected by sedation and anesthesiacommon <strong>in</strong> pediatric imag<strong>in</strong>g [2], orwhen babies are swaddled <strong>for</strong> imag<strong>in</strong>g[1]. <strong>Children</strong> also have a greater surfacearea to weight ratio than adults. Thismeans <strong>for</strong> a given weight we often needto expose a greater surface area of thepatients to the RF field. This can lead to<strong>in</strong>creased heat<strong>in</strong>g <strong>in</strong> children, anddecrease their ability to dissipate thisheat. There is <strong>in</strong>tr<strong>in</strong>sic uncerta<strong>in</strong>ty <strong>in</strong>current specific absorption rate (SAR)predictions based on extrapolated datafrom phantom models [3] particularlydue to factors such as body shape, size,composition, and position with<strong>in</strong> the MRscanner. While def<strong>in</strong>itive data on safetyrisks are not yet available, close monitor<strong>in</strong>gof children, particularly critically illor compromised <strong>in</strong>fants, is desirablewhen us<strong>in</strong>g higher field strengths andhigh SAR scan techniques [1].Anesthesia is an important safety consideration<strong>in</strong> pediatric <strong>MRI</strong>. While seriouscomplications such as death are rare,there are significantly higher rates ofmorbidity, particularly amongst neonates,when compared to adult anesthesia [2].Aside from adverse events there are anumber of common side effects <strong>in</strong>clud<strong>in</strong>gnausea, vomit<strong>in</strong>g, drows<strong>in</strong>ess andagitation upon awaken<strong>in</strong>g, which affectabout one third of pediatric patients [2].The challenge of monitor<strong>in</strong>g patients <strong>in</strong>the MR environment coupled with thereduced ability <strong>for</strong> the patient to communicateadverse events creates significantadditional risks [4]. If sedation is required,the associated risks need to be taken<strong>in</strong>to account when decid<strong>in</strong>g to imageyoung children.AnatomyNormal structures <strong>in</strong> children are smallerthan <strong>in</strong> the average adult. This createsa challenge both <strong>in</strong> terms of the availablesignal, and the limits of our scan resolution.Anatomy is further complicated bycongenital anomalies and mal<strong>for</strong>mationsas well as developmental changes [5].At birth we are about 75% water and wedry out as we age to about 55<strong>–</strong>65%water <strong>for</strong> an average adult. This is bestappreciated <strong>in</strong> the neonatal bra<strong>in</strong>. Thehigh water content, and lack of fattymyel<strong>in</strong>, requires an <strong>in</strong>crease <strong>in</strong> TE onT2-weighted imag<strong>in</strong>g to around 150<strong>–</strong>160 ms to improve contrast. With somuch of the available hydrogen <strong>in</strong> looselybound water, there often is not muchto <strong>in</strong>fluence relaxation. The use of fastrecovery (restore) pulses at the end ofthe echo tra<strong>in</strong> improves the signal-tonoiseratio (SNR) while allow<strong>in</strong>g <strong>for</strong>shorter TRs to be used (Fig. 1).T1 contrast can be particularly flat requir<strong>in</strong>gan <strong>in</strong>crease <strong>in</strong> TR to around 1,200 msat 1.5 Tesla. The use of <strong>in</strong>version recoverytechniques, and magnetization prepared3D imag<strong>in</strong>g such as MPRAGE, are evidentat many <strong>in</strong>stitutions, particularly athigher field strengths [5].2Pathology<strong>Children</strong> are notoriously poor reportersof symptomatology, and their oftenvague and non-specific symptoms canbelie the seriousness of their condition.Cl<strong>in</strong>ical exam<strong>in</strong>ation is often very difficult,so <strong>MRI</strong> requests are seldom specific.There are many transient appearanceson MR images that can be considerednormal at some stages of developmentand abnormal at others. Recogniz<strong>in</strong>g theappearance of normal from abnormaldevelopment on MR images and determ<strong>in</strong><strong>in</strong>gthe optimal sequences and factorsto best display them presents a challengeto technologists with little pediatricexperience.An awareness of the conditions thatare commonly found <strong>in</strong> the pediatricpopulation is necessary to tailor scansappropriately.PhysiologyPulse rate, blood flow, and respirationrates are considerably faster <strong>in</strong> children,with normal heart rates that can be <strong>in</strong>excess of 140 bpm and respiratory ratesof 40/m<strong>in</strong> [5]. <strong>Children</strong> typically f<strong>in</strong>d itdifficult to satisfactorily hold their breath,creat<strong>in</strong>g significant challenges <strong>in</strong> cardiac,2 Coronal PD-weighted image of an osteo-chondral defect (OCD) of the distal phalynx of theright toe.MAGNETOM Flash · 2/2011 · www.siemens.com/magnetom-world 7
How-I-do-it3chest and abdom<strong>in</strong>al imag<strong>in</strong>g. Increasedflow rates lead to artifacts from bloodvessels and cerebrosp<strong>in</strong>al fluid (CSF)pulsations, creat<strong>in</strong>g difficulties withsp<strong>in</strong>e and Time-of-Flight (TOF) vesselimag<strong>in</strong>g [5]. Differences and evolution<strong>in</strong> pediatric physiology may also leadwto changes <strong>in</strong> the mechanism of <strong>in</strong>jury,or the types of <strong>in</strong>juries that occur <strong>in</strong>children, such as growth plate <strong>in</strong>juriesand osteo-chondral defects (OCD) [6].BehavioralSedation or anesthetic is commonlyrequired <strong>for</strong> younger children or thosewith significant behavioral problems.Factors such as temperament, stress,pa<strong>in</strong>, and illness play an important role<strong>in</strong> patient compliance, creat<strong>in</strong>g difficulties<strong>in</strong> establish<strong>in</strong>g def<strong>in</strong>itive age limits<strong>for</strong> identify<strong>in</strong>g which children will requirethese procedures [7]. Encourag<strong>in</strong>g childrento co-operate <strong>for</strong> an <strong>MRI</strong> exam<strong>in</strong>ationand identify<strong>in</strong>g those who cannotare arguably the most significant challenges<strong>in</strong> pediatric <strong>MRI</strong>.<strong>Techniques</strong> <strong>in</strong> scann<strong>in</strong>gchildren without sedationPreparationAt our <strong>in</strong>stitution we beg<strong>in</strong> scann<strong>in</strong>gwithout sedation from about five yearsof age, although some positive outcomeshave been obta<strong>in</strong>ed with patientsas young as three years. Adequate preparationof children <strong>for</strong> the <strong>MRI</strong> procedurehas been vital <strong>in</strong> achiev<strong>in</strong>g these results.Our facility employs the services of educationalplay therapists who use a rangeof resources to assist children to complywith the procedure, such as brochures,<strong>MRI</strong> toys and storybooks, discussions withparents, and, most importantly, the‘mock <strong>MRI</strong>’ procedure.SimulationThe ‘mock <strong>MRI</strong>’ procedure <strong>in</strong>volves childrenundergo<strong>in</strong>g a simulated scan withthe assistance of a play therapist priorto the actual diagnostic scan. It acts asboth a screen<strong>in</strong>g tool, to assist <strong>in</strong> identify<strong>in</strong>gchildren who are likely to be ableto comply with the <strong>MRI</strong> procedure,and also helps to prepare these children,by familiariz<strong>in</strong>g them with the environment,sounds, and equipment, whileteach<strong>in</strong>g them skills (such as breath<strong>in</strong>g,relaxation, or distraction) to cope withthe actual procedure (Fig. 2). Use ofthe ‘mock’ magnet has led to a markedreduction <strong>in</strong> the numbers of patientswho have required anesthetic [7] andreduced the time required <strong>for</strong> the diagnosticscan [8]. Several pediatric facilities<strong>in</strong> various countries have <strong>in</strong>troduceda mock procedure <strong>in</strong> their facilities <strong>in</strong>recent years [9].CommunicationSpecialist staff and equipment are clearlyhelpful <strong>in</strong> assist<strong>in</strong>g children to complywith an MR scan. However, <strong>for</strong> technologists,an awareness of how to talk to childrenand adolescents at different stagesof development and the use of psychologicaltechniques, such as distraction andrelaxation, can be the critical factor determ<strong>in</strong><strong>in</strong>gwhether a young person is will<strong>in</strong>g,or able, to carry out the procedure.Many children are withdrawn or uncommunicativewhen nervous about a medicalprocedure, and tak<strong>in</strong>g the time tohelp the child to feel safe and secure <strong>in</strong>the environment is important. Compliancewith preschool children may befacilitated by engag<strong>in</strong>g <strong>in</strong> pretend play,where the child can be encouraged toframe the experience <strong>in</strong> familiar and nonthreaten<strong>in</strong>gways [10]. Nonverbal communicationcomprises a significant proportionof a child’s <strong>in</strong>teraction with theworld at this stage, and young childrencan pick up on their parents’ anxiety orthe technologist’s impatience throughnonverbal clues. They may not understandthese feel<strong>in</strong>gs and can <strong>in</strong>terpretthem as anger or fear of the exam<strong>in</strong>ation.Professionals who work with childrentypically take steps to ensure that boththeir verbal communication and body3 Mock <strong>MRI</strong> simulator <strong>–</strong> this procedure identifies patients that are able to comply withthe requirements of an <strong>MRI</strong> exam<strong>in</strong>ation, as well as prepare them <strong>for</strong> the cl<strong>in</strong>ical scan,sav<strong>in</strong>g unnecessary appo<strong>in</strong>tments and valuable scanner time.8 MAGNETOM Flash · 2/2011 · www.siemens.com/magnetom-world
How-I-do-itTable 1: Communicat<strong>in</strong>g with childrenEngage with the child Get down on their level Use simple language Ma<strong>in</strong>ta<strong>in</strong> eye contactFrame the experience Help them verbalize Involve the child’s past Smiletheir experienceexperiences / playEmpower the child Offer limited choices Praise good behavior Be positive “I know you can do this”language are reassur<strong>in</strong>g and convey calmnessand confidence (Table 1). Positivere<strong>in</strong><strong>for</strong>cement, where the child is praised<strong>for</strong> their ef<strong>for</strong>ts at each step, can be veryhelpful.School age children are able to engagemore actively <strong>in</strong> the procedure, and mayrespond well to ef<strong>for</strong>ts to <strong>in</strong>crease theirperceived control. Medical exam<strong>in</strong>ationsoften take the locus of control awayfrom the patient, and this is particularlytrue <strong>in</strong> pediatrics where someone elseusually makes the decisions <strong>for</strong> thepatient. Empower<strong>in</strong>g children by offer<strong>in</strong>gsome choice <strong>in</strong> how they can havethe scan can be helpful. This is particularlyimportant dur<strong>in</strong>g adolescence; aperiod of rapid social and physicalchanges [10], when <strong>in</strong>creased autonomyis important, yet can be hampered byserious illness. Adolescents are less likelythan children or adults to bl<strong>in</strong>dly follow<strong>in</strong>structions, and may be reluctant toaccept or comply with the scan <strong>in</strong> theabsence of a flexible approach, where thetechnologist is sensitive to their concerns.Distraction and relaxationDistraction can be a powerful tool <strong>for</strong>reduc<strong>in</strong>g anxiety and <strong>in</strong>creas<strong>in</strong>g patientcompliance. Distraction techniquescan be either active or passive. Passivetechniques such as audiovisual aids areuseful dur<strong>in</strong>g the scan when patients arerequired to lie still <strong>in</strong> the bore. Hav<strong>in</strong>ga po<strong>in</strong>t of <strong>in</strong>terest (such as a parent orvideo screen) is helpful <strong>in</strong> ma<strong>in</strong>ta<strong>in</strong><strong>in</strong>gthe patient <strong>in</strong> one position. Active techniqueswhich require patient participationsuch as relaxation breath<strong>in</strong>g, guidedimagery, or complex puzzle tasks, areuseful <strong>in</strong> relax<strong>in</strong>g children be<strong>for</strong>e <strong>MRI</strong> orper<strong>for</strong>m<strong>in</strong>g <strong>in</strong>terventions such as <strong>in</strong>travenouscannulation and general anesthetic(GA) <strong>in</strong>ductions.Successful use of<strong>in</strong>travenous (IV) contrastIV cannulation is a major cause of anxiety<strong>in</strong> young patients present<strong>in</strong>g <strong>for</strong><strong>MRI</strong> exam<strong>in</strong>ation. Limit<strong>in</strong>g the use of IVcontrast <strong>in</strong> pediatric exam<strong>in</strong>ations canoften mean the difference between asuccessful awake scan and a rebook <strong>for</strong>sedation. This requires the support ofthe radiologists to make decisions regard<strong>in</strong>gwhether the benefits of contrast areworth the potential distress to the patient.Where contrast is necessary, it is oftenhelpful to separate the procedures ofIV placement and the MR exam by eitherplac<strong>in</strong>g the cannula be<strong>for</strong>e the exam<strong>in</strong>ationor offer<strong>in</strong>g a break between thepre and post contrast scans. Manychildren respond well to be<strong>in</strong>g able tochoose an IV site. Active distractiontechniques can be helpful, and there areseveral aids available to assist with thepa<strong>in</strong>, such as local anesthetic creams,ice, or nitrous oxide.Protocols and sequencesProtocol based scann<strong>in</strong>g can be difficult<strong>in</strong> present<strong>in</strong>g pediatric patients, as therequired sequences differ dramaticallydepend<strong>in</strong>g upon pathology, patient age,compliance, and the cl<strong>in</strong>ical questionsbe<strong>in</strong>g asked. It is often necessary <strong>for</strong> thetechnologist or radiologist to screen theexam<strong>in</strong>ation as it progresses and tailorthe sequences <strong>for</strong> the patient and pathology.A wide field-of-view scan can behelpful to obta<strong>in</strong> an overview to screen<strong>for</strong> other pathologies, particularly <strong>in</strong>children who are difficult to exam<strong>in</strong>ecl<strong>in</strong>ically. <strong>Children</strong> can be unpredictable<strong>in</strong> how long they will rema<strong>in</strong> still, so itis important to prioritize sequences withthe highest diagnostic yield such as T2,FLAIR, and diffusion. Scann<strong>in</strong>g <strong>in</strong> multipleplanes or us<strong>in</strong>g 3D sequences canhelp del<strong>in</strong>eate disorders as well as m<strong>in</strong>imizethe chance of pathology be<strong>in</strong>gmissed through partial volum<strong>in</strong>g or <strong>in</strong>terslicegap.Often it is necessary to modify a protocolor sequence when imag<strong>in</strong>g childrenof different sizes or capabilities. It isimportant to strike a balance betweenoptimum image resolution and scan time.MAGNETOM Flash · 2/2011 · www.siemens.com/magnetom-world 9
How-I-do-it4A4B4C4D4 Images of a 3-month-old child with a lipomatous tether of thesp<strong>in</strong>al cord. The patient was scanned awake <strong>in</strong> a bean bag restra<strong>in</strong>t(4A) us<strong>in</strong>g the 4-channel flex array (4B) positioned flat beneath.The high SNR af<strong>for</strong>ded by this coil allowed high resolution th<strong>in</strong> sliceimag<strong>in</strong>g and the addition of iPAT to reduce scan time. <strong>Siemens</strong> Timarchitecture allows flexibility to use coils <strong>in</strong> a number of orientations,or <strong>in</strong> comb<strong>in</strong>ation with other coils, vital <strong>for</strong> imag<strong>in</strong>g pediatricanatomy.10 MAGNETOM Flash · 2/2011 · www.siemens.com/magnetom-world
How-I-do-itWhen modify<strong>in</strong>g pulse sequences, thefollow<strong>in</strong>g suggestions may be helpful:■ Select pulse sequences that closelymatch the FOV required and the coilbe<strong>in</strong>g used. The less changes you needto make to a sequence, the less chance<strong>for</strong> error.■ Concentrate on ma<strong>in</strong>ta<strong>in</strong><strong>in</strong>g voxel sizeand signal-to-noise when chang<strong>in</strong>gfield-of-view or matrix size, and considerus<strong>in</strong>g <strong>in</strong>terpolation to ma<strong>in</strong>ta<strong>in</strong> signaland resolution. The day optimiz<strong>in</strong>gthroughput (Dot) eng<strong>in</strong>es on the newer<strong>Siemens</strong> scanners can be used to automatemany of these decisions.■ Utilize recovery pulses, where available,to achieve reduction <strong>in</strong> TR timesand to collect the images <strong>in</strong> multipleconcatenations. When comb<strong>in</strong>ed with<strong>in</strong>terleav<strong>in</strong>g this dramatically reducesthe chance of crosstalk when us<strong>in</strong>gm<strong>in</strong>imal slice gaps.■ Use the shortest TE that will ma<strong>in</strong>ta<strong>in</strong>image contrast to boost signal andreduce image blur.Scann<strong>in</strong>g techniquesCoil selectionNovel uses of MR coils are possible andoften necessary <strong>in</strong> pediatric imag<strong>in</strong>g.Choos<strong>in</strong>g a coil that closely matches theFOV you are imag<strong>in</strong>g is important <strong>in</strong>extract<strong>in</strong>g the maximum signal from yourpatients. Use of multichannel arrays isdesirable when available to take advantageof parallel imag<strong>in</strong>g techniques (Fig. 4).Volume imag<strong>in</strong>g3D imag<strong>in</strong>g can be utilized <strong>in</strong> all areas ofthe body. The use of 3D sequences permitsre<strong>for</strong>matt<strong>in</strong>g, which can be helpful5A5B5 Volume imag<strong>in</strong>g: Re<strong>for</strong>matt<strong>in</strong>g of 3D imag<strong>in</strong>g is useful <strong>in</strong> the <strong>in</strong>vestigation of complex congenital conditions. The curved re<strong>for</strong>mat ofthe T1-weighted MPRAGE sequence allows appreciation of the disorganised left cerebral cortex, and helped <strong>in</strong> identification of a region ofpolymicrogyria which was the seizure focus <strong>in</strong> this 12-year-old girl.MAGNETOM Flash · 2/2011 · www.siemens.com/magnetom-world 11
How-I-do-it6A6B6C6D6E6F6 Motion correction <strong>–</strong> syngo BLADE can be used to provide a limited study <strong>in</strong> uncooperative patients (6A, 6B), but is particularly useful <strong>in</strong>imag<strong>in</strong>g posterior fossa lesions <strong>in</strong> pediatric patients where complex and high flow from CSF and vascular structures cause artifacts that mayobscure some lesions (6C, 6D). High parallel imag<strong>in</strong>g factors can also be utilised with multiple excitations to average out motion artifacts(6E None, 6F PAT3).12 MAGNETOM Flash · 2/2011 · www.siemens.com/magnetom-world
How-I-do-it<strong>in</strong> review<strong>in</strong>g and diagnos<strong>in</strong>g complexcongenital conditions, and may reducethe number of 2D sequences per<strong>for</strong>med.It allows <strong>for</strong> high resolution, no gapimag<strong>in</strong>g which can be used to accuratelymeasure lesion size, and monitor changes<strong>in</strong> follow up imag<strong>in</strong>g (Fig. 5).BLADERotat<strong>in</strong>g k-space techniques are utilised<strong>in</strong> pediatric MR imag<strong>in</strong>g to reduce artifactsfrom physiological motion <strong>in</strong> thebra<strong>in</strong>, as well as other body areas suchas the shoulder, chest, abdomen, andpelvis. It is particularly useful withyounger patients scanned at 3T wherecomplex and turbulent flow artifacts canmask pathology [11]. Recent studiesshow improvement <strong>in</strong> lesion conspicuity<strong>in</strong> the posterior fossa through reduction<strong>in</strong> pulsation artifacts [12]. Disadvantagesof BLADE <strong>in</strong>clude <strong>in</strong>creased scantime, altered image contrast, <strong>in</strong>creasedSAR, and reduction <strong>in</strong> sensitivity to somepathology, particularly haemorrhage[13]. Motion reduction with propellersequences can be utilized to obta<strong>in</strong> limiteddiagnostic <strong>in</strong><strong>for</strong>mation <strong>in</strong> mov<strong>in</strong>gpatients; however, their limitationsrestrict widespread use <strong>for</strong> correct<strong>in</strong>gvoluntary patient motion <strong>in</strong> pediatricpatients (Fig. 6).Parallel imag<strong>in</strong>gThe advent of parallel imag<strong>in</strong>g techniquesand multiple element, phasedarray coils has trans<strong>for</strong>med pediatricimag<strong>in</strong>g <strong>in</strong> recent years, provid<strong>in</strong>g aboost <strong>in</strong> either signal or speed. Parallelimag<strong>in</strong>g techniques comb<strong>in</strong>e signalsfrom several coil elements to produce animage with <strong>in</strong>creased SNR, or allow partialsampl<strong>in</strong>g to reduce scan time. Theuse of parallel image acceleration andmultiple acquisitions can be used to averagemotion artifacts <strong>in</strong> pediatric imag<strong>in</strong>g.Parallel imag<strong>in</strong>g techniques can alsobe exploited to reduce the duration ofbreathhold imag<strong>in</strong>g, allow<strong>in</strong>g dynamiccapture of fast mov<strong>in</strong>g pediatricanatomy. Parallel imag<strong>in</strong>g also reduces<strong>in</strong>homogeneity artifacts such as seen <strong>in</strong>diffusion-weighted imag<strong>in</strong>g [14].Time resolved angiographyWhen imag<strong>in</strong>g arterio-venous mal<strong>for</strong>mationsand vascular shunts it is important<strong>for</strong> treatment and management to identifyfeeder vessels as well as the directionof blood flow. Rapid heart rates and highflow rates <strong>in</strong> children often make imag<strong>in</strong>gof complex vasculature difficult withtraditional MR angiography techniques.Time resolved contrast-enhanced MRangiography (MRA) techniques can provideanatomical as well as functionalassessment of these vascular conditions[14].High field strengthimag<strong>in</strong>g (3T)Higher field strengths offer the opportunityto address many of the difficultiesencountered with pediatric MR imag<strong>in</strong>g.The <strong>in</strong>creased SNR allows <strong>for</strong> smaller voxelsand <strong>in</strong>creased resolution, or reducedaverages <strong>for</strong> <strong>in</strong>creased speed. Parallelimag<strong>in</strong>g factors can be <strong>in</strong>creased furtherreduc<strong>in</strong>g scan time. Prolonged T1 timesfacilitate better background suppression<strong>for</strong> MRA and improved visualization ofparamagnetic contrast agents [5]. Theadvantages offered by higher fieldstrengths have lead to the viability ofseveral new techniques <strong>in</strong> pediatric <strong>MRI</strong>.Un<strong>for</strong>tunately, higher field strengthscan also present a number of challenges.The <strong>in</strong>creased field strength leads togreater RF deposition, result<strong>in</strong>g <strong>in</strong><strong>in</strong>creased heat<strong>in</strong>g (SAR), which can causesequence limitation <strong>in</strong> pediatric imag<strong>in</strong>g.B 1 -field <strong>in</strong>homogeneities, chemicalshift, motion artifacts and susceptibilityartifacts are more pronounced at higherfield strengths. However, there are anumber of new techniques, which offerpotential to mitigate aga<strong>in</strong>st these difficulties.Prolonged T1 relaxation at higherfield strengths creates challenges <strong>in</strong>image contrast, particularly <strong>in</strong> the neonatalbra<strong>in</strong> [5].Emerg<strong>in</strong>g techniques<strong>in</strong> pediatric <strong>MRI</strong>SWISusceptibility-weighted imag<strong>in</strong>g is be<strong>in</strong>g<strong>in</strong>creas<strong>in</strong>gly utilized <strong>in</strong> pediatric patients<strong>for</strong> imag<strong>in</strong>g trauma, vascular disease suchas haemorrhage, telangiectasia, and cavernousand venous angiomas, tumors andepilepsy imag<strong>in</strong>g, as well as <strong>in</strong>vestigat<strong>in</strong>gmetabolic disorders (Figs. 7, 8). The useof the phase images can be used to differentiatecalcification from haemhorrage <strong>in</strong>lesions [15].Parallel transmit technologyThe use of multiple coil elements totransmit part of the RF pulse results <strong>in</strong>shorter pulse durations, reductions <strong>in</strong>SAR, and corrections of patient-related<strong>in</strong>homogeneities [16]. This addressessome major challenges of pediatric <strong>MRI</strong>,particularly at higher field strengths.Diffusion Tensor Imag<strong>in</strong>gDTI has provided <strong>in</strong>sights <strong>in</strong>to connectivityand plasticity <strong>in</strong> the develop<strong>in</strong>g bra<strong>in</strong>.It is now enter<strong>in</strong>g the cl<strong>in</strong>ical realm <strong>in</strong>the assessment of traumatic bra<strong>in</strong> <strong>in</strong>jury,epilepsy and white matter disease [14].Arterial Sp<strong>in</strong> Label<strong>in</strong>gASL provides functional <strong>in</strong><strong>for</strong>mation ofblood perfusion by magnetically tagg<strong>in</strong>g<strong>in</strong>flow<strong>in</strong>g blood upstream from the regionof <strong>in</strong>terest. Persistence of the ‘tag’ limitsits use <strong>in</strong> adults; however, this is of lessconcern <strong>in</strong> pediatric patients, due to fastflows and relatively short perfusion distances[5]. This technique offers thepotential to <strong>in</strong>vestigate regions of hypoandhyper-perfusion, <strong>in</strong> conditions suchas stroke or tumors, without the use of<strong>in</strong>travenous contrast media; however,further validation is required to demonstratethe cl<strong>in</strong>ical utility of this technique<strong>in</strong> pediatric patients [17].MR urographyMagnetic resonance urography providesboth anatomical and functional assessmentof the kidneys and ur<strong>in</strong>ary collect<strong>in</strong>gsystem. The multi-planar capabilitiesMAGNETOM Flash · 2/2011 · www.siemens.com/magnetom-world 13
How-I-do-it7A7B7 Images of a 1-month-old who presented with acute seizures. T2w, T1w and diffusion-weighted imag<strong>in</strong>g were unremarkable. Susceptibilityweightedimag<strong>in</strong>g (7A) shows <strong>in</strong>creased venous dra<strong>in</strong>age <strong>in</strong> the right temporal-parietal region. (7B) The same patient imaged 48 hours later afterseizure control with phenobarbital show<strong>in</strong>g normalization of the cerebral flow. The sensitivity of syngo SWI is be<strong>in</strong>g <strong>in</strong>creas<strong>in</strong>gly utilized <strong>in</strong> thepediatric population.8A8B8 Venous angioma as imaged on syngo SWI (8A) and T2w sequences (8B). The ability to obta<strong>in</strong> this level of detail has allowed us to reduce ourreliance on <strong>in</strong>travenous contrast agents to del<strong>in</strong>eate these lesions.14 MAGNETOM Flash · 2/2011 · www.siemens.com/magnetom-world
How-I-do-it9A9B9C9D9 These images are of a patient with a p<strong>in</strong>eal cyst caus<strong>in</strong>g obstruction of the cerebral aqueduct with associated enlargement of the lateral andthird ventricles. The sensitivity to flow of the T2w SPACE sequence can be used to demonstrate the obstruction <strong>in</strong> the pre surgical images (9A)as well as the <strong>in</strong>creased retrograde flow through the <strong>for</strong>amen of Monro. The post surgical image (9B) shows the reduction <strong>in</strong> the size of the cystas well as the restored flow to the cerebral aqueduct. The 3D sequence can be easily re<strong>for</strong>matted to show the site of the fenestration of the thirdventricle (9C, 9D arrows). Third ventricultomies have been traditionally difficult to demonstrate with standard 2D and phase contrast imag<strong>in</strong>g,however, with a s<strong>in</strong>gle 3D acquisition we can now easily answer all of the questions of the neurosurgeon.MAGNETOM Flash · 2/2011 · www.siemens.com/magnetom-world 15
How-I-do-itof <strong>MRI</strong> are ideal <strong>for</strong> display<strong>in</strong>g complexcongenital anomalies of the genitour<strong>in</strong>arytract. This <strong>in</strong><strong>for</strong>mation can beused to predict outcome and selectpatients that are most likely to benefitfrom surgical <strong>in</strong>tervention [18].MR enterographyCrohn’s disease is a serious and lifelongcondition affect<strong>in</strong>g the digestive system.It affects primarily the ileum and coloncaus<strong>in</strong>g <strong>in</strong>flammation, ulceration andcan lead to abscess <strong>for</strong>mation or fistulaeto other organs. Approximately 30% ofpatients with Crohn’s disease will presentbe<strong>for</strong>e the age of 20. <strong>MRI</strong> providesthe ability to diagnose and monitor thiscondition as well as complications suchas peri-anal fistulae without expos<strong>in</strong>gthe patient to radiation [19].ConclusionMagnetic resonance imag<strong>in</strong>g referrals<strong>for</strong> children cont<strong>in</strong>ue to rise. The lack ofioniz<strong>in</strong>g radiation coupled with the highlevel of detail af<strong>for</strong>ded by MR imag<strong>in</strong>ghas made it the exam<strong>in</strong>ation of choice <strong>for</strong>a grow<strong>in</strong>g number of pediatric presentations.Most children who require magneticresonance imag<strong>in</strong>g will be exam<strong>in</strong>ed<strong>in</strong> specialist pediatric centers or hospitals;however, heightened pressure onspecialist centers has lead to many childrenbe<strong>in</strong>g scanned <strong>in</strong> non-specialistfacilities where technologists may havelittle experience <strong>in</strong> pediatric imag<strong>in</strong>g.These referrals need to be treated differentlyto standard adult imag<strong>in</strong>g requests<strong>in</strong> order to ensure diagnostic imag<strong>in</strong>gwith m<strong>in</strong>imal distress and <strong>in</strong>terventionto the patient. There is no ‘one size fitsall’ approach to imag<strong>in</strong>g children andpediatric <strong>MRI</strong> requires dedicated specialistknowledge, flexibility, and expert<strong>in</strong>put from the technologist. An awarenessof the challenges <strong>in</strong> pediatric <strong>MRI</strong>and experience <strong>in</strong> pediatric imag<strong>in</strong>gtechniques is vital to successful exam<strong>in</strong>ation<strong>in</strong> this population. <strong>MRI</strong> <strong>in</strong> childrencan be extremely challeng<strong>in</strong>g physically,mentally, and emotionally, even <strong>for</strong> aseasoned pediatric technologist; however,these very challenges are also what makepediatric imag<strong>in</strong>g such an <strong>in</strong>terest<strong>in</strong>gand reward<strong>in</strong>g field <strong>for</strong> MR technologists.AcknowledgmentsI would like to thank the patients andstaff of the Royal <strong>Children</strong>’s Hospital,Melbourne, <strong>for</strong> their <strong>in</strong>spiration, advice,and support <strong>in</strong> compil<strong>in</strong>g this paper.References1 Machata AM, Willshke H, Kaban B, Prayer D,Marhofer P (2009) “ Effect of Bra<strong>in</strong> <strong>MRI</strong> on BodyCore Temperature <strong>in</strong> Sedated Infants and <strong>Children</strong>”British Journal of Anaesthesia 102(3):385-9.2 Cohen MM, Cameron Cal B, Duncan PG (1990)“<strong>Pediatric</strong> Anesthesia Morbidity and Mortality<strong>in</strong> the Perioperative Period” Anesthesia andAnalgesia 70”160-7.3 Homman H, Bornert P, Eggers H, Nehrke K, DosselO, Graessl<strong>in</strong> I (2011) “Toward <strong>in</strong>dividualised SARmodels and <strong>in</strong> vivo validation” Magnetic resonance<strong>in</strong> Medic<strong>in</strong>e doi: 10.1002/mrm.22948.4 Seraf<strong>in</strong>i G, Ongaro C, Mori A, Rossi C, Cavalloro F,Tagliaferri C, Mencher<strong>in</strong>i S, Braschi A (2005)“Anesthesia <strong>for</strong> <strong>MRI</strong> <strong>in</strong> the <strong>Pediatric</strong> Patient”M<strong>in</strong>erva Anesthesiology Jun 71(6) 361-6.5 Dagia C, Ditchfield M. (2008) “3T <strong>MRI</strong> <strong>in</strong>paediatrics: Challenges and cl<strong>in</strong>ical applications”European Journal of Radiology doi:10.1016/j.ejrad.2008.05.019.6 Hussa<strong>in</strong> HM, Barnes CE (2007) “<strong>Pediatric</strong> skeletaltrauma- Pla<strong>in</strong> film to <strong>MRI</strong>” Applied Radiology36(8):24-33.7 Carter AJ, Greer ML, Gray SE, Ware, RS (2010)“Mock <strong>MRI</strong>: reduc<strong>in</strong>g the need <strong>for</strong> anaesthesia <strong>in</strong>children” <strong>Pediatric</strong> Radiology Aug;40(8):1368-74.8 de Amorim e Silva,C.T.J., Mackenzie,A.,Hallowell,L.M., Stewart, S.E., Ditchfield, M.R.(2006) “Practice <strong>MRI</strong>: Reduc<strong>in</strong>g the need <strong>for</strong> sedationand general anaesthesia <strong>in</strong> children undergo<strong>in</strong>g<strong>MRI</strong>” Australasian Radiology 50(4),319-323.9 Hallowell, L.M., Stewart, S.E., de Amorim e Silva,C.T., Ditchfield, M.R. (2008) “Review<strong>in</strong>g theprocess of prepar<strong>in</strong>g children <strong>for</strong> <strong>MRI</strong>” <strong>Pediatric</strong>Radiology 38(3), 271-279.10 Gable S (2010) “Communicat<strong>in</strong>g effectivelywith children” University of Missouri, Columbia,Outreach and Extension <strong>in</strong><strong>for</strong>mation sheet.11 Vert<strong>in</strong>sky AT, et al. (2009) “Per<strong>for</strong>mance ofPROPELLER relative to standard FSE T2-weightedimag<strong>in</strong>g <strong>in</strong> pediatric bra<strong>in</strong> <strong>MRI</strong>” <strong>Pediatric</strong>Radiology. Oct;39(10):1038-47.12 Von Kalle T, et al. (2010) “Diagnostic RelevantReduction of Motion Artifacts <strong>in</strong> the PosteriorFossa by syngo BLADE Imag<strong>in</strong>g” MAGNETOMFlash 43(1/2010):6-11.13 Forbes KP, et al. (2003) “Bra<strong>in</strong> Imag<strong>in</strong>g <strong>in</strong> theUnsedated <strong>Pediatric</strong> Patient: Comparison ofPeriodically Rotated Overlapp<strong>in</strong>g Parallel L<strong>in</strong>eswith Enhanced Reconstruction and S<strong>in</strong>gle-ShotFast Sp<strong>in</strong>-Echo Sequences” American Journal ofNeuroradiology 24:794-798.14 Shenoy-Bangle A, Nimk<strong>in</strong> K, Gee MS (2010)“<strong>Pediatric</strong> Imag<strong>in</strong>g: Current and EmergentTrends” Journal of Postgrad Medic<strong>in</strong>e 56:98-102.15 Zhen Wu, Sandeep Mittal, Karl Kish, Y<strong>in</strong>gjian Yu,J. Hu, Mark Haake (2009) “Identification of Calcificationwith Magnetic Resonance Imag<strong>in</strong>g Us<strong>in</strong>gSusceptibility-Weighted Imag<strong>in</strong>g: A Case Study”Journal of Magnetic Resonance Imag<strong>in</strong>g 29(1):177-182.16 Wald LL, Adalste<strong>in</strong>sson E (2009) “Parallel TransmitTechnology <strong>for</strong> High Field <strong>MRI</strong>” MAGNETOMFlash 40(1/2009):124-135.17 Chen J, et al. (2009) “Arterial Sp<strong>in</strong> Labell<strong>in</strong>gPerfusion <strong>MRI</strong> <strong>in</strong> <strong>Pediatric</strong> Arterial IschemicStroke- Initial Experiences” Journal of MagneticResonance Imag<strong>in</strong>g February; 29(2) 282-290.18 Grattan-Smith JD, Jones R (2008) “Magneticresonance urography <strong>in</strong> <strong>Children</strong>” MagneticResonance Imag<strong>in</strong>g Cl<strong>in</strong>ics of North America16 515-531.19 S<strong>in</strong>ha R (2009) “Role of <strong>MRI</strong> <strong>in</strong> Chron’s disease”Cl<strong>in</strong>ical Radiology 64 (4):341-352.ContactGlenn CahoonRoyal <strong>Children</strong>’s HospitalMelbourneAustraliaGlenn.Cahoon@rch.org.au*MR scann<strong>in</strong>g has not been established as safe <strong>for</strong>imag<strong>in</strong>g fetuses and <strong>in</strong>fants under two years of age.The responsible physician must evaluate the benefitof the <strong>MRI</strong> exam<strong>in</strong>ation <strong>in</strong> comparison to otherimag<strong>in</strong>g procedures.16 MAGNETOM Flash · 2/2011 · www.siemens.com/magnetom-world





![WalkAway plus Technical Specifications [41 KB] - Siemens Healthcare](https://img.yumpu.com/51018135/1/190x253/walkaway-plus-technical-specifications-41-kb-siemens-healthcare.jpg?quality=85)