PRE-SEDATION EVALUATION FORM (DRAFT) - Mission Health
PRE-SEDATION EVALUATION FORM (DRAFT) - Mission Health
PRE-SEDATION EVALUATION FORM (DRAFT) - Mission Health
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
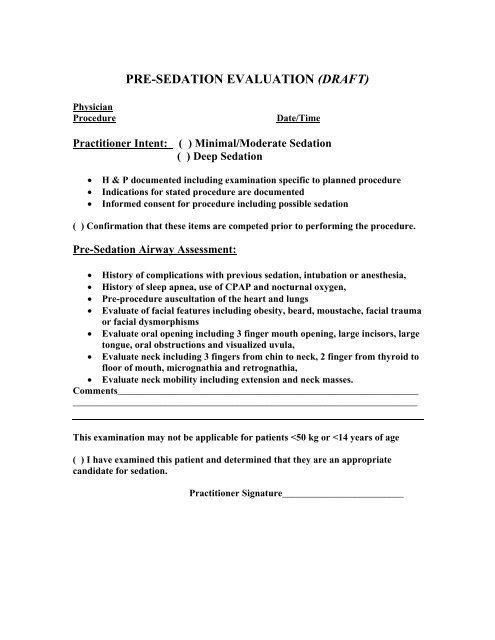
<strong>PRE</strong>-<strong>SEDATION</strong> <strong>EVALUATION</strong> (<strong>DRAFT</strong>)PhysicianProcedureDate/TimePractitioner Intent: ( ) Minimal/Moderate Sedation( ) Deep SedationH & P documented including examination specific to planned procedureIndications for stated procedure are documentedInformed consent for procedure including possible sedation( ) Confirmation that these items are competed prior to performing the procedure.Pre-Sedation Airway Assessment: History of complications with previous sedation, intubation or anesthesia, History of sleep apnea, use of CPAP and nocturnal oxygen, Pre-procedure auscultation of the heart and lungs Evaluate of facial features including obesity, beard, moustache, facial traumaor facial dysmorphisms Evaluate oral opening including 3 finger mouth opening, large incisors, largetongue, oral obstructions and visualized uvula, Evaluate neck including 3 fingers from chin to neck, 2 finger from thyroid tofloor of mouth, micrognathia and retrognathia, Evaluate neck mobility including extension and neck masses.Comments_____________________________________________________________________________________________________________________________________This examination may not be applicable for patients
Administrative Policy and Procedure Policy Number: 300.005Subject: Sedation Page: 1 Of: 9Effective: March 3, 1997Revised:Approved:.<strong>DRAFT</strong> 11/19/09after meetingDeleted: Signed by Kathy Guyette, VPand Chief Nursing Officer, 3/24/2009,and original filed in Administration.Deleted: March 24, 2009Deleted: Signed by Alan Baumgarten,Chief of Staff, 3/24/2009PURPOSE:This policy seeks to establish minimum requirements for administering and monitoring sedation forall patients throughout <strong>Mission</strong> Hospitals. This Administrative Policy of <strong>Mission</strong> <strong>Health</strong> System,Inc. ("<strong>Mission</strong>") is applicable to <strong>Mission</strong> Hospitals, Memorial and St. Joseph campuses, the AshevilleSurgery Center and other locations where services of the hospital are being provided. Site specificsedation guidelines may be more, but not less restrictive than the hospital guidelines, and mustconform to requirements that patients with the same health status receive a comparable level of carethroughout <strong>Mission</strong> Hospitals. These standards are intended for patients undergoing a diagnostic ortherapeutic procedure. This policy is applicable to all patients undergoing procedures with the intentto receive sedation.DEFINITIONS:1. Minimal Sedation (Anxiolysis)A drug-induced state during which patients respond normally to verbal commands. Althoughcognitive function and coordination may be impaired, ventilatory and cardiovascular functionsare unaffected.2. Moderate Sedation/Analgesia (Conscious Sedation)A drug-induced depression of consciousness during which patients respond purposefully toverbal commands, either alone or accompanied by light tactile stimulation. No interventions arerequired to maintain a patent airway, and spontaneous ventilation is adequate. Cardiovascularfunction is usually maintained.Deleted: Minimal Sedation (Deleted: )Deleted: Although cognitive functionand coordination may be impaired,ventilatory and cardiovascular functionsare unaffected.Minimal Sedation3. Deep Sedation/AnalgesiaA drug induced depression of consciousness during which patients cannot be easily arousedbut respond purposefully after repeated or painful stimulation. The ability to independentlymaintain ventilatory function may be impaired. Patients may require assistance in maintaininga patent airway and spontaneous ventilation may be inadequate. Cardiovascular function
Policy #300.005 – Sedation Page 2 of 7is usually maintained.4. AnesthesiaConsists of general anesthesia and spinal or major regional anesthesia. It does not includelocal anesthesia. General anesthesia is a drug induced loss of consciousness during whichpatients are not arousable, even by painful stimulation. The ability to independently maintainventilatory function is often impaired. Patients often require assistance in maintaining apatent airway, and positive pressure ventilation may be required because of depressedspontaneous ventilation or drug induced depression of neuromuscular function. Cardiovascularfunction may be impaired.5. ProceduralistThe person qualified to perform the procedure. This person may be a physician, midlevelprovider, or others privileged to perform an invasive procedure or may be a technologistor other personnel qualified to perform the procedure for noninvasive procedures such aschest radiographs, nuclear medicine scans, ultrasound examinations, or MRI’s.6. SedationistThe physician or advanced practitioner privileged to perform the sedation.7. MonitorA person qualified to monitor and respond appropriately to the patient's responseto medication and assist in any supportive or resuscitative measures required. Themonitor will not engage in any tasks that would compromise continuous patientmonitoring.SCOPE:1. This policy applies to patients who receive drugs with the intent of sedation/analgesiafor procedures. This policy does not apply to mediations given for anticonvulsant effects,minimal sedation (anxiolysis) without an intended procedure or pain control; however,should any such agents be given and followed by deeper levels of sedation (moderatesedation), appropriate monitoring/interventions in keeping with this policy should beimmediately instituted.2. This policy is not intended to address situations in which an anesthesiologist or nurseanesthetist is engaged in the administration of anesthesia/sedation.Deleted: EXCLUSIONSFormatted: Font: 12 ptFormatted: Font: 12 ptFormatted: Font: 12 ptFormatted: Font: 12 ptFormatted: Font: 12 ptFormatted: Font: 12 ptFormatted: Font: 12 ptFormatted: No underlineFormatted: Bullets and Numbering3 This policy does not apply to sedation used to secure an airway, for ventilatory management, forpain control, or when sedation is used as chemical restraint in the psychiatric patient.LOCATION:Moderate Sedation may be administered in the following primary locations: Emergency Department,Intensive Care Units, Operating Rooms, Asheville Surgery Center, Radiology Department, CardiacCath Lab, Echo Lab, Endoscopy Department including mobile endoscopy, and Pediatrics, PediatricOutpatient, Pediatric Adolescent Unit, Pediatric Intensive Care Unit, Neonatal Intensive Care Unit
Policy #300.005 – Sedation Page 3 of 7and Trauma Care Unit.Secondary locations may be used when the personnel and equipment needed to perform moderatesedation (as outlined in this policy) are present.Deep Sedation may be administered in adult and pediatric Intensive Care Units, Neonatal IntensiveCare Unit, Pediatric Outpatient, Trauma Care Unit, Cardiac Cath Lab, Radiology, and in theEmergency Department.PRIVILEGING AND SKILL COMPETENCY:Practitioners responsible for the administration of moderate and deep sedation will be privilegedthrough the Medical Staff Credentials Committee. This committee, in consultation withAnesthesiology Clinical Services, establishes the credentialing process and criteria.The RN monitoring the patient during procedures requiring moderate sedation will have BLScertification and will demonstrate satisfactory completion of the sedation learning module.The RN monitoring the patient during procedures requiring deep sedation will have ACLScertification and will demonstrate satisfactory completion of the sedation learning module.The person monitoring the pediatric patients during procedures requiring moderate or deepsedation will be a Pediatric Advanced Life Support (PALS) and/or Emergency Nurse PediatricCourse (ENPC) certified RN and will demonstrate successful completion of the pediatricsedation learning module.PATIENT SELECTION:1. The need for any short term, therapeutic, diagnostic, or surgical procedure and subsequentuse of sedation will remain under the individual practitioner's practice direction.2. There must be a documented pre-sedation evaluation of the patient prior to any shortterm therapeutic, diagnostic, or surgical procedure requiring sedation.A. Pre-Sedation Evaluation to include:1. A medical history and physical examination that should include an examinationspecific to procedure being performed2. Indications for the stated procedure,3. Confirmation of informed consent including possible sedation,4. A Pre-Sedation Airway assessment documenting,a. History of complications with previous sedation, intubation or anesthesia,b. History of sleep apnea, use of CPAP and nocturnal oxygen,c. Pre-procedure auscultation of heart and lungs,d. Facial features that could indicate difficulty with oxygen mask includingobesity, beard , moustache, facial trauma, and facial dysmophisms,e. Oral opening including three finger mouth opening, large incisors, largetongue, oral obstructions and visualized uvula,f. Neck size and shape including 3 fingers from chin to neck, 2 fingers fromDeleted: procedureDeleted: moderate or deepFormatted: Bullets and NumberingDeleted: AFormatted: Indent: Left: 54 ptDeleted: must be performed anddocumented in the medical recordprior to procedure or sedation. Minimalcontent required includes:Deleted: EDeleted: Deleted: .Formatted: Indent: Left: 36 pt,First line: 18 ptDeleted: /symptomsDeleted: Formatted: Numbered + Level: 1 +Numbering Style: a, b, c, … + Startat: 1 + Alignment: Left + Aligned at:72 pt + Tab after: 90 pt + Indentat: 90 pt
Policy #300.005 – Sedation Page 4 of 7thyroid to floor of mouth, micrognathia and retrognathia,g. Neck mobility including ability to extend and neck masses.B. There is to be a reevaluation immediately prior to administration of intravenousmedications to determine that the patient is at this time an appropriate candidate forsedation.3. Practitioners are encouraged to consult with a member of the Anesthesiology ClinicalService when there is a question regarding the appropriate delivery of sedation.IN<strong>FORM</strong>ED CONSENT:Informed consent for any short term therapeutic, diagnostic or surgical procedure in whichmoderate or deep sedation is to be employed will be signed, dated, and timed and will include therisks/benefits/alternatives of sedation as appropriate. The informed consent should read"(Procedure) with sedation".MANAGEMENT:Minimal/Moderate Sedation1. The minimum number of personnel for employing moderate sedation shall be two.• The Proceduralist is the person qualified to perform the procedure.• The Sedationist is the physician or advanced practitioner privileged to performmoderate sedation. The Sedationist selects and orders the medications to producesedation.• If the Proceduralist is also the Sedationist, then a monitor is needed.• If the Sedationist is not the Proceduralist, then a monitor is not necessary.• The monitor is the person qualified to monitor and respond appropriately to thepatient’s response to medication and assist in any supportive or resuscitativemeasures required. The monitor will not engage in any tasks that wouldcompromise continuous patient monitoring.• The Sedationist and the monitor will be available to the patient from the time ofadministration of sedation until recovery or until the care of the patient istransferred to personnel performing recovery care.2. The following minimum equipment must be present and ready for use in the room wheremoderate sedation is being administered.A. Oxygen.B. Suction.C. Emergency airway equipment.D. Cardiac monitor if indicated by practitioner.E. Noninvasive blood pressure monitor or manual blood pressure cuff applied.F. Pulse oximeter applied with audible variable pitch pulse tone and low threshold alarm.G. Code cart with defibrillator must be located in close proximity to theprocedure/sedation area.H. Reversal agents.Deleted: .Auscultation of heart and lungs.Deleted: Airway assessmentPrevious anesthesia/sedation history.Formatted: Indent: Left: 0 ptDeleted: Components of airwayassessment include relevant history and aphysical exam, including habitus andfeatures of the head and neck, mouth, andjaw. Factors which may be associatedwith difficulty in airway managementinclude:History of difficult intubation, sleepapnea, or advanced rheumatoid arthritis.Obesity or dysmorphic facialfeatures.Short neck, limited neck extension, orneck masses.Small oral opening or nonvisibleuvula.Micrognathia or retrognathiaDeleted: diagnostic,Deleted: Minimal Sedation(Anxiolyxis).The practitioner selects and orders themedication. The use of intravenousVersed is considered at least minimalsedation.Obtain vital signs to include bloodpressure, pulse, respirations, and oxygensaturation prior to the administration ofmedication for minimal sedation. A RNmonitor will continuously monitoroxygen saturation and document vitalsigns and the patient's response tomedication. Documentation will occurevery fifteen (15) minutes during theprocedure, at the end of the procedure,and one hour following procedure or untilthe patient meets discharge criteria.Formatted: Bullets and Numbering
Policy #300.005 – Sedation Page 5 of 73. All patients receiving IV moderate sedation must have a patent IV with continuousadministration of IV fluids per practitioner order. Patent saline or heparin locks (INTs) areacceptable for patients with contraindications to IV fluids. IV fluid for resuscitation should bereadily available. The need for IV access in patients receiving sedation by any other route ofadministration shall be determined by the practitioner.4. The patient's NPO status will be assessed. The recommended guidelines for nonurgent/nonemergent procedures is the patient be NPO for a minimum of two (2) hours for clearliquids, six (6) hours for light meal (nonfat, nonmeat, example: toast), and eight (8) hoursfor other solid food. Infants may have breast milk up to four (4) hours or infant formulaup to six (6) hours prior to procedure.Deep Sedation.1. The minimum number of personnel for employing deep sedation shall be two.• The Proceduralist is the person qualified to perform the procedure.• The Sedationist is the physician privileged to perform deep sedation. TheSedationist selects and orders the medications required for deep sedation.• If the Proceduralist is also the Sedationist, then a monitor must be present.• If the Sedationist is not the Proceduralist, then no monitor is required.• The monitor is the person competent to monitor and respond appropriately to thepatient’s response to medication and assist in any supportive or resuscitativemeasures required. The monitor will not engage in any tasks that wouldcompromise continuous patient monitoring.• The Sedationist and the monitor will be available to the patient from the time ofadministration of sedation until recovery or until the care of the patient istransferred to personnel performing recovery care.When Propofol is being administered for deep sedation, the minimum number of personnelshall be three.If the Sedationist is not the Proceduralist, then one additional monitor is required.The monitor is the person competent to monitor and respond appropriately to thepatient’s response to medication and assist in any supportive or resuscitativemeasures required. The monitor will not engage in any tasks that wouldcompromise continuous patient monitoring. If the Sedationist is also the Proceduralist, then two additional persons arerequired.One monitor is the person competent to monitor and respond appropriately to thepatient’s response to medication and assist in any supportive or resuscitativemeasures required. The monitor will not engage in any tasks that wouldcompromise continuous patient monitoring.A second monitor capable of assistance in maintaining a patent airway andsupporting respirations in case ventilatory function is impaired. The secondmonitor may be another physician or may be a respiratory therapist.2. The following minimum equipment must be available for use where deep sedation is beingadministered.A. Oxygen.
Policy #300.005 – Sedation Page 6 of 7B. Suction.C. Emergency airway equipment.D. Cardiac monitor applied.E. Noninvasive blood pressure monitor or manual blood pressure cuff applied.F. Pulse oximeter applied with audible variable pitch pulse tone and low threshold alarm.G. Code cart with defibrillator must be located in close proximity to theprocedure/sedation area.H. Reversal agents.Formatted: Bullets and NumberingFormatted: Bullets and Numbering3. All patients receiving IV deep sedation must have a patent IV with continuousadministration of IV fluids per practitioner order. Patent saline or heparin locks (INTs) areacceptable for patients with contraindications to IV fluids. IV fluid for resuscitation shouldbe readily available. The need for IV access in patients receiving sedation by any otherroute of administration shall be determined by the practitioner.4. The patient's NPO status will be assessed. The recommended guidelines fornonurgent/non emergent procedures is the patient be NPO for a minimum of two (2)hours for clear liquids, six (6) hours for light meal (nonfat, nonmeat, example: toast),and eight (8) hours for other solid food. Infants may have breast milk up to four (4)hours or infant formula up to six (6) hours prior to procedure.PROCEDURE MANAGEMENT:1. A standardized sedation flow sheet will be completed by the monitor for all patients receivingmoderate or deep sedation.2. Documentation on the sedation flow sheet must include:A. Verification that informed consent is signed.B. Weight.C. NPO status.D. Prior adverse drug reactions including allergies.E. Premedication.F. Beginning and end time of procedure.G. Baseline blood pressure, pulse, respiratory rate, oxygen saturation on room air (unless thepatient is receiving oxygen preprocedure), level of consciousness.H. Name, dose, route, and time of all drugs given.I. Patient response to all medications given.J. Oxygen delivery.K. Type and amount of IV fluids (if administered).L. Any adverse drug reactions or significant responses; management and outcome of theseevents.Formatted: Bullets and NumberingFormatted: Bullets and NumberingFormatted: Bullets and Numbering3. Minimum monitoring will include: blood pressure, pulse, respiratory rate, oxygen saturation,level of consciousness (cardiac monitoring required for deep sedation). Minimum monitoringmust be documented on the flow sheet at least every ten minutes during the procedure for theadult patient; document on the flow sheet at least every five minutes during the procedure for thepediatric patient. When frequent monitoring of blood pressure and pulse interrupt the procedure,those measures will be waived intraprocedure.
Policy #300.005 – Sedation Page 7 of 7POST PROCEDURE MANAGEMENT FOR MODERATE OR DEEP <strong>SEDATION</strong>:1. Patients who receive sedation will be monitored post procedure. They will be consideredrecovered when monitoring shows a return to safe physiological and psychological levels. Anequivalent to the Aldrete Scoring System will be used.Deleted: This flow sheet will be deletedLou2. Any person receiving a reversal agent must be observed for one hour after the last dose ofreversal agent.3. Inpatient monitoring and documentation:A. Blood pressure, pulse, respirations, oxygen saturation, and level of consciousness at leastevery fifteen minutes.B. Observation of any post procedure complications, management of those events, andpatient response.C. Name, dose, time, route and response of any medications given in the post procedureperiod.D. Discharge summary and verbal report to nurse caring for patient on patient care unit.Include pre-procedure vital signs and level of consciousness, any problems encounteredduring or post procedure, total medications given, IV fluid total, and status of IV.4. Outpatient monitoring and documentation:A. Blood pressure, pulse, respiration, oxygen saturation, and level of consciousness at leastevery fifteen minutes.B. Observation of any post procedure complications, management of those events andpatient response.C. Name, dose, time, route and response of any medications given in the post procedureperiod.D. Verbal and written discharge instructions to patient and responsible adult accompanyingpatient and driving them home to include restrictions following sedation.PER<strong>FORM</strong>ANCE IMPROVEMENT:The Chairperson or designee of the Anesthesiology Clinical Service is responsible to oversee themonitoring and evaluation of sedation use. The following data is gathered for review following theadministration of sedation:> Unplanned intubation> Unplanned admission or transfer to higher level of care> Administration of reversal agent> Drop in oxygen saturation to less than 92% not responsive rapidly to oxygen therapy> Nausea and vomiting> Unable to complete procedure> Achieved sedation level deeper than intent> Failure to comply with documentation requirementsCMS: WHAT CONSTITUTES ... [1]
Page 7: [1] Deleted11/18/2009 10:30:00 PMThis flow sheet will be deletedLou
CMS: WHAT CONSTITUTES SURGERY?“For the purposes of determining compliance with the hospital surgical services Conditions ofParticipation (CoP), CMS relies, with minor modification, upon the definition of surgerydeveloped by the American College of Surgeons. Accordingly, the following definition is usedto determine whether or not a procedure constitutes surgery and is subject to this CoP:Surgery is performed for the purpose of structurally altering the human body by theincision or destruction of tissues and is part of the practice of medicine. Surgery also is thediagnostic or therapeutic treatment of conditions or disease processes by any instrumentscausing localized alteration or transposition of live human tissue which include lasers,ultrasound, ionizing radiation, scalpels, probes, and needles. The tissue can be cut, burned,vaporized, frozen, sutured, probed, or manipulated by closed reductions for major dislocationsor fractures, or otherwise altered by mechanical, thermal, light-based, electromagnetic, orchemical means. Injection of diagnostic or therapeutic substances into body cavities, internalorgans, joints, sensory organs, and the central nervous system also is considered to besurgery (this does not include the administration by nursing personnel of some injections,subcutaneous, intramuscular, and intravenous, when ordered by a physician). All of thesesurgical procedures are invasive, including those that are performed with lasers, and therisks of any surgical procedure are not eliminated by using a light knife or laser in place of ametal knife, or scalpel. “This definition does not include such things as x-ray examinations, MRI’s, nuclear medicineexaminations, ultrasounds used for examination only, placement of noncentral intravenouscatheters, and other such activities.