2012-09-16
2012-09-16
2012-09-16
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
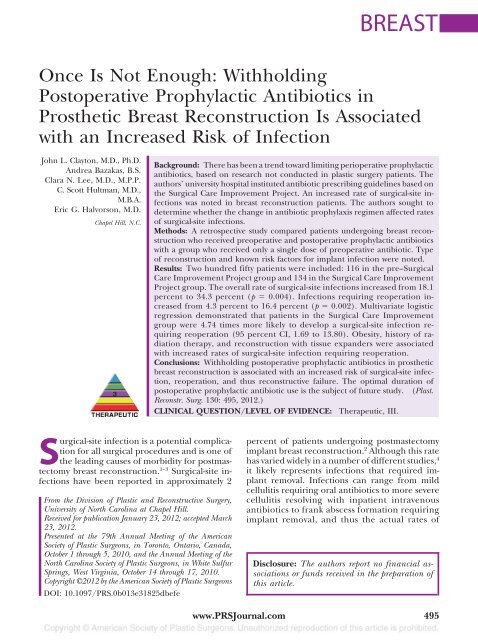
BREASTOnce Is Not Enough: WithholdingPostoperative Prophylactic Antibiotics inProsthetic Breast Reconstruction Is Associatedwith an Increased Risk of InfectionJohn L. Clayton, M.D., Ph.D.Andrea Bazakas, B.S.Clara N. Lee, M.D., M.P.P.C. Scott Hultman, M.D.,M.B.A.Eric G. Halvorson, M.D.Chapel Hill, N.C.Background: There has been a trend toward limiting perioperative prophylacticantibiotics, based on research not conducted in plastic surgery patients. Theauthors’ university hospital instituted antibiotic prescribing guidelines based onthe Surgical Care Improvement Project. An increased rate of surgical-site infectionswas noted in breast reconstruction patients. The authors sought todetermine whether the change in antibiotic prophylaxis regimen affected ratesof surgical-site infections.Methods: A retrospective study compared patients undergoing breast reconstructionwho received preoperative and postoperative prophylactic antibioticswith a group who received only a single dose of preoperative antibiotic. Typeof reconstruction and known risk factors for implant infection were noted.Results: Two hundred fifty patients were included: 1<strong>16</strong> in the pre–SurgicalCare Improvement Project group and 134 in the Surgical Care ImprovementProject group. The overall rate of surgical-site infections increased from 18.1percent to 34.3 percent (p 0.004). Infections requiring reoperation increasedfrom 4.3 percent to <strong>16</strong>.4 percent (p 0.002). Multivariate logisticregression demonstrated that patients in the Surgical Care Improvementgroup were 4.74 times more likely to develop a surgical-site infection requiringreoperation (95 percent CI, 1.69 to 13.80). Obesity, history of radiationtherapy, and reconstruction with tissue expanders were associatedwith increased rates of surgical-site infection requiring reoperation.Conclusions: Withholding postoperative prophylactic antibiotics in prostheticbreast reconstruction is associated with an increased risk of surgical-site infection,reoperation, and thus reconstructive failure. The optimal duration ofpostoperative prophylactic antibiotic use is the subject of future study. (Plast.Reconstr. Surg. 130: 495, <strong>2012</strong>.)CLINICAL QUESTION/LEVEL OF EVIDENCE: Therapeutic, III.Surgical-site infection is a potential complicationfor all surgical procedures and is one ofthe leading causes of morbidity for postmastectomybreast reconstruction. 1–3 Surgical-site infectionshave been reported in approximately 2From the Division of Plastic and Reconstructive Surgery,University of North Carolina at Chapel Hill.Received for publication January 23, <strong>2012</strong>; accepted March23, <strong>2012</strong>.Presented at the 79th Annual Meeting of the AmericanSociety of Plastic Surgeons, in Toronto, Ontario, Canada,October 1 through 5, 2010, and the Annual Meeting of theNorth Carolina Society of Plastic Surgeons, in White SulfurSprings, West Virginia, October 14 through 17, 2010.Copyright ©<strong>2012</strong> by the American Society of Plastic SurgeonsDOI: 10.1<strong>09</strong>7/PRS.0b013e31825dbefepercent of patients undergoing postmastectomyimplant breast reconstruction. 2 Although this ratehas varied widely in a number of different studies, 4it likely represents infections that required implantremoval. Infections can range from mildcellulitis requiring oral antibiotics to more severecellulitis resolving with inpatient intravenousantibiotics to frank abscess formation requiringimplant removal, and thus the actual rates ofDisclosure: The authors report no financial associationsor funds received in the preparation ofthis article.www.PRSJournal.com 495
Volume 130, Number 3 • Antibiotics and Breast ReconstructionCare Improvement Project guidelines, we begancapturing the distribution profile of organismsisolated from women who experienced postoperativeinfection. Bacterial isolates for women requiringremoval of the implant are reported.The majority of patients undergoing breast reconstructionhad mastectomy for curative resection.Other patients underwent prophylactic mastectomyafter positive genetic testing for the BRCAI andBRCAII genes or because of a strong familial historyof breast cancer. In subset analyses, we also examinedthe use of AlloDerm (LifeCell Corp., Branchburg,N.J.) and axillary lymph node dissection, eitherbefore or concurrent with the mastectomy.Sample Size EstimationAlthough the published rate of infection afterimplant reconstruction is approximately 2 percent,this rate likely reflects only cases requiringremoval of the implant. In a pilot study at ourinstitution, patients undergoing implant reconstructionexperienced an increase in the baselineinfection rate from 5.4 percent to 18.2 percentwith the implementation of the Surgical Care ImprovementProject protocol. This study was adequatelypowered to detect a 20 percent differencein the rate of infection between the two groupsstudied. A type I error probability of 5 percent(alpha) and a type II error probability of 10 percent(beta) were used for this calculation. We estimatedan event rate (proportion) of 10 percentin the group treated with preoperative antibioticsonly. The required sample size in each of the twostudy groups was 47 patients, or a total sample sizeof 94 patients.Statistical AnalysesDescriptive statistics, including frequencies forthe independent variables and unadjusted rates ofinfection, are reported. Pearson’s chi-square andFisher’s exact tests were used for categorical variablesand t tests were used for continuous independentvariables. Multivariate logistic regression usinga backward, conditional modeling technique wasused to investigate predictors of surgical-site infectionrequiring reoperation. Values of p 0.05 wereconsidered statistically significant. SPSS version 19(SPSS, Inc., Chicago, Ill.) was used for all analyses.RESULTSA total of 250 women were included for analyses(1<strong>16</strong> in the pre–Surgical Care ImprovementProject group and 134 in the Surgical Care ImprovementProject group). There were no statistically significantdifferences in the mean age of patients,diabetic status, current smoking status, radiationhistory, chemotherapy history, or tumor stage betweenthe two groups (Table 1). The women in theSurgical Care Improvement Project group had aslightly higher body mass index (27.2 versus 28.8;p 0.052). The overall rate of surgical-site infection(treated with any modality) increased from18.1 percent in the pre–Surgical Care ImprovementProject group to 34.3 percent after the adoptionof the Surgical Care Improvement Projecttreatment protocol (p 0.004) (Table 2). No statisticallysignificant differences were noted in therates of surgical-site infection successfully treatedwith oral or intravenous antibiotics alone, but therate of infection requiring reoperation increasedfrom 4.3 percent to <strong>16</strong>.4 percent (p 0.002). Regardingthe different types of reconstruction, theTable 1. Patient Demographic and ClinicalCharacteristicsPre-SCIP (%) SCIP (%) pNo. of patients 1<strong>16</strong> 134Mean age, yr 48.5 10.1 49.5 11.5 0.502Mean BMI 27.2 5.7 28.8 7.2 0.052Diabetic 4 (3.4) 7 (5.2) 0.495Currently smokingstatus 17 (14.7) 14 (10.4) 0.314Radiation therapy 32 (27.6) 46 (34.3) 0.251Neoadjuvantchemotherapy 37 (31.9) 54 (40.3) 0.189Concurrentchemotherapy 9 (7.7) 14 (10.4) 0.5<strong>16</strong>Adjuvantchemotherapy 3 (2.6) 5 (3.7) 0.728Average tumor stage 1 1 0.953SCIP, Surgical Care Improvement Project; BMI, body mass index.Table 2. Surgical Site Infection, by Type ofReconstructionPre-SCIP (%) SCIP (%) p*No. of patients 1<strong>16</strong> 134Total patients with SSI 21 (18.1) 46 (34.3) 0.004SSI treated with oralantibiotics 10 (8.6) 15 (11.2) 0.499SSI treated with IVantibiotics 6 (5.2) 9 (6.7) 0.608SSI requiring reoperation 5 (4.3) 22 (<strong>16</strong>.4) 0.002Reconstruction with tissueexpander 92 (79.3) 99 (73.9) 0.313Infected tissue expander 17 (18.5) 34 (34.3) 0.013Infected tissue expanderrequiring reoperation 5 (5.4) 18 (18.2) 0.007Reconstruction withautologous flap 24 (20.7) 35 (26.1) 0.313Infected autologous flap 4 (<strong>16</strong>.7) 12 (34.3) 0.135Infected autologous flaprequiring reoperation 0 (0) 4 (11.4) 0.115SCIP, Surgical Care Improvement Project; SSI, surgical-site infection;IV, intravenous.*Italicized values represent significant findings.497
Plastic and Reconstructive Surgery • September <strong>2012</strong>Table 3. Multivariate Logistic Regression ResultsPredicting Surgical-Site Infection RequiringReoperation*AdjustedOdds Ratio (95% CI) p †Pre-SCIP group 1.00SCIP group 4.74 (1.69–13.80) 0.004Radiation therapyNo 1.00Yes 4.50 (1.80–11.29) 0.001Body mass index30 1.0030 4.99 (2.03–12.31) 0.001Tissue expander/implantNo 1.00Yes 3.77 (1.11–12.83) 0.033CI, confidence interval; SCIP, Surgical Care Improvement Project.*N 250 patients.†All p values represent significant findings.number of tissue expander surgical-site infectionsincreased from 18.5 percent to 34.3 percent in thepre–Surgical Care Improvement Project group versusthe Surgical Care Improvement Project group(p 0.013). The number of tissue expanders requiringremoval increased from 5.4 percent to 18.2percent (p 0.007). Among women undergoingautologous reconstruction, we did note an overallincrease in surgical-site infection rates from <strong>16</strong>.7 percentin the pre–Surgical Care Improvement Projectto 34.3 percent in the Surgical Care ImprovementProject group; however, this difference was not statisticallysignificant (p 0.135). We also noted anincrease in the number of autologous flap reconstructionsurgical-site infections requiring reoperation(0 percent versus 11.4 percent); however, thisdifference was also not statistically significant (p 0.115).In multivariate analyses, after adjusting for historyof radiation therapy, body mass index (categorizedas 30 versus 30), treatment group (pre–Surgical Care Improvement Project versus SurgicalCare Improvement Project), and type of reconstructionperformed (autologous versus tissue expander/implant), patients in the Surgical Care ImprovementProject group were 4.74 times (95 percent confidenceinterval, 1.69 to 13.80) more likely to developa surgical-site infection requiring reoperation thanpatients treated in the pre–Surgical Care ImprovementProject group. Furthermore, patients with ahistory of radiation therapy were 4.50 times (95percent confidence interval, 1.80 to 11.29) morelikely to develop a surgical-site infection requiringreoperation than patients not treated with radiation.Obese women (body mass index 30) were4.99 times (95 percent confidence interval, 2.03 to12.31) more likely to develop a surgical-site infectionrequiring reoperation, and women who underwentreconstruction with tissue expanders/implantswere 3.77 times (95 percent confidenceinterval, 1.11 to 12.83) more likely to develop asurgical-site infection requiring reoperation andremoval of the tissue expander/implant after adjustingfor the above covariates (Table 3).In subset analyses of the women who developeda surgical-site infection requiring reoperation(n 27), history of axillary lymph node dissectionand use of AlloDerm were not associatedwith a surgical-site infection requiring reoperation(p 0.334 and p 0.819, respectively). Use ofAlloDerm was less common (43.8 percent) in theSurgical Care Improvement Project group versusthe pre–Surgical Care Improvement Project group(56.3 percent); however, the difference was notstatistically significant (p 0.128). We also examinedthe time interval between initial surgery andthe development of a surgical-site infection requiringimplant removal, and compared resultsbetween the two treatment groups. We found thatwomen in the pre–Surgical Care ImprovementProject group developed a surgical-site infection amean of 256 182 days after surgery comparedwith women in the Surgical Care ImprovementProject group, who developed a surgical-site infectiona mean of 90 93 days (p 0.011) aftersurgery. Regarding early infections requiring explantation(30 days), fewer women in the pre–Surgical Care Improvement Project group (20 percent)developed such an infection compared withwomen in the Surgical Care Improvement Projectgroup (35 percent) (p 0.477). Bacterial isolatesbefore and after implementation of the SurgicalCare Improvement Project guidelines are reportedin Figures 1 and 2. After implementationof the Surgical Care Improvement Project protocol,the bacterial isolates became more diverse,with a much higher incidence of Gram-negativebacteria (Fig. 2).DISCUSSIONWomen undergo mastectomies for both prophylacticand therapeutic reasons. Whether performedto treat breast cancer or as a preventativemeasure for women with a genetic predispositionto cancer or strong familial indicators, breast reconstructionfollowing a mastectomy can be performedby placement of an implant or by meansof autologous techniques. Surgical-site infectionfollowing breast reconstruction can necessitateoral or intravenous antibiotic therapy, lengthenthe duration of the hospital stay, or lead to loss of498
Volume 130, Number 3 • Antibiotics and Breast ReconstructionFig. 1. Bacteria isolated before implementation of the Surgical Care ImprovementProject protocol. PO, oral; IV, intravenous; OSSA, oxacillinsensitiveStaphylococcus aureus.Fig. 2. Bacteria isolated after implementation of the Surgical Care Improvement Project protocol.PO, oral; IV, intravenous; MRSA, methicillin-resistant Staphylococcus aureus; ORSA, oxacillin-resistantStaphylococcus aureus; OSSA, oxacillin-sensitive Staphylococcus aureus.the implant or flap. An evidence-based universalprotocol governing the use of prophylactic antibioticsto prevent postoperative surgical-site infectionsfollowing breast reconstruction does not currentlyexist. 1,2The current standard of care is that a preoperativedose of prophylactic antibiotic should begiven to patients undergoing postmastectomy breastreconstruction. 4,13 In an advisory statement fromthe National Surgical Infection Prevention Project,which is based on published evidence, infusion ofthe first antimicrobial dose should begin no soonerthan 60 minutes before the incision. 12 Based on publishedevidence, the same workgroup endorsed thenational performance measure (Surgical Care ImprovementProject guidelines) that prophylactic antimicrobialagents should be discontinued within 24hours of the end of surgery. 12 However, specificrecommendations for plastic surgery were not included.Many surgeons prescribe postoperative antibioticsfor up to 1 week following postmastectomybreast reconstruction, whereas others routinely continuepostoperative antibiotics until all drains areremoved, which can be as long as 2 weeks. 5499
Plastic and Reconstructive Surgery • September <strong>2012</strong>According to the published Guideline for Preventionof Surgical-Site Infection, 14 three categoriesof variables have proven to be reliable predictorsof surgical-site infection risk: (1) those thatestimate the intrinsic degree of microbial contaminationof the surgical site, (2) those that measurethe duration of an operation, and (3) those thatserve as markers for host susceptibility. Patientrelatedfactors possibly associated with an increasedrisk of surgical-site infection include remote site infectionor colonization, diabetes, cigarette smoking,obesity, extremes of age, and poor nutritional andimmunocompromised status. 15–22 Many of thesecharacteristics are present in the plastic surgery patientpopulation, including overweight and obesepatients, current smoking status and, to a lesser extent,diabetes and immunosuppression.There have been a number of excellent studiesfrom the general surgery and surgical oncologyliterature examining surgical-site infection ratesamong women undergoing surgery for breast cancer.A review of this literature by Penel et al. 23 andothers have documented surgical-site infectionrates ranging from 1.9 to 50 percent. 24–37 In theprospective study by Penel et al. comparing surgical-siteinfection rates before and after the implementationof prophylactic antibiotics, the authorsconclude that the antibiotic prophylaxisreduced the risk of surgical-site infection in breastcancer surgery by 81 percent.A recent systematic review of the literatureexamining preoperative and perioperative prophylacticantibiotic use in breast surgery includedseven articles with a total of 1924 participants in ameta-analysis. 38 No eligible studies evaluating prophylacticantibiotics used during reconstructivesurgery (with or without implants) were identifiedin this study. From this review, pooling of theresults demonstrated that prophylactic antibioticssignificantly reduce the incidence of surgical-siteinfection for patients undergoing breast cancersurgery without reconstruction (pooled relativerisk, 0.66; 95 percent confidence interval, 0.48 to0.89). No studies presented separate data for patientswho underwent reconstructive surgery at thetime of removal of the breast tumor.Other studies have examined the overall incidenceof periprosthetic infection following tissueexpander insertion for breast cancer reconstruction.In a review by Francis et al., 39 the authors notedinfection rates ranging from 2.5 to 24 percent. 40–45Other authors have reported infection rates afterexpander-based reconstructions ranging between 1and 24 percent. 41,44,46,47 However, no consensus regardingthe use of postoperative antibiotics afterimplant reconstruction exists.There have been only a small number of randomizedclinical trials examining antibiotic prophylaxisfollowing breast reconstruction. In theonly prospective, double-blinded, placebo-controlledtrial of a single dose of azithromycin onpostoperative wound infections in plastic surgerypatients conducted by Amland et al., 48 the authorsreported significantly fewer wound infections (5percent versus 20 percent) in patients undergoingbreast reconstruction who received prophylacticantibiotics. There was a significant reduction inpostoperative complications with the additionaluse of antibiotics postoperatively in the prophylaxisgroup. 48Recent findings published by the National SurgicalInfection Prevention Project suggest that theadministration of prophylactic antibiotics shouldbe discontinued within 24 hours of the completionof surgery. 2 These recommendations, however,are based on studies outside of the practiceof plastic surgery and are not based on studiesconducted with women undergoing implant-basedreconstructions. Reconstructive breast surgery differsfrom other types of surgery because of a greatersurface area of undermined tissue, nearly universalischemia to the skin flaps from the mastectomy,breast duct bacteria, and the possible presence of animplant.We have noted an increase in the rate of surgical-siteinfections requiring treatment with oraland intravenous antibiotics and a statistically significantincrease in the rate of surgical-site infectionrequiring reoperation since the adoption ofthe Surgical Care Improvement Project guidelinesat our institution. Before the adoption of the SurgicalCare Improvement Project guidelines, ourrate of surgical-site infection requiring reoperationwas similar (4.3 percent) to the rates reportedin the literature (approximately 2 to 15 percent);however, we currently have an unacceptably highrate of surgical-site infection requiring reoperation(<strong>16</strong>.4 percent). In our patient population,single-dose prophylactic intravenous antibiotic usehas not been associated with a decreased risk ofsurgical-site infection, resulting in a greater numberof reconstructive failures in patients undergoingprosthetic breast reconstruction. This risk is 4.74times higher than in patients receiving postoperativeprophylactic antibiotics. We have also noted a higherproportion of Gram-negative bacteria from thewound culture isolates of women requiring implantremoval after the implementation of the SurgicalCare Improvement Project guidelines (Fig. 2). Bac-500
Volume 130, Number 3 • Antibiotics and Breast Reconstructionterial isolates from women treated with postoperativeantibiotics who required removal of the implantbefore the implementation of the Surgical Care ImprovementProject guidelines were more likely togrow Staphylococcus (Fig. 1). The use of postoperativeprophylactic antibiotics in this group may have preventedGram-negative infections and selected formore common and/or resistant Staphylococcus species,although we were unable to demonstrate thisstatistically.We acknowledge several limitations of thisstudy, with the foremost being its retrospectivenature. Patients were not randomized and the durationof antibiotic therapy in the pre–SurgicalCare Improvement Project group was not controlledfor. Antibiotics were stopped after drainremoval, which was performed when output wasless than 30 ml/day. Although this was consistent,we did not record the mean duration of postoperativeantibiotic use. Surgeons at our institutionadopted the use of AlloDerm at approximately thesame time; however, it was not used in all implantbasedreconstructions. We did not record the rateof AlloDerm use for the entire study population,as the purpose of this study was not to examine riskassociated with this product and it was used selectivelyand infrequently. Our group has been usingthis product for a number of years before the studyand therefore we do not feel a learning curveeffect was present. We are currently undertakinga prospective randomized study of the duration ofantibiotic use at our institution and its impact onthe development of surgical-site infection in patientsundergoing prosthetic breast reconstruction.We will compare the efficacy of postoperativeantibiotic prophylaxis in patients receiving themaximum allowed by current Surgical Care ImprovementProject protocol (24 hours) to thosereceiving an experimental protocol (7 days).The optimal duration of postoperative prophylacticantibiotic therapy has not been well establishedin the plastic surgery literature, and webelieve the current recommendations are inadequate.We believe that a single dose of preoperativeprophylactic antibiotics is not enough and hasresulted in higher rates of surgical-site infectionrequiring reoperation in patients undergoing prostheticbreast reconstruction.Eric G. Halvorson, M.D.Division of Plastic and Reconstructive SurgeryDepartment of SurgeryUniversity of North Carolina at Chapel HillChapel Hill, N.C. 27599-7195eric_halvorson@med.unc.eduREFERENCES1. Mukhtar RA, Throckmorton AD, Alvarado MD, et al. Bacteriologicfeatures of surgical site infections following breastsurgery. Am J Surg. 20<strong>09</strong>;198:529–531.2. Olsen MA, Lefta M, Dietz JR, et al. Risk factors for surgicalsite infection after major breast operation. J Am Coll Surg.2008;207:326–335.3. Landes G, Harris PG, Lemaine V, et al. Prevention of surgicalsite infection and appropriateness of antibiotic prescribinghabits in plastic surgery. J Plast Reconstr Aesthet Surg. 2008;61:1347–1356.4. Pittet B, Montandon D, Pittet D. Infection in breast implants.Lancet Infect Dis. 2005;5:94–106.5. Phillips BT, Wang ED, Mirrer J, et al. Current practice amongplastic surgeons of antibiotic prophylaxis and closed-suctiondrains in breast reconstruction: Experience, evidence, andimplications for postoperative care. Ann Plast Surg. 2011;66:460–465.6. Lyle WG, Outlaw K, Krizek TJ, Koss N, Payne WG, RobsonMC. Prophylactic antibiotics in plastic surgery: Trends of useover 25 years of an evolving specialty. Aesthetic Surg J. 2003;23:177–183.7. Hunter JG. Appropriate prophylactic antibiotic use in plasticsurgery: The time has come. Plast Reconstr Surg. 2007;120:1732–1734.8. Grunebaum LD, Reiter D. Perioperative antibiotic usage byfacial plastic surgeons: National survey results and comparisonwith evidence-based guidelines. Arch Facial Plast Surg.2006;8:88–91.9. Perrotti JA, Castor SA, Perez PC, Zins JE. Antibiotic use inaesthetic surgery: A national survey and literature review.Plast Reconstr Surg. 2002;1<strong>09</strong>:<strong>16</strong>85–<strong>16</strong>93; discussion <strong>16</strong>94–<strong>16</strong>95.10. Peled IJ, Gur D, Berger J, Ramon I, Ullmann Y, Nachlieli T.Prophylactic antibiotics in aesthetic and reconstructive surgery.Aesthetic Plast Surg. 2000;24:299–302.11. Rohrich RJ, Rios JL. The role of prophylactic antibiotics inplastic surgery: Whom are we treating? Plast Reconstr Surg.2003;112:617–618.12. Hawn MT, Vick CC, Richman J, et al. Surgical site infectionprevention: Time to move beyond the surgical care improvementprogram. Ann Surg. 2011;254:494–499; discussion 499–501.13. Bratzler DW, Houck PM; Surgical Infection PreventionGuideline Writers Workgroup. Antimicrobial prophylaxis forsurgery: An advisory statement from the National SurgicalInfection Prevention Project. Am J Surg. 2005;189:395–404.14. Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR.Guideline for prevention of surgical site infection, 1999.Hospital Infection Control Practices Advisory Committee.Infect Control Hosp Epidemiol. 1999;20:250–278.15. Gordon SM. Antibiotic prophylaxis against postoperativewound infections. Cleve Clin J Med. 2006;73(Suppl 1):S42–S45.<strong>16</strong>. Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG.CDC definitions of nosocomial surgical site infections, 1992:A modification of CDC definitions of surgical wound infections.Infect Control Hosp Epidemiol. 1992;13:606–608.17. Greenhalgh DG. Wound healing and diabetes mellitus. ClinPlast Surg. 2003;30:37–45.18. Haley RW, Culver DH, White JW, Morgan WM, Emori TG.The nationwide nosocomial infection rate: A new need forvital statistics. Am J Epidemiol. 1985;121:159–<strong>16</strong>7.501
Plastic and Reconstructive Surgery • September <strong>2012</strong>19. Wilson AP, Weavill C, Burridge J, Kelsey MC. The use of thewound scoring method ‘ASEPSIS’ in postoperative woundsurveillance. J Hosp Infect. 1990;<strong>16</strong>:297–3<strong>09</strong>.20. Wilson AP, Gibbons C, Reeves BC, et al. Surgical woundinfection as a performance indicator: Agreement of commondefinitions of wound infection in 4773 patients. BMJ. 2004;329:720.21. Wilson AP, Hodgson B, Liu M, et al. Reduction in woundinfection rates by wound surveillance with postdischarge follow-upand feedback. Br J Surg. 2006;93:630–638.22. Bertin ML, Crowe J, Gordon SM. Determinants of surgicalsite infection after breast surgery. Am J Infect Control 1998;26:61–65.23. Penel N, Yazdanpanah Y, Chauvet MP, et al. Prevention ofsurgical site infection after breast cancer surgery by targetedprophylaxis antibiotic in patients at high risk of surgical siteinfection. J Surg Oncol. 2007;96:124–129.24. Rotstein C, Ferguson R, Cummings KM, Piedmonte MR,Lucey J, Banish A. Determinants of clean surgical woundinfections for breast procedures at an oncologic center. InfectControl Hosp Epidemiol. 1992;13:207–214.25. Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG.CDC definitions of nosocomial surgical site infections, 1992:A modification of CDC definitions of surgical wound infections.Am J Infect Control 1992;20:271–274.26. Wedgwood KR, Benson EA. Non-tumour morbidity and mortalityafter modified radical mastectomy. Am R Coll Surg Engl.1992;79:314–317.27. Barber GR, Miransky J, Brown AE, et al. Direct observationsof surgical wound infections at a comprehensive cancer centre.Arch Surg. 1995;130:1042–1047.28. Morimoto K, Kinoshita H. Once-daily use of ofloxacin forprophylaxis in breast cancer surgery. Chemotherapy 1998;44:135–141.29. Gupta R, Sinnett D, Carpenter R, Preece PE, Royle GT.Antibiotic prophylaxis for postoperative wound infection inclean elective breast surgery. Eur J Surg Oncol. 2000;26:363–366.30. Danforth DN Jr, Lippman ME, McDonald H, et al. Effect ofpreoperative chemotherapy on mastectomy for locally advancedbreast cancer. Am Surg. 1990;56:6–11.31. Badr el Din A, Coibion M, Guenier C, et al. Local postoperativemorbidity following pre-operative irradiation in locallyadvanced breast cancer. Eur J Surg Oncol. 1989;15:486–489.32. Thomas R, Alvino P, Cortino GR, et al. Long-acting versusshort-acting cephalosporins for preoperative prophylaxis inbreast surgery: A randomized double-blind trial involving1,766 patients. Chemotherapy 1999;45:217–223.33. Canavese G, Catturich A, Vecchio C, et al. Surgical complicationsrelated to peri-operative adjuvant chemotherapy inbreast cancer: Results of a prospective controlled, randomizedclinical trial. Eur J Surg Oncol. 1997;23:10–12.34. Platt R, Zaleznik DF, Hopkins CC, et al. Perioperative antibioticprophylaxis for herniorrhaphy and breast surgery.N Engl J Med. 1990;18:153–<strong>16</strong>0.35. Vilar-Compte D, Jacquemin B, Robles-Vidal C, Volkow P.Surgical site infections in breast surgery: Case-control study.World J Surg. 2004;28:242–246.36. Rey JE, Gardner SM, Cushing RD. Determinants of surgicalsite infection after breast biopsy. Am J Infect Control 2005;33:126–129.37. Kompatscher P, von Planta A, Spicher I, et al. Comparisonof the incidence and predicted risk of early surgical siteinfections after breast reduction. Aesthetic Plast Surg. 2003;27:308–314.38. Cunningham ME, Bunn F, Handscomb K. Prophylactic antibioticsto prevent surgical site infection after breast cancersurgery. Cochrane Database Syst Rev. 2006;(2):CD005360.39. Francis SH, Ruberg RL, Stevenson KB, et al. Independentrisk factors for infection in tissue expander breast reconstruction.Plast Reconstr Surg. 20<strong>09</strong>;124:1790–1796.40. Cordeiro PG, McCarthy CM. A single surgeon’s 12-year experiencewith tissue expander/implant breast reconstruction:Part I. A prospective analysis of early complications.Plast Reconstr Surg. 2006;118:825–831.41. Armstrong RW, Berkowitz RL, Bolding F. Infection followingbreast reconstruction. Ann Plast Surg. 1989;23:284–288.42. Pinsolle V, Grinfeder C, Mathoulin-Pelissier S, Faucher A.Complications analysis of 266 immediate breast reconstructions.J Plast Reconstr Aesthet Surg. 2006;59:1017–1024.43. Nahabedian MY, Tsangaris T, Momen B, Manson P. Infectiouscomplications following breast reconstruction with expandersand implants. Plast Reconstr Surg. 2003;112:467–476.44. Handel N, Jensen JA, Black Q, Waisman JR, Silverstein MJ.The fate of breast implants: A critical analysis of complicationsand outcomes. Plast Reconstr Surg. 1995;96:1521–1533.45. Spear SL, Majidian A. Immediate breast reconstruction intwo stages using textured, integrated-valve tissue expandersand breast implants: A retrospective review of 171 consecutivebreast reconstructions from 1989 to 1996. Plast ReconstrSurg. 1998;101:53–63.46. Disa JJ, Ad-El DD, Cohen SM, Cordiero PG, Hidalgo DA. Thepremature removal of tissue expanders in breast reconstruction.Plast Reconstr Surg. 1999;104:<strong>16</strong>62–<strong>16</strong>65.47. Brown SL, Heflin B, Woo EK, Parmentier CM. Infectionsrelated to breast implants reported to the Food and DrugAdministration, 1977–1997. J Long Term Eff Med Implants2001;11:1–12.48. Amland PF, Andenaes K, Samdal F, et al. A prospective,double-blind, placebo-controlled trial of a single dose ofazithromycin on postoperative wound infections in plasticsurgery. Plast Reconstr Surg. 1995;96:1378–1383.502
ArticlesPatients were discharged within 2 days of surgery.About two weeks after surgery, they were examined andasked to come back in a year’s time. We informed themthat postoperative pain would last for about 2 weeksand that the wound would take 2 months to heal(epithelialisation), at which point they would be able toresume sexual intercourse. At the 1-year visit, womenwere questioned about pain and functionality. Wecompared the 1-year group with the total group atinclusion to check for representativeness.Statistical analysisWe prospectively entered the data in Stata 10, and didpost-hoc analyses. We worked on the assumption thatmissing data were not a reason for exclusion, andanalysed all the variables in a pragmatic way, according toavailable data. We provide the numerator for eachvariable. We used the χ² test to compare characteristics atinclusion. We took the year of attendance into accountfor all the preoperative criteria (Pearson test). We analysedthe odd ratios and 95% CIs, and used logisticregression for the prognosis variables. Logistic was usedfor statistical analyses.Role of the funding sourceThe sponsor of the study supported the data analysis andthe English editing of the report, but had no role in thestudy design, data collection, data analysis, the writing ofthe report, or the decision to submit for publication. Thecorresponding author had full access to all the data in thestudy and had final responsibility for the decision tosubmit for publication.Year of consultation*Clitoral pleasure before surgical procedureNever1998–2003 46/143(32%)2004 149/390(38%)2005 235/534(44%)2006 271/459(59%)2007 253/454(56%)2008 218/397(55%)20<strong>09</strong> 131/235(56%)Total 1303/2613(50%)Age (years)†18–19 60/94(64%)20–24 411/744(55%)25–29 368/768(48%)30–34 213/466(46%)35–39 127/267(48%)40–44 88/193(46%)≥45 55/136(40%)Total 1322/2668(50%)Minorsensation32/143(22%)67/390(17%)58/390(11%)27/459(6%)14/454(3%)7/397(2%)3/235(1%)208/21 613(8%)6/94(6%)63/744(8%)66/768(9%)43/466(9%)17/267(6%)14/193(7%)8/136(6%)217/2668(8%)Pleasantwithoutorgasm47/143(33%)98/390(33%)105/390(20%)79/459(17%)99/454(22%)85/397(21%)29/235(12%)542/21 613(21%)19/94(20%)145/744(19%)172/768(22%)104/466(22%)52/267(19%)34/193(18%)29/136(21%)555/2668(21%)Mutilationrestrictedorgasm<strong>16</strong>/143(11%)50/390(11%)85/390(<strong>16</strong>%)42/459(9%)26/454(8%)33/397(8%)31/235(13%)283/21 613(11%)5/94(5%)67/744(9%)79/768(10%)59/466(13%)39/267(15%)29/193(15%)15/136(11%)293/2668(11%)Regularorgasm2/143(1%)26/390(7%)52/390(10%)40/459(9%)62/454(14%)54/397(14%)41/235(17%)277/21 613(11%)4/94(4%)58/744(8%)83/768(11%)47/466(10%)32/267(12%)28/193(15%)29/136(21%)281/2668(11%)Pain before surgical procedureTotal No pain Minordiscomfortduringintercourse143 83/173(48%)390 202/392(52%)534 355/552(64%)459 327/464(70%)454 336/455(74%)397 297/398(75%)235 198/261(76%)2613 1798/2695(67%)94 73/105(70%)744 522/755(69%)768 496/772(64%)466 315/467(64%)267 <strong>16</strong>9/267(63%)193 124/194(64%)136 99/125(73%)2668 1798/2695(67%)41/173(24%)77/392(20%)45/552(8%)27/464(6%)<strong>16</strong>/455(4%)4/398(1%)4/261(2%)214/2695(8%)8/105(8%)53/755(7%)63/772(8%)39/467(8%)23/267(9%)19/194(10%)9/125(7%)214/2695(8%)Moderatepain duringintercourse22/173(13%)71/392(18%)84/552(15%)59/464(13%)59/455(13%)59/398(15%)36/261(14%)390/2695(14%)13/105(12%)99/755(13%)121/772(<strong>16</strong>%)72/467(<strong>16</strong>%)36/267(13%)32/194(<strong>16</strong>%)17/125(13%)390/2695(14%)Strong tounbearablepain duringintercourse<strong>16</strong>/173(9%)30/392(8%)44/552(8%)39/464(8%)34/455(7%)23/398(6%)11/261(4%)197/2695(7%)7/105(7%)53/755(7%)68/772(9%)30/467(9%)22/267(8%)10/194(5%)7/125(5%)197/2695(7%)Painwithoutintercourse11/173(6%)12/392(3%)24/552(4%)12/464(3%)10/455(2%)15/398(4%)12/261(5%)96/2695(4%)4/105(4%)28/755(4%)24/772(3%)11/467(3%)17/267(6%)9/194(5%)3/125(2%)96/2695(4%)Total17339255246445539826126951057557724672671941252695Data are n/N (%). *Pearson’s χ² for clitoral pleasure before surgical procedure was 301·61<strong>09</strong> Pr
ArticlesPreoperative clitoral pleasureTotal Pain Discomfort SlightimprovementRealimprovementRestrictedorgasmRegular orgasmNever 368 1/368 (
ArticlesProportion ofpatients in pain (%)Crude OR Adjusted OR Adjusted95% CIYear of first consultation 0·0239* 0·0765†1998–2003 43% (92/2<strong>16</strong>) 1 1 ··2004 50% (277/556) 0·92 0·91 0·63–1·312005 31% (178/578) 0·89 0·88 0·62–1·252006 25% (1<strong>16</strong>/470) 1·37 1·30 0·90–1·872007 23% (104/456) 1·05 1·00 0·70–1·442008 24% (97/398) 0·97 0·92 0·64–1·3320<strong>09</strong> 24% (62/264) 0·87 0·89 0·59–1·30Age at excision 0·0065 0·0001≤1 year 27% (152/567) 1 1 ··1–4 years 28% (236/849) 0·70 0·7 0·61–0·925–9 years 34% (370/1<strong>09</strong>1) 0·67 0·7 0·61–0·9410–14 years 38% (143/375) 0·69 0·7 0·63–1·08≥15 years 46% (25/55) 0·76 0·9 0·55–1·72Excision country 0·0<strong>16</strong>2 0·0379Burkina Faso 30% (64/217) 1 1 ··CÔte d’Ivoire 33% (102/311) 1·30 1·36 0·94–1·97Guinea 40% (82/203) 1·89 1·85 1·22–2·80Mali 30% (211/699) 1·89 1·56 1·12–2·18Mauritania 37% (40/1<strong>09</strong>) 1·92 1·60 0·97–2·65Senegal 31% (201/654) 1·33 1·23 0·88–1·71West Africa 39% (19/49) 1·70 1·51 0·78–2·92East and central Africa 44% (57/129) 1·20 1·12 0·69–1·81France 26% (149/564) 1·47 1·19 0·84–1·69Expectations
Articlesincluded women (mostly from Somalia) with type IIImutilation, which does not involve the systematicremoval of the clitoris. The WHO definition of type IIImutilation covers two states: with clitoris (closed butnot cut) and without (cut and closed). These differencesare clearly described in the Population ReferenceBureau’s 2010 report. 23 This is the reason why we didnot use the technique described by Johnson andcolleagues. 14 The aim of reconstructive genital surgeryafter female genital mutilation should be to restore thenormal anatomy as far as possible.Another point of discussion is population selection.In 20<strong>09</strong>, Andro and colleagues 24 published a case-controlstudy designed to measure the effect of female genitalmutilation on the health of women living in France,including 714 excised women versus 2<strong>16</strong>8 non-excisedwomen. The authors noted that only 55% of participantswith female genital mutilation were aware of theavailability of surgical repair, 27% were interested inhaving it done, but only 3% had actually gone ahead with it.The design of the present study had several limitations,notably the fact that it was an open before-and-afterassessment and we had no long-term follow-up data fornon-operated women, so causality could not be shown.Because we could not envisage a sham procedure, acomparative randomised study was not feasible. Wedesigned our own rating scales for clitoral pleasure andpain, and these should doubtless have been morestandardised and validated formally. Assessments werebased on assumption, but as they were done both beforeand after the surgical procedure, each patient was herown control. Moreover, having the same investigator forall the procedures and assessments might have decreasedsome biases.No scales currently exist specifically to assess painand clitoral pleasure, and more studies in this area wouldbe welcome. Some studies have explored the quality of thesex lives of patients with female genital mutilation. Usingthe validated female sexual function index (FSFI), Cataniaand colleagues 25 reported significant differences between57 infibulated women and 57 controls in desire, arousal,orgasm, and satisfaction, with mean scores higher in thegroup of mutilated women than in the control group. Butthese findings cannot lead to a clear conclusion since webelieve that matching Italian women with African womenconstituted a major bias, and the FSFI has yet to beformally validated in a population of African women.Interestingly, in another group of patients, 25 theinvestigators noted that 86% of 137 women with femalegenital mutilation experienced orgasm (69% always).Even if these findings are limited by important grouprecruitment biases, they could be compared with the91% of women who experienced orgasm (only 9% always)noted in another group of 58 youngest women. At last, thefact that the sample essentially consisted of women withtype III mutilation from Somalia (no cutting) well haveexplained the high orgasm rate.Proportion of patientswith no pleasure (%)Year of first consultation 0·0239 0·07651998–2003 58% (99/172) 1 1In another study, 15 14 of 18 patients who had undergonedefibulation and who were assessed on the FSFI scalebefore and after, came from Somalia (not cut) andreported no improvement in orgasmic function. Eventhough we used a pragmatic scale, we consider that ourprocedure did indeed correct type II and type III (withcutting) mutilations, by giving the women a morefunctional clitoris. Further research should include alarge case-control study (excised and non-excised)women with the administration of a validated questionnairesuch as the FSFI, to fully understand and describethe subpopulation concerned by clitoral repair.We had no data about the sexual partners women hadbefore and after surgery. Sexual pleasure varies fromone sexual partner to another, and this could thereforebe another major limitation. The complexity of thesexual dysfunctions that can be associated with femalegenital mutilation underlines, for us, the need tosystematically offer sexual therapy to patients. Furthermore,these women might have experienced sufferingCrude OR Adjusted OR Adjusted 95% CI2004 55% (2<strong>16</strong>/390) 0·92 0·91 0·63–1·312005 55% (293/535) 0·89 0·88 0·62–1·252006 65% (298/459) 1·37 1·30 0·90–1·872007 59% (267/454) 1·05 1·00 0·70–1·442008 57% (225/397) 0·97 0·92 0·64–1·3320<strong>09</strong> 54% (141/261) 0·87 0·89 0·59–1·30Age at excision 0·0065 0·0001≤1 year 65% (343/529) 1 1 ··1–4 years 56% (433/767) 0·70 0·7 0·6–0·95–9 years 55% (543/980) 0·67 0·7 0·6–0·910–14 years 56% (192/343) 0·69 0·7 0·6–1·0≥15 years 58% (28/48) 0·76 0·9 0·5–1·7Excision country 0·0<strong>16</strong>2 0·0379Burkina Faso 48% (95/199) 1 1 ··Ivory Coast 54% (153/282) 1·30 1·36 0·94–1·97Guinea 63% (121/191) 1·89 1·85 1·22–2·80Mali 63% (405/640) 1·89 1·56 1·12–2·18Mauritania 64% (63/99) 1·92 1·60 0·97–2·65Senegal 55% (325/592) 1·33 1·23 0·88–1·71West Africa 61% (28/46) 1·70 1·51 0·78–2·92East and central Africa 52% (56/107) 1·20 1·12 0·69–1·81France 57% (292/5<strong>09</strong>) 1·47 1·19 0·84–1·69Expectations
ArticlesPanel: Research in contextSystematic reviewWe searched PubMed with the keywords “female genitalmutilation”, “repair”, “consequences”, “sexuality”, and “study”,for all years and all languages, up to the end of December,2011. Our objective was to select randomised trials andobservational studies of more than 50 patients. We found101 articles and selected the 17 highest level studies that arecited here. 3–5,7–9,11,13–<strong>16</strong>,18,19,22–25 This systematic review allowed us todescribe both the immediate health complications and thelong-term health risks. The frequency of clitoral pain isunknown, even though the reparative surgery was initiallyoffered to alleviate pain. With the exception of our own earlierstudy, all existing publications on repair of female genitalmutilation concern type III mutilation without clitoral excision.The defibulation technique they describe might improvewomen’s sex lives by suppressing the dyspareunia that oftenaccompanies this type of mutilation. Descriptions of the sexlives of excised women also mainly concern type III mutilation.InterpretationOur study of 2938 patients showed that among the866 women who were followed up at 1 year, reconstructivesurgery after female genital mutilation is effective. There wasno mortality, only 5·3% morbidity and good feasibility. Weoperated mainly on women who had undergone type IIexcision. These patients reported pain reduction and animprovement in orgasmic function.and violence in many different forms, which couldresult in post-traumatic stress disorder 4 —an aspect weare currently exploring.564 patients in our series had undergone femalegenital mutilation in France, even though this practicehas been strongly condemned in France. This exportedtradition, hidden, and very much taboo, was first broughtto light some 20 years ago in several French cities.Although no specific legislation has ever been passed,since 1978, 25 prosecutions (French Penal Code Art222)of circumcisors or parents have taken place in France(the only country where this has happened). 26From the public health point of view, these womenwere poor, and were only able to access surgical carebecause the French national health-care system bore thecosts incurred. In most developed and all developingcountries, reconstructive surgery is prohibitively expensive.Women have major unmet needs, and access tosurgery is poor. In France, where most of the healthexpenses are reimbursed, there is only limited provision,because only a handful of surgeons have been trained inthis technique, and fewer than ten offer this service inFrance. And yet, this surgery is rewarding for surgeons,in that we believe it genuinely helps women.In developing countries, where the needs are greatest,reconstructive surgery is rarely accessible. Reconstructivesurgery after female genital mutilation is not a priority incountries beset by public health emergencies. Informinginternational organisations that want to decrease femalegenital mutilation is key. They should help with reconstructivesurgery.Evidence-based health care should be the ultimateobjective when developing a new surgical technique.Reconstructive surgery after female genital mutilationconcerns very vulnerable populations, even in France.We focused our attention on the potential benefits forpatients. We obtained safety data and proof of concept.We used our own prospective database, but moreregistries should be developed. We aim to conductfurther investigations, such as comparative studies,and training programmes a multicentre evaluation programmeshould be implemented. The diffusion of anew technique takes time, and evaluation must be thefirst step. 27–29 The assessment of the surgery ischallenged by factors, such as learning curves, qualityvariations, and perception of equipoise. A large-scaleprogramme is mandatory for assessing this techniquebefore any diffusion. The unmet needs are great indeed.To help these mutilated women more effectively, wemust not only define the innovative surgery moreclearly, but also consider time, communication channels,and the social system.Clitoral reconstruction after female genital mutilationis feasible. It can certainly improve women’s pleasureand lessen their pain. It also allows mutilated womento recover their identity. Age at excision and age atattendance do not affect outcome. The operation mustbe followed by an adaptation period, and can only everrestore a potential. The extent to which this potential isrealised will depend on each individual woman’s lifecourse and the many complex factors known to berelated to sexuality. Reparative surgery can be a liberatingexperience, but many women have to strike adifficult balance between their desire for this liberationand the ordeal of calling family values and localtraditions into question.Clitoral reconstruction after female genital mutilationis feasible. It can improve women’s pleasure and lessentheir pain. It also allows mutilated women to recovertheir identity. Age at excision and age at attendance donot affect outcome. The operation must be followed byan adaptation period, and can only ever restore apotential. The extent to which this potential is realisedwill depend on each individual woman’s life course andthe many complex factors known to be related tosexuality. Reparative surgery can be a liberating experience,but many women have to strike a difficult balancebetween their desire for this liberation and the ordeal ofcalling family values and local traditions into question.Finally, although clitoral reconstruction is extremelyimportant, we believe that women should be offered amultidisciplinary care package, including sexual therapy,if this is acceptable to them.140 www.thelancet.com Vol 380 July 14, <strong>2012</strong>
ArticlesContributorsPF and BC did the literature search and study design. PF did the datacollection. AA, PF, and BC did the data analysis and interpretation.BC, PF, and AA wrote the report.Conflicts of interestWe declare that we have no conflicts of interest.AcknowledgmentsThis study was funded by the French Urological Association (AFU). Wethank Pierre-Jean Cousteix (French National Health Insurance Fund forSalaried Workers, CNAMTS) for advice on the reimbursementprocedure, Hervé Maisonneuve and Elizabeth Portier for editing andtranslating the paper into English, and Christine Louis Sylvestre for theinitial analysis of results.References1 World Health Organization, Department of Reproductive Healthand Research. Eliminating female genital mutilation: an interagencystatement. OHCHR, UNAIDS, UNDP, UNECA, UNESCO, UNFPA,UNHCR, UNICEF, UNIFEM, WHO. Geneva: World HealthOrganization; 2008; p 48. http://www.who.int/reproductivehealth/publications/fgm/9789241596442/en/index.html (accessed April 14,<strong>2012</strong>).2 Yoder PS, Abderrahim N, Zhuzhuni A. Female genital cutting inthe demographic and health surveys: a critical and comparativeanalysis. DHS Comparative Reports 7. Calverton, MD: ORC Macro;2004. http://www.measuredhs.com/pubs/pdf/CR7/CR7.pdf (DHSComparative Reports No. 7) (accessed April 14, <strong>2012</strong>).3 WHO. Female genital mutilation, Fact sheet N241. Geneva: WorldHealth Organization, <strong>2012</strong>. http://www.who.int/mediacentre/factsheets/fs241/en/ (accessed April 14, <strong>2012</strong>).4 Behrendt A, Moritz S. Posttraumatic stress disorder and memoryproblems after female genital mutilation. Am J Psychiatry 2005;<strong>16</strong>2: 1000–02.5 Almroth L, Elmusharaf S, Hadi NE, et al. Primary infertility aftergenital mutilation in girlhood in Sudan: a case-control study. Lancet2005; 366: 385–91.6 WHO study group on female genital mutilation and obstetricoutcome. Female genital mutilation and obstetric outcome:WHO collaborative prospective study in six African countries.Lancet 2006; 367: 1835–41.7 Adam T, Bathija H, Bishai D, et al. for the FGM Cost Study Groupof World Health Organization. Estimating the obstetric costs offemale genital mutilation in six African countries.Bull World Health Organ 2010; 88: 281–88.8 Fox EF, de Ruiter A, Bingham JS. Female genital mutilation.Int J STD AIDS 1997; 8: 599–601.9 Osifo DO, Evbuomwan I. Female genital mutilation amongEdo people: the complications and pattern of presentation at apediatric surgery unit, Benin City. Afr J Reprod Health 20<strong>09</strong>;13: 17–25.10 Women’s Policy Inc. Female genital mutilation. Women’s HealthEquity Act of 1996: legislative summary and overview. WashingtonDC: Women’s Policy Inc, 1996: 48.11 Anon. Female genital mutilation and social change. Lancet 2010;376: 1800.12 WHO Technical Working Group. Female genital mutilation.Geneva: World Health Organization, 1996.13 Nour NM, Michels KB, Bryant AE. Defibulation to treat femalegenital cutting: effect on symptoms and sexual function.Obstet Gynecol 2006; 108: 55–60.14 Johnson C, Nour NM. Surgical techniques: defibulation of type IIIfemale genital cutting. J Sex Med 2007; 4: 1544–47.15 Krause E, Brandner S, Mueller MD, Kuhn A. Out of Eastern Africa:defibulation and sexual function in woman with female genitalmutilation. J Sex Med 2011; 8: 1420–25.<strong>16</strong> Foldes P, Louis-Sylvestre C. Résultats de la réparation chirurgicaledu clitoris après mutilation sexuelle: 453 cas. Gynecol Obstet Fertil2006; 34: 1137–41.17 Johnsdotter S, Essen B. Sexual health among young Somali womenin Sweden: living with conflicting culturally determined sexualideologies. International Network to Analyze, Communicate andTransform the Campaign against Female Genital Cutting, FemaleGenital Mutilation, Female Circumcision (INTACT) conference;Alexandria, Egypt; Oct 10–12, 2004. http://www.mbali.info/doc311.htm (accessed April 14, <strong>2012</strong>).18 Dorkenoo E. Combating female genital mutilation: an agenda forthe next decade. World Health Stat Q 1996; 49: 142–47.19 Foldes P. Reconstructive plastic surgery of the clitoris after sexualmutilation. Prog Urol 2004; 14: 47–50 (in French).20 O’Connell HE, Sanjeevan KV, Hutson JM. Anatomy of the clitoris.J Urol 2005; 174: 1189–95.21 Johnsdotter S, Essen B. Sexual health among young Somali womenin Sweden: living with conflicting culturally determined sexualideologies. International Network to Analyze, Communicate andTransform the Campaign against Female Genital Cutting, FemaleGenital Mutilation, Female Circumcision (INTACT) conference;Alexandria, Egypt; Oct 10–12, 2004. http://www.mbali.info/doc311.htm (accessed April 14, <strong>2012</strong>).22 Gruenbaum E. Socio-cultural dynamics of female genital cutting:research findings, gaps, and directions. Cult Health Sex 2005;7: 429–41.23 Population Reference Bureau Report 2010 Female GenitalMutilation/Cutting: Data and Trends. http://www.prb.org/pdf08/fgm-wallchart.pdf (accessed April 14, <strong>2012</strong>).24 Andro A, Lescligand M, Cambois E. Handicap et excision, 20<strong>09</strong>.http://www.univ-paris1.fr/fileadmin/CRIDUP/Rapport_final_ExH_volet_quantitatif.pdf. (accessed April 14, <strong>2012</strong>).25 Catania L, Abdulcadir O, Puppo V, Verde JB, Abdulcadir J,Abdulcadir D. Pleasure and orgasm in women with female genitalmutilation/cutting (FGM/C). J Sex Med 2007; 4: <strong>16</strong>66–78.26 Foundation for Women’s Health, Research and Development.Report on female genital mutilation 2002. http://www.forwarduk.org.uk/download/10 (accessed April 14, <strong>2012</strong>).27 Barkun JS, Aronson JK, Feldman LS, et al. Evaluation and stagesof surgical innovations. Lancet 20<strong>09</strong>; 374: 1089–96.28 Ergina PL, Cook JA, Blazeby JM, et al. Challenges in evaluatingsurgical innovation. Lancet 20<strong>09</strong>; 374: 1<strong>09</strong>7–104.29 McCulloch P, Altman DG, Campbell WB, et al. No surgicalinnovation without evaluation: the IDEAL recommendations. Lancet20<strong>09</strong>; 374: 1105–12.www.thelancet.com Vol 380 July 14, <strong>2012</strong> 141
RECONSTRUCTIVEFree Flap Take-Back following PostoperativeMicrovascular Compromise: Predicting Salvageversus FailureMichael N. Mirzabeigi, M.D.Theresa Wang, M.D.Stephen J. Kovach, M.D.Jesse A. Taylor, M.D.Joseph M. Serletti, M.D.Liza C. Wu, M.D.Philadelphia, Pa.Background: The purpose of this study is twofold: (1) to stratify preoperativerisk factors that predict successful free flap salvage and (2) to identify perioperativestrategies that correlate with successful salvage.Methods: A retrospective chart review was performed on all free flaps performedfrom January of 2005 to April of 2011. The time until salvage was definedas the end of the initial procedure until the initiation of the salvage attempt. Theprimary endpoint, successful salvage, was defined as any flap that did not resultin total loss.Results: A total of 2260 free flaps were reviewed, and 47 take-backs for delayedmicrovascular compromise were identified. Twenty-three of 47 flaps (49 percent)were salvaged. The mean time until take-back, presence of thrombophilia,and preoperative platelet counts were factors predictive of unsuccessful salvage.Preoperative platelet counts above 300 were associated with the lowest rates ofsalvage. Intraoperative maneuvers were examined, and surgeon experience(defined as 5 years in practice) was the only factor that was significant; however,intraoperative heparin anticoagulation and complete mechanical thrombectomytrended toward significance. The type of thrombolytic agent used wasnot found to result in a statistically significant difference.Conclusions: There is evidence to suggest that there may be preoperative factorspredictive of flap salvage success, including thrombophilia and routinepreoperative platelet values. Shorter time to take-back and surgeon experiencemay improve salvage, whereas intraoperative heparin anticoagulation and completemechanical removal of the thrombus demonstrate preliminary evidenceas effective intraoperative strategies. (Plast. Reconstr. Surg. 130: 579, <strong>2012</strong>.)CLINICAL QUESTION/LEVEL OF EVIDENCE: Risk, III.Postoperative microvascular compromise remainsan infrequent yet devastating complicationfollowing free tissue transfer. Largeseries suggest that the rate of postoperative vascularthrombosis varies but may be at least 5percent. 1–6 Meanwhile, flap loss rates are now publishedto be less than 2 percent at many largemicrosurgery centers. 4,7–9 The disparity in the rateFrom the Division of Plastic Surgery, University of PennsylvaniaHealth System.Received for publication November 10, 2011; acceptedMarch 13, <strong>2012</strong>.Presented at the 28th Annual Meeting of the NortheasternSociety of Plastic Surgeons, in Amelia Island, Florida, October20 through 23, 2011, and the 91st Annual Meetingand Symposium of the American Association of Plastic Surgeons,in San Francisco, California, April 14 through 17,<strong>2012</strong>.Copyright ©<strong>2012</strong> by the American Society of Plastic SurgeonsDOI: 10.1<strong>09</strong>7/PRS.0b013e31825dbfb7of delayed vascular compromise and flap loss isdependent on the ability to successfully salvage aflap that has undergone postoperative venous orarterial thrombosis. Take-back procedures areboth relatively uncommon and technically complex,making successful flap salvage a challengingendeavor. As a result, rates of flap salvage havebeen described to be 30 to 60 percent, and thusthere is great room for improvement. 10–12 Giventhe patient morbidity and financial implications offree flap loss, optimizing free flap salvage stands asan important yet largely unexplored area of clinicalknowledge.Disclosure: No author of this article has anyfinancial interests or commercial associations todisclose.www.PRSJournal.com 579
Plastic and Reconstructive Surgery • September <strong>2012</strong>As approximately one-half of flaps are lost insalvage attempts, little is known about what separatesthese failures from the other half of takebacksthat ultimately survive. To date, the literaturehas described early intervention as the onlyevidence-based strategy or factor that is associatedwith flap salvage. Otherwise, limited clinical datahave come forth to supplant questions surroundingsuccessful free flap salvage. Furthermore, intraoperativestrategies have been relegated to levelIV and V data when describing methods that maylead to flap salvage. The purpose of this study istwofold: (1) to stratify preoperative risk factorsthat predict the success of a take-back and (2) toidentify evidence-based perioperative strategiesthat correlate with successful salvage.PATIENTS AND METHODSA retrospective review of records was performedon all patients undergoing free flap reconstructionat the Division of Plastic Surgery,University of Pennsylvania from January of 2005 toApril of 2011. Free tissue transfer was examined incases of breast, head/neck, and lower extremityreconstruction. Hospital records detailing the intraoperativeand immediate postoperative coursewere used to identify patients who underwent atake-back for attempted flap salvage. A take-backwas defined as any return to the operating roomfollowing the conclusion of the initial free flapprocedure, departure from the operating room,and full reversal of general anesthesia.The major inclusion criterion among takebackcases was delayed microvascular compromise;most often, this is a delayed venous or arterialthrombosis. After the patient leaves theoperating room following the initial procedure,any vascular compromise is then considered “delayed.”To clarify the inclusion criteria, the varioustake-backs were separated into distinct categories(Fig. 1). Take-backs for general purposes such ashematoma, seroma, or infection were designatedclass 1 take-backs and were excluded from thisstudy. Class 2 take-backs were those take-backs thatwere cases of delayed vascular compromise thatunderwent emergent reexploration. Class 2 takebackswere further subdivided into classes 2a, 2b,and 2c. Finally, class 3 take-backs were cases inwhich a necrotic flap underwent a planneddébridement with no salvage maneuvers, andthese cases were excluded from this study.The primary endpoint, successful salvage, wasdefined as any flap that did not result in total flaploss. We specifically chose not to incorporate theoften-described endpoint of “partial flap loss,” asthis is a rather ambiguous and imprecise variableFig. 1. The inclusion criteria and classification scheme.580
Volume 130, Number 3 • Free Flap Take-Backas far as retrospective studies are concerned. Wedid not feel this was an appropriate categoricalvariable, and for partial flap loss to be meaningfulit would need to be a continuous variable (i.e., anyportion of the flap débrided would have to beweighed and calculated as a percentage of thetotal flap). Likewise, we had no way of quantitatingfat necrosis, to make it a proper continuous variable.When the primary endpoint of the study isflap loss, these are nearly meaningless endpointsunless they are properly quantitated. There is intersurgeonvariability in how partial flap loss andfat necrosis are documented. Moreover, variablessuch as partial loss or fat necrosis can be ultimatelyattributed to potentially more significant variablessuch as perforator selection. Thus, one could arguethat a case of fat necrosis would have occurredregardless of postoperative thrombosis. The truegoal of this study is how to prevent total flap failureor, perhaps more specifically, how we can preventrecurrent thrombosis or the no-reflow phenomenon.These more nuanced variables such as fatnecrosis or partial flap loss are too multifactorialor, at the very least, require more careful, prospectivestudy.Other data points of interest included patientdemographics, comorbidities, presence of thrombophilia(confirmed by means of laboratory testingand/or prior history of blood clots), preoperativehematologic values, prior irradiation,surgeon experience, and time until salvage. Thetime until salvage was defined as the end of theinitial procedure until the initiation of the salvageattempt. Intraoperative salvage maneuvers wereexamined, including the use of thrombolytics, anticoagulation,vein grafting, anastomotic sitechange, and mechanical thrombus removal.Univariate statistical analyses included Fisher’sexact test for categorical variables and theMann-Whitney U test for continuous variables. Inaddition, a binary logistic regression model wasused to test for multivariate significance. All testswere two-sided, and a value of p 0.05 was usedto determine statistical significance. Statisticalanalysis was performed using SPSS for Windowsversion 18.0 (SPSS, Inc., Chicago, Ill.).Flap MonitoringAll flaps were monitored by a standardizedprotocol, and this did not vary between the surgeons.Flap monitoring was performed by meansof conventional clinical indicators (i.e., color, temperaturechange, capillary refill, turgor) andhand-held arterial Doppler ultrasonography. Buriedflaps, or those without a skin paddle, weremonitored by means of an implantable Dopplersystem. Doppler checks were performed bytrained nursing staff every 15 minutes for the firsthour, then every hour for the next 48 hours, andthen every 4 hours until the time of discharge,which usually occurred on postoperative day 4.Surgical TechniqueOn changes in Doppler signaling and/or clinicalindicators suggestive of thrombosis, flaps arereturned to the operating room immediately (typicallywithin 1 hour). There is intersurgeon variabilityregarding perioperative protocol and intraoperativesalvage maneuvers. Surgeons oftenadminister intravenous heparin (typically 5000units) following elevation of the flap. The anastomosisis routinely taken down and a mechanicalthrombectomy is performed (with the goal of removingthe thrombus in its entirety). The thrombosedvessel segment is cut back until, ideally,pristine intima is reached. Thrombolytic agentsare used based on the availability of a particularagent, surgeon preference, type of thrombus, andappearance of the flap following thrombectomy.Typically, 250,000 units of thrombolytic agent isinfused with a 25-gauge butterfly needle while theflap is occluded from the systemic circulation. 13Anastomotic site change is typically not performed;however, this is done when the recipientvessels are no longer judged to be viable. Similarly,vein grafting is not routinely performed unless alength discrepancy results following the cut-backof the vessel.RESULTSA total of 2260 flaps were examined in thestudy period from January of 2005 to April of 2011.Forty-seven flaps met the inclusion criteria as class2 cases returning to the operating room for anemergent take-back following delayed microvascularcompromise (Fig. 1). Twenty-three of 47flaps (49 percent) were salvaged. The rates of salvagefor arterial and venous compromise were 52and 46 percent, respectively.Time until Take-Back and Salvage RateFigure 2 is a bar graph demonstrating the timeuntil take-back for the 47 flaps, and Table 1 liststhe corresponding salvage rates for each time period.The first 24 hours had the highest frequencyof take-backs. Postoperative days 2, 3, and 4 had arelatively equal distribution in both the numberand type of take-backs. Figure 3 describes the sal-581
Plastic and Reconstructive Surgery • September <strong>2012</strong>Fig. 2. The number and type of suspected microvascularly compromised flaps (venous or arterialbased on the presence or loss of the arterial Doppler signal with particular clinical indicators) aredescribed for each respective time period.Table 1. Number of Take-Backs for Each Respective Time Period and the Respective Salvage RatesNo Doppler SignalLoss (n 24)*Loss of Arterial DopplerSignal (n 23)†All Take-Backs(n 47)‡Hours untilTake-BackNo. ofFlapsNo. of SalvagedFlaps (%)No. ofFlapsNo. of SalvagedFlaps (%)No. ofFlapsNo. of SalvagedFlaps (%)0–24 10 6 (60) 9 7 (78) 19 13 (68)25–48 3 1 (33) 4 3 (75) 7 4 (57)49–72 2 1 (50) 4 2 (50) 6 3 (50)73–96 4 3 (75) 3 0 7 3 (43)97–120 2 0 0 0 2 0121–144 1 0 2 0 3 0145–<strong>16</strong>8 0 0 1 0 1 0170 2 0 0 0 2 0*p 0.358.†p 0.083.‡p 0.145.vage rate in the first 48 hours versus the 49- to96-hour period versus greater than 96-hour timeperiod. No flap beyond postoperative day 4 (96hours) was salvaged. When examining the “allflapsgroup” and those with “arterial compromise,”rates of salvage declined progressively furtherinto the postoperative time period. Thisdecline in salvage rate was statistically significantfor the all-flaps group (p 0.005) and the arterialcompromise group (p 0.018). The rate of salvagein the “venous compromise group” improvedbefore subsequently declining. However, this wasnot significant (p 0.06).Risk FactorsPreoperative factors were then examined forthose flaps that were salvaged compared withthose that ultimately failed. After univariate analysis,the mean time until take-back, presence of582
Volume 130, Number 3 • Free Flap Take-BackFig. 3. The salvage rate for microvascularly compromised flaps (venous or arterial based on thepresence or loss of the arterial Doppler signal with particular clinical indicators) are described foreach respective time period.thrombophilia, and mean preoperative plateletcounts were significant factors predictive of unsuccessfulsalvage (Table 2). A multivariate binarylogistic regression model examining mean timeuntil take-back, thrombophilia, and preoperativeplatelet counts demonstrated platelet counts toremain significant (p 0.05) (Table 3).Class 2b (Intraoperative Analysis)In an attempt to determine effective intraoperativemaneuvers for cases of delayed vascularthrombosis, a more homogenous subgroup (class2b) was created for analysis (Fig. 1). As a class 2bsubgroup, the remaining 36 flaps that underwentsalvage maneuvers were examined for both preoperativeand intraoperative factors that could potentiallypredict success. After univariate analysisof this subgroup, preoperative platelet values remainedsignificant (Table 4). In examining intraoperativesalvage data, surgeon experience (definedas 5 years in practice) was significant.Intraoperative heparin anticoagulation (p 0.06)and complete mechanical removal of a thrombus(p 0.06) trended toward significance (Table 5).Platelet ValuesFigure 4 contrasts preoperative platelet valuesfor flaps that were salvaged versus those that werenot salvaged. The values are plotted separately forvenous and arterial compromise. The overall percentageof flap salvage was calculated for arterialand venous compromise combined. Patients withpreoperative values less than or equal to 200 experiencedthe highest levels of salvage success (71percent), whereas those patients with preoperativevalues approaching or beyond 300 experiencedthe lowest rates of salvage. Figure 4 alsosuggests that those who experience venous thrombosistend to have higher preoperative plateletvalues than those who experience arterial thrombosis.DISCUSSIONThis study represents one of the largest takebackseries in the published literature. The overallflap salvage rate was 49 percent. The rates of salvagefor arterial and venous compromise were 52and 46 percent, respectively. It is difficult to compareour salvage rate to the few other series ontake-backs because we chose to exclusively examinemicrovascular compromise rather than includegeneral complications (e.g., hematoma). Inexclusively examining thrombosis, Vijan and Transimilarly published a 55 percent salvage rate in 18breast reconstruction take-backs. 14583
Plastic and Reconstructive Surgery • September <strong>2012</strong>Table 2. Analysis of Perioperative Factors Associated with Successful SalvageSalvage (%) Failure (%) pTotal no. flaps 24 23Patient demographicsMean age at surgery 51.5 50.9 0.99COPD 1 (2.1) 0 (0) 1Diabetes 2 (4.3) 4 (17.4) 0.46Mean BMI 28.7 29 0.68Hypertension 4 (<strong>16</strong>.7) 10 (43.5) 0.05Dyslipidemia 2 (4.3) 4 (17.4) 0.40Smoking statusFormer 10 6Current 5 6 0.77Current smoker 5 (20.8) 6 (26) 0.61Thrombophilia (positive historyand/or laboratory testing) 1 (2.1) 8 (34.8) 0.01Mean hemoglobin 9.7 9.64 0.56Mean platelets* 194 289 0.01Perioperative settingMean hours until take-back 35.3 70.1 0.02Hospital (community vs. academic) 3 community (12.5) 1 community (4.3) 0.60Breast vs. head and neck vs. lower extremityBreast 19 17Head and neck 4 5Lower extremity 1 1 0.90Breast vs. nonbreast 19 breast (79.2) 17 breast (73.9) 0.74Preoperative XRT 10 (37) 11 (47.8) 0.44Intraoperative thrombosis† 1 (2.1) 2 (8.7) 0.60Loss of Doppler signal 13 (54.2) 10 (43.5) 0.56COPD, chronic obstructive pulmonary disease; BMI, body mass index; XRT, radiation therapy.*Platelet counts from preoperative laboratory tests before take-back.†Intraoperative thrombosis during initial surgery.Table 3. Binary Logistic Regression Analysisof Factors That Were Significant followingUnivariate AnalysisOdds Ratio 95% CI pMean time until take-back 1.0 0.99–1.03 0.<strong>09</strong>Thrombophilia 10.9 0.87–138 0.06Preoperative platelets 1.0 0.99–1.03 0.05CI, confidence interval.The mean time until take-back was significantlydifferent between those flaps that failed andthose flaps that were salvageable. The mean timeuntil take-back was nearly twice as long in thefailure group in comparison with the salvagegroup (35.3 and 70.1 hours, respectively; p 0.02). We chose to define time until take-back asthe number of hours from the end of the initialprocedure to the start of the take-back. This waschosen rather than attempting to examine thetime from thrombosis to take-back. Even withmeticulous documentation and vigilant flap observation,these values are neither reliably accuratenor precise enough for scientific scrutiny.Operating room start and end times allowed formore definitive values while still providing insightand utility. Furthermore, our intention was to providepractical data for use by other microsurgeonsto predict the likelihood of flap salvage. In theclinical setting, there often exists the same frustrationand ambiguity regarding the exact time atwhich thrombosis occurred. By examining thesedata, surgeons can more objectively identify thetime from the end of the initial operation until thestart of the salvage attempt.Interestingly, it seems that flaps undergoing atake-back on later postoperative days have lowerrates of salvage even when it is thought that thevascular compromise was readily detected (Table1 and Fig. 3). In another large series of pediclethromboses, Panchapakesan et al. noted that despiteseemingly timely intervention for all cases ofvascular compromise, the time from surgery tosalvage was a significant factor. 12 There are twopossible explanations for this: (1) thrombosismost often occurs early and these late salvage attemptsare nearly all cases of delayed detection;and (2) late thrombosis is inherently more devastatingor difficult to correct even with a promptreturn to the operating room. Perhaps both of theaforementioned explanations contribute to lowsalvage rates in very late take-backs. We were unableto salvage any flaps beyond postoperative day4, and Kroll et al. could not salvage flaps beyondpostoperative day 3. 10584
Volume 130, Number 3 • Free Flap Take-BackTable 4. Class 2b Subgroup Analysis of Perioperative Factors Associated with Successful SalvageSalvage (%) Failure (%) pTotal no. flaps 21 15Patient demographicsAge at surgery 50.9 48.3 0.80COPD 1 (4.8) 0 (0) 1Diabetes 2 (9.5) 2 (13.3) 1Mean BMI 27.8 30.2 0.29Hypertension 4 (19) 5 (33.3) 0.43Dyslipidemia 2 (9.5) 3 (20) 0.36Smoking statusFormer 8 4Current 5 5 0.72Current smokers 5 (23.8) 5 (33.3) 1Thrombophilia (positive historyand/or laboratory testing) 1 (4.8) 3 (20) 0.18Mean hemoglobin 9.8 9.7 0.65Mean platelets* 200 252 0.05Perioperative settingMean hours until take-back 34.9 46.3 0.24Hospital 3 community (14.3) 1 community (6.7) 0.62Breast vs. head and neck vs. lower extremityBreast 17 12Head and neck 3 2Lower extremity 1 1 0.96Breast vs. nonbreast 17 (80.9) 12 (80) 1Preoperative XRT 8 (38) 5 (33.3) 1Intraoperative thrombosis† 1 (4.8) 2 (13.3) 0.55Vein vs. artery 10 vein, 11 artery 9 vein, 5 artery, 1 both 0.30COPD, chronic obstructive pulmonary disease; BMI, body mass index; XRT, radiation therapy.*Platelet counts from preoperative laboratory tests before take-back.†Intraoperative thrombosis during initial surgery.Table 5. Analysis of Intraoperative Factors and Maneuvers for Association with Successful SalvageManeuver UsedManeuver Not UsedNo. (%) Salvage Rate No. (%) Salvage Rate pSurgeon experience (5 yr practice) 10 (28) 90% 26 (72) 62% 0.005Intraoperative heparin anticoagulation 20 (56) 67% <strong>16</strong> (44) 17% 0.06Use of thrombolytics 23 (64) 57% 13 (36) 62% 1Type of thrombolytics 0.24tPA 4 6Urokinase 8 2Streptokinase 1 2Unable to remove a thrombus in its entirety 6 (17) 17% 30 (83) 67% 0.06New anastomotic site 4 (11) 50% 32 (89) 59% 1Vein grafting 23 (64) 61% 13 (46) 54% 0.73tPA, tissue plasminogen activator.In plotting the take-back time and successrates for venous versus arterial compromise,some interesting observations were made. First,our results are in accordance with those of Krollet al., who suggested that most thrombi occurwithin the first 24 hours. Second, arterial compromiseappeared to be correctable at muchhigher rates in comparison with venous compromise,particularly in the first 48 hours (77percent arterial salvage rate versus 50 percentvenous salvage rate). It has been speculated thatthis is in part because of the difficulty in detectingloss of venous flow with routine Doppler systems.The complete loss of the Doppler signal iseasier to recognize rather than the monophasic,“water-hammer” signal unique to loss of venousflow. Furthermore, animal studies have demonstratedthat skin change may be an unreliable anduntimely clinical detector for the severity of venouscongestion. 15 It seems, however, that any potentialdelay in detection with venous compromise cannotfully explain the large discrepancy in salvage rates.Perhaps the interstitial edema and physiologic microvascularchange resulting from severe venouscongestion is a far less reversible state than a temporaryloss of arterial inflow. As a result, the damage585
Plastic and Reconstructive Surgery • September <strong>2012</strong>Fig. 4. The platelet values are contrasted. Four have been excluded because reliable preoperative platelet values were notavailable. The rates provided on the right side of the figure represent salvage rates for each respective range of platelets.incurred from venous failure may be more swift anddefinite.In examining Table 1, the salvage rates declinewhen examining arterial loss and all flaps combined;however, this linear decline is not observedwith venous compromise. When finely dichotomizingthese data by individual day and type ofvascular compromise, all statistical significance islost (Table 1). We then constructed Figure 3,which groups flaps by 48-hour time intervalsrather than by 24-hour time periods. Figure 3 suggeststhat the salvage rate of venous compromiseactually improved in the later 45- to 96-hour postoperativeperiod. There is likely a multifactorialexplanation. First, this could simply be a matter ofinadequate study power, as it should be emphasizedthat this observation was not statistically significant.It has, however, been speculated that veryearly venous thrombosis is a more ominous sign incomparison with later venous thrombosis. Thisfinding of improved venous compromise salvagein the 45- to 96-hour time period can also be anartifact of our choice to use time until take-back(as opposed to time from thrombosis to take-back)and the fact that venous thromboses tend to occurlater than arterial thromboses. Thus, the sharpdecline in arterial salvage rate could be explainedby the fact that most arterial thromboses occur inthe first 24 hours and that later take-backs in the45- to 96-hour time period were likely more amatter of delayed intervention, leading to a sharpdecline for arterial thrombosis salvage.In addition to improving statistical analysis,Figure 3 represents critical changes in postoperativemonitoring. After 48 hours postoperatively,flap monitoring becomes every-4-hour Dopplerchecks, and after 96 hours patients are most oftendischarged. At each of these time intervals in Figure3, the salvage rate generally declines. Clearly,there are multiple reasons why salvage rates decline(particularly in how we defined time untiltake-back); however, one may reason that the declinein salvage rate could be strongly associatedwith these essential changes in flap monitoring.With our current flap monitoring protocol, flapsonly undergo Doppler checks every 4 hours beyond48 hours postoperatively, but clearly issuescan still arise in this time period. In fact, there wasa relatively equal distribution of take-backs on days2, 3, and 4. As seen in Figure 1, at least eight flapswere necrotic by the time the flap was elevated. Inaddition, authors who have attempted to monitor586
Volume 130, Number 3 • Free Flap Take-Backthe time from thrombosis to salvage have stressedthe seemingly small time window separating successfrom failure. In the study by Vijan and Tran, 14the mean time of successful salvage and failure was127 minutes and 192 minutes, respectively (thelatest flap they were able to salvage was 188 minutesafter detection of thrombosis). Along with theaforementioned study by Vijan and Tran, our datacould insinuate that Doppler checks every 4 hoursare insufficient, and now with Doppler monitoring,our time interval for monitoring does notexceed every 2 hours at any point prior to discharge.Yet, checks every 1 to 2 hours for over 96hours would be an arduous task for the floornurses, thus making the call to other methods ofmonitoring. While our data are not conclusive,they should be the impetus for questioning theefficacy of the standard Doppler monitoring protocoland perhaps the previously underestimatedrole of constant monitoring techniques.Systems more sophisticated than hand-heldDoppler probes have been described in the literature,including near-infrared spectroscopy, microdialysis,and laser Doppler flowmetry. Therehas been conflicting evidence as to whether implantableDoppler probes improve the salvagerate. 11,<strong>16</strong>,17 A recent study by Lin et al. claims animproved salvage rate from 57.7 percent to 93.75percent with tissue oximetry monitoring. 18 Perhapsutilization of these more sensitive measurestruly leads to higher rates of salvage, as animalstudies have demonstrated that changes at themicrovascular level begin as early as 60 minutesafter ischemia. 19Even still, our data indicate that intrinsic factorsof the patient may be at least as important,regardless of the timing of the take-back. Accordingly,in moving beyond the long-established andintuitive matter regarding the timing of the takeback,our data are the first to provide level IIIevidence to establish that it is also dependent onwho is undergoing salvage and how it is done. Patientswith a known thrombophilia were poor candidatesfor take-back procedures. Seven of eightpatients with a thrombophilia ultimately failed thesalvage attempt. It is also worth noting that the onepatient whose flap was salvaged had the “softest”history of hypercoagulability and no laboratoryconfirmation of a blood disorder. Patients with aknown thrombophilia may not be contraindicatedfor free tissue transfer, but they should be stronglycounseled as to the grim prognosis of postoperativethrombosis.Although named hypercoagulable states (e.g.,protein C deficiency) are difficult to detect, ourdata suggest that preoperative platelet values maybe a simple and reliable routine laboratory valuethat could predict the ability to salvage a flap.Preoperative platelet values were significantlyhigher in those who underwent a failed salvageattempt (Fig. 4). Interestingly, this may also befurther evidence to suggest that platelets play acritical role in the physiology of thrombosis, ischemia,and reperfusion injury.It has been long established that platelets canbe the source of microemboli that travel downstreamfrom an arterial anastomosis to disruptcapillary perfusion. 20 Rather than just the physicaleffects of platelets on the microcirculation, plateletsappear to cause deleterious effects on the microvasculatureby chemical means as well. Clinicaland laboratory studies from the cardiovascular literaturehave elucidated the critical role that plateletsplay in myocardial ischemia-perfusion injury.These studies on myocardium have found thatplatelets cause damage to microvasculature inways including but not limited to (1) releasingvasoconstrictive substances (e.g., thromboxaneA2, serotonin), (2) potentiating the inflammatorycascade [e.g., release interleukin-1, RANTES(regulated upon activation, normal T-cell expressed,and secreted), or CD40 ligand], (3) activatingand adhering to leukocytes, and (4) releasingoxygen free radicals and thrombin. 21Our data further suggest that platelets play arole in tissue injury following thrombosis and, furthermore,that platelets may be a worthwhile therapeutictarget during flap salvage. An animal studyby Peter et al. demonstrated that the pretreatmentof aspirin resulted in decreased thrombus formationat the anastomosis and increased downstreamcapillary perfusion. By reducing thromboxane A2formation (a platelet aggregator and vasoconstrictor),low-dose aspirin has demonstrated potentialbenefits in the setting of flap salvage. 22,23 Even still,aspirin has a limited ability to modulate plateletactivity; perhaps adenosine diphosphate receptorantagonists (clopidogrel or faster acting cangrelor)may be more efficacious. 21Previous laboratory studies have compared theeffects of fish oil versus systemic heparin on plateletmicroemboli. Heparin reduced the number ofemboli but did not improve capillary perfusion.Conversely, neither fish oil nor ridogrel reducedthe number of platelet emboli, but both improvedcapillary perfusion. Their conclusion, whichseems to have since been validated by the aforementionedcardiovascular literature, is that plateletsalso play a substantial biochemical role indecreased capillary perfusion. 22,24 In our series,587
Plastic and Reconstructive Surgery • September <strong>2012</strong>intraoperative heparin use was associated with improvedoutcomes, perhaps by decreasing the physicalpresence of platelet microemboli in the microcirculation.Evidence of physical emboli in themicrocirculation seems to be emphasized with thesuccessful infusion of thrombolytics. During a successfulinfusion, the real-time change in Dopplersignal and decrease in syringe pressure (microvascularresistance) suggest the clearance of aphysical obstruction. 13In an attempt to identify efficacious intraoperativemaneuvers for cases of delayed microvascularthrombosis, the class 2b subgroup analysiswas performed. Including class 2a or 2c patientswould have precluded a reasonable analysis of intraoperativemaneuvers. Consequently, this createda more homogenous subgroup of delayedmicrovascular thromboses, all of which appearedto be viable after flap elevation and likely returnedto the operating room in a timelier manner thanthe class 2c counterparts (notice that the timeuntil take-back is no longer significant in the class2b subgroup analysis; Table 4). In this subgroupanalysis, surgeon experience was highly significant.Given the infrequency of take-backs, particularlythose that are the result of a thrombosis,many years of high-volume microsurgery are requiredto obtain any reasonable level of experiencewith this scenario. It should also be noted,however, that the most senior surgeon has thehighest volume of breast microsurgery, and thishas been demonstrated to result in higher rates ofsalvage than head/neck or lower extremity cases. 25It should also be noted that this most senior surgeonmost liberally uses aspirin in the perioperativeperiod.Given the paucity of evidence-based data forsuccessful salvage, expert opinion and experienceare seemingly paramount to success, along withtechnical proficiency. The importance of the technicalexpertise is demonstrated, as the mechanicalremoval of a thrombus, in its entirety, also trendedstrongly toward significance (p 0.06). Understandably,this is associated with success, as residualclot may be the nidus for another large thrombosisor potentially the source of microemboli.Unfortunately, we were unable to glean dataon the efficacy of thrombolytics for salvage. Theseclinical data will continue to be difficult to obtainbecause of study power and, moreover, the factthat thrombolytics are preferentially used in moredifficult cases of salvage. 26,27 Even more difficult todemonstrate is a difference in efficacy betweenstreptokinase (which enhances plasminogen toplasmin conversion), urokinase (which directlyconverts plasminogen), or tissue plasminogen activator(which directly converts plasminogen).Nonetheless, we feel strongly about their role insalvage, particularly for recalcitrant cases of ischemia/congestion,and their effects are often readilyapparent intraoperatively. The same can be saidfor other intraoperative factors such as anastomoticsite change, use of a Fogarty catheter, orvein grafting. The low power and selection biasmakes their efficacy difficult to determine.One of the weaknesses of this study is the heterogeneityof the flap type and patient population.This is the constant dilemma of clinical research—study population homogeneity versus study power.With over 2000 free flaps, there are still likely somecomponents of our study that our underpowered.Removing all nonbreast cases would likely makethe entire study underpowered. To be sure, we didnot find nonbreast cases to be a risk factor in ourpatient population, as we examined breast versusnonbreast cases and breast versus head/neck versuslower extremity cases. Because this is not a riskfactor on univariate analysis, there is no compellingcase from a statistical standpoint to removethe head/neck and lower extremity patients. Perhaps,as our data suggest, these flaps truly aresalvaged at equivalent rates. At the very least, it isnot a risk factor in our patient population; therefore,we do not feel compelled to remove thesepatients from our study. Many of the factors weidentified (e.g., surgeon experience or thrombophilia)are likely relevant regardless of flap type orsite of reconstruction.CONCLUSIONSTo achieve the highest levels of success in microsurgery,it is necessary to improve rates of salvagefollowing delayed microvascular compromise.There is evidence to suggest that there arepreoperative factors that are predictive of flap salvagesuccess, including the time until take-back,preoperative platelet values, and the presence ofthrombophilia. Shorter time to take-back and surgeonexperience may improve salvage, and intraoperativeheparin anticoagulation and completemechanical removal of the thrombus demonstratepreliminary evidence as effective intraoperativestrategies.Liza C. Wu, M.D.Division of Plastic Surgery10 Penn Tower3400 Spruce StreetPhiladelphia, Pa. 19104liza.wu@uphs.upenn.edu588
Volume 130, Number 3 • Free Flap Take-BackREFERENCES1. Blondeel PN. One hundred free DIEP flap breast reconstructions:A personal experience. Br J Plast Surg. 1999;52:104–111.2. Saint-Cyr M, Chang DW, Robb GL, Chevray PM. Internalmammary perforator recipient vessels for breast reconstructionusing free TRAM, DIEP, and SIEA flaps. Plast ReconstrSurg. 2007;120:1769–1773.3. Knight MA, Nguyen DT IV, Kobayashi MR, Evans GR. Institutionalreview of free TRAM flap breast reconstruction. AnnPlast Surg. 2006;56:593–598.4. Gill PS, Hunt JP, Guerra AB, et al. A 10-year retrospectivereview of 758 DIEP flaps for breast reconstruction. PlastReconstr Surg. 2004;113:1153–1<strong>16</strong>0.5. Nahabedian MY, Momen B, Galdino G, Manson PN. Breastreconstruction with the free TRAM or DIEP flap: Patientselection, choice of flap, and outcome. Plast Reconstr Surg.2002;110:466–475; discussion 476–477.6. Enajat M, Rozen WM, Whitaker IS, Smit JM, Acosta R. Asingle center comparison of one versus two venous anastomosesin 564 consecutive DIEP flaps: Investigating the effecton venous congestion and flap survival. Microsurgery 2010;30:185–191.7. Blondeel PN, Arnstein M, Verstraete K, et al. Venous congestionand blood flow in free transverse rectus abdominismyocutaneous and deep inferior epigastric perforator flaps.Plast Reconstr Surg. 2000;106:1295–1299.8. Disa JJ, Cordeiro PG, Hidalgo DA. Efficacy of conventionalmonitoring techniques in free tissue transfer: An 11-yearexperience in 750 consecutive cases. Plast Reconstr Surg. 1999;104:97–101.9. Vega S, Smartt JM Jr, Jiang S, et al. 500 consecutive patientswith free TRAM flap breast reconstruction: A single surgeon’sexperience. Plast Reconstr Surg. 2008;122:329–339.10. Kroll SS, Schusterman MA, Reece GP, et al. Timing of pediclethrombosis and flap loss after free-tissue transfer. Plast ReconstrSurg. 1996;98:1230–1233.11. Smit JM, Werker PM, Liss AG, et al. Introduction of theimplantable Doppler system did not lead to an increasedsalvage rate of compromised flaps: A multivariate analysis.Plast Reconstr Surg. 2010;125:1710–1717.12. Panchapakesan V, Addison P, Beausang E, Lipa JE, GilbertRW, Neligan PC. Role of thrombolysis in free-flap salvage.J Reconstr Microsurg. 2003;19:523–529.13. Serletti JM, Moran SL, Orlando GS, O’Connor T, HerreraRH. Urokinase protocol for free-flap salvage following prolongedvenous thrombosis. Plast Reconstr Surg. 1998;102:1947–1953.14. Vijan SS, Tran NV. Microvascular breast reconstruction pediclethrombosis: How long can we wait? Microsurgery 2007;27:544–547.15. Russell JA, Conforti ML, Connor NP, Hartig GK. Cutaneoustissue flap viability following partial venous obstruction. PlastReconstr Surg. 2006;117:2259–2266; discussion 2267–2268.<strong>16</strong>. Kind GM, Buntic RF, Buncke GM, Cooper TM, Siko PP,Buncke HJ Jr. The effect of an implantable Doppler probeon the salvage of microvascular tissue transplants. Plast ReconstrSurg. 1998;101:1268–1273; discussion 1274–1275.17. Paydar KZ, Hansen SL, Chang DS, Hoffman WY, Leon P.Implantable venous Doppler monitoring in head and neckfree flap reconstruction increases the salvage rate. Plast ReconstrSurg. 2010;125:1129–1134.18. Lin SJ, Nguyen MD, Chen C, et al. Tissue oximetry monitoringin microsurgical breast reconstruction decreases flaploss and improves rate of flap salvage. Plast Reconstr Surg.2011;127:1080–1085.19. Gabriel A, Chaney N, Stephenson LL, Zamboni WA. Effectof total venous occlusion on capillary flow and necrosis inskeletal muscle. Plast Reconstr Surg. 2001;108:430–433.20. Barker JH, Acland RD, Anderson GL, Patel J. Microcirculatorydisturbances following the passage of emboli in an experimentalfree-flap model. Plast Reconstr Surg. 1992;90:95–102; discussion 103–104.21. Barrabés JA, Inserte J, Agulló L, Alonso A, Mirabet M, Garcia-Dorado D. Microvascular thrombosis: An exciting but elusivetherapeutic target in reperfused acute myocardial infarction.Cardiovasc Hematol Disord Drug Targets 2010;10:273–283.22. Peter FW, Franken RJ, Wang WZ, et al. Effect of low doseaspirin on thrombus formation at arterial and venous microanastomosesand on the tissue microcirculation. Plast ReconstrSurg. 1997;99:1112–1121.23. Ashjian P, Chen CM, Pusic A, Disa JJ, Cordeiro PG, MehraraBJ. The effect of postoperative anticoagulation on microvascularthrombosis. Ann Plast Surg. 2007;59:36–39; discussion39–40.24. Barker JH, Gu JM, Anderson GL, et al. The effects of heparinand dietary fish oil on embolic events and the microcirculationdownstream from a small-artery repair. Plast ReconstrSurg. 1993;91:335–343.25. Smit JM, Acosta R, Zeebregts CJ, Liss AG, Anniko M, HartmanEH. Early reintervention of compromised free flapsimproves success rate. Microsurgery 2007;27:612–6<strong>16</strong>.26. Tran NV, Bishop AT, Convery PA, Yu AY. Venous congestiveflap salvage with subcutaneous rtPA. Microsurgery 2006;26:370–372.27. Yii NW, Evans GR, Miller MJ, et al. Thrombolytic therapy:What is its role in free flap salvage? Ann Plast Surg. 2001;46:601–604.589
EBM SPECIAL TOPICThe Levels of Evidence and Their Role inEvidence-Based MedicinePatricia B. Burns, M.P.H.Rod J. Rohrich, M.D.Kevin C. Chung, M.D., M.S.Ann Arbor, Mich.; and Dallas, TexasAs the name suggests, evidence-based medicineis about finding evidence and usingthat evidence to make clinical decisions. Acornerstone of evidence-based medicine is the hierarchicalsystem of classifying evidence. This hierarchyis known as the levels of evidence. Physiciansare encouraged to find the highest level ofevidence to answer clinical questions. Several articlespublished in plastic surgery journals concerning evidence-basedmedicine topics have touched on thissubject. 1–6 Specifically, previous articles have discussedthe lack of higher level evidence in Plastic andReconstructive Surgery and the need to improve theevidence published in the Journal. Before that can beaccomplished, it is important to understand the historybehind the levels and how they should be interpreted.This article focuses on the origin of levelsof evidence, their relevance to the evidence-basedmedicine movement, and the implications for thefield of plastic surgery and the everyday practice ofplastic surgery.HISTORY OF LEVELS OF EVIDENCEThe levels of evidence were originally describedin a report by the Canadian Task Force onthe Periodic Health Examination in 1979. 7 Thereport’s purpose was to develop recommendationson the periodic health examination and basethose recommendations on evidence in the medicalliterature. The authors developed a system ofrating evidence (Table 1) when determining theeffectiveness of a particular intervention. The evidencewas taken into account when grading recommendations.For example, a grade A recommendationwas given if there was good evidence toFrom the Section of Plastic Surgery, Department of Surgery,University of Michigan Health System, and the Departmentof Plastic Surgery, University of Texas Southwestern MedicalCenter.Received for publication February 2, 2011; accepted March10, 2011.Copyright ©2011 by the American Society of Plastic SurgeonsDOI: 10.1<strong>09</strong>7/PRS.0b013e318219c171support a recommendation that a condition beincluded in the periodic health examination. Thelevels of evidence were further described and expandedby Sackett 8 in an article on levels of evidencefor antithrombotic agents in 1989 (Table2). Both systems place randomized controlledtrials at the highest level and case series or expertopinions at the lowest level. The hierarchies rankstudies according to the probability of bias. Randomizedcontrolled trials are given the highestlevel because they are designed to be unbiased andhave less risk of systematic errors. For example, byrandomly allocating subjects to two or more treatmentgroups, these types of studies also randomizeconfounding factors that may bias results. A caseseries or expert opinion is often biased by theauthor’s experience or opinions, and there is nocontrol of confounding factors.MODIFICATION OF LEVELSSince the introduction of levels of evidence,several other organizations and journals have adoptedvariations of the classification system. Diversespecialties are often asking different questions,and it was recognized that the type and levelof evidence needed to be modified accordingly.Research questions are divided into the followingcategories: treatment, prognosis, diagnosis, andeconomic/decision analysis. For example, Table 3shows the levels of evidence developed by theAmerican Society of Plastic Surgeons for prognosis 9and Table 4 shows the levels developed by the Centrefor Evidence-Based Medicine for treatment. 10 Thetwo tables highlight the types of studies that areappropriate for the question (prognosis versustreatment) and how quality of data is taken intoaccount when assigning a level. For example, ran-Disclosure: The authors have no financial intereststo declare in relation to the content of thisarticle.www.PRSJournal.com 305
Plastic and Reconstructive Surgery • July 2011Table 1. Canadian Task Force on the Periodic HealthExamination’s Levels of Evidence*LevelIII.1II.2IIIType of EvidenceAt least 1 RCT with proper randomizationWell-designed cohort or case-control studyTime series comparisons or dramatic resultsfrom uncontrolled studiesExpert opinionsRCT, randomized controlled trial.*Adapted from Canadian Task Force on the Periodic Health Examination.The periodic health examination. Can Med Assoc J. 1979;121:1193–1254.Table 2. Levels of Evidence from Sackett*LevelType of EvidenceILarge RCTs with clear-cut resultsIISmall RCTs with unclear resultsIIICohort and case-control studiesIVHistorical cohort or case-control studiesVCase series, studies with no controlsRCTs, randomized controlled trials.*Adapted from Sackett DL. Rules of evidence and clinical recommendationson the use of antithrombotic agents. Chest 1989;95:2S–4S.Table 3. Levels of Evidence for Prognostic Studies*LevelIIIIIIIVVType of EvidenceHigh-quality prospective cohort study with adequatepower or systematic review of these studiesLesser quality prospective cohort, retrospectivecohort study, untreated controls from an RCT, orsystematic review of these studiesCase-control study or systematic review of thesestudiesCase seriesExpert opinion; case report or clinical example;or evidence based on physiology, bench research,or “first principles”RCT, randomized controlled trial.*Adapted from the American Society of Plastic Surgeons. Availableat: http://www.plasticsurgery.org/For_Medical-Professionals/Legislationand-Advocacy/Health-Policy-Resources/Evidence-based-GuidelinesPractice-Parameters/Description-and-Development-of-Evidence-based-Practice-Guidelines/ASPS-Evidence-Rating-Scales.html. Accessed December17, 2010.domized controlled trials are not appropriatewhen looking at the prognosis of a disease. Thequestion in this instance is, “What will happen ifwe do nothing at all?” Because a prognosis questiondoes not involve comparing treatments, thehighest evidence would come from a cohort studyor a systematic review of cohort studies. The levelsof evidence also take into account the quality ofthe data. For example, in the chart from the Centrefor Evidence-Based Medicine, a poorly designedrandomized controlled trial has the samelevel of evidence as a cohort study.A grading system that provides strength of recommendationsbased on evidence has also changedTable 4. Levels of Evidence for Therapeutic Studies*LevelType of Evidence1a Systematic review (with homogeneity) of RCTs1b Individual RCT (with narrow confidence intervals)1c All-or-none study2a Systematic review (with homogeneity) of cohortstudies2b Individual cohort study, including low-quality RCTs(e.g., 80% follow-up)2c “Outcomes” research; ecological studies3a Systematic review (with homogeneity) ofcase-control studies3b Individual case-control study4 Case series (and poor quality cohort andcase-control study)5 Expert opinion without explicit critical appraisalor based on physiology, bench research,or “first principles”RCT, randomized controlled trial.*From the Centre for Evidence-Based Medicine (Web site). Availableat: http://www.cebm.net. Accessed December 17, 2010.over time. Table 5 shows the Grade Practice Recommendationsdeveloped by the American Societyof Plastic Surgeons. The grading system providesan important component in evidence-basedmedicine and assists in clinical decision making.For example, a strong recommendation is givenwhen there is level I evidence and consistent evidencefrom level II, III, and IV studies available.The grading system does not degrade lower levelevidence when deciding recommendations if theresults are consistent.INTERPRETATION OF LEVELSMany journals assign a level to the articles theypublish, and authors often assign a level whensubmitting an abstract to conference proceedings.This allows the reader to know the level of evidenceof the research, but the designated level ofevidence does always guarantee the quality of theresearch. It is important that readers not assumethat level I evidence is always the best choice orappropriate for the research question. This conceptwill be very important for all of us to understandas we evolve into the field of evidence-basedmedicine in plastic surgery. By design, our designatedsurgical specialty will always have importantarticles that may have a lower level of evidencebecause of the level of innovation and techniquearticles that are needed to move our surgical specialtyforward.Although randomized controlled trials are oftenassigned the highest level of evidence, not allrandomized controlled trials are conducted properly,and the results should be scrutinized carefully.Sackett 8 stressed the importance of estimatingtypes of errors and the power of studies when306
Volume 128, Number 1 • Levels of EvidenceTable 5. Grade Practice Recommendations*Grade Descriptor Qualifying Evidence Implications for PracticeA StrongLevel I evidence or consistent Clinicians should follow a strong recommendationrecommendation findings from multipleunless a clear and compelling rationale for anstudies of levels II, III, or IVB Recommendation Levels II, III, or IV evidenceand findings are generallyconsistentC Option Levels II, III, or IV evidence,but findings are inconsistentD Option Level V evidence: little or nosystematic empiricalevidencealternative approach is presentGenerally, clinicians should follow arecommendation but should remain alert to newinformation and sensitive to patient preferencesClinicians should be flexible in their decision-makingregarding appropriate practice, although they mayset bounds on alternatives; patient preferenceshould have a substantial influencing roleClinicians should consider all options in theirdecision making and be alert to new publishedevidence that clarifies the balance of benefit vs.harm; patient preference should have a substantialinfluencing role*From the American Society of Plastic Surgeons. Evidence-based clinical practice guidelines. Available at: http://www.plasticsurgery.org/For-Medical-Professionals/Legislation-and-Advocacy/Health-Policy-Resources/Evidence-based-GuidelinesPractice-Parameters/Description-and-Development-of-Evidence-based-Practice-Guidelines/ASPS-Grade-Recommendation-Scale.html. Accessed March 3, 2011.interpreting results from randomized controlledtrials. For example, a poorly conducted randomizedcontrolled trial may report a negative resultbecause of low power when in fact a real differenceexists between treatment groups. Scales suchas the Jadad scale have been developed to judgethe quality of randomized controlled trials. 11 Althoughphysicians may not have the time or inclinationto use a scale to assess quality, there aresome basic items that should be taken into account.Items used for assessing randomized controlledtrials include randomization, blinding, adescription of the randomization and blindingprocess, a description of the number of subjectswho withdrew or dropped out of the study, theconfidence intervals around study estimates, anda description of the power analysis. For example,Bhandari et al. 12 published an article assessing thequality of surgical randomized controlled trials.The authors evaluated the quality of randomizedcontrolled trials reported in the Journal of Bone andJoint Surgery from 1988 to 2000. Articles with ascore of greater than 75 percent were deemedhigh quality, and 60 percent of the articles had ascore less than 75 percent. The authors identified72 randomized controlled trials during this timeperiod, and the mean score was 68 percent. Themain reason for the low-quality score was lack ofappropriate randomization, blinding, and a descriptionof patient exclusion criteria. Another articlefound the same quality score of articles in theJournal of Bone and Joint Surgery with a level 1 ratingcompared with level 2. 13 Therefore, one shouldnot assume that level 1 studies are of higher qualitythan level 2 studies.A resource for surgeons to use when appraisinglevels of evidence are the users’ guides publishedin the Canadian Journal of Surgery 14,15 andthe Journal of Bone and Joint Surgery. <strong>16</strong> Similar articlesthat are not specific to surgery have beenpublished in the Journal of the American MedicalAssociation. 17,18PLASTIC SURGERY AND EVIDENCE-BASED MEDICINEThe field of plastic surgery has been slow toadopt evidence-based medicine. This was demonstratedin an article examining the level of evidenceof articles published in Plastic and ReconstructiveSurgery. 19 The authors assigned levels ofevidence to articles published in Plastic and ReconstructiveSurgery over a 20-year period. The majorityof studies (93 percent in 1983) were level IV or V,which denotes case series and case reports. Althoughthe results were disappointing, there wassome improvement over time. By 2003, there weremore level I studies (1.5 percent) and fewer levelIV and V studies (87 percent). A recent analysislooked at the number of level I studies in fivedifferent plastic surgery journals from 1978 to20<strong>09</strong>. The authors defined level I studies as randomizedcontrolled trials and meta-analyses andrestricted their search to these studies. The numberof level I studies increased from one in 1978to 32 by 20<strong>09</strong>. 20 From these results, we see that thefield of plastic surgery is improving the level ofevidence but still has a long way to go, especiallyin improving the quality of studies published. Forexample, approximately one-third of the studiesinvolved double blinding, but the majority did notrandomize subjects, describe the randomizationprocess, or perform a power analysis. Power analysisis another area of concern in plastic surgery.307
Plastic and Reconstructive Surgery • July 2011A review of the plastic surgery literature found thatthe majority of published studies have inadequatepower to detect moderate to large differences betweentreatment groups. 21 Regardless of the levelof evidence for a study, if the study is underpowered,the interpretation of results is questionable.Although the goal is to improve the overalllevel of evidence in plastic surgery, this does notmean that all lower level evidence should be discarded.Case series and case reports are importantfor hypothesis generation and can lead to morecontrolled studies. In addition, in the face of overwhelmingevidence to support a treatment, such asthe use of antibiotics for wound infections, thereis no need for a randomized controlled trial.CLINICAL EXAMPLES USING LEVELSOF EVIDENCETo understand how the levels of evidence workand aid the reader in interpreting levels, we providesome examples from the plastic surgery literature.The examples also show the peril of medicaldecisions based on results from case reports.An association was hypothesized between lymphomaand silicone breast implants based on casereports. 22–27 The level of evidence for case reports,depending on the scale used, is IV or V. These casereports were used to generate the hypothesis thata possible association existed. Because of theseresults, several large retrospective cohort studiesfrom the United States, Canada, Denmark, Sweden,and Finland were conducted. 28–32 The level ofevidence for a retrospective cohort study is II. Allof these studies had many years of follow-up for alarge number of patients. Some of the studiesfound an elevated risk and others found no risk forlymphoma. None of the studies reached statisticalsignificance. Therefore, higher level evidencefrom cohort studies does not provide evidence ofany risk of lymphoma. Finally, a systematic reviewwas performed that combined the evidence fromthe retrospective cohorts. 27 The results found anoverall standardized incidence ratio of 0.89 (95percent confidence interval, 0.67 to 1.18). Becausethe confidence interval includes 1, the resultsindicate there is no increased incidence. Thelevel of evidence for the systematic review is I.Based on the best available evidence, there is noassociation between lymphoma and silicone implants.This example shows how studies with a lowlevel of evidence were used to generate a hypothesis,which then led to higher level evidence thatdisproved the hypothesis. This example also demonstratesthat randomized controlled trials are notfeasible for rare events such as cancer and emphasizesthe importance of observational studiesfor a specific study question. A case-control studyis a better option and provides higher level evidencefor testing the prognosis of the long-termeffect of silicone breast implants.Another example is the injection of epinephrinein fingers. Based on case reports before 1950,physicians were advised that epinephrine injectioncan result in finger ischemia. 33 We see in thisexample that level IV or V evidence was acceptedas fact and incorporated into medical textbooksand teaching. However, not all physicians acceptedthis evidence and were performing injections of epinephrineinto the fingers, with no adverse effects onthe hand. Obviously, it was time for higher levelevidence to resolve this issue. An in-depth review ofthe literature from 1880 to 2000 by Denkler 33 identified48 cases of digital infarction, of which 21 hadbeen injected with epinephrine. Further analysisfound that the addition of procaine to the epinephrineinjection was the cause of the ischemia. 34 Theprocaine used in these injections included toxicacidic batches that were recalled in 1948. In addition,several cohort studies found no complicationsfrom the use of epinephrine in the fingers andhand. 35–37 The results from these cohort studies increasedthe level of evidence. Based on the bestavailable evidence from these studies, the hypothesisthat epinephrine injection will harm fingers was rejected.This example highlights the biases inherentin case reports. It also shows the risk when spuriousevidence is handed down and integrated into medicalteaching.OBTAINING THE BEST EVIDENCEWe have established the need for randomizedcontrolled trials to improve evidence in plastic surgerybut have also acknowledged the difficulties, particularlywith randomization and blinding. Althoughrandomized controlled trials may not be appropriatefor many surgical questions, well-designed and wellconductedcohort or case-control studies couldboost the level of evidence. Many of the currentstudies tend to be descriptive and lack a controlgroup. The way forward seems clear. Plastic surgeryresearchers need to consider using a cohort or casecontroldesign whenever a randomized controlledtrial is not possible. If designed properly, the level ofevidence for observational studies can approach orsurpass those from a randomized controlled trial. Insome instances, observational studies and randomizedcontrolled trials have yielded similar results. 38 Ifenough cohort or case-control studies become available,the prospect of systematic reviews of these stud-308
Volume 128, Number 1 • Levels of Evidenceies will increase, which will increase overall evidencelevels in plastic surgery.CONCLUSIONSThe levels of evidence are an important componentof evidence-based medicine. Understandingthe levels and why they are assigned to publicationsand abstracts helps the reader to prioritize information.This is not to say that all level IV evidenceshould be ignored and all level I evidence acceptedas fact. The levels of evidence provide aguide, and the reader needs to be cautious wheninterpreting these results.Kevin C. Chung, M.D., M.S.Section of Plastic SurgeryDepartment of SurgeryUniversity of Michigan Health System2130 Taubman Center, SPC 53401500 East Medical Center DriveAnn Arbor, Mich. 481<strong>09</strong>-5340kecchung@umich.eduACKNOWLEDGMENTSThis work was supported in part by a MidcareerInvestigator Award in Patient-Oriented Research (K24AR053120) from the National Institute of Arthritis andMusculoskeletal and Skin Diseases (to K.C.C.).REFERENCES1. McCarthy CM, Collins ED, Pusic AL. Where do we find thebest evidence? Plast Reconstr Surg. 2008;122:1942–1947; discussion1948–1951.2. Chung KC, Swanson JA, Schmitz D, Sullivan D, Rohrich RJ.Introducing evidence-based medicine to plastic and reconstructivesurgery. Plast Reconstr Surg. 20<strong>09</strong>;123:1385–1389.3. Chung KC, Ram AN. Evidence-based medicine: The fourthrevolution in American medicine? Plast Reconstr Surg. 20<strong>09</strong>;123:389–398.4. Rohrich RJ. So you want to be better: The role of evidencebasedmedicine in plastic surgery. Plast Reconstr Surg. 2010;126:1395–1398.5. Burns PB, Chung KC. Developing good clinical questionsand finding the best evidence to answer those questions. PlastReconstr Surg. 2010;126:613–618.6. Sprague S, McKay P, Thoma A. Study design and hierarchyof evidence for surgical decision making. Clin Plast Surg.2008;35:195–205.7. The periodic health examination. Canadian Task Force onthe Periodic Health Examination. Can Med Assoc J. 1979;121:1193–1254.8. Sackett DL. Rules of evidence and clinical recommendationson the use of antithrombotic agents. Chest 1989;95(2 Suppl):2S–4S.9. American Society of Plastic Surgeons. Scales for ratinglevels of evidence. Available at: http://www.plasticsurgery.org/Medical_Professionals/Health_Policy_and_Advocacy/Health_Policy_Resources/Evidence-based_GuidelinesPractice_Parameters/Description_and_Development_of_Evidence-based_Practice_Guidelines/ASPS_Evidence_Rating_Scales.html. AccessedDecember 17, 2010.10. Centre for Evidence Based Medicine (Web site). Available at:http://www.cebm.net. Accessed December 17, 2010.11. Jadad AR, Moore RA, Carroll D, et al. Assessing the qualityof reports of randomized clinical trials: Is blinding necessary?Control Clin Trials 1996;17:1–12.12. Bhandari M, Richards RR, Sprague S, Schemitsch EH. Thequality of reporting of randomized trials in the Journal of Boneand Joint Surgery from 1988 through 2000. J Bone Joint Surg Am.2002;84:388–396.13. Poolman RW, Struijs PA, Krips R, Sierevelt IN, Lutz KH,Bhandari M. Does a “Level I Evidence” rating imply highquality of reporting in orthopaedic randomised controlledtrials? BMC Med Res Methodol. 2006;6:44.14. Urschel JD, Goldsmith CH, Tandan VR, Miller JD. Users’guide to evidence-based surgery: How to use an article evaluatingsurgical interventions. Evidence-Based Surgery WorkingGroup. Can J Surg. 2001;44:95–100.15. Thoma A, Farrokhyar F, Bhandari M, Tandan V; Evidence-Based Surgery Working Group. Users’ guide to the surgicalliterature: How to assess a randomized controlled trial insurgery. Can J Surg. 2004;47:200–208.<strong>16</strong>. Bhandari M, Guyatt GH, Swiontkowski MF. User’s guide tothe orthopaedic literature: How to use an article about prognosis.J Bone Joint Surg Am. 2001;83:1555–1564.17. Guyatt GH, Sackett DL, Cook DJ. Users’ guides to the medicalliterature: II. How to use an article about therapy orprevention. A. Are the results of the study valid? Evidence-Based Medicine Working Group. JAMA 1993;270:2598–2601.18. Guyatt GH, Haynes RB, Jaeschke RZ, et al. Users’ Guides to theMedical Literature: XXV. Evidence-based medicine: Principlesfor applying the Users’ Guides to patient care. Evidence-BasedMedicine Working Group. JAMA 2000;284:1290–1296.19. Loiselle F, Mahabir RC, Harrop AR. Levels of evidence inplastic surgery research over 20 years. Plast Reconstr Surg.2008;121:207e–211e.20. McCarthy JE, Chatterjee A, McKelvey TG, Jantzen EM, KerriganCL. A detailed analysis of level I evidence (randomized controlledtrials and meta-analyses) in five plastic surgery journalsto date: 1978 to 20<strong>09</strong>. Plast Reconstr Surg. 2010;126:1774–1778.21. Chung KC, Kalliainen LK, Spilson SV, Walters MR, Kim HM.The prevalence of negative studies with inadequate statisticalpower: An analysis of the plastic surgery literature. Plast ReconstrSurg. 2002;1<strong>09</strong>:1–6; discussion 7–8.22. Newman MK, Zemmel NJ, Bandak AZ, Kaplan BJ. Primarybreast lymphoma in a patient with silicone breast implants:A case report and review of the literature. J Plast ReconstrAesthet Surg. 2008;61:822–825.23. Gaudet G, Friedberg JW, Weng A, Pinkus GS, Freedman AS.Breast lymphoma associated with breast implants: Two casereportsand a review of the literature. Leuk Lymphoma 2002;43:115–119.24. Sahoo S, Rosen PP, Feddersen RM, Viswanatha DS, Clark DA,Chadburn A. Anaplastic large cell lymphoma arising in asilicone breast implant capsule: A case report and review ofthe literature. Arch Pathol Lab Med. 2003;127:e115–e118.25. Keech JA Jr, Creech BJ. Anaplastic T-cell lymphoma in proximityto a saline-filled breast implant. Plast Reconstr Surg.1997;100:554–555.26. Duvic M, Moore D, Menter A, Vonderheid EC. CutaneousT-cell lymphoma in association with silicone breast implants.J Am Acad Dermatol. 1995;32:939–942.27. Lipworth L, Tarone RE, McLaughlin JK. Breast implants andlymphoma risk: A review of the epidemiologic evidencethrough 2008. Plast Reconstr Surg. 20<strong>09</strong>;123:790–793.3<strong>09</strong>
Plastic and Reconstructive Surgery • July 201128. Lipworth L, Tarone RE, Friis S, et al. Cancer among Scandinavianwomen with cosmetic breast implants: A pooledlong-term follow-up study. Int J Cancer 20<strong>09</strong>;124:490–493.29. Deapen DM, Hirsch EM, Brody GS. Cancer risk among LosAngeles women with cosmetic breast implants. Plast ReconstrSurg. 2007;119:1987–1992.30. Brisson J, Holowaty EJ, Villeneuve PJ, et al. Cancer incidencein a cohort of Ontario and Quebec women having bilateralbreast augmentation. Int J Cancer 2006;118:2854–2862.31. Pukkala E, Boice JD Jr, Hovi SL, et al. Incidence of breast andother cancers among Finnish women with cosmetic breastimplants, 1970-1999. J Long Term Eff Med Implants 2002;12:271–279.32. Brinton LA, Lubin JH, Burich MC, Colton T, Brown SL, HooverRN. Cancer risk at sites other than the breast following augmentationmammoplasty. Ann Epidemiol. 2001;11:248–256.33. Denkler K. A comprehensive review of epinephrine in the finger:To do or not to do. Plast Reconstr Surg. 2001;108:114–124.34. Thomson CJ, Lalonde DH, Denkler KA, Feicht AJ. A criticallook at the evidence for and against elective epinephrine usein the finger. Plast Reconstr Surg. 2007;119:260–266.35. Lalonde D, Bell M, Benoit P, Sparkes G, Denkler K, ChangP. A multicenter prospective study of 3,110 consecutive casesof elective epinephrine use in the fingers and hand: TheDalhousie Project clinical phase. J Hand Surg Am. 2005;30:1061–1067.36. Chowdhry S, Seidenstricker L, Cooney DS, Hazani R, WilhelmiBJ. Do not use epinephrine in digital blocks: Myth ortruth? Part II: A retrospective review of 1111 cases. PlastReconstr Surg. 2010;126:2031–2034.37. Wilhelmi BJ, Blackwell SJ, Miller JH, et al. Do not use epinephrinein digital blocks: Myth or truth? Plast Reconstr Surg.2001;107:393–397.38. Concato J, Shah N, Horwitz RI. Randomized, controlledtrials, observational studies, and the hierarchy of researchdesigns. N Engl J Med. 2000;342:1887–1892.310