Hematologic Malignancies - Siteman Cancer Center
Hematologic Malignancies - Siteman Cancer Center
Hematologic Malignancies - Siteman Cancer Center
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
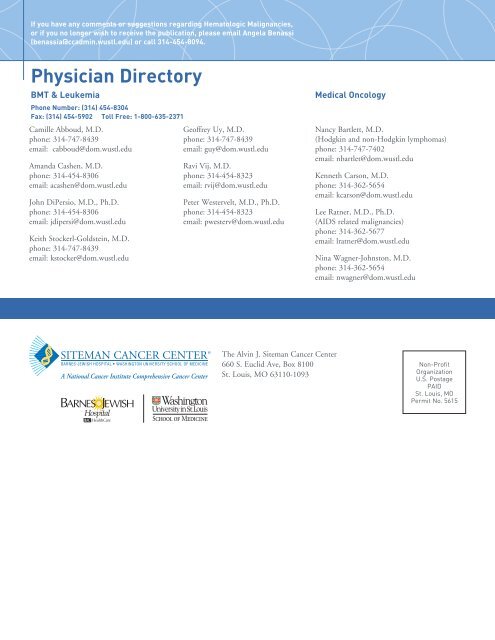
If you have any comments or suggestions regarding <strong>Hematologic</strong> <strong>Malignancies</strong>,or if you no longer wish to receive the publication, please email Angela Benassi(benassia@ccadmin.wustl.edu) or call 314-454-8094.Physician DirectoryBMT & LeukemiaPhone Number: (314) 454-8304Fax: (314) 454-5902 Toll Free: 1-800-635-2371Camille Abboud, M.D.phone: 314-747-8439email: cabboud@dom.wustl.eduAmanda Cashen, M.D.phone: 314-454-8306email: acashen@dom.wustl.eduJohn DiPersio, M.D., Ph.D.phone: 314-454-8306email: jdipersi@dom.wustl.eduKeith Stockerl-Goldstein, M.D.phone: 314-747-8439email: kstocker@dom.wustl.eduGeoffrey Uy, M.D.phone: 314-747-8439email: guy@dom.wustl.eduRavi Vij, M.D.phone: 314-454-8323email: rvij@dom.wustl.eduPeter Westervelt, M.D., Ph.D.phone: 314-454-8323email: pwesterv@dom.wustl.eduMedical OncologyNancy Bartlett, M.D.(Hodgkin and non-Hodgkin lymphomas)phone: 314-747-7402email: nbartlet@dom.wustl.eduKenneth Carson, M.D.phone: 314-362-5654email: kcarson@dom.wustl.eduLee Ratner, M.D., Ph.D.(AIDS related malignancies)phone: 314-362-5677email: lratner@dom.wustl.eduNina Wagner-Johnston, M.D.phone: 314-362-5654email: nwagner@dom.wustl.eduThe Alvin J. <strong>Siteman</strong> <strong>Cancer</strong> <strong>Center</strong>660 S. Euclid Ave, Box 8100St. Louis, MO 63110-1093Non-ProfitOrganizationU.S. PostagePAIDSt. Louis, MOPermit No. 5615
CONNECTING LIFE AND SCIENCE<strong>Hematologic</strong> <strong>Malignancies</strong>Leukemia, Lymphoma, Myelomaand Stem Cell TransplantationIssue Number 4 — Spring 2009Multiple Myeloma: Research Program and Clinical TrialsKeith Stockerl-Goldstein, M.D., Associate Professor of Medicine, Division of Oncology, Section of Bone Marrow Transplantation,Washington University School of MedicineThe treatment of multiple myeloma has changed dramatically inthe past decade with the introduction of new classes of medicationsapproved for this malignancy. Since 1999 when thalidomide wasfirst being reported as an active agent in multiple myeloma, thetreatment of newly diagnosed as well as recurrent myeloma hasmoved away from alkylator-based therapy to more defined treatmentsthat affect the myeloma microenvironment. Along with these newpharmacologic treatments there has been a significant increase inour knowledge of the biology of multiple myeloma. Our myelomaprogram is very active with 91 transplantslast year and approximately 200 myelomapatient referrals.Washington University/<strong>Siteman</strong> <strong>Cancer</strong><strong>Center</strong> MGUS-Multiple Myeloma ProgramOver the past 4 years, a multidisciplinarygroup of investigators has joined togetherto focus their research efforts on multiplemyeloma and other plasma cell dyscrasiasand now includes researchers from adiverse group of specialties throughout the Medical School and<strong>Cancer</strong> <strong>Center</strong>. Our current membership includes Ravi Vij andKeith Stockerl-Goldstein (BMT/Leukemia), Michael Tomasson(Stem Cell Biology), Kathy Weilbaecher (Molecular Oncology),Graham Colditz (Surgery), Feng Gao (Biostatistics), Anjum Hassan(Hematopathology) and Shashikant Kulkarni (Cytogenomics). Ourresearch efforts are focused on developing new treatments for patientswith multiple myeloma and on a better understanding of the geneticsof multiple myeloma.Bone marrow samples from untreated patients with plasma celldyscrasias are an important part of our efforts. Drs. Colditz andTo refer a patient, please call: 877-251-6485Call Monday-Friday 8:30 a.m. to 4:30 p.m.central time.Within 24 hours (excluding weekend and holidays)a new patient coordinator will contact your office tofacilitate the referral process.If a patient requires direct admission oremergent transfer, please call 800-252-3627.Available 24 hours a day, seven days a week.Tomasson are leading an effort to use genome wide associationstudies to isolate factors that predict for the development of multiplemyeloma. In addition, we are entering a major collaborationwith the Washington University Genome Sequencing <strong>Center</strong> tofurther understand the genetic changes in multiple myeloma. Dr.Weilbaecher, who specializes in the molecular pathogenesis of bonemetastases, is developing laboratory models of multiple myelomato allow testing of new agents using patient samples to help usadvance from our limitations of relying on myeloma cell lines fordrug testing. An integral component ofour growing research program is a multiplemyeloma tissue bank containing pairedmyeloma samples and normal tissue fromover 350 patients. We are in the advanceddevelopment phase of a comprehensivelongitudinal myeloma database that will linktissue samples, experimental data and clinicalinformation in a single electronic portal tofacilitate a more rapid translation of researchdata into clinical use. We are activelycollecting bone marrow specimens from patients with multiplemyeloma, primary systemic amyloidosis and MGUS to continueto expand this important tissue repository.The Multiple Myeloma Program physicians recently joined theMultiple Myeloma Research Consortium (MMRC). This is a groupof 15 academic centers that are part of a new model of researchdesigned to speed the development of new therapies for multiplemyeloma. The MMRC has facilitated 17 Phase I and Phase II clinicaltrials since its inception, and our membership in this importantcollaboration allows us to provide access to exciting new drugs for thetreatment of patients with multiple myeloma.(continued on page 2)
Radiological Terrorism: Preparedness and Response forTransplant/Hematology/Oncology <strong>Center</strong>sLinda Laub, RN, MSN, Nurse Manager, Outpatient BMT, Leukemia & Lymphoma and Marita Wehde, RN, BSN,CHTC, Assistant Nurse Manager, Outpatient BMT, Leukemia & Lymphoma“Events involving radioactive material, either accidental orintentional, are potentially devastating. Hematologists andoncologists are uniquely suited to help manage radiation victims,as myelosuppression and other multi-organ injury are frequentcomplications. Experience in managing severe myelosuppressionsuggests that hematology, oncology and transplantation physiciansshould participate in preparedness planning.” 1 After a devastatingevent, such as a nuclear detonation, there may be a nationalcall that involves hematologists/oncologists across the countryin the disaster response. In preparation, the National MarrowDonor Program (NMDP) and the American Society for Bloodand Marrow Transplantation have established the RadiationInjury Treatment Network (RITN), a voluntary organization oftransplant centers, donor centers and umbilical cord blood banks.The goals of RITN are the following:1. To develop standardized treatment guidelines for thehematologic toxicity of radiation exposure.2. To educate health care professionals regarding theirpotential participation in response to a radiation event.3. To educate health care systems and providers about theaspects of managing radiation exposure.4. To coordinate national readiness exercises.The RITN is a network of 52 stem cell transplant centers, donorcenters and umbilical cord blood banks all strategically locatedacross the United States. The <strong>Siteman</strong> <strong>Cancer</strong> <strong>Center</strong> at Barnes-Jewish Hospital and Washington University School of Medicinewas one of the first transplant centers to participate in this network.Barnes-Jewish Hospital (BJH) is a member of a local collaborationof hospitals called the St. Louis Area Regional Response System(STARRS). This group consists of 22 hospitals that work to share theload when needed, and effectively respond to mass casualty scenarios.Should there be a radioactive event, the RITN will assist BJH withthe coordination of the response so that comprehensive evaluation andtreatment of victims at this stem cell transplant center can be realized.As a part of preparedness, the transplant team at BJH has developed,maintained and improved standard operating procedures on howthe organization would respond to a nuclear detonation. Annually,the transplant program participates in RITN directed exercises anddrills. Additionally, the program supports internal and external basedtraining programs to expand the medical knowledge of the healthcare professionals in hematology/oncology within thecommunity. BJH presents itself as one of the most preparedcenters of the RITN. This was recently confirmed whenit was honored as one of the top five “highly prepared”hospitals by the National Foundation of Trauma Care.Preparedness, planning and education may notalways be adequate when managing a highvolume of medical emergencies, particularlywhen the situation is as frightening as a nucleardetonation. The challenge for the hematology,oncology and transplant community is toplan ahead and develop the expertise in theevent that they may be called upon to carefor victims. The RITN and its contingencyefforts will assist the community inmanaging this challenge, although it ishoped that such devastation never occurs.Additional information and resources canbe found on the following websites:RITN: www.nmdp.org/RITNHHA Radiation Event MedicalManagement (REMM):www.remm.nlm.govCDC:- Radiological Terrorism: Medical Responseto Mass Casualties:www.bt.cdc.gov/radiation/masscasualities/training.asp- Radiological Terrorism: Just in TimeTraining for Hospital Clinicians:www/bt.cdc.gov/radiation/justintime.asp- Medical Response to Nuclear and Radiological Terrorism:www2.cdc.gov/phtn/webcast/radiation-04/default.asp- The Role of Public Health in a Nuclearor Radiological Terrorist Incident:www2.cdc.gov/phtn/nuclear05/default.aspReferences:1. Blood. 2008; 5440-5445, Radiological and nuclear events; contingencyplanning for hematologists/oncologists.3
<strong>Hematologic</strong> <strong>Malignancies</strong>Leukemia, Lymphoma, Myelomaand Stem Cell TransplantationClinical TrialsTo learn more about the clinical studies, or to enroll a patient,please contact the listed study coordinator at 314-454-8377.AML, newly diagnosedAcute Leukemia /MDSCALGB 10503 PI: Geoffrey Uy Study Coordinator:Ryan MonahanPhase II Study of Maintenance Therapy With DecitabineFollowing Standard Induction and Cytogenetic Risk-AdaptedIntensification in Previously Untreated Patients With AML< 60 Years.Notes: Newly dx de novo AML age 18-59, decitabine maintenanceafter induction and risk adapted consolidation based on cytogeneticsto either HiDAC or auto transplant08-0126 PI: Geoffrey Uy Study Coordinator:Ryan MonahanSWOG S0521— A Randomized Trial of Maintenance VersusObservation for Patients with Previously Untreated Low andIntermediate Risk Acute Promyelocytic Leukemia (APL),Phase III.Notes: Low or intermediate risk APL 18 years and older withno prior systemic therapy or recurrent disease.08-0172 PI: Geoffrey Uy Study Coordinator:Alissa NelsonA Phase I/II Study of LBH589 plus Decitabine for PatientsAge > 60 Years with High Risk MDS or AMLNotes: Age > 60 with MDS (IPSS>2) or AML with no prior treatmentwith a hypomethylating agent08-0847 PI: Geoffrey Uy Study Coordinator:Ryan MonahanSWOG S0535— A Phase II Study of ATRA, Arsenic Trioxide andGemtuzumab Ozogamicin in patients with previously UntreatedHigh-Risk Acute Promyelocytic LeukemiaNotes: High risk APL 18 years and older with no prior systemictherapy or recurrent disease.AML, relapsed refractory07-0227 PI: Geoffrey Uy Study Coordinator:Sandra LopezA Phase I/II Study of AMD3100 With Mitoxantrone, Etoposide andCytarabine (AMD3100+MEC) in Relapsed or Refractory AML.Notes: Age 18-65 with either primary refractory AML, relapsed AMLwith initial CR less than 1 yr or in 2nd relapse or higherMDS/AML, otherP2C 05-1159PI: Amanda CashenPhase II Study of the Histone Deacetylase Inhibitor PXD101for the Treatment of Myelodysplastic SyndromeNotes: 18 years old and up with a diagnosis of MDS, no morethan 2 previous lines of therapy and either ineligible or refusedallo transplant.CALGB 100103 PI: Ravi Vij Study Coordinator:Ryan MonahanA Phase II Study Of Allogeneic Transplant For Older PatientsWith AML In First Morphologic Complete Remission UsingA Non-Myeloablative Preparative Regimen.Notes: CR1, Fludarabine, Busulfan, Thymoglobulin conditioning07-0643 PI: John DiPersio Study Coordinator:Jeremy GabrielA Phase II Study of Active Immunotherapy With GRNVAC1,Autologous Mature Dendritic Cells Transfected With mRNAEncoding Human Telomerase Reverse Transcriptase, inPatients With Acute Myelogenous Leukemia in CompleteClinical Remission.Notes: Age 18-65 with AML in 1st or 2nd CR using dendriticcell vaccine directed against telomerase (hTERT)Study Coordinator:07-0916 PI: Ravi VijLiz ProcknowA Phase II study of intravenous Decitabine in combinationwith Arsenic Trioxide and Ascorbic Acid in patients withmyelodysplastic syndromesNotes: MDS defined by FAB classification.08-0172 PI: Geoffrey Uy Study Coordinator:Alissa NelsonA Phase I/II Study of LBH589 plus Decitabine for PatientsAge > 60 Years with High Risk MDS or AMLNotes: Age > 60 with MDS (IPSS>2) or AML with no prior treatmentwith a hypomethylating agent08-1161 PI: Ravi Vij Study Coordinator:Sarah WitowskiA Phase I, Open-Label, Dose-Ranging Study to Evaluate thePharmacokinetics and Safety of Azacitidine AdministeredSubcutaneously (SC) and as Different Oral Formulationsin Subjects with Myelodysplastic Syndromes (MDS), AML,Lymphoma, and Multiple Myeloma08-0853 PI: Ravi Vij Study Coordinator:Sarah WitowskiPhase I Study of Oral Clofarabine Consolidation in Adults Aged60 and Older with Acute Myeloid LeukemiaNotes AML in CR1, > 60 years old.ALLCALGB 10403 PI: Geoffrey Uy Study Coordinator:Ryan MonahanAn Intergroup Phase II Clinical Trial for Adolescents and Youngadults with Untreated Acute Lymphoblastic Leukemia.Notes: Newly diagnosed and untreated ALL between the age of16 and 29.4
<strong>Hematologic</strong>al <strong>Malignancies</strong> is published by The Alvin J. <strong>Siteman</strong> <strong>Cancer</strong> <strong>Center</strong> at Barnes-Jewish Hospital and Washington UniversitySchool of Medicine. The <strong>Siteman</strong> <strong>Cancer</strong> <strong>Center</strong> is designated as a Comprehensive <strong>Cancer</strong> <strong>Center</strong> by the National <strong>Cancer</strong> Institute (NCI) andis a member of the National Comprehensive <strong>Cancer</strong> <strong>Center</strong> Network (NCCN).Editors: Geoffrey Uy, M.D. and Ryan Monahan | Article Contributors: Keith Stockerl-Goldstein, M.D., Linda Laub, RN, MSN andMarita Wehde, RN, BSN, CHTC | Production Manager: Angela BenassiFollicularNON-HODGKIN LYMPHOMA (NHL)CALGB 50401 PI: Nancy L.BartlettStudy Coordinator:Rachael KeeleyA Randomized Phase II trial of Rituximab vs. Lenalidomide(Revlimid TM , CC-5013) (IND # 73034) vs. Rituximab + Lenalidomidein Recurrent Follicular Non-Hodgkin Lymphoma (NHL) ThatIs Not Rituximab-Refractory (Arm A, Rituximab Alone, waspermanently closed effective 9/15/2007)Notes: Patients must have been treated with rituximab either aloneor in combination with chemotherapy. The last prior treatmentregimen need not include rituximab but must have progressed>6 months from their last rituximab dose.CALGB 50701 PI: Nancy L.BartlettStudy Coordinator:Justina FirstA Phase II Trial of Extended Induction Epratuzumab (Anti-CD22Monoclonal Antibody) Plus Rituximab in Previously UntreatedFollicular Non-Hodgkin’s Lymphoma08-0332 PI: Amanda Cashen Study Coordinator:Rachael KeeleyA Phase II Study of Bortezomib in Combination withBendamustine and Rituximab in Subjects with Relapsed orRefractory Follicular LymphomaNotes: Prior treatment with Bortezomib or Bendamustine is notallowed; at least 4 prior doses of Rituximab; prior allogeneic stemcell transplant not allowed.Large CellCALGB 50303 PI: Nancy L.BartlettStudy Coordinator:Sarah LarsonPhase III Randomized Study of R-CHOP vs. Dose-AdjustedEPOCH-R with Molecular Profiling in Untreated De Novo DiffuseLarge B-Cell LymphomasNotes: Patients must have a new biopsy if fresh/frozen tissue wasnot available from their first biopsy, unless contraindicated.07-1073 PI: Nancy L.BartlettStudy Coordinator:Justina FirstA Randomized Phase IIb Placebo-Controlled Study of R-ICEChemotherapy (Rituximab, Ifosfamide, Carboplatin, andEtoposide) with and without SGN-40 (Anti-CD40 humanizedmonoclonal antibody) for Second-line Treatment of Patients withDiffuse Large B-Cell LymphomaNotes: Patients must have achieved a complete response, partialresponse, or stable disease from their most recent prior therapyconsisting of combination chemotherapy and rituximab.Mantle Cell08-0851 PI: Nancy L.BartlettStudy Coordinator:Rachael KeeleyAn open-label, Single Arm Phase II Study of RAD001 in Patientswith Refractory Mantle Cell LymphomaNotes: Patients must have been refractory to Bortezomib and to theirlast line of therapy (if other than Bortezomib).CALGB 50403 PI: Nancy L.BartlettStudy Coordinator:Rachael KeeleyA Randomized Phase II Trial of Maintenance vs. ConsolidationBortezomib Therapy Following Aggressive Chemo-Immunotherapy and Autologous Stem Cell Transplant forPreviously Untreated Mantle Cell LymphomaNotes: Patients must be between the ages of 18 and 69 years withany stage (I-IV).CALGB 50501 PI: Nancy L.BartlettStudy Coordinator:Rachael KeeleyA Phase II Trial of Bortezomib (NSC #681239) + Lenalidomide(Revlimid TM , CC-5013) (NSC#703813) For Relapsed/RefractoryMantle Cell LymphomaNotes: Patients may not have received prior bortezomib orlenalidomide therapy.AIDS/HTLVAMC 047 PI: Lee Ratner Study Coordinator:Lee RatnerA Phase II Trial of Doxil, Rituximab, Cyclophosphamide,Vincristine, and Prednisone (DR-COP) in Patients with NewlyDiagnosed AIDS-Associated B-Cell Non-Hodgkin’s LymphomaAMC 048 PI: Lee Ratner Study Coordinator:Lee RatnerProspective Phase II Study of a High Dose, Short CourseRegimen (R-CODOX-M/IVAC) Including Central Nervous System(CNS) Penetration and Intensive Intrathecal (IT) Prophylaxis inHIV-Associated Burkitt’s and Atypical Burkitt’s Lymphoma.Primary CNSRTOG 0227PI: DavidMansurStudy Coordinator:Shannon RickeyPhase I/II Study of Pre-Irradiation Chemotherapy withMethotrexate, Rituximab, and Temozolomide and Post-Irradiation Temozolomide for Primary Central NervousSystem Lymphoma08-0500 PI: Nancy L.BartlettStudy Coordinator:Sarah LarsonA Phase Ib Study of SGN-40 in Combination with Rituximab andGemcitabine for the Treatment of Patients with Relapsed orRefractory Diffuse Large B-Cell Lymphoma(continued on page 6)5
<strong>Hematologic</strong> <strong>Malignancies</strong>Clinical Trials (continued)Leukemia, Lymphoma, Myelomaand Stem Cell TransplantationAll Lymphoma Histologies08-0494 PI: Nancy L.BartlettStudy Coordinator:Justina FirstA Phase I/II Dose Escalation Study of the Pan-HistoneDeacetylase (HDAC) Inhibitor PCI-24781 in LymphomaNotes: Patients must have had no more than 4 prior therapies; priorallogeneic transplant not allowed.08-0543 PI: Nancy L.BartlettStudy Coordinator:Justina FirstA Phase I/IIa Open-Label Study of Pralatrexate and Gemcitabinewith Vitamin B12 and Folic Acid Supplementation in Patients withRelapsed or Refractory Lymphoproliferative <strong>Malignancies</strong>Notes: Patients must have at least 1 prior treatment; no priorallogeneic transplant; patients must have relapsed > 100 days fromautologous transplant.08-1270 PI: Nina Wagner-JohnstonStudy Coordinator:Justina FirstPhase I Sequential Dose Escalation Study to Investigate theSafety, Pharmacokinetics, Pharmacodynamics, and ClinicalActivity of CAL-101 in Patients with Select, Relapsed orRefractory <strong>Hematologic</strong> <strong>Malignancies</strong>.T-Cell08-0170 PI: Nancy L.BartlettStudy Coordinator:Sarah LarsonA Phase I Dose Escalation Study of Weekly SGN-35 Alone andIn Combination with Gemcitabine in Patients with Relapsed/Refractory CD30-Positive <strong>Hematologic</strong> <strong>Malignancies</strong>Notes: Patients with relapsed/refractory ALCL are eligible forthis trial.09-0017 PI: Nancy L.BartlettStudy Coordinator:Sarah LarsonPivotal Study of SGN-35 in Treatment of Patients with Relapsedor Refractory Systemic Anaplastic Large Cell Lymphoma (ALCL)07-1079 PI: Nancy L.BartlettStudy Coordinator:Justina FirstA Phase 1, Open-Label Study of Pralatrexate with Vitamin B 12and Folic Acid Supplementation in Patients with Relapsed orRefractory Cutaneous T-Cell LymphomaNotes: Patients must have had at least 1 prior therapy. Patientswith mycosis fungoides and Sezary syndrome are eligible.08-0443 PI: Nancy L.BartlettStudy Coordinator:Justina FirstTreatment of Peripheral T-Cell Lymphoma with AggressiveInduction Chemotherapy Followed by Autologous Stem CellTransplant using Denileukin Diftitox (Ontak) for in-vivo Purgingand Post-Transplant Therapy: A Multicenter Phase II Clinical TrialNotes: For patients with previously untreated T-Cell Lymphoma orcould have received up to 1 prior cycle of chemotherapy07-0878 PI: Nancy L.BartlettStudy Coordinator:Rachael KeeleySingle Agent Phase II Study of Forodesine (BCX1777) in theTreatment of Cutaneous T-Cell LymphomaNotes: Patients must have progressed/recurred following 3 formsof systemic therapy, one of which must have been oral bexaratone(unless it was not tolerated or medically contraindicated). Patientsmust have stage IB-IVA CTCL; mycosis fungoides or Sezarysyndrome are eligible.HODGKIN LYMPHOMA (HL)08-0170 PI: Nancy L.BartlettStudy Coordinator:Sarah LarsonA Phase I Dose Escalation Study of Weekly SGN-35 Alone andin Combination with Gemcitabine in Patients with Relapsed/Refractory CD30-Positive <strong>Hematologic</strong> <strong>Malignancies</strong>Notes: Patients with recurrent Hodgkin’s lymphoma must havefailed systemic therapy either as induction for advanced stagedisease or salvage therapy after initial radiotherapy for early stageand were ineligible for, refused treatment by or previously receivedstem cell transplant.09-0014 PI: Nancy L.BartlettStudy Coordinator:Sarah LarsonPivotal Study of SGN-35 in Treatment of Patients with Relapsedor Refractory Hodgkin Lymphoma (HL)07-0233 PI: Nancy L.BartlettStudy Coordinator:Sarah LarsonA Phase II Multicenter Study of Lenalidomide in Relapsed orRefractory Classical Hodgkin LymphomaNotes: Patients must have recurred after at least 1 prior therapy.Patients with any stage and who have had prior autologous orallogeneic stem cell transplant are eligible.CALGB 50602 PI: Nancy L.BartlettStudy Coordinator:Sarah LarsonA Phase II Study of Galiximab in Patients with Relapsed/Refractory Hodgkin’s LymphomaNotes: Patients must have had at least 2 prior treatments; priorautologous and/or allogeneic stem cell transplant is allowed.08-0719 PI: Nancy L.BartlettStudy Coordinator:Sarah LarsonA Randomized Phase II study of Rituximab with ABVD vs. StandardABVD for Patients with Advanced-Stage Classical HodgkinLymphoma with Poor Risk FeaturesNotes: IPS Score >26
Chronic Lymphocytic Leukemia (CLL)CALGB 10404 PI: Nancy L.BartlettStudy Coordinator:Kris McDonaldA Randomized Phase II Study of Three Fludarabine/antibodyCombinations for Patients with Symptomatic, PreviouslyUntreated Chronic Lymphocytic LeukemiaNotes: For previously untreated CLL patients requiring therapy(symptomatic, intermediate or high-risk by Rai staging system).CALGB 10501 PI: Nancy L.BartlettStudy Coordinator:Kris McDonaldA Phase III Intergroup CLL Study of Asymptomatic Patients withUntreated Chronic Lymphocytic Leukemia Randomized to EarlyIntervention Versus Observation with Later Treatment in theHigh Risk Genetic Subset with IGV H Unmutated DiseaseNotes: For patients who are within 6 months of their initialdiagnosis, asymptomatic and low risk by Rai staging system.Multiple MyelomaCALGB 100104 PI: Ravi Vij Study Coordinator:Ryan MonahanA Phase III Randomized, Double-Blind Study of MaintenanceTherapy with CC-5013 or Placebo Following AutologousStem Cell Transplantation for Multiple MyelomaNotes: At least stage 1 MM, 2 months stable following therapy,no more than 12 months total prior therapy for MM.07-1136 PI: Ravi Vij Study Coordinator:Deborah GensburgPhase I/II Trial of combination CCI-779 (Temsirolimus) andBortezomib (VELCADE) in Relapsed and/or Relapsed/RefractoryMultiple Myeloma (MMRC CCI-779).Notes: Relapsed or relapsed/refractory Multiple Myeloma patients18 years old or greater with measurable disease.07-0775 PI: Ravi Vij Study Coordinator:Mark FialaAn Open-label, Single-arm, Phase 2 Study of Carfilzomib inPatients with Relapsed and Refractory Multiple MyelomaNotes: Ages 18 and older with a previous response with relapseand refractory to last line of therapy, must have been treated withbortezomib and either thalidomide or lenalidomide.07-0776 PI: Ravi Vij Study Coordinator:Mark FialaAn Open-label, Single-arm, Phase 2 Study of Carfilzomib inPatients with Relapsed Multiple MyelomaNotes: Ages 18 and older with a response to their prior line oftherapy.08-0705 PI: Ravi Vij Study Coordinator:Deborah GensburgA Phase 1b, Multicenter, Open-label, Dose-escalation Study ofHuLuc63 (Humanized Anti-CS1 Monoclonal IgG1 Antibody) inCombination with Lenalidomide and Dexamethasone in subjectswith Relapsed Multiple Myeloma08-1161 PI: Ravi Vij Study Coordinator:Sarah WitowskiA Phase I, Open-Label, Dose-Ranging Study to Evaluate thePharmacokinetics and Safety of Azacitidine AdministeredSubcutaneously (SC) and as Different Oral Formulationsin Subjects with Myelodysplastic Syndromes (MDS), AML,Lymphoma, and Multiple MyelomaGeneralTransplant08-0897 PI: Amanda Cashen Study Coordinator:Stefanie GoranA Phase I/II Study of Intravenous AMD3100 Added to a MobilizationRegimen of G-CSF to Increase the Number of Peripheral BloodStem Cells Collected From Patients with Lymphoma.Notes: Any patient aged 18-75 with hodgkins or non-hodgkinslymphoma and eligible for autologous transplant.CTN 0201 PI: John DiPersio Study Coordinator:Jeremy GabrielA Phase III Randomized, Multicenter Trial ComparingG-CSF Mobilized Peripheral Blood Stem Cell with MarrowTransplantation from HLA Compatible Unrelated DonorsNotes: AML, ALL, CML, MDS08-0011 PI: John DiPersio Study Coordinator:Liz ProcknowA Multicenter, Prospective Trial to Evaluate the Role of NKCell Kir Epitope Mismatch on Mortality and Disease Relapse inT-Cell Depleted Hematopoietic Stem Cell Transplantation fromHLA-C Mismatched, Unrelated Donors for Myeloid <strong>Malignancies</strong>(MT2004-04).CTN 0603PI: Peter Westervelt Study Coordinator:Jeremy GabrielA Multicenter, Phase II Trial of Nonmyeloblative Conditioning(NST)and Transplantation of Partially HLA-Mismatched BoneMarrow for Patients with <strong>Hematologic</strong> <strong>Malignancies</strong> (BMT CTN0603).Notes: Open to AML in 2nd or subsequent CR or AML in highrisk CR1, ALL in high risk CR1, Burkitt’s Lymphoma in 2nd orsubsequent CR, Lymphoma (large cell, Mantle cell and Hodgkin’s inCR or PR and marginal and B-cell lymphoma progressed after 2 ormore therapies).7
CTN 0604PI: Peter Westervelt Study Coordinator:Jeremy GabrielA Multicenter, Phase II Trial of Nonmyeloblative Conditioning(NST)and Transplantation of Partially HLA-Mismatched BoneMarrow for Patients with <strong>Hematologic</strong> <strong>Malignancies</strong> (BMT CTN0603).Notes: Open to AML in 2nd or subsequent CR or AML in highrisk CR1, ALL in high risk CR1, Burkitt’s Lymphoma in 2nd orsubsequent CR, Lymphoma (large cell, Mantle cell and Hodgkin’s inCR or PR and marginal and B-cell lymphoma progressed after 2 ormore therapies).GVHD08-1093 PI: John DiPersio Study Coordinator:Stefanie GoranA Phase 2, Open-Label, Single Arm, Pilot Study of Safety andEfficacy of CC-4047 (Pomalidomide) in Patients with AdvancedChronic Graft-Versus-Host Disease.08-0072 PI: PeterWesterveltStudy Coordinator:Jeremy GabrielA Phase III, Randomized, Double-Blind, Placebo-ControlledStudy to Evaluate the Efficacy and Safety of Prochymal (Ex-vivo Cultured Adult Human Mesenchymal Stem Cells)Infusion in Combination with Corticosteroids for the Treatmentof newly diagnosed Acute GVHD.Continuing Medical Education:Advances in Diagnosis and Treatmentof <strong>Hematologic</strong> <strong>Malignancies</strong>August 22, 2009Four Seasons HotelSt. Louis, Missouri<strong>Siteman</strong> <strong>Cancer</strong> <strong>Center</strong> at Barnes-Jewish Hospitaland Washington University School of Medicine ishosting an educational symposium entitled “Advances inDiagnosis and Treatment of <strong>Hematologic</strong> <strong>Malignancies</strong>”.The symposium will take place on Saturday, August 22at the Four Seasons Hotel in St. Louis, Missouri.The annual symposium provides the audience withupdated information from Washington UniversityPhysicians on cancer treatment and diagnosis throughdiscussions on hematological malignancies.In addition to the conference, we are hosting our16th Annual Bone Marrow Transplant PatientCelebration on Saturday, August 22, in the ballroomof the Four Seasons Hotel - St. Louis. The celebrationis held to honor our survivors. All who attend theeducation symposium, and a guest, are welcometo join us for the celebration. A private physicianreception an hour prior to the patient celebrationwill also take place in the Four Seasons Hotel.If you are interested in attending the symposium,please register at http://cme.wustl.edu. PleaseRSVP for the patient celebration and privatephysician reception by calling 314-747-7222or 800-600-3606 by August 10.