The forced oscillation technique in clinical practice ... - Assobrafir
The forced oscillation technique in clinical practice ... - Assobrafir
The forced oscillation technique in clinical practice ... - Assobrafir
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
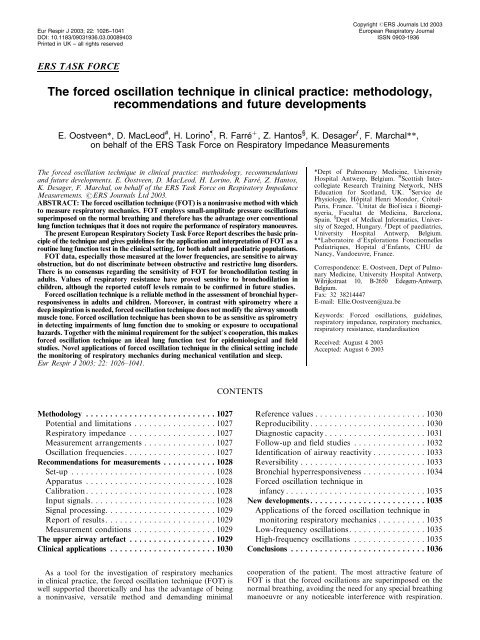
Eur Respir J 2003; 22: 1026–1041DOI: 10.1183/09031936.03.00089403Pr<strong>in</strong>ted <strong>in</strong> UK – all rights reservedCopyright #ERS Journals Ltd 2003European Respiratory JournalISSN 0903-1936ERS TASK FORCE<strong>The</strong> <strong>forced</strong> <strong>oscillation</strong> <strong>technique</strong> <strong>in</strong> cl<strong>in</strong>ical <strong>practice</strong>: methodology,recommendations and future developmentsE. Oostveen*, D. MacLeod # , H. Lor<strong>in</strong>o } , R. Farré z , Z. Hantos § , K. Desager ƒ , F. Marchal**,on behalf of the ERS Task Force on Respiratory Impedance Measurements<strong>The</strong> <strong>forced</strong> <strong>oscillation</strong> <strong>technique</strong> <strong>in</strong> cl<strong>in</strong>ical <strong>practice</strong>: methodology, recommendationsand future developments. E. Oostveen, D. MacLeod, H. Lor<strong>in</strong>o, R. Farré, Z. Hantos,K. Desager, F. Marchal, on behalf of the ERS Task Force on Respiratory ImpedanceMeasurements. #ERS Journals Ltd 2003.ABSTRACT: <strong>The</strong> <strong>forced</strong> <strong>oscillation</strong> <strong>technique</strong> (FOT) is a non<strong>in</strong>vasive method with whichto measure respiratory mechanics. FOT employs small-amplitude pressure <strong>oscillation</strong>ssuperimposed on the normal breath<strong>in</strong>g and therefore has the advantage over conventionallung function <strong>technique</strong>s that it does not require the performance of respiratory manoeuvres.<strong>The</strong> present European Respiratory Society Task Force Report describes the basic pr<strong>in</strong>cipleof the <strong>technique</strong> and gives guidel<strong>in</strong>es for the application and <strong>in</strong>terpretation of FOT as arout<strong>in</strong>e lung function test <strong>in</strong> the cl<strong>in</strong>ical sett<strong>in</strong>g, for both adult and paediatric populations.FOT data, especially those measured at the lower frequencies, are sensitive to airwayobstruction, but do not discrim<strong>in</strong>ate between obstructive and restrictive lung disorders.<strong>The</strong>re is no consensus regard<strong>in</strong>g the sensitivity of FOT for bronchodilation test<strong>in</strong>g <strong>in</strong>adults. Values of respiratory resistance have proved sensitive to bronchodilation <strong>in</strong>children, although the reported cutoff levels rema<strong>in</strong> to be confirmed <strong>in</strong> future studies.Forced <strong>oscillation</strong> <strong>technique</strong> is a reliable method <strong>in</strong> the assessment of bronchial hyperresponsiveness<strong>in</strong> adults and children. Moreover, <strong>in</strong> contrast with spirometry where adeep <strong>in</strong>spiration is needed, <strong>forced</strong> <strong>oscillation</strong> <strong>technique</strong> does not modify the airway smoothmuscle tone. Forced <strong>oscillation</strong> <strong>technique</strong> has been shown to be as sensitive as spirometry<strong>in</strong> detect<strong>in</strong>g impairments of lung function due to smok<strong>in</strong>g or exposure to occupationalhazards. Together with the m<strong>in</strong>imal requirement for the subject9s cooperation, this makes<strong>forced</strong> <strong>oscillation</strong> <strong>technique</strong> an ideal lung function test for epidemiological and fieldstudies. Novel applications of <strong>forced</strong> <strong>oscillation</strong> <strong>technique</strong> <strong>in</strong> the cl<strong>in</strong>ical sett<strong>in</strong>g <strong>in</strong>cludethe monitor<strong>in</strong>g of respiratory mechanics dur<strong>in</strong>g mechanical ventilation and sleep.Eur Respir J 2003; 22: 1026–1041.*Dept of Pulmonary Medic<strong>in</strong>e, UniversityHospital Antwerp, Belgium. # Scottish IntercollegiateResearch Tra<strong>in</strong><strong>in</strong>g Network, NHSEducation for Scotland, UK.} Service dePhysiologie, Hôpital Henri Mondor, Créteil-Paris, France. z Unitat de Biofísica i Bioeng<strong>in</strong>yeria,Facultat de Medic<strong>in</strong>a, Barcelona,Spa<strong>in</strong>. § Dept of Medical Informatics, Universityof Szeged, Hungary. ƒ Dept of paediatrics,University Hospital Antwerp, Belgium.**Laboratoire d9Explorations FonctionnellesPediatriques, Hopital d9Enfants, CHU deNancy, Vandoeuvre, France.Correspondence: E. Oostveen, Dept of PulmonaryMedic<strong>in</strong>e, University Hospital Antwerp,Wilrijkstraat 10, B-2650 Edegem-Antwerp,Belgium.Fax: 32 38214447E-mail: Ellie.Oostveen@uza.beKeywords: Forced <strong>oscillation</strong>s, guidel<strong>in</strong>es,respiratory impedance, respiratory mechanics,respiratory resistance, standardisationReceived: August 4 2003Accepted: August 6 2003CONTENTSMethodology . . .........................1027Potential and limitations .................1027Respiratory impedance . .................1027Measurement arrangements . . .............1027Oscillation frequencies . . .................1027Recommendations for measurements . . .........1028Set-up . .............................1028Apparatus . . .........................1028Calibration . . .........................1028Input signals. .........................1028Signal process<strong>in</strong>g. . .....................1029Report of results. . .....................1029Measurement conditions .................1029<strong>The</strong> upper airway artefact . .................1029Cl<strong>in</strong>ical applications . .....................1030Reference values .......................1030Reproducibility . .......................1030Diagnostic capacity . . ...................1031Follow-up and field studies ...............1032Identification of airway reactivity ...........1033Reversibility . . . .......................1033Bronchial hyperresponsiveness . . ...........1034Forced <strong>oscillation</strong> <strong>technique</strong> <strong>in</strong><strong>in</strong>fancy . . ...........................1035New developments . .......................1035Applications of the <strong>forced</strong> <strong>oscillation</strong> <strong>technique</strong> <strong>in</strong>monitor<strong>in</strong>g respiratory mechanics . . . .......1035Low-frequency <strong>oscillation</strong>s. ...............1035High-frequency <strong>oscillation</strong>s ...............1035Conclusions . ...........................1036As a tool for the <strong>in</strong>vestigation of respiratory mechanics<strong>in</strong> cl<strong>in</strong>ical <strong>practice</strong>, the <strong>forced</strong> <strong>oscillation</strong> <strong>technique</strong> (FOT) iswell supported theoretically and has the advantage of be<strong>in</strong>ga non<strong>in</strong>vasive, versatile method and demand<strong>in</strong>g m<strong>in</strong>imalcooperation of the patient. <strong>The</strong> most attractive feature ofFOT is that the <strong>forced</strong> <strong>oscillation</strong>s are superimposed on thenormal breath<strong>in</strong>g, avoid<strong>in</strong>g the need for any special breath<strong>in</strong>gmanoeuvre or any noticeable <strong>in</strong>terference with respiration.
CLINICAL APPLICATION OF FOT1027Dur<strong>in</strong>g the past decade, advances <strong>in</strong> basic research and FOTapplications, as well as new developments <strong>in</strong> technology, haveevoked new <strong>in</strong>terest from both the cl<strong>in</strong>ical and <strong>in</strong>dustrialfields. To address demands for further standardisation ofFOT, a European Respiratory Society Task Force wasestablished to update the standardisation work carried outdur<strong>in</strong>g the Commission of the European CommunitiesBiomedical Eng<strong>in</strong>eer<strong>in</strong>g Advisory Committee (COMAC-BME) programme of respiratory impedance (Zrs) measurementdevelopment [1], and to develop cl<strong>in</strong>ical guidel<strong>in</strong>es forZrs measurement. <strong>The</strong> present report summarises the mostimportant underly<strong>in</strong>g concepts of the FOT, offers guidel<strong>in</strong>esfor its implementation and use <strong>in</strong> the cl<strong>in</strong>ical environment,and gives a brief overview on the latest developments ofpotential cl<strong>in</strong>ical impact.MethodologyS<strong>in</strong>ce the first FOT measurements by DUBOIS et al. [2],numerous variants of the FOT have been developed <strong>in</strong> termsof measurement configuration, <strong>oscillation</strong> frequencies andevaluation pr<strong>in</strong>ciples. This short review is focussed on therout<strong>in</strong>e cl<strong>in</strong>ical applications, address<strong>in</strong>g the most basicconcepts only, and the reader is referred for more detailed<strong>in</strong>formation to monograph articles [3–7].Potential and limitations<strong>The</strong> essence of the FOT can be elucidated by contrast<strong>in</strong>g itspr<strong>in</strong>ciple with that of the respiratory mechanical measurementsthat depend on spontaneous breath<strong>in</strong>g activity orrespiratory manoeuvres. Uniquely, for the FOT, externaldriv<strong>in</strong>g signals (i.e. <strong>forced</strong> <strong>oscillation</strong>s) are used to determ<strong>in</strong>ethe mechanical response of the respiratory system and the<strong>in</strong>vestigator uses specifically developed forc<strong>in</strong>g waveforms toexplore the respiratory mechanical properties, rely<strong>in</strong>g on thewell-developed arsenal of l<strong>in</strong>ear system analysis. FOT thuspossesses solid theoretical foundations and a high degree ofversatility, which are far beyond the capability of conventionalrespiratory mechanical tests. However, the requirementof l<strong>in</strong>earity necessitates the use of small-amplitude <strong>oscillation</strong>s,which may leave undisclosed some energetically andfunctionally important nonl<strong>in</strong>ear properties that manifestdur<strong>in</strong>g tidal breath<strong>in</strong>g, and assumes methodological rigor <strong>in</strong>both data collection and analysis.Respiratory impedance<strong>The</strong> key concept of the <strong>forced</strong> oscillatory respiratorymechanics is the "impedance" (Z), the spectral (frequencydoma<strong>in</strong>) relationship between pressure (P) and airflow (V9)(see Appendix). In simple terms, Z can be conceived as ageneralisation of resistance, s<strong>in</strong>ce it embodies both the <strong>in</strong>phaseand out-of-phase relationships between P and V9. <strong>The</strong><strong>in</strong>-phase component is called the real part of Z (or resistance(R)), whereas the out-of-phase relationship is expressed bythe imag<strong>in</strong>ary part (or reactance (X)), and both appear asfunctions of the frequency of <strong>oscillation</strong> (f). In other words, Rdescribes the dissipative mechanical properties of the respiratorysystem, whereas X is related to the energy storagecapacity and thus determ<strong>in</strong>ed jo<strong>in</strong>tly by the elastic properties(the relationship between P and volume) dom<strong>in</strong>ant at low<strong>oscillation</strong> frequencies and the <strong>in</strong>ertive properties (therelationship between P and volume acceleration), whichbecome progressively more important with <strong>in</strong>creas<strong>in</strong>g f.Measurement arrangementsDepend<strong>in</strong>g on the sites of the P and V9 measurements andof the application of the <strong>forced</strong> <strong>oscillation</strong>s, different k<strong>in</strong>ds ofimpedance of the respiratory system can be def<strong>in</strong>ed. Mostcommonly, the <strong>forced</strong> <strong>oscillation</strong>s are applied at the airwayopen<strong>in</strong>g, and the central airflow (V9ao) is measured with apneumotachograph attached to the mouthpiece, face mask orendotracheal tube (ETT). Pressure is also sensed at the airwayopen<strong>in</strong>g (Pao) with reference to body surface (<strong>in</strong> this case,atmospheric) pressure (Pbs). <strong>The</strong> <strong>in</strong>put impedance of therespiratory system (Zrs,<strong>in</strong>) is then the spectral (frequencydoma<strong>in</strong>) relationship between transrespiratory pressure(Prs=Pao-Patm) and V9ao: Zrs,<strong>in</strong>(f)=Prs(f)/V9ao(f). When Zrsis partitioned <strong>in</strong>to pulmonary (ZL) and chest wall impedance(Zw) on the basis of the measurement of <strong>in</strong>traoesophagealpressure (Pes), ZL and Zw are obta<strong>in</strong>ed from ZL=(Pao-Pes)/V9ao and Zw=(Pes-Pbs)/V9ao, respectively. A special version ofthe <strong>in</strong>put FOT is the head generator <strong>technique</strong>, where Pao isapplied around the head, <strong>in</strong> order to m<strong>in</strong>imise upper airwaywall shunt<strong>in</strong>g [8]. An alternative <strong>in</strong>strument that can be usedto estimate Zrs,<strong>in</strong> and that does not require the record<strong>in</strong>g offlow (V9), is a wave tube connect<strong>in</strong>g the source of <strong>forced</strong><strong>oscillation</strong>s (usually a loudspeaker) and the subject; Zrs,<strong>in</strong> ismeasured as the load impedance on the wave tube, on thebasis of the geometric and physical properties of the tube andthe <strong>in</strong>side air, and the pressure recorded at the <strong>in</strong>let and outletof the tube [9]. Transfer impedance is obta<strong>in</strong>ed when the<strong>oscillation</strong>s are imposed and P and V9 are measured atdifferent sites of the respiratory system; accord<strong>in</strong>gly, variousmeasurements of transfer impedance can be <strong>in</strong>strumented.However, if the impedance of the total respiratory system(Zrs,tr) is considered, either the oscillatory excitation at theairway open<strong>in</strong>g is comb<strong>in</strong>ed with the plethysmographicmeasurement of output, "body surface" flow, or the <strong>oscillation</strong>sare imposed <strong>in</strong> a "head-out" plethysmograph on thebody surface, with the measurement of V9ao. AsZrs,<strong>in</strong> andthese two variants of Zrs,tr are affected differently by theparallel elements of the respiratory system, such as alveolargas compressibility and upper airway wall movements, theycan be selected or comb<strong>in</strong>ed to obta<strong>in</strong> more reliable estimatesof the airway and tissue impedance. <strong>The</strong> present review isrestricted to the most easily implementable FOT, namely Zrs,<strong>in</strong>.Oscillation frequenciesFor rout<strong>in</strong>e cl<strong>in</strong>ical applications of FOT it is usual to applya medium frequency range, i.e. the imposed <strong>oscillation</strong>s startfrom 2–4 Hz, roughly 1 decade above the spontaneous breath<strong>in</strong>grate, and extend up to a few times 10 Hz. In this frequencyrange, the healthy respiratory system exhibits a largely frequency<strong>in</strong>dependentrespiratory resistance (Rrs) whose major componentis airway resistance (Raw) (fig. 1). Respiratory reactance(Xrs) undergoes the transition from negative values (when theelastic reactance dom<strong>in</strong>ates) to positive values <strong>in</strong>creas<strong>in</strong>g withf (the dom<strong>in</strong>ance of <strong>in</strong>ertial reactance). At the characteristicresonant frequency (fres), where Xrs crosses zero, the elasticand <strong>in</strong>ertial forces are equal <strong>in</strong> magnitude and opposite. <strong>The</strong>low-frequency <strong>oscillation</strong>s <strong>in</strong>clude the frequencies of spontaneousbreath<strong>in</strong>g and, accord<strong>in</strong>gly, can be applied dur<strong>in</strong>gapnoeic conditions only, whereas the high-frequency rangeconta<strong>in</strong>s <strong>oscillation</strong>s up to several 100 Hz. Use of lowfrequencyand high-frequency <strong>forced</strong> <strong>oscillation</strong>s reveals differentmechanical properties of the respiratory system, andthese <strong>technique</strong>s are promis<strong>in</strong>g as lung function test methods;for this reason they are considered <strong>in</strong> the "New developments"section. <strong>The</strong> present section of this report focuses on the mostcommonly used medium-frequency range FOT.
CLINICAL APPLICATION OF FOT1029<strong>in</strong>put signals. A peak-to-peak size of the composite signal of0.1–0.3 kPa seems optimal [12].In studies explor<strong>in</strong>g the frequency dependence of Zrs, theuse of multifrequency (composite) signals, preferably <strong>in</strong>clud<strong>in</strong>gthe 4–30 Hz range, is recommended. Usually, the amplitudespectrum of the composite signal is coloured so as to enhancethe power at lower test frequencies. This improves the signalto-noiseratio at the lower frequencies that are more contam<strong>in</strong>atedby components of the spontaneous breath<strong>in</strong>g signal.Special procedures have been developed to optimise thecomposite forc<strong>in</strong>g waveform [13]. Alternatively, when the Zrsdata at a s<strong>in</strong>gle frequency are of <strong>in</strong>terest, a s<strong>in</strong>usoidal signal atthe lowest possible frequency should be used. <strong>The</strong> lowestfrequency at which Zrs can be measured reliably is governedby the relative power of the harmonics of the breath<strong>in</strong>g signaland applied <strong>forced</strong> <strong>oscillation</strong> at that frequency.Signal process<strong>in</strong>gAverag<strong>in</strong>g pseudorandom signal epochs by time [14] or theuse of the so-called "unbiased estimators" [15, 16] reduces theerrors <strong>in</strong>troduced at the low frequencies (<strong>in</strong> adults belowy6 Hz) by the higher harmonics of the breath<strong>in</strong>g signal.<strong>The</strong> FOT device should be specified accord<strong>in</strong>g to the dataprocess<strong>in</strong>g <strong>technique</strong> used <strong>in</strong> the calculation of Zrs (numberand length of time blocks, overlapp<strong>in</strong>g, w<strong>in</strong>dow<strong>in</strong>g, lowpassand/or highpass filter<strong>in</strong>g, way of calculat<strong>in</strong>g coherence function,etc.) [17].Report of results<strong>The</strong> mean and SD of all Zrs data obta<strong>in</strong>ed from successivemeasurements should be reported. <strong>The</strong> coefficient of variation(CV) at every measured frequency is the ma<strong>in</strong> <strong>in</strong>dex of thereliability and repeatability of Zrs data. Reliability <strong>in</strong>dices ofthe <strong>in</strong>dividual measurements, such as the coherence function,are optional to report.In addition to the Rrs and Xrs data measured at a givenfrequency (Rrsf, Xrsf), impedance parameters may be estimatedus<strong>in</strong>g various model analyses. However, model parameters andcurve (polynomial) fitt<strong>in</strong>gs without raw data are unacceptable.Measurement conditionsSubject9s position. Measurements are performed <strong>in</strong> the sitt<strong>in</strong>gposition with the head <strong>in</strong> a neutral or slightly extendedposition. Flexion of the head should be avoided. Dur<strong>in</strong>g themeasurement, the subject (or technician) firmly supports his/her cheeks and the floor of the mouth us<strong>in</strong>g both hands and anoseclip is worn. <strong>The</strong> subject is <strong>in</strong>structed to breathe quietly atFRC level. When measur<strong>in</strong>g young children, allow<strong>in</strong>g theparents to accompany them <strong>in</strong> the lung function laboratoryimproves cooperation. <strong>The</strong> child should be given some time toadjust to the laboratory environment and tra<strong>in</strong>ed to breathequietly through the mouthpiece and to wear the noseclip for ashort period of time. <strong>The</strong> parents can also be given those piecesof equipment to tra<strong>in</strong> their child at home should difficulties beencountered.Volume history. Immediately before the measurement is made,the volume history of the subject should be monitored for atleast 30 s. At least 3 m<strong>in</strong> of quiet breath<strong>in</strong>g should be allowedfor recovery if <strong>forced</strong> respiratory manoeuvres have been madebefore Zrs is measured.Measurement acceptance criteria. Swallow<strong>in</strong>g, glottis closure,leak around the mouthpiece, improper seal with the noseclip,irregular breath<strong>in</strong>g or acute hyperventilation dur<strong>in</strong>g the measurementare reasons to discard the measurement. Most ofthese events can be detected on the flow signal which shouldtherefore be displayed on the screen dur<strong>in</strong>g the measurement. Ifa measurement is considered artefactual, both Rrs and Xrsshould be rejected.Number of measurements. A total of three to five technicallyacceptable measurements should be performed. <strong>The</strong> subjectshould come off the mouthpiece <strong>in</strong> between successive measurements<strong>in</strong> order to establish the short-term variability of Zrs <strong>in</strong> auniform manner. A further <strong>in</strong>dication of basel<strong>in</strong>e variabilitymay be obta<strong>in</strong>ed by repeat<strong>in</strong>g the basel<strong>in</strong>e measurements10–20 m<strong>in</strong> later; this is important <strong>in</strong> the <strong>in</strong>terpretation ofbronchomotor tests, particularly when Zrs is the sole <strong>in</strong>dexused <strong>in</strong> evaluat<strong>in</strong>g bronchial reactivity. Evaluation of a change<strong>in</strong> Rrs <strong>in</strong> response to challenge is dependent on the basel<strong>in</strong>e CVvalue. When basel<strong>in</strong>e reproducibility is poor, further histam<strong>in</strong>e(His) or methachol<strong>in</strong>e (Mch) study is <strong>in</strong>appropriate bothbecause of difficulty with test <strong>in</strong>terpretation and the risk ofunderly<strong>in</strong>g poor asthma control.<strong>The</strong> upper airway artefactWith the standard Zrs,<strong>in</strong> set-up, a component of the measured<strong>in</strong>put flow is lost <strong>in</strong> the oscillatory motion of thecompliant upper airway walls and never enters the lowerrespiratory system. By the support of the cheeks and mouthfloor, it is not possible to elim<strong>in</strong>ate this shunt effect completely[18–20], which <strong>in</strong>creases as Zrs rises. Overall, as upper airwayimpedance (Zuaw) falls steeply with <strong>in</strong>creas<strong>in</strong>g frequency,upper airway shunt<strong>in</strong>g is m<strong>in</strong>imal at low frequencies andbecomes <strong>in</strong>creas<strong>in</strong>gly important as <strong>oscillation</strong> frequency rises.This leads to an artifactual frequency-dependence of Rrs anda shift of Xrs to higher frequencies (with an <strong>in</strong>creased fres) <strong>in</strong>children and adults [19, 20]. <strong>The</strong> upper airway artefact isparticularly important <strong>in</strong> children for whom Zuaw approximatesadult values [21], s<strong>in</strong>ce Zrs is larger <strong>in</strong> children andrises progressively with decreas<strong>in</strong>g age.Several different approaches have been proposed to m<strong>in</strong>imisethe effects of the upper airway shunt. One method usedto correct for the upper airway shunt by separately determ<strong>in</strong><strong>in</strong>gZuaw dur<strong>in</strong>g a Valsalva manoeuvre [18] has been shown toundercorrect Zrs [19, 22], and is also impractical dur<strong>in</strong>g rout<strong>in</strong>eZrs measurements. Another approach is to apply the oscillat<strong>in</strong>gpressure signals around the head and at the mouth (thehead generator <strong>technique</strong> [8]) and this considerably reducesthe motion of the cheeks, m<strong>in</strong>imis<strong>in</strong>g though slightly overcorrect<strong>in</strong>gfor the Zuaw shunt artefact. Compared to thestandard method, use of the head generator <strong>technique</strong> results<strong>in</strong> Rrs values that are larger but less frequency dependent, asteeper <strong>in</strong>crease <strong>in</strong> Xrs with frequency (and therefore lowerfres) and larger Rrs changes dur<strong>in</strong>g Mch challenge that are<strong>in</strong>dependent of basel<strong>in</strong>e Zrs [19, 23, 24]. By us<strong>in</strong>g the change<strong>in</strong> admittance (the <strong>in</strong>verse of impedance) <strong>in</strong>stead of Rrs toexpress the response to bronchoprovocation, the result ispractically free from the upper airway artefact [25], this waypotentially <strong>in</strong>creas<strong>in</strong>g the sensitivity of the conventional set-up.Studies differ <strong>in</strong> their assessment of the convenience of thehead generator <strong>technique</strong>. One study suggested that tolerancewas poor by some subjects and that data rejection <strong>in</strong>creased atlow frequencies (v10 Hz) [24]. However, <strong>in</strong> another studysatisfactory data could be obta<strong>in</strong>ed <strong>in</strong> all the 380 normal adultsubjects but one [26]. In adults, the sensitivity <strong>in</strong> detect<strong>in</strong>gairway obstruction appeared to be similar with both <strong>technique</strong>s[24]. In children, the diagnostic value of Rrs10 <strong>in</strong>identify<strong>in</strong>g responses to bronchodilators improved slightlywith the head generator compared to the standard method,
1030 E. OOSTVEEN ET AL.whereas the parameters derived from Xrs obta<strong>in</strong>ed with thestandard method had a better diagnostic value than the headgenerator <strong>technique</strong> [27].In conclusion, with the standard FOT <strong>technique</strong>, Zrs,especially at higher frequency, is affected by the motion of theupper airway walls. This upper airway shunt results <strong>in</strong> anartificial frequency dependency of Rrs and Xrs is decreasedwith <strong>in</strong>creased fres <strong>in</strong> the presence of a high Zrs. Althoughelim<strong>in</strong>ation of the upper airway shunt dur<strong>in</strong>g standard Zrs,<strong>in</strong>measurement is impossible, firm and uniform support of theupper airway walls should be applied. More accurate Zrs datacan be obta<strong>in</strong>ed us<strong>in</strong>g the head generator <strong>technique</strong>, whichm<strong>in</strong>imises the upper airway shunt. However, further studiesare needed to identify the improvements offered by this method<strong>in</strong> terms of its sensitivity and specificity <strong>in</strong> cl<strong>in</strong>ical <strong>practice</strong>.Reference valuesCl<strong>in</strong>ical applicationsAdults. A relatively limited number of reference studies ofZrs,<strong>in</strong> as a function of frequency exist <strong>in</strong> adult subjects. Healthysubjects exhibit a virtually frequency-<strong>in</strong>dependent Rrs, with afrequency-dependent Xrs usually behav<strong>in</strong>g accord<strong>in</strong>g to an<strong>in</strong>ertance-compliance system exhibit<strong>in</strong>g an fres v10 Hz.An overview of the average Rrs values of healthy adultsubjects reported from different laboratories is given <strong>in</strong>table 1. In half of the studies, relatively young subjects (anaverage age of v35 yrs) were <strong>in</strong>vestigated; the selectioncriterion of the subjects was not always reported, or thesample population was limited to a specific subgroup ofsubjects. Nevertheless, the average Rrs of healthy adultsvaried little among the different studies, and slightly higherRrs values were found for females (0.31 kPa?s?L -1 ) comparedwith males (0.25 kPa?s?L -1 ). Prediction equations for theaverage Rrs and Xrs, and the slope of the Rrs versus f relationshipare given <strong>in</strong> table 2 [32]. ZERAH et al. [33] analysed Rrsdata obta<strong>in</strong>ed <strong>in</strong> 40 healthy volunteers by perform<strong>in</strong>g l<strong>in</strong>earregression on the data from 4–16 Hz, and back-extrapolat<strong>in</strong>gthe regression l<strong>in</strong>e to 0 Hz to obta<strong>in</strong> the parameter Rrs0, andits <strong>in</strong>verse, respiratory conductance at 0 Hz (Grs0). Grs0 wasdependent on height and age but not on sex or body weight.Children. Normal values have been collected by several researchgroups [30, 34–45]. An overview of the regression equations ofRrs as a function of body height is given <strong>in</strong> table 3, and theTable 2. – Prediction equations for the average resistance(Rrs(0)), average reactance (Xrs(0)) and slope of resistance tofrequency (Rrs(1)), and the residual SD (RSD)MaleRrs(0)=-0.2454.Hz0.001564.W–0.00055.Az0.5919 (RSD=0.0493)Rrs(1)=0.00842.H–0.000047.W–0.000018.A–0.0095 (RSD=0.00197)Xrs(0)=0.1479.H–0.000402.W–0.00022.A–0.1721 (RSD=0.0306)FemaleRrs(0)=-0.4300.Hz0.00165.W–0.00070.Az0.9312 (RSD=0.0619)Rrs(1)=0.01176.H–0.000106.W–0.000045.A–0.00817 (RSD=0.00256)Xrs(0)=0.2487.H–0.001700.W–0.00053.A–0.2158 (RSD=0.0406)Rrs(0) and Xrs(0) <strong>in</strong> kPa?s?L -1 , Rrs(1) <strong>in</strong> kPa?s 2 ?L -1 . H: height (m);W: weight (kg); A: age (yrs). Reproduced with permission from [32].correspond<strong>in</strong>g data are shown <strong>in</strong> figure 3. Rrs usually falls<strong>in</strong>versely with height, and, except for one study [34], no sexrelateddifferences <strong>in</strong> Rrs have been described. In most of thesestudies, a similar Rrs versus height dependence has been obta<strong>in</strong>ed.<strong>The</strong> negative frequency-dependence of Rrs becomes morepronounced with decreas<strong>in</strong>g age [34–36, 40, 41]. In smallchildren, fres is high (sometimes w20 Hz) and then decreasesas Xrs becomes less negative with growth. <strong>The</strong> characteristicsof the Xrs versus f relationship are significantly modified whena head generator is used to m<strong>in</strong>imise the upper airway wallmotion, shift<strong>in</strong>g the curve to the left and reduc<strong>in</strong>g fres [20, 46, 47].Clearly, further large scale studies <strong>in</strong> adults across a wideage range are needed to validate exist<strong>in</strong>g reference values. Inchildren, available regression equations of Rrs as a function ofbody height show a fairly close agreement.Reproducibility<strong>The</strong> short term <strong>in</strong>tra-<strong>in</strong>dividual CV of FOT <strong>in</strong>dices <strong>in</strong>healthy adults range 5–15% (table 4), which is comparable tothe variability of resistance values obta<strong>in</strong>ed with other methods(body plethysmography (sGaw), <strong>in</strong>terrupter <strong>technique</strong>, etc).For adult patients with airway obstruction the CV values werehardly different from that of healthy subjects.Similar estimates of short term CV, rang<strong>in</strong>g v5–14% havebeen obta<strong>in</strong>ed <strong>in</strong> children [34, 38, 39, 51, 53–57]. A significantcircadian rhythm has been identified <strong>in</strong> about one-third of anasthmatic children population, although the amplitude of thediurnal variations of Rrs did not exceed 20% [58].<strong>The</strong> day-to-day variability has been reported to be slightlylarger than the with<strong>in</strong>-day variations <strong>in</strong> adults, with a CV of10.0 versus 8.3% [49] and 10.8 versus 8.6% [51]. In children,Table 1. – Overview of the average respiratory resistance (Rrs) value obta<strong>in</strong>ed <strong>in</strong> healthy adults.Reference Selection criteria Frequencyband HzMaleFemaleRrs kPa?s?L -1 n Age yrs Rrs kPa?s?L -1 n Age yrs[28] Male Air Force4–24 0.25 (0.06) 224 26 (10)members/applicants[29] ? 8–24 y0.26 442 29[30] Patients undergo<strong>in</strong>g10 0.29 (0.08) MzF 102 50rehabilitation andhealthy hospital workers[31] ? 6–24 0.26 (0.06) 126 33 (12) 0.30 (0.06) 100 29 (12)[24] "Healthy" subjects10–32 0.26 (0.07) 32 48 (15) 0.34 (0.07) 28 55 (13)referred for lungfunction test<strong>in</strong>g[32] "Healthy" subjectsreferred for lungfunction test<strong>in</strong>g6–24 0.25 (0.05) 137 53 (14) 0.31 (0.07) 140 58 (14)Data are presented as mean (SD). M: male; F: female; n: number of subjects studied.
CLINICAL APPLICATION OF FOT1031Table 3. – Overview of the regression equations of respiratory resistance (Rrs) as a function of height <strong>in</strong> healthy childrenReferenceFrequencyband HzSubjectsnAgeyrsRrs kPa?s?L -1RSD[42] 15–35 16 3–5 Rrs(15–35)=-0.005296Hz1.102[41] 4, 9 130 3–14 Rrs4=2.47–0.0136H[36] 3–10 121 4–16 Rrs4=1.87610 4 6H –2.12[38] 2–26 138 2–16 Rrs6=9.2610 -5 6H 2 –0.03416Hz3.52 0.15[40] 2, 4, 12 218 2–18 log(Rrs4)=4.413–2.186log (H) 10.2%[34] 2–26 255 2–12 Rrs6=0.000176H 2 –0.054076Hz4.77323 0.175[39] 10 377 3–18 Rrs10=1.392–0.006356H 0.066[44] 5 247 3–6.5 Rrs5=-0.0095286Hz2.0643065[45] 8, 12, 16 199 3–17 ln (Rrs8)=10.990–2.3706ln (H)H: height (cm); RSD: residual SD.Rrs kPa·s·L -11.21.110.90.80.70.60.50.40.30.290 100 110 120 130 140 150 160 170 180Height cmFig. 3. – Regression curves or mean values of respiratory resistance(Rrs) versus height <strong>in</strong> different studies. –– : [40]; – – – : [37]; - - - : [36];.......... : [35]; : [41]; : [44]; – - – : [38]; – - - – : [39]; -- -- -- :[42]; : [34]; : [45].the day-to-day CV and the weekly variability were found tobe 16% [54] and 17% [34].Diagnostic capacityWhereas the difference <strong>in</strong> Zrs parameters between subjectswith normal and abnormal spirometry has been repeatedlyTable 4. – Short term (with<strong>in</strong> day) <strong>in</strong>tra-<strong>in</strong>dividual variability of<strong>forced</strong> <strong>oscillation</strong> <strong>technique</strong> (FOT) <strong>in</strong>dices <strong>in</strong> adult, healthysubjects and patientsReference FOT <strong>in</strong>dex Subjects studied CV %[48] Rrs10 Healthy subjects 11.3Asthmatics 10.3[49] Rrs8 Healthy subjects 8.3Asthmatics 10.0[50] |Zrs10| Asthmatics 4.9[12] Rrs4–32 Healthy subjects 4.7[30] Rrs10 Healthy subjects 9.8[51] Rrs10 Healthy subjects 8.6COPD patients 8.8[52] Rrs6 Patients with airway obstruction 15.2[52] Rrs6-26 Patients with airway obstruction 12.1Rrs6, Rrs8, Rrs10: Rrs measured at 6, 8 or 10 Hz; |Zrs10|: modulus at10 Hz; CV: coefficient of variation.po<strong>in</strong>ted out, there is currently no recognised FOT <strong>in</strong>dex of airwayobstruction. Interpretation of Rrs deviations from normal<strong>in</strong>patients and pathological conditions should take <strong>in</strong>to accountthe wide scatter of Rrs values among normal <strong>in</strong>dividuals. Tothis end, the difference between observed and predicted Rrsmay be divided by the SD of the correspond<strong>in</strong>g referencepopulation. This ratio will be referred to as the SD <strong>in</strong>dex.Adults. <strong>The</strong> pattern of change <strong>in</strong> Zrs <strong>in</strong> various pulmonaryfunction abnormalities consists of an <strong>in</strong>crease <strong>in</strong> Rrs, especially<strong>in</strong> the lower frequency range, and a decrease <strong>in</strong> Xrs, associatedwith an <strong>in</strong>crease <strong>in</strong> fres.CLÉMENT et al. [29] demonstrated thatconventional FOT was a sensitive tool to separate healthysubjects from patients with respiratory compla<strong>in</strong>ts (both withand without a reduced <strong>forced</strong> expiratory volume <strong>in</strong> one second(FEV1)). In a later study, the same <strong>in</strong>vestigators showed thatthe sensitivity to detect symptomatic people was similar forFOT and spirometry [32].In adult patients with <strong>in</strong>trapulmonary airway obstruction,Rrs is <strong>in</strong>creased at the lower frequencies and falls with <strong>in</strong>creas<strong>in</strong>gf. <strong>The</strong> negative frequency-dependence of Rrs is expla<strong>in</strong>edon the basis of mechanical <strong>in</strong>homogeneities of the lungs [2].VAN NOORD et al. [59] studied the discrim<strong>in</strong>ative power ofconventional lung function parameters and FOT <strong>in</strong> threegroups of patients suffer<strong>in</strong>g from asthma, chronic bronchitisor emphysema with a similar reduction <strong>in</strong> FEV1. A discrim<strong>in</strong>antanalysis showed that the FOT parameters were amongthe best lung function <strong>in</strong>dices <strong>in</strong> discrim<strong>in</strong>at<strong>in</strong>g between thethree groups; Rrs was highest <strong>in</strong> asthmatics and the frequencydependence of Rrs and decrease <strong>in</strong> Xrs were lowest <strong>in</strong> emphysema.In early emphysema, patients may present with normalvalues of Rrs and Xrs [60]. WESSELING and WOUTERS [61]found abnormal Zrs data <strong>in</strong> 70% of the subjects with chronicbronchitis <strong>in</strong> the presence of normal spirometry.<strong>The</strong> negative frequency dependence of Rrs, which is characteristicof patients with bronchial obstruction, has also beenobserved <strong>in</strong> adult patients with upper airway obstruction butwithout any sign of <strong>in</strong>trapulmonary disease [62]. This f<strong>in</strong>d<strong>in</strong>gcan readily be expla<strong>in</strong>ed by the shunt effect of the upperairway walls on the elevated distal impedance. Although theFOT may fail <strong>in</strong> dist<strong>in</strong>guish<strong>in</strong>g between <strong>in</strong>tra and extrapulmonaryobstruction, it may be very useful for the non<strong>in</strong>vasivediagnosis and follow-up of patients at risk for tracheostenosis[63]. In this recent study, FOT <strong>in</strong>dices proved to be muchmore closely related to the tracheal dimensions than spirometric<strong>in</strong>dices, thus suggest<strong>in</strong>g that FOT is more sensitive <strong>in</strong>disclos<strong>in</strong>g the upper airway stenosis.Surpris<strong>in</strong>gly, no dist<strong>in</strong>ctive patterns <strong>in</strong> Zrs have been observed<strong>in</strong> restrictive lung disorders: the changes <strong>in</strong> Zrs are similar tothose of moderate obstructive lung disease. Greater negativefrequency dependence and higher values of Rrs and decreases<strong>in</strong> Xrs were measured <strong>in</strong> patients with restrictive disorders,
1032 E. OOSTVEEN ET AL.such as fibros<strong>in</strong>g alveolitis [64] and kyphoscoliosis or ankylos<strong>in</strong>gspondylitis [62]. Aga<strong>in</strong>, this observation can be expla<strong>in</strong>edon the basis of the upper airway shunt impedance, which maymask the differences between the alterations <strong>in</strong> pulmonary mechanicsresult<strong>in</strong>g from various respiratory disorders. Furtherstudies employ<strong>in</strong>g the head generator <strong>technique</strong> are necessaryto confirm this assumption. Obese subjects exhibit an <strong>in</strong>creasedRrs result<strong>in</strong>g from a reduction <strong>in</strong> lung volume [65].In conclusion, <strong>in</strong> patients with various diseases associatedwith pulmonary function abnormalities, an <strong>in</strong>crease <strong>in</strong> Rrs,especially <strong>in</strong> the lower frequency range, and a decrease <strong>in</strong> Xrswith a concomitant <strong>in</strong>crease <strong>in</strong> fres, are observed. However,the standard FOT does not offer the dist<strong>in</strong>ction between theunderly<strong>in</strong>g restrictive and obstructive changes, or <strong>in</strong>tra andextrapulmonary disorders.Children. Stable asthma. Most FOT studies <strong>in</strong> well characterisedpaediatric asthma deal with children <strong>in</strong> a stablecondition who undergo provocation tests (see below), andrelatively few data are available regard<strong>in</strong>g the assessment ofbasel<strong>in</strong>e airway obstruction. In an early study by COGSWELL[37] 23 of 42 asthmatic children showed an Rrs5 SD <strong>in</strong>dexw2. LEBECQUE and STANESCU [66] found that Rrs10 provided<strong>in</strong>formation concordant with FEV1 <strong>in</strong> most asthmaticchildren. HOLMGREN et al. [67] observed a larger basel<strong>in</strong>eRrs4 SD <strong>in</strong>dex <strong>in</strong> asthmatic children compared with healthycontrols, <strong>in</strong> keep<strong>in</strong>g with the FEV1 SD <strong>in</strong>dex. In a largepopulation of children with various respiratory conditions,<strong>in</strong>clud<strong>in</strong>g chronic cough and asthma, Rrs was characterisedby the extrapolated Rrs0 value [57]. <strong>The</strong> SD <strong>in</strong>dex of Rrs0was significantly larger <strong>in</strong> children with abnormal FEV1than <strong>in</strong> those with normal FEV1 and, with<strong>in</strong> the latterpopulation, significantly different between the children withnormal and those with abnormal midexpiratory flow.Rrs measured by the FOT <strong>in</strong> the lower range of thefrequency spectrum is significantly different between healthyand asthmatic children, and it dist<strong>in</strong>guishes between theasthmatics with and without abnormal spirometry. Furtherresearch is needed to establish a practical FOT <strong>in</strong>dex to def<strong>in</strong>eairway obstruction on a rout<strong>in</strong>e basis.Acute asthma. A recent study evaluated the feasibility ofFOT <strong>in</strong> an emergency department, assess<strong>in</strong>g 150 children (age2–17 yrs) [68]. One-quarter of the subjects (median age 3 yrs)were unable to breathe steadily via the measur<strong>in</strong>g device.<strong>The</strong> success rate for achiev<strong>in</strong>g reproducible measurements<strong>in</strong>creased from 0% (at age 2 yrs) to 83% (at age 5 yrs),respectively. Across all ages, the ability to cooperate withspirometry and its reproducibility was similarly poor. Rrs8% pred was found to correlate with cl<strong>in</strong>ical asthma severity[68]. A further emergency room study <strong>in</strong> preschoolchildrenrevealed how Rrs8 related only marg<strong>in</strong>ally to asthma severityrat<strong>in</strong>gs, but showed that significant correlations betweenthese two rat<strong>in</strong>g methods were present when assess<strong>in</strong>g responsesto treatment [69].In acute asthma, FOT measurements may prove useful forobjectively assess<strong>in</strong>g bronchodilator responses and to a lesserextent <strong>in</strong> scor<strong>in</strong>g asthma severity. Limitations of FOT <strong>in</strong>preschoolchildren <strong>in</strong>clude lack of cooperation, poor toleranceof the dead space of the test <strong>in</strong>strument, poor signal-to-noiseratios due the more rapid respiratory rate, and impaireddiscrim<strong>in</strong>ative power, due to the <strong>in</strong>creased <strong>in</strong>fluence of theupper airway wall compliance. Methodological improvements<strong>in</strong> FOT may ameliorate some of these factors.Cystic fibrosis. In children with cystic fibrosis (CF), Zrsexhibits a generally poor relationship to the conventionalspirometric <strong>in</strong>dices [37, 66, 70, 71]. Specifically, FEV1correlated poorly to Rrs10 [66] and Rrs6 [71], <strong>in</strong> sharp contrastto the good agreement observed <strong>in</strong> asthmatics [66].As the relationship between spirometry and plethysmographicRaw was similarly poor, this problem is unlikely to beunique to FOT. In CF patients who demonstrated paradoxicalresponse to a bronchodilator, the decrease <strong>in</strong> FEV1<strong>in</strong>duced by salbutamol was not paralleled by an <strong>in</strong>crease<strong>in</strong> Rrs6 [71]. From this, salbutamol was postulated to relievebronchoconstriction and <strong>in</strong>crease airway wall compliance.Consequently, Rrs was decreased dur<strong>in</strong>g tidal breath<strong>in</strong>g butflow limitation dur<strong>in</strong>g <strong>forced</strong> expiration was facilitated [71].<strong>The</strong> discrepant <strong>in</strong>formation between FOT and spirometry<strong>in</strong> CF patients may reflect alterations <strong>in</strong> the elastic propertiesof the bronchial wall. Whatever the mechanisms, the rout<strong>in</strong>eassessment of lung function <strong>in</strong> these children should be<strong>in</strong>terpreted with much caution, when either spirometry orFOT is available alone. Further comparative assessments are<strong>in</strong>dicated to clarify the mechanisms of impairment <strong>in</strong>respiratory function <strong>in</strong> CF.Chronic lung disease of prematurity. In a small populationof children with a history of premature birth andchronic lung disease studied at a mean age of 6 yrs, thevalues of Rrs6 were weakly related to the cl<strong>in</strong>ical history,whereas the frequency dependence of Rrs was a moresensitive <strong>in</strong>dex <strong>in</strong> discrim<strong>in</strong>at<strong>in</strong>g between children with andwithout chronic lung disease [72]. At a mean age of 8 yrs,significant alterations <strong>in</strong> Rrs5 and Xrs5 were observed <strong>in</strong>subjects with chronic lung disease as compared with thehealthy controls. Furthermore, Xrs5 and fres bothdifferentiated between the presence and absence of chronicdisease <strong>in</strong> premature <strong>in</strong>fants [73]. In the same study, Xrs5and Rrs5 also showed significant correlations with FEV1.A good agreement between Rrs5 and plethysmographicRaw was reported up to 1 kPa?s?L -1 , while the relationshipplateaued at higher values of Raw [73], possibly becauseof the <strong>in</strong>creased impact of the upper airway artefact [23].In conclusion, abnormal Rrs and Xrs may be found atschool age <strong>in</strong> children with a history of premature birth andchronic lung disease. However, more studies are needed to characterisethe changes <strong>in</strong> Zrs dur<strong>in</strong>g growth <strong>in</strong> these children.Follow-up and field studiesIn evaluat<strong>in</strong>g the development of pulmonary disease, thelong-term monitor<strong>in</strong>g of therapeutic efficiency and the stag<strong>in</strong>gof respiratory function decl<strong>in</strong>e dur<strong>in</strong>g ag<strong>in</strong>g, FOT provides aconvenient follow-up <strong>technique</strong> [74]. However, for longitud<strong>in</strong>alfollow-up of chronic obstructive pulmonary disease(COPD) patients, changes <strong>in</strong> Rrs up to 26% may result fromspontaneous variation <strong>in</strong> resistance [51].Smok<strong>in</strong>g. In an early study, use of FOT alone failed toclearly separate smokers from nonsmokers [28]. COE et al. [75]analysed Rrs and its frequency dependence <strong>in</strong> healthy neversmokersand <strong>in</strong> smokers. <strong>The</strong>re was a strong trend for Rrs(especially at lower frequencies) and the frequency dependenceof Rrs to elevate with <strong>in</strong>creas<strong>in</strong>g age <strong>in</strong> the smokers. Increases<strong>in</strong> Rrs and the frequency dependence of Rrs were usually presentwhen spirometry <strong>in</strong>dicated bronchial obstruction. <strong>The</strong>frequency dependence of Rrs proved even somewhat more sensitivethan spirometry <strong>in</strong> the detection of mild airway disease.<strong>The</strong> frequency dependence of Rrs and its change betweenair and helium (He)/oxygen (O 2 ) breath<strong>in</strong>g were shown to bemore sensitive than the results of spirometry <strong>in</strong> the detectionof early airway abnormalities associated with smok<strong>in</strong>g historyand occupational exposure [76]. A study on the additional
CLINICAL APPLICATION OF FOT1033effects of smok<strong>in</strong>g habits on the activity of m<strong>in</strong>ers showedthat, although FOT provided sensitive <strong>in</strong>dices of the effect ofoccupational exposure on central airways, it did not detect theadditional effect of smok<strong>in</strong>g [77].Epidemiological surveys and field studies. <strong>The</strong> <strong>in</strong>formationoffered by FOT on respiratory impairment is <strong>in</strong> everyway as significant as spirometry and FOT does not requireactive cooperation. Feasibility <strong>in</strong> various epidemiologicalsurveys and field studies has been excellent [78]. Both thestandard and head generator methods exhibit comparablepotential to classify a variety of respiratory status measuresamongst agricultural workers (smok<strong>in</strong>g status, cough,expectoration and airway obstruction assessed by maximumexpiratory flow/volume curve) [79].FOT has proved as sensitive as spirometry <strong>in</strong> the detectionof impairment <strong>in</strong> ventilatory function <strong>in</strong> workers exposed tooccupational dangers [80, 81].<strong>The</strong> performance of FOT <strong>in</strong> the assessment of bronchialhyperresponsiveness (BHR), as compared with spirometrywas studied <strong>in</strong> 119 active workers with normal basel<strong>in</strong>epulmonary function [81]. When a 65% <strong>in</strong>crease <strong>in</strong> Rrs0 wasused to classify the subjects accord<strong>in</strong>g to the presence orabsence of a 20% fall <strong>in</strong> FEV1, FOT reached a sensitivity of75% and a specificity of 76%. Us<strong>in</strong>g a simplified FOT <strong>in</strong>dex,the two-po<strong>in</strong>t dose response slope of the change <strong>in</strong> Rrs10,BOHADANA et al. [82] established a sensitivity of 91% and aspecificity of 96% <strong>in</strong> the accurate detection of "spirometric"BHR <strong>in</strong> various patients referred for BHR test<strong>in</strong>g. Thissuggests that this simple <strong>in</strong>dex can be used for BHR test<strong>in</strong>g <strong>in</strong>occupational epidemiology.In sickle cell disease, an <strong>in</strong>crease <strong>in</strong> Rrs is correlated withthe number of acute chest syndrome episodes, which demonstratesthat obstructive lung dysfunction is fairly common <strong>in</strong>this type of disease [83].In a survey of respiratory health <strong>in</strong>volv<strong>in</strong>g w1,500 childrenaged 6–12 yrs, measurements of Zrs failed to differentiatesymptom-free children from those with a history of chroniccough or asthma-like symptoms <strong>in</strong> the previous year [35]. Thiswas thought to reflect either the poor diagnostic value of the<strong>technique</strong> or the lack of functional abnormality associatedwith such a history of respiratory symptoms.In conclusion FOT has proven to be at least as sensitiveas spirometry to detect impairment of lung function due toexposure to cigarette smoke or occupational hazards. <strong>The</strong>sensitivity to detect mild airway disease and the m<strong>in</strong>imalrequirements for subject9s cooperation make FOT a very suitablelung function test for epidemiological and field studies.Identification of airway reactivity<strong>The</strong> <strong>in</strong>terpretation of changes <strong>in</strong> a lung function parametermeasured <strong>in</strong> response to bronchomotor agents must rely onan estimate of the variability of that parameter. For <strong>in</strong>stance,a response larger than twice the average basel<strong>in</strong>e CV is usuallyconsidered positive. <strong>The</strong> magnitude of the change <strong>in</strong>duced bybronchodilat<strong>in</strong>g or bronchoconstrict<strong>in</strong>g agents can also beexpressed as the difference between postbronchodilator (orchallenge) Rrs and Rrs at basel<strong>in</strong>e divided by the (average<strong>in</strong>trasubject) SD of the basel<strong>in</strong>e measurements. This ratio willbe referred to as the SD score.ReversibilityAdults. <strong>The</strong> first reports on the changes <strong>in</strong> Zrs <strong>in</strong> response tobronchodilation <strong>in</strong> COPD patients were based on measurementsmade <strong>in</strong> a very limited number of patients [18, 84].Overall, Rrs decreases after bronchodilation, especially at lowfrequencies. This reduces the negative frequency dependence ofRrs, and, by <strong>in</strong>creas<strong>in</strong>g Xrs, fres returns towards lower and morenormal values. Study<strong>in</strong>g Zrs changes <strong>in</strong> COPD patients,WOUTERS et al. [85] noted that only Xrs data showed significantchanges, whereas low-frequency data suffered from poorcoherence. In a large group of patients with airway obstruction(presumably ma<strong>in</strong>ly COPD patients), VAN NOORD et al. [52]observed significant postdilator falls <strong>in</strong> Rrs, with a significantcorrelation between FEV1 and Rrs6. In this study, a thresholdvalue for significant bronchodilation was def<strong>in</strong>ed from thewith<strong>in</strong>-subject variability of the different lung function <strong>in</strong>dices,a decrease of w45% <strong>in</strong> Rrs6 from basel<strong>in</strong>e value. Here, FOT<strong>in</strong>dices were markedly less sensitive than body plethysmographicor spirometric <strong>in</strong>dices for detect<strong>in</strong>g significant bronchodilation.By contrast, ZERAH et al. [33], who studied thereversibility of airway obstruction <strong>in</strong> two small yet well-def<strong>in</strong>edgroups of patients with asthma and COPD, came to preciselythe opposite conclusion. Employ<strong>in</strong>g a threshold value of 10%predicted for both <strong>in</strong>dices, the changes <strong>in</strong> FEV1 and Grs0 afterbronchodilator <strong>in</strong>halation were compared. FEV1 and Grs0both exhibited comparable changes with a similar sensitivityand specificity to differentiate asthmatics from COPD patients.<strong>The</strong>se authors concluded that FOT can be used as analternative, equivalent <strong>technique</strong> to <strong>forced</strong> expiration toassess the degree of bronchodilation.It is obvious that the correlation between the changes <strong>in</strong>FEV1 and those <strong>in</strong> Zrs <strong>in</strong>dices strengthens with <strong>in</strong>creas<strong>in</strong>g responseto bronchodilation. <strong>The</strong>refore, the correlation betweenspirometry and Zrs is dependent on the population studied(asthmatics versus COPD patients).To summarise, there is no consensus regard<strong>in</strong>g the sensitivityof Zrs measurement compared with that of spirometryand the correlation between their <strong>in</strong>dices <strong>in</strong> bronchodilationtest<strong>in</strong>g. Further research <strong>in</strong> larger, well-def<strong>in</strong>ed groups isneeded to establish whether FOT and spirometry areequivalent or complementary lung function <strong>technique</strong>s <strong>in</strong>the assessment of reversibility of airway obstruction.Children. Indirect evidence of airway obstruction associatedwith asthma may be provided by a positive response to abronchodilator. In a large population of children with chronicrespiratory symptoms, the best cut-off value to establishsignificant reversibility <strong>in</strong> response to salbutamol with referenceto an <strong>in</strong>crease <strong>in</strong> FEV1 o10% pred was a decrease <strong>in</strong> Rrs0of o-1 SD score, or equivalently a 27.8% decrease <strong>in</strong> Rrs0 [57].This cut-off value was associated with a sensitivity andspecificity of 69% and 78%, respectively. In addition, <strong>in</strong>children unable to perform <strong>forced</strong> expiration manoeuvres, thecut-off value identified a subgroup of patients whose highbasel<strong>in</strong>e Rrs0 normalised after bronchodilator <strong>in</strong>halation [57].In a study of asthmatic children, <strong>in</strong>halation of salbutamol<strong>in</strong>duced a decrease <strong>in</strong> Rrs10 from 155–99% pred, whichcorresponded to an <strong>in</strong>crease <strong>in</strong> FEV1 from 65–85% pred [66]. Inchildren treated for acute asthma <strong>in</strong> a paediatric emergencydepartment, the decrease <strong>in</strong> Rrs8 after salbutamol was found tocorrelate with the reduction of signs of respiratory distress andthe improvement <strong>in</strong> FEV1. In those children unable to performspirometric manoeuvres, the reduction <strong>in</strong> Rrs8 after salbutamolwas also associated with a cl<strong>in</strong>ical response, and the optimalchange <strong>in</strong> Rrs8 to assess reversibility was 19% [86]. Below aged7 yrs, considerable overlap exists <strong>in</strong> bronchodilator responsebetween healthy and asthmatic children. An average decreaseof 12% <strong>in</strong> Rrs5 was observed <strong>in</strong> the healthy children; to exceedthe 95% confidence <strong>in</strong>terval for bronchodilator response <strong>in</strong>healthy children, a cut-off value of a 41% decrease <strong>in</strong> Rrs5should be used to support the diagnosis of asthma <strong>in</strong>reversibility test<strong>in</strong>g [44]. In young children, FOT has been
1034 E. OOSTVEEN ET AL.shown to provide a useful and objective method to assessairway responses to bronchodilator drugs, such as metaproterenol,ipratropium bromide or salbutamol versus placebo[87–90], and to characterise dose/response curves [88, 91]. Forexample, the bronchodilat<strong>in</strong>g effect of nebulised oxitropiumbromide (750 and 1500 mg) <strong>in</strong> preschool asthmatic children wasshown to last for up to 4 h post<strong>in</strong>halation, whereas no additivebronchodilation by fenoterol could be shown [92] .When def<strong>in</strong><strong>in</strong>g reversibility of airway obstruction, the FOTcriterion should take <strong>in</strong>to account the "normal" physiologicalresponse to <strong>in</strong>haled b 2 agonist. This has been reported to be a12% decrease from the basel<strong>in</strong>e value for Rrs <strong>in</strong> youngchildren. Us<strong>in</strong>g comparison with spirometry, the optimumdef<strong>in</strong>ition of significant bronchodilation has been def<strong>in</strong>ed as adecrease <strong>in</strong> Rrs of o1 SD score. However, more research isneeded <strong>in</strong> well-def<strong>in</strong>ed and different age groups of children toconfirm that this cut-off level is appropriate.Bronchial hyperresponsiveness<strong>The</strong> degree of airway responsiveness is commonly assessedwith a bronchial challenge test where His, or Mch, isadm<strong>in</strong>istered <strong>in</strong> <strong>in</strong>creas<strong>in</strong>g doses until either a bronchoconstrictionis observed or a preset maximum concentration hasbeen reached. Cl<strong>in</strong>ical methodology for BHR test<strong>in</strong>g has beenstandardised and the result of the test is expressed as theprovocative dose (PD) or concentration (PC), which <strong>in</strong>duces apredeterm<strong>in</strong>ed deterioration of lung function, usually def<strong>in</strong>edas a decrease <strong>in</strong> FEV1 of 20% of the basel<strong>in</strong>e value, noted asthe PD20FEV1 or PC20FEV1 [93, 94]. In terms of FOTparameters, the dose of the bronchoconstrictor agent thatproduces a 50% <strong>in</strong>crease <strong>in</strong> Rrs, or equivalently a 33%decrease <strong>in</strong> Grs, will be noted as PD50Rrs or PD33Grs.Adults. A significant correlation between the changes <strong>in</strong> Rrsand FEV1 follow<strong>in</strong>g bronchoconstriction has been reported byseveral <strong>in</strong>vestigators [50, 81, 95–97]. SNASHALL et al. [50]compared FEV1 to the modulus of Zrs at 10 Hz (|Zrs10|) <strong>in</strong> theassessment of BHR <strong>in</strong> 24 asthmatic patients; the <strong>in</strong>crease <strong>in</strong>|Zrs10| after challenge was on average 2.7 times as much as thedecrease <strong>in</strong> FEV1. Based on the average with<strong>in</strong>-subject CV,they argued that PC30|Zrs10| was equivalent to PC20FEV1. Inall but one patient, PC20FEV1 was larger than PC30|Zrs10|, and<strong>in</strong> six patients PC20FEV1 was more than two doubl<strong>in</strong>g doses ofPC30|Zrs10|. In another study, PC20FEV1 was compared withPC40Rrs8 when analys<strong>in</strong>g the response to His and Mchchallenge <strong>in</strong> 23 stable asthmatics [97]. For both agents,PC40Rrs8 was about three times lower than PC20FEV1. Us<strong>in</strong>gthe same argument on the average with<strong>in</strong>-subject CV,BOHADANA et al. [82] compared PD47Rrs10 (and PD47Rrsmean)to PD20FEV1 <strong>in</strong> assess<strong>in</strong>g BHR to carbachol challenge.However, by us<strong>in</strong>g this cut-off value, far more patients wereclassified as positive responders than based on FEV1 (forRrsmean and Rrs10, 58 and 52 positive responders of the 71tested patients, respectively, compared to the 23 positiveresponders for FEV1). In volunteers subjected to His challenge,NEILD et al. [48] showed that PD35Rrs10 was comparable toPD10FEV1, and, consequently, lower than PD20FEV1. <strong>The</strong>repeatability of PD35Rrs10 was slightly lower than that ofPD10FEV1. VAN NOORD et al. [98] compared PD15FEV1,PD47Grs6 and PD40sGaw <strong>in</strong> analys<strong>in</strong>g the response to Hischallenge <strong>in</strong> 53 subjects with a history of episodic wheez<strong>in</strong>g.<strong>The</strong> parameters with the best sensitivity to detect the effect ofHis were, <strong>in</strong> decreas<strong>in</strong>g order, sGaw, Grs6 and FEV1; theirresults also suggested that the sensitivity of Grs6 was largerthan that of FEV1 <strong>in</strong> subjects with a more pronouncedbronchial hyperreactivity. FOT was also compared withspirometry <strong>in</strong> the assessment of BHR <strong>in</strong> an active work<strong>in</strong>gpopulation [81]; the best cut-off po<strong>in</strong>t was an <strong>in</strong>crease of 65% <strong>in</strong>Rrs0, which reached a sensitivity of 75% and a specificity of 76%with PD20FEV1 as the gold standard for classification of thesubjects. SCHMEKEL and SMITH [99] used <strong>in</strong>halation of cold airas a bronchial challenge test <strong>in</strong> both asthmatics and healthycontrols. <strong>The</strong>ir results <strong>in</strong>dicated that FOT was more able todiscrim<strong>in</strong>ate between the two groups than spirometry, whenus<strong>in</strong>g the cl<strong>in</strong>ical diagnosis as the gold standard. fres had thehighest specificity (100%) and sensitivity (89%), and even Rrs5had a higher diagnostic capacity than FEV1 (specificity andsensitivity of 89% and 88%, and 88% and 73% for Rrs5 andFEV1, respectively). CHINET et al. [100] compared FOT (Grs0)with sGaw <strong>in</strong> provid<strong>in</strong>g <strong>in</strong>formation on bronchial sensitivity.<strong>The</strong>y found a close relationship between Grs0 and sGaw <strong>in</strong>terms of threshold dose and the slope of the dose/responsecurves <strong>in</strong> normal and hyperresponsive subjects, with equivalencebetween PD50sGaw and PD42Grs0.<strong>The</strong> deep <strong>in</strong>spiration that precedes <strong>forced</strong> expiration maymodify airway smooth muscle tone, and, therefore, may<strong>in</strong>fluence the result of the BHR test. FOT has the considerableadvantage that it measures airway properties dur<strong>in</strong>g quietbreath<strong>in</strong>g. This may be the reason why FOT has proved moresensitive than FEV1 to detect changes <strong>in</strong> BHR <strong>in</strong> asthmaticsafter corticosteroid treatment [101].FOT has been used to study the site of airway obstructiondur<strong>in</strong>g <strong>in</strong>duced bronchoconstriction <strong>in</strong> normal subjects [102,103] and <strong>in</strong> asthmatics [104], to evaluate the response to<strong>in</strong>haled allergen <strong>in</strong> asthmatics [96], to exam<strong>in</strong>e the effect ofposture [105] and hypoxia on BHR [106] and to <strong>in</strong>vestigatethe ventilatory pattern after <strong>in</strong>duced bronchoconstriction <strong>in</strong>asthmatics and normal subjects [107].In conclusion, the values of Rrs (or Grs) at low frequencyhave been shown to be reliable and sensitive <strong>in</strong>dices to assessthe bronchial response <strong>in</strong> cl<strong>in</strong>ical BHR test<strong>in</strong>g. <strong>The</strong>re isevidence that FOT and plethysmography provide comparable<strong>in</strong>formation on bronchial sensitivity and responsiveness andmay be superior to spirometry. It is not yet clear which cut-offvalue for Rrs corresponds best to the 20% decrease <strong>in</strong> FEV1.Threshold values up to the 47% <strong>in</strong>crease <strong>in</strong> Rrs have beenassociated with lower PD, or a higher number of positiveresponders than <strong>in</strong> the case of PD20FEV1; other studiesestimate this threshold value between 65–90% <strong>in</strong>crease <strong>in</strong>Rrs.Children. <strong>The</strong> Mch or His dose/response curves have usuallybeen characterised by the values of PD40Rrs or PD50Rrs. Mostof the mean<strong>in</strong>gful FOT data have been obta<strong>in</strong>ed at lowfrequency. A better sensitivity to detect a bronchial reaction toallergen challenge was reported for Rrs4 (determ<strong>in</strong>ed us<strong>in</strong>gs<strong>in</strong>usoidal excitation) than for FEV1 <strong>in</strong> asthmatic schoolchildrenaged 6–14 yrs [53]. Significant l<strong>in</strong>ear relationshipsbetween changes <strong>in</strong> FEV1 and Rrs <strong>in</strong>dices were observed byDUIVERMAN et al. [108] and LEBECQUE et al. [109] dur<strong>in</strong>g Mchand His provocation, respectively. In 20 asthmatic childrenaged 9–16 yrs, the PD40Rrs6 was found to correlate well withPD20FEV1 [108]. A close relationship was found between theeffect of His and of Mch <strong>in</strong> asthmatic children, aged 3–7 yrs, asdeterm<strong>in</strong>ed with FOT [110]. <strong>The</strong> sensitivity of Zrs values tocarbachol challenge <strong>in</strong> children aged 5–16 yrs was foundequivalent to that of specific airway resistance (sRaw) [55]. In apopulation of asthmatics aged 8–15 yrs, the response to Hiswas similarly estimated by transcutaneously determ<strong>in</strong>ed PO 2(PtcO 2 ) and Rrs4, and PD50Rrs4 was <strong>in</strong>versely correlated to thecl<strong>in</strong>ical severity of asthma [67]. By contrast, <strong>in</strong> a detailed study<strong>in</strong> children aged 5 yrs, compar<strong>in</strong>g the Mch-<strong>in</strong>duced changes <strong>in</strong>Zrs,<strong>in</strong> and PtcO 2 , a low diagnostic power for Rrs6 and Rrs8 wasobserved [111]. FOT has been evaluated <strong>in</strong> young asthmaticsfor the detection of the response to Mch <strong>in</strong> comparison with
CLINICAL APPLICATION OF FOT1035PtcO 2 ,sRaw and the Rrs measured by the <strong>in</strong>terrupter <strong>technique</strong>(Rrs,<strong>in</strong>t). <strong>The</strong> sensitivity was lower for Xrs5 than for sRaw, butlarger than for PtcO 2 , Rrs 5 or Rrs,<strong>in</strong>t <strong>in</strong> the children aged 2–4 yrs[112]. In the asthmatics aged 4–6 yrs, a better sensitivity <strong>in</strong>detect<strong>in</strong>g the Mch response was observed for Rrs5 and Xrs5than for sRaw, PtcO 2 , Rrs,<strong>in</strong>t and FEV1, whereas the higherfrequencyvalues of Rrs and Xrs were apparently not associatedwith a good diagnostic score [113].In the pattern of impedance change after provocation, the<strong>in</strong>crease <strong>in</strong> Rrs was accompanied by a decrease <strong>in</strong> Xrs <strong>in</strong> mostof the studies. S<strong>in</strong>ce the apparent elastic properties of therespiratory system as reflected by Xrs at lower frequencies[112, 114], appear as a sensitive measure <strong>in</strong> the provocationtests, the variations of the Xrs values should be documented.FOT measurements have shown to reliably reflect thechanges <strong>in</strong> lung function dur<strong>in</strong>g bronchial challenge <strong>in</strong>children, with sensitivity comparable to that of bodyplethysmographyand spirometry. PD50Rrs is closely related toPD20FEV1. <strong>The</strong>re are <strong>in</strong>dications that Xrs may be moresensitive than Rrs to detect the response to bronchial challenge,especially <strong>in</strong> the very young child, but more research isneeded to establish the place of Xrs <strong>in</strong> the evaluation of BHR.Additionally, it is recommended that measurement of Zrs isassociated with the careful cl<strong>in</strong>ical evaluation, which <strong>in</strong>cludesmonitor<strong>in</strong>g of transcutaneous sO 2 dur<strong>in</strong>g bronchial challenge.<strong>The</strong>se aspects are important because of the lack of criteria todef<strong>in</strong>e airway obstruction <strong>in</strong> the basel<strong>in</strong>e condition, especially<strong>in</strong> the young child.Forced <strong>oscillation</strong> <strong>technique</strong> <strong>in</strong> <strong>in</strong>fancyLike other pulmonary function tests <strong>in</strong> this age group, poorcooperation means that Zrs must be measured dur<strong>in</strong>gsedation and that test<strong>in</strong>g can be lengthy and technicallyextremely demand<strong>in</strong>g. For this reason, collection of normalZrs data <strong>in</strong> <strong>in</strong>fants has been hampered, as have rout<strong>in</strong>eapplications of FOT <strong>in</strong> this subject group.Standardisation of the measurement conditions for lungfunction test<strong>in</strong>g is a crucial issue for the <strong>in</strong>fant9s safety and theaccuracy of the test. Recommendations have been developedby an American Thoracic Society/European RespiratorySociety Work<strong>in</strong>g Party [115] and the specific preparationmeasures for the FOT and details of the methodologyhave been described by DESAGER et al. [116]. <strong>The</strong> largevalues of Zrs <strong>in</strong> <strong>in</strong>fants impose particularly strict performancerequirements concern<strong>in</strong>g the measurement set-up and thecalibration procedure [117–119].Most studies <strong>in</strong> <strong>in</strong>fants deal with validation of the <strong>technique</strong>.<strong>The</strong> measurements of Zrs have shown to be reproduciblewith an average difference <strong>in</strong> Rrs from measurements made15 m<strong>in</strong> apart of 0.5¡5.7% [118], and a reasonably goodcorrelation has been reported between the results of FOT andthose of the s<strong>in</strong>gle-breath occlusion method [120]. <strong>The</strong> impactof the upper airway wall shunt [121, 122] and the nasalbreath<strong>in</strong>g [123] on Zrs has been evaluated. <strong>The</strong> nasal Z wasshown to correlate with the cl<strong>in</strong>ical observation of nasalobstruction [123]. <strong>The</strong> feasibility of the FOT dur<strong>in</strong>g artificialventilation has been demonstrated <strong>in</strong> <strong>in</strong>fants with bronchiolitis[124] and FOT has proved to be helpful <strong>in</strong> titrat<strong>in</strong>g optimalpositive end-expiratory pressure [125]. In a prospective cohortstudy, low values of Grs6 measured dur<strong>in</strong>g the neonatalperiod were reported to represent a significant risk factor forthe occurrence of wheez<strong>in</strong>g later <strong>in</strong> <strong>in</strong>fancy [126]. FOT comb<strong>in</strong>edwith FRC measurements detected lung function abnormalities<strong>in</strong> a m<strong>in</strong>ority of wheez<strong>in</strong>g <strong>in</strong>fants dur<strong>in</strong>g a symptom-free<strong>in</strong>terval [127]. Support<strong>in</strong>g previously cl<strong>in</strong>ical observations, thecharacteristic bronchodilator effects of nebulised salbutamol,phenylefr<strong>in</strong>e, fenoterol and ipratropium bromide were confirmedus<strong>in</strong>g FOT [128]. No cl<strong>in</strong>ical or bronchodilat<strong>in</strong>g effectof furosemide was observed <strong>in</strong> <strong>in</strong>termittently <strong>in</strong>fant wheezers[129]. Recently, methodological and cl<strong>in</strong>ical feasibility studieshave employed special low and high-frequency test signalsand these are addressed <strong>in</strong> the next section.New developmentsApplications of <strong>forced</strong> <strong>oscillation</strong> <strong>technique</strong> <strong>in</strong> monitor<strong>in</strong>grespiratory mechanics<strong>The</strong> FOT has recently been applied to follow the changes <strong>in</strong>respiratory mechanics dur<strong>in</strong>g conventional mechanical ventilation(CMV), respiratory manoeuvres and sleep studies.Monitor<strong>in</strong>g of Zrs may be a useful complementary tool <strong>in</strong> theadaptation of ventilator sett<strong>in</strong>gs dur<strong>in</strong>g <strong>in</strong>vasive and non<strong>in</strong>vasiveventilation [130–135]. <strong>The</strong> FOT has also been usedto improve the diagnosis of sleep disturbances [136] and todeterm<strong>in</strong>e the optimal cont<strong>in</strong>uous positive airway pressure(CPAP) level required to treat obstructive sleep apnoea[137–140]. In sleep studies, changes of Zrs along the breath<strong>in</strong>gcycle are followed, s<strong>in</strong>ce obstructive sleep apnoeas/hypopnoeasare characterised by marked changes with<strong>in</strong> the breath<strong>in</strong>gcycle [138]. Separate analysis of <strong>in</strong>spiratory and expiratoryimpedance has also been suggested <strong>in</strong> the monitor<strong>in</strong>g ofthe mechanically ventilated patients [130]. S<strong>in</strong>gle-frequencyFOT has recently been proved an ideal tool to track Rrs orpulmonary resistance dur<strong>in</strong>g a respiratory manoeuvre <strong>in</strong>clud<strong>in</strong>ga deep <strong>in</strong>halation [141, 142], s<strong>in</strong>ce it offers a good temporalresolution and the small amplitude <strong>oscillation</strong>s do not <strong>in</strong>terferewith the mechanical changes evoked by the manoeuvre.<strong>The</strong> application of FOT <strong>in</strong> patients subjected to positivepressure requires a modification of the conventional FOTsystem based on a loudspeaker. Different approaches havebeen proposed to apply <strong>forced</strong> <strong>oscillation</strong>s at elevated airwaypressure [130, 133, 138, 143–145]. If the <strong>oscillation</strong>s areapplied through a nasal/face mask or ETT, further technicalproblems need to be taken <strong>in</strong>to consideration. First, imperfectseal<strong>in</strong>g around the mask or the ETT can cause air leaks, soprovid<strong>in</strong>g a shunt pathway that leads to a misestimation ofZrs. Secondly, when us<strong>in</strong>g a full face mask <strong>in</strong> which thepatient can breathe freely through the nose or the mouth, theactual route of breath<strong>in</strong>g must be known, s<strong>in</strong>ce the nasalimpedance constitutes a significant fraction of Zrs [133].Thirdly, for <strong>in</strong>tubated patients, the high impedance and nonl<strong>in</strong>earbehaviour of the ETT pose a further problem, whichcan be circumvented by measur<strong>in</strong>g the tracheal pressure [146].An alternative approach is to correct the Zrs values for theeffective impedance of the ETT [130] estimated <strong>in</strong> vitro us<strong>in</strong>gsimilar flow conditions to those of <strong>in</strong> vivo measurements.Low-frequency <strong>oscillation</strong>sIf the oscillatory signal is superimposed on spontaneousbreath<strong>in</strong>g, <strong>oscillation</strong> frequencies higher than 2–4 Hz must beused. However, the characteristic rheology of the respiratorytissues below 2 Hz can be revealed by <strong>in</strong>vestigation dur<strong>in</strong>gvoluntary apnoea, as has been shown us<strong>in</strong>g a modified set-up<strong>in</strong> normal subjects between 0.25–5 Hz [147] and <strong>in</strong> anaesthetisedand paralysed patients from 0.25–32 Hz [146] or to26 Hz [143]. <strong>The</strong> advantages of the low-frequency range arethat the markedly different frequency dependences of the airwayand tissue impedance allow the model-based separateestimation of their parameters [148], and that these parametersare more relevant to the mechanical properties manifested
1036 E. OOSTVEEN ET AL.dur<strong>in</strong>g spontaneous breath<strong>in</strong>g than those estimated withhigher-frequency <strong>oscillation</strong>s. Although the requirement ofapnoea limits the applicability of the low-frequency FOT,there are special conditions where its advantages can beexploited. First of all, measurements dur<strong>in</strong>g suspension ofmechanical ventilation <strong>in</strong> anaesthetised and paralysed subjectsfor short <strong>in</strong>tervals of <strong>oscillation</strong> [143, 146] allow themonitor<strong>in</strong>g of the airway and tissue mechanics far morespecifically than that offered by commercial respiratorymonitors [135].Another target population of the low-frequency FOT is<strong>in</strong>fants, whose lack of cooperation permits lung functiontest<strong>in</strong>g only <strong>in</strong> the sedated state. Here, activation of the end<strong>in</strong>spiratoryHer<strong>in</strong>g-Breuer reflex can be used to evoke theapnoea needed for low-frequency FOT measurements [149].<strong>The</strong> post-hyperventilation apnoea permits oscillatory measurementsat lower transrespiratory pressures [150]. Furtherstudies with this <strong>technique</strong> <strong>in</strong>cluded the establishment ofnormal values of the mechanical parameters for this agegroup [151], the evaluation of bronchodilator [152] andbronchoconstrictor provocation tests [153], addressed thealterations <strong>in</strong> the mechanical properties <strong>in</strong> wheeze [154] andthe contribution of the nasal pathways to Zrs [155].A special version of the low-frequency FOT uses an optimalventilatory waveform (OVW) to drive the respiratorysystem, the comb<strong>in</strong>ation of mechanical ventilation andimpedance estimation [144]. <strong>The</strong> OVW has been used <strong>in</strong>studies on the pulmonary and chest wall mechanics <strong>in</strong> normalsubjects before and after bronchoconstriction [156], thebroncholytic responses <strong>in</strong> asthmatics [157] and the <strong>in</strong>spiratoryimpedance <strong>in</strong> flow-limited patients [158].<strong>The</strong> technical requirements imposed by the application ofFOT dur<strong>in</strong>g CMV or CPAP, which were addressed brieflyabove, perta<strong>in</strong> to all applications of the low-frequency FOT.Most importantly, any leak around the airway open<strong>in</strong>gshould be elim<strong>in</strong>ated; a shunt that may not affect Zrs atthe medium frequency range would substantially distort thelow-frequency values.laboratories and, therefore, the technical experience ga<strong>in</strong>edand the amount of data obta<strong>in</strong>ed are still limited.ConclusionsOverall, the cl<strong>in</strong>ical diagnostic capacity of respiratoryimpedance measurement by <strong>forced</strong> <strong>oscillation</strong> <strong>technique</strong> iscomparable to that of spirometry. With respect to the latter,the ma<strong>in</strong> weakness of respiratory impedance determ<strong>in</strong>ation isthat it does not enable the dist<strong>in</strong>ction between obstructive andrestrictive lung disorders. <strong>The</strong> ma<strong>in</strong> advantages of the <strong>forced</strong><strong>oscillation</strong> <strong>technique</strong> are that m<strong>in</strong>imal cooperation of thepatient and no respiratory manoeuvres are needed; therefore,the measurement of respiratory impedance should be consideredwhenever spirometry cannot be performed or appearsto be unreliable. <strong>The</strong>se qualities of the <strong>forced</strong> <strong>oscillation</strong><strong>technique</strong> make it an ideal tool to study airway patencydur<strong>in</strong>g sleep or to monitor the respiratory properties dur<strong>in</strong>gmechanical ventilation. Additionally, the small amplitude<strong>oscillation</strong>s do not <strong>in</strong>fluence the respiratory mechanicalproperties studied, and this is particularly important whenassess<strong>in</strong>g bronchoactive responses. <strong>The</strong> high time resolutionthat can be obta<strong>in</strong>ed when a s<strong>in</strong>gle frequency is used makes<strong>forced</strong> <strong>oscillation</strong> <strong>technique</strong> the method of choice to studyvariations <strong>in</strong> mechanical properties with<strong>in</strong> the respiratorycycle or temporal changes, such as those <strong>in</strong>duced by a deep<strong>in</strong>halation.Chair and coord<strong>in</strong>ator of the committee: E. Oostveen(University Hospital Antwerp, Belgium).Appendix A: Glossary of symbols and abbreviations forimpedance measurementsHigh-frequency <strong>oscillation</strong>sSimilarly to the <strong>in</strong>clusion of low-frequency components, theelevation of <strong>oscillation</strong> frequencies above y100 Hz revealsnew patterns of frequency dependence of Zrs, with the potentialof estimat<strong>in</strong>g additional mechanical parameters [159–163].In particular, at frequencies well above fres, Xrs crosses zero <strong>in</strong>the negative direction: this is called the first antiresonantfrequency (far,1). Healthy subjects and patients with airwayobstruction have been differentiated on the basis of both fresand far,1, and the <strong>forced</strong> spirometry <strong>in</strong>dices have been shownto correlate better with far,1 than with the medium-frequency<strong>oscillation</strong> parameters [163]. <strong>The</strong> high-frequency Zrs is dom<strong>in</strong>atedby wave propagation processes <strong>in</strong> the airway tree andmuch less affected by tissue properties. Although the modelbasedanalysis of these phenomena rema<strong>in</strong>s far from complete[159], current work suggests that far,1 carries <strong>in</strong>formationabout airway wall compliance, which may be an importantdescriptor <strong>in</strong> the understand<strong>in</strong>g of airway <strong>in</strong>stability occurr<strong>in</strong>g<strong>in</strong> wheez<strong>in</strong>g disorders <strong>in</strong> <strong>in</strong>fancy [162].Although the low-frequency and high-frequency <strong>oscillation</strong>sreveal different mechanical characteristics of the respiratorysystem and, hence, require different modell<strong>in</strong>g approaches,comb<strong>in</strong>ed studies <strong>in</strong>volv<strong>in</strong>g both <strong>oscillation</strong> ranges <strong>in</strong> the samesubjects would certa<strong>in</strong>ly be useful, particularly <strong>in</strong> facilitat<strong>in</strong>gthe <strong>in</strong>terpretation of the medium-frequency Zrs data.F<strong>in</strong>ally, it should be noted that these new applicationsof FOT have been developed at research level by fewAbbreviation Description UnitaoAirway open<strong>in</strong>gawAirwaybsBody surfaceesOesophagealf Frequency Hzfres Resonant frequency HzFRC Function residual capacity LG Conductance (1/R) L?kPa -1 ?s -1Gaw Airway conductance (1/Raw) L?kPa -1 ?s -1Grs Total respiratory conductance (1/Rrs) L?kPa -1 ?s -1sGaw Specific airway conductancekPa -1 ?s -1(=Gaw/FRC)<strong>in</strong>InputLPulmonary systemP Pressure kPaR Real part of Z or resistance kPa?s?L -1rsRespiratory systemRawAirway resistance measured by kPa?s?L -1body plethysmographysRaw Specific airway resistance (1/sGaw) kPa?sRrsfTotal respiratory resistancemeasured at frequency ftiTissuetrTransferV9 Airflow L?s -1wChest wallX Imag<strong>in</strong>ary part of Z or reactance kPa?s?L -1Z Impedance kPa?s?L -1
CLINICAL APPLICATION OF FOT1037Acknowledgements. Dur<strong>in</strong>g the Task Forceactivities, A-M. Lor<strong>in</strong>o passed away. <strong>The</strong> membersof this Task Force are <strong>in</strong>debted to A-M.Lor<strong>in</strong>o, who besides be<strong>in</strong>g a warm personality andpersonal friend, was also a highly respectedcolleague who made a major contribution <strong>in</strong> thefield of basic research on the <strong>forced</strong> <strong>oscillation</strong><strong>technique</strong> and its development <strong>in</strong> cl<strong>in</strong>ical applications.References1. van de Woestijne KP, Desager KN, Duiverman EJ, MarchalF. Recommendations for measurement of respiratory <strong>in</strong>putimpedance by means of the <strong>forced</strong> <strong>oscillation</strong> method. EurRespir Rev 1994; 4: 235–237.2. DuBois AB, Brody AW, Lewis DH, Burgess BF. Oscillationmechanics of lungs and chest <strong>in</strong> man. J Appl Physiol 1956; 8:587–594.3. Pesl<strong>in</strong> R, Fredberg JJ. Oscillation mechanics of therespiratory system. In: Macklem PT, Mead J, eds. Handbookof Physiology. <strong>The</strong> Respiratory System. Mechanics ofBreath<strong>in</strong>g. Bethesda, MD, American Physiological Society,1986; pp. 145–178.4. Pride NB. Forced <strong>oscillation</strong> <strong>technique</strong>s for measur<strong>in</strong>gmechanical properties of the respiratory system. Thorax1992; 47: 317–320.5. Marchal F, Loos N. Respiratory <strong>oscillation</strong> mechanics <strong>in</strong><strong>in</strong>fant and preschool children. Eur Respir Mon 1997; 5: 58–87.6. Navajas D, Farré R. Forced <strong>oscillation</strong> <strong>technique</strong>: fromtheory to cl<strong>in</strong>ical applications. Monaldi Arch Chest Dis 2001;56: 555–562.7. MacLeod D, Birch M. Respiratory <strong>in</strong>put impedancemeasurement: <strong>forced</strong> <strong>oscillation</strong> methods. Med Biol EngComput 2001; 39: 505–516.8. Pesl<strong>in</strong> R, Duvivier C, Didelon J, Gall<strong>in</strong>a C. Respiratoryimpedance measured with head generator to m<strong>in</strong>imize upperairway shunt. J Appl Physiol 1985; 59: 1790–1795.9. van de Woestijne KP, Franken H, Cauberghs M, LàndsérFJ, Clément J. A modification of the <strong>forced</strong> <strong>oscillation</strong><strong>technique</strong>. In: Hutàs I, Debreczeni LA, eds. Respiration.Budapest, Adv Physiol Sci, 1981; pp. 655–660.10. Pesl<strong>in</strong> R, Jard<strong>in</strong> P, Duvivier C, Beg<strong>in</strong> P. In-phase requirementsfor measur<strong>in</strong>g respiratory <strong>in</strong>put impedance. J AppliedPhysiol 1984; 56: 804–809.11. Hell<strong>in</strong>ckx J, Cauberghs M, De Boeck K, Demedts M.Evaluation of impulse <strong>oscillation</strong> system: comparison with<strong>forced</strong> <strong>oscillation</strong> <strong>technique</strong> and body plethysmography.Eur Respir J 2001; 18: 564–570.12. Rotger M, Pesl<strong>in</strong> R, Farré R, Duvivier C. Influence ofamplitude, phase and frequency content of pseudorandompressure <strong>in</strong>put on impedance data and their variability.Eur Respir Rev 1991; 1: 178–182.13. Daróczy B, Hantos Z. Generation of optimum pseudorandomsignals for respiratory impedance measurements. IntJ Biomed Comput 1990; 25: 21–31.14. Farré R, Rotger M, Navajas D. Optimized estimation ofrespiratory impedance by signal averag<strong>in</strong>g <strong>in</strong> the timedoma<strong>in</strong>. J Appl Physiol 1992; 73: 1181–1189.15. Navajas D, Farré R, Rotger M, Pesl<strong>in</strong> R. A new estimate tom<strong>in</strong>imize the error due to breath<strong>in</strong>g <strong>in</strong> the measurements ofrespiratory impedance. IEEE Trans Biomed Eng 1988; 35:1001–1005.16. Daróczy B, Hantos Z. An improved <strong>forced</strong> oscillatoryestimation of respiratory impedance. Int J Biomed Comput1982; 1982: 221–225.17. Lor<strong>in</strong>o H, Mariette C, Karouia M, Lor<strong>in</strong>o AM. Influence ofsignal process<strong>in</strong>g on estimation of respiratory impedance.J Appl Physiol 1993; 74: 215–223.18. Michaelson ED, Grassman ED, Peters WR. Pulmonarymechanics by spectral analysis of <strong>forced</strong> random noise. J Cl<strong>in</strong>Invest 1975; 56: 1210–1230.19. Cauberghs M, Van de Woestijne KP. Effect of upper airwayshunt and series properties on respiratory impedancemeasurements. J Appl Physiol 1989; 66: 2274–2279.20. Pesl<strong>in</strong> R, Duvivier C, Gall<strong>in</strong>a C, Cervantes P. Upper airwayartefact <strong>in</strong> respiratory impedance measurements. Am RevRespir Dis 1985; 132: 712–714.21. Marchal F, Haouzi P, Pesl<strong>in</strong> R, Duvivier C, Gall<strong>in</strong>a C.Mechanical properties of the upper airway wall <strong>in</strong> childrenand their <strong>in</strong>fluence on respiratory impedance measurements.Pediatr Pulmonol 1992; 13: 28–33.22. Pesl<strong>in</strong> R, Duvivier C, Jard<strong>in</strong> P. Upper airway wallsimpedance measured with head plethysmograph. J ApplPhysiol 1984; 57: 596–600.23. Marchal F, Mazurek H, Habib M, Duvivier C, Derelle J,Pesl<strong>in</strong> R. Input respiratory impedance to estimate airwayhyperreactivity <strong>in</strong> children: standard method versus headgenerator. Eur Respir J 1994; 7: 601–607.24. Govaerts E, Cauberghs M, Demedts M, Van de WoestijneKP. Head generator versus conventional <strong>technique</strong> <strong>in</strong>respiratory <strong>in</strong>put impedance measurements. Eur Respir Rev1994; 4: 143–149.25. Farré R, Rotger M, Marchal F, Pesl<strong>in</strong> R, Navajas D.Assessment of bronchial reactivity by <strong>forced</strong> <strong>oscillation</strong>admittance avoids the upper airway artefact. Eur Respir J1999; 13: 761–766.26. Pesl<strong>in</strong> R, Teculescu D, Locuty J, Gall<strong>in</strong>a C, Duvivier C.Normal values of the total respiratory <strong>in</strong>put impedance withthe head generator <strong>technique</strong>. Eur Resp Rev 1994; 4: 138–142.27. Mazurek HK, Marchal F, Derelle J, Hatahet R, Moneret-Vautr<strong>in</strong> D, Mon<strong>in</strong> P. Specificity and sensitivity of respiratoryimpedance <strong>in</strong> assess<strong>in</strong>g reversibility of airway obstruction <strong>in</strong>children. Chest 1995; 107: 996–1002.28. Làndsér FJ, Clément J, Van de Woestijne KP. Normal valuesof total respiratory resistance and reactance determ<strong>in</strong>ed by<strong>forced</strong> <strong>oscillation</strong>s: <strong>in</strong>fluence of smok<strong>in</strong>g. Chest 1982; 81:586–591.29. Clément J, Làndsér FJ, van de Woestijne KP. Totalresistance and reactance <strong>in</strong> patients with respiratory compla<strong>in</strong>tswith and without airways obstruction. Chest 1983; 83:215–220.30. Gimeno F, van der Weele LT, Koëter GH, van Altena R.Forced <strong>oscillation</strong> <strong>technique</strong>. Reference values for totalrespiratory resistance obta<strong>in</strong>ed with the Siemens SiregnostFD5. Ann Allergy 1992; 68: 155–158.31. Pasker HG, Mertens I, Clément J, Van de Woestijne KP.Normal values of total respiratory <strong>in</strong>put resistance andreactance for adult men and women. Eur Respir Rev 1994; 4:134–137.32. Pasker HG, Schepers R, Clément J, van de Woestijne KP.Total respiratory impedance measured by means of the<strong>forced</strong> <strong>oscillation</strong> <strong>technique</strong> <strong>in</strong> subjects with and withoutrespiratory compla<strong>in</strong>ts. Eur Respir J 1996; 9: 131–139.33. Zerah F, Lor<strong>in</strong>o AM, Lor<strong>in</strong>o H, Harf A, Macqu<strong>in</strong>-Mavier I.Forced <strong>oscillation</strong> <strong>technique</strong> vs spirometry to assess bronchodilatation<strong>in</strong> patients with asthma and COPD. Chest 1995;108: 41–47.34. Duiverman EJ, Clément J, van de Woestijne KP, Neijens HJ,van den Bergh ACM, Kerrebijn KF. Forced <strong>oscillation</strong><strong>technique</strong>. Reference values for resistance and reactance overa frequency spectrum of 2–26 Hz <strong>in</strong> healthy children aged2.3–12.5 years. Bull Eur Physiopathol Respir 1985; 21: 171–178.35. Cuijpers CE, Wessel<strong>in</strong>g G, Swaen GM, Wouters EF.Frequency dependence of oscillatory resistance <strong>in</strong> healthyprimary school children. Respiration 1993; 60: 149–154.36. Hantos Z, Daróczy B, Gyurkovits K. Total respiratoryimpedance <strong>in</strong> healthy children. Pediatr Pulmonol 1985; 1: 91–98.37. Cogswell JJ. Forced <strong>oscillation</strong> <strong>technique</strong> for determ<strong>in</strong>ationof resistance to breath<strong>in</strong>g <strong>in</strong> children. Arch Dis Child 1973;48: 259–266.
1038 E. OOSTVEEN ET AL.38. Hordvik NL, König P, Morris DA, Kreutz C, Pimmel RL.Normal values for <strong>forced</strong> oscillatory respiratory resistance <strong>in</strong>children. Pediatr Pulmonol 1985; 1: 145–148.39. Lebecque P, Desmond K, Swartebroeckx Y, Dubois P,Lull<strong>in</strong>g J, Coates A. Measurement of respiratory systemresistance by <strong>forced</strong> <strong>oscillation</strong> <strong>in</strong> normal children: acomparison with spirometric values. Pediatr Pulmonol1991; 10: 117–122.40. Solymar L, Aronsson PH, Bake B, Bjure J. Respiratoryresistance and impedance magnitude <strong>in</strong> healthy children aged2–18 years. Pediatr Pulmonol 1985; 1: 134–140.41. Stanescu D, Moavero NE, Veriter C, Brasseur L. Frequencydependence of respiratory resistance <strong>in</strong> healthy children.J Appl Physiol 1979; 47: 268–272.42. Williams SP, Fullton JM, Tsai MJ, Pimmel RL, Collier AM.Respiratory impedance and derived parameters <strong>in</strong> youngchildren by <strong>forced</strong> random noise. J Appl Physiol 1979; 47:169–174.43. Mansell A, Levison H, Kruger K, Tripp TL. Measurementof respiratory resistance <strong>in</strong> children by <strong>forced</strong> <strong>oscillation</strong>s.Am Rev Respir Dis 1972; 106: 710–714.44. Hell<strong>in</strong>ckx J, De Boeck K, Bande-Knops J, van der Poel M,Demedts M. Bronchodilator response <strong>in</strong> 3–6.5 years oldhealthy and stable asthmatic children. Eur Respir J 1998; 12:438–443.45. Ducharme FM, Davis GM, Ducharme GR. Pediatricreference values for respiratory resistance measured by<strong>forced</strong> <strong>oscillation</strong>. Chest 1998; 113: 1322–1328.46. Mazurek H, Willim G, Marchal F, Haluszka J, Tomalak W.Input respiratory impedance measured by head generator <strong>in</strong>preschool children. Pediatr Pulmonol 2000; 30: 47–55.47. Willim G, Mazurek H, Kurzawa R, et al. Reference values oflung function measurements <strong>in</strong> polish children and adolescents.Part 1: respiratory resistance and reactance measuredby <strong>forced</strong> <strong>oscillation</strong> <strong>technique</strong> (FOT). J Int Rev Allergol Cl<strong>in</strong>Immunol 2000; 6: 70–78.48. Neild JE, Twort CH, Ch<strong>in</strong>n S, et al. <strong>The</strong> repeatability andvalidity of respiratory resistance measured by the <strong>forced</strong><strong>oscillation</strong> <strong>technique</strong>. Respir Med 1989; 83: 111–118.49. van den Elshout FJ, van de Woestijne KP, Folger<strong>in</strong>g HT.Variations of respiratory impedance with lung volume <strong>in</strong>bronchial hyperreactivity. Chest 1990; 98: 358–364.50. Snashall PD, Parker S, Phil M, Ten Haave P, Simmons D,Noble MIM. Use of an impedance meter for measur<strong>in</strong>gairways responsiveness to histam<strong>in</strong>e. Chest 1991; 99: 1183–1185.51. Gimeno F, van der Weele LT, Koëter GH, de Monchy JGR,van Altena R. Variability of <strong>forced</strong> <strong>oscillation</strong> (SiemensSiregnost FD 5) measurements of total respiratory resistance<strong>in</strong> patients and healthy subjects. Ann Allergy 1993; 71: 56–60.52. van Noord JA, Smeets J, Clément J, van de Woestijne KP,Demedts M. Assessment of reversibility of airflow obstruction.Am J Respir Crit Care Med 1994; 150: 551–554.53. Solymar L, Aronsson PH, Engstrom I, Bake B, Bjure J.Forced <strong>oscillation</strong> <strong>technique</strong> and maximum expiratory flows<strong>in</strong> bronchial provocation tests <strong>in</strong> children. Eur J Respir Dis1984; 65: 486–495.54. Timonen KL, Randell JT, Salonen RO, Pekkanen J. Shorttermvariations <strong>in</strong> oscillatory and spirometric lung function<strong>in</strong>dices among school children. Eur Respir J 1997; 10: 82–87.55. Buhr W, Jorres R, Berdel D, Landser FJ. Correspondencebetween <strong>forced</strong> <strong>oscillation</strong> and body plethysmographydur<strong>in</strong>g bronchoprovocation with carbachol <strong>in</strong> children.Pediatr Pulmonol 1990; 8: 280–288.56. Lenney W, Milner AD. At what age do bronchodilator drugswork? Arch Dis Child 1978; 53: 532–735.57. Delacourt C, Lor<strong>in</strong>o H, Herve-Guillot M, Re<strong>in</strong>ert P, Harf A,Housset B. Use of the <strong>forced</strong> <strong>oscillation</strong> <strong>technique</strong> to assessairway obstruction and reversibility <strong>in</strong> children. Am J RespirCrit Care Med 2000; 161: 730–736.58. Tomalak W, Elbousefi A, Kurzawa R, Doniec Z. Diurnalvariations of respiratory system resistance and compliancederived from <strong>in</strong>put impedance <strong>in</strong> asthmatic children. RespirPhysiol 2000; 123: 101–108.59. van Noord JA, Clément J, van de Woestijne KP, Demedts M.Total respiratory resistance and reactance <strong>in</strong> patients withasthma, chronic bronchitis, and emphysema. Am Rev RespirDis 1991; 143: 922–927.60. Govaerts E, Demedts M, Van de Woestijne KP. Totalrespiratory impedance and early emphysema. Eur Respir J1993; 6: 1181–1185.61. Wessel<strong>in</strong>g GJ, Wouters EF. Analysis of respiratory impedancecharacteristics <strong>in</strong> chronic bronchitis. Respiration 1992;59: 81–88.62. van Noord JA, Cauberghs M, van de Woestijne KP,Demedts M. Total respiratory resistance and reactance <strong>in</strong>ankylos<strong>in</strong>g spondylitis and kyphoscoliosis. Eur Respir J1991; 4: 945–951.63. Horan T, Mateus S, Beraldo P, et al. Forced <strong>oscillation</strong><strong>technique</strong> to evaluate tracheostenosis <strong>in</strong> patients withneurological <strong>in</strong>jury. Chest 2001; 120: 69–73.64. van Noord JA, Clément J, Cauberghs M, Mertens I, van deWoestijne KP, Demedts M. Total respiratory resistance andreactance <strong>in</strong> patients with diffuse <strong>in</strong>terstitial lung disease. EurRespir J 1989; 2: 846–852.65. Zerah F, Harf A, Perlemuter L, Lor<strong>in</strong>o H, Lor<strong>in</strong>o AM,Atlan G. Effects of obesity on respiratory resistance. Chest1993; 103: 1470–1476.66. Lebecque P, Stanescu D. Respiratory resistance by the<strong>forced</strong> <strong>oscillation</strong> <strong>technique</strong> <strong>in</strong> asthmatic children and cysticfibrosis patients. Eur Respir J 1997; 10: 891–895.67. Holmgren D, Engstrom I, Bjure J, Sixt R, Aberg N.Respiratory resistance and transcutaneous PO2 dur<strong>in</strong>ghistam<strong>in</strong>e provocation <strong>in</strong> children with bronchial asthma.Pediatr Pulmonol 1993; 15: 168–174.68. Ducharme FM, Davis GM. Measurement of respiratoryresistance <strong>in</strong> the emergency department: feasibility <strong>in</strong> youngchildren with acute asthma. Chest 1997; 111: 1519–1525.69. Chalut DS, Ducharme FM, Davis GM. <strong>The</strong> preschoolrespiratory assessment measure (PRAM): a responsive <strong>in</strong>dexof acute asthma severity. J Pediatr 2000; 137: 762–768.70. Solymar L, Aronsson PH, Sixt R. <strong>The</strong> <strong>forced</strong> <strong>oscillation</strong><strong>technique</strong> <strong>in</strong> children with respiratory disease. PediatrPulmonol 1985; 1: 256–261.71. Hell<strong>in</strong>ckx J, De Boeck K, Demedts M. No paradoxicalbronchodilator response with <strong>forced</strong> <strong>oscillation</strong> <strong>technique</strong> <strong>in</strong>children with cystic fibrosis. Chest 1998; 113: 55–59.72. Duiverman EJ, Den Boer JA, Roorda RJ, RooyackersCMHM, Valstar M, Kerrebijn KF. Lung function andbronchial responsiveness measured by <strong>forced</strong> oscillometryafter bronchopulmonary dysplasia. Arch Dis Child 1988; 63:727–732.73. Malmberg LP, Mieskonen S, Pelkonen A, Kari A, SovijärviARA, Turpe<strong>in</strong>en M. Lung function measured by theoscillometric method <strong>in</strong> prematurely born children withchronic lung disease. Eur Respir J 2000; 16: 598–603.74. Carvalhaes-Neto N, Lor<strong>in</strong>o H, Gall<strong>in</strong>ari C, et al. Cognitivefunction and assessment of lung function <strong>in</strong> the elderly.AmJRespir Crit Care Med 1995; 152: 1611–1615.75. Coe CI, Watson A, Joyce H, Pride NB. Effects of smok<strong>in</strong>gon changes <strong>in</strong> respiratory resistance with <strong>in</strong>creas<strong>in</strong>g age. Cl<strong>in</strong>Sci (Colch) 1989; 76: 487–494.76. Brochard L, Pelle G, de Palmas J, et al. Density andfrequency dependence of resistance <strong>in</strong> early airway obstruction.Am Rev Respir Dis 1987; 135: 579–584.77. Pesl<strong>in</strong> R, Pham QT, Teculescu D, Gall<strong>in</strong>a C, Duvivier C.Comparative value of respiratory <strong>in</strong>put and transfer impedances<strong>in</strong> field studies. Bull Eur Physiopathol Respir 1987; 23:37–42.78. Pham QT, Bourgkard E, Chau N, et al. Forced <strong>oscillation</strong><strong>technique</strong> (FOT): a new tool for epidemiology of occupationallung diseases? Eur Respir J 1995; 8: 1307–1313.79. Iwatsubo Y, Lor<strong>in</strong>o H, Hubert C, et al. Measurement ofrespiratory impedance by <strong>forced</strong> <strong>oscillation</strong>: comparison of
CLINICAL APPLICATION OF FOT1039the standard and head generator methods. Eur Respir J 1994;7: 901–906.80. Pasker HG, Peeters M, Genet P, Clément J, Nemery B, vande Woestijne KP. Short-term ventilatory effects <strong>in</strong> workersexposed to fumes conta<strong>in</strong><strong>in</strong>g z<strong>in</strong>coxide: comparison of <strong>forced</strong><strong>oscillation</strong> <strong>technique</strong> with spirometry. Eur Respir J 1997; 10:1523–1529.81. Pairon JC, Iwatsubo Y, Hubert C, et al. Measurement ofbronchial responsiveness by <strong>forced</strong> <strong>oscillation</strong> <strong>technique</strong> <strong>in</strong>occupational epidemiology. Eur Respir J 1994; 7: 484–489.82. Bohadana AB, Pesl<strong>in</strong> R, Megherbi SE, et al. Dose-responseslope of <strong>forced</strong> <strong>oscillation</strong> and <strong>forced</strong> expiratory parameters<strong>in</strong> bronchial challenge test<strong>in</strong>g. Eur Respir J 1999; 13: 295–300.83. Santoli F, Zerah F, Vasile N, Bachir D, Galacteros F,Atlan G. Pulmonary function <strong>in</strong> sickle cell disease with orwithout acute chest syndrome. Eur Respir J 1998; 12: 1124–1129.84. Làndsér FJ, Nagels J, van de Woestijne KP. Implementationby means of microprocessor <strong>technique</strong>s for the measurementof total respiratory impedance dur<strong>in</strong>g spontaneous breath<strong>in</strong>g.Prog Resp Res 1979; 11: 135–143.85. Wouters EF, Verschoof AC, Polko AH, Visser BF.Impedance measurements of the respiratory system beforeand after salbutamol <strong>in</strong> COPD patients. Respir Med 1989;83: 309–313.86. Ducharme FM, Davis GM. Respiratory resistance <strong>in</strong> theemergency department: a reproducible and responsivemeasure of asthma severity. Chest 1998; 113: 1566–1572.87. Wanner A, Zarzecki S, Marks MB. Cont<strong>in</strong>uous measurementof respiratory resistance <strong>in</strong> asthmatic children. Respiration1977; 34: 61–68.88. Menon P, Hilman BC, Menon V, Bairnsfather L. Assessmentof response to oral metaproterenol sulfate by <strong>forced</strong><strong>oscillation</strong> <strong>in</strong> young children. Ann Allergy 1988; 60: 547–551.89. Konig P, Gayer D, Kantak A, Kreutz C, Douglass B,Hordvik NL. A trial of metaproterenol by metered-dose<strong>in</strong>haler and two spacers <strong>in</strong> preschool asthmatics. PediatrPulmonol 1988; 5: 247–251.90. Grogg<strong>in</strong>s RC, Milner AD, Stokes GM. Bronchodilatoreffects of clemast<strong>in</strong>e, ipratropium, bromide, and salbutamol<strong>in</strong> preschool children with asthma. Arch Dis Child 1981; 56:342–344.91. Nussbaum E, Eyzaguirre M, Galant SP. Dose-responserelationship of <strong>in</strong>haled metaproterenol sulfate <strong>in</strong> preschoolchildren with mild asthma. Pediatrics 1990; 85: 1072–1075.92. Pauwels JH, Desager KN, Creten WL, Van der Veken J, VanBever HP. Study of the bronchodilat<strong>in</strong>g effect of three dosesof nebulized oxitropium bromide <strong>in</strong> asthmatic preschoolchildren us<strong>in</strong>g the <strong>forced</strong> <strong>oscillation</strong> <strong>technique</strong>. Eur J Pediatr1997; 156: 329–332.93. Crapo RO, Casaburi R, Coates AL, et al. Guidel<strong>in</strong>es formethachol<strong>in</strong>e and exercise challenge test<strong>in</strong>g-1999. Thisofficial statement of the American Thoracic Society wasadopted by the ATS Board of Directors, July 1999. AmJ Respir Crit Care Med 2000; 161: 309–329.94. Sterk PJ, Fabbri LM, Quanjer PH, et al. Airway responsiveness.Standardized challenge test<strong>in</strong>g with pharmacological,physical and sensitiz<strong>in</strong>g stimuli <strong>in</strong> adults. Eur Respir J1993; 6: Suppl. 16, 53–83.95. Wessel<strong>in</strong>g GJ, Vanderhoven-August<strong>in</strong> IM, Wouters EF.Forced <strong>oscillation</strong> <strong>technique</strong> and spirometry <strong>in</strong> cold airprovocation tests. Thorax 1993; 48: 254–259.96. Tamura G, Mue S, Ishihara T, Takishima T. <strong>The</strong> s<strong>in</strong>gleexposure method for <strong>in</strong>halation challenge with allergen.J Allergy Cl<strong>in</strong> Immunol 1985; 75(1 Pt 1): 47–54.97. Weers<strong>in</strong>k EJ, vd Elshout FJ, van Herwaarden CV, Folger<strong>in</strong>g H.Bronchial responsiveness to histam<strong>in</strong>e and methachol<strong>in</strong>emeasured with <strong>forced</strong> expirations and with the <strong>forced</strong><strong>oscillation</strong> <strong>technique</strong>. Respir Med 1995; 89: 351–356.98. van Noord JA, Clément J, van de Woestijne KP, Demedts M.Total respiratory resistance and reactance as a measurementof response to bronchial challenge with histam<strong>in</strong>e. Am RevRespir Dis 1989; 139: 921–926.99. Schmekel B, Smith HJ. <strong>The</strong> diagnostic capacity of <strong>forced</strong><strong>oscillation</strong> and <strong>forced</strong> expiration <strong>technique</strong>s <strong>in</strong> identify<strong>in</strong>gasthma by isocapnic hyperpnoea of cold air. Eur Respir J1997; 10: 2243–2249.100. Ch<strong>in</strong>et T, Pelle G, Macqu<strong>in</strong>-Mavier I, Lor<strong>in</strong>o H, Harf A.Comparison of the dose-response curves obta<strong>in</strong>ed by <strong>forced</strong><strong>oscillation</strong> and plethysmography dur<strong>in</strong>g carbachol <strong>in</strong>halation.Eur Respir J 1988; 1: 600–605.101. Penn<strong>in</strong>gs HJ, Wouters EF. Effect of <strong>in</strong>haled beclomethasonedipropionate on isocapnic hyperventilation with cold air <strong>in</strong>asthmatics, measured with <strong>forced</strong> <strong>oscillation</strong> <strong>technique</strong>. EurRespir J 1997; 10: 665–671.102. Manço JC, Hyatt RE, Rodarte JR. Respiratory impedance<strong>in</strong> normal humans: effects of bronchodilatation and bronchoconstriction.Mayo Cl<strong>in</strong> Proc 1987; 62: 487–497.103. Sekizawa K, Yanai M, Shimizu Y, Sasaki H, Takishima T.Serial distribution of bronchoconstriction <strong>in</strong> normal subjects.Methachol<strong>in</strong>e versus histam<strong>in</strong>e. Am Rev Respir Dis 1988;137: 1312–1316.104. Sekizawa K, Sasaki H, Shimizu Y, Takishima T. Doseresponseeffects of methachol<strong>in</strong>e <strong>in</strong> normal and <strong>in</strong> asthmaticsubjects. Relationship between the site of airway responseand overall airway hyperresponsiveness. Am Rev Respir Dis1986; 133: 593–599.105. Wang YT, Coe CI, Pride NB. Effect on histam<strong>in</strong>e responsivenessof reduc<strong>in</strong>g airway dimensions by alter<strong>in</strong>g posture.Thorax 1990; 45: 530–535.106. Saito H, Nishimura M, Sh<strong>in</strong>ano H, Sato F, Miyamoto K,Kawakami Y. Effect of mild hypoxia on airway responsivenessto methachol<strong>in</strong>e <strong>in</strong> subjects with airway hyperresponsiveness.Chest 1999; 116: 1653–1658.107. Fujimori K, Satoh M, Arakawa M. Ventilatory response tocont<strong>in</strong>uous <strong>in</strong>cremental changes <strong>in</strong> respiratory resistance <strong>in</strong>patients with mild asthma. Chest 1996; 109: 1525–1531.108. Duiverman EJ, Neijens HJ, Van der Snee-van Smaalen M,Kerrebijn KF. Comparison of <strong>forced</strong> oscillometry and <strong>forced</strong>expirations for measur<strong>in</strong>g dose-related responses to <strong>in</strong>haledmethachol<strong>in</strong>e <strong>in</strong> asthmatic children. Bull Eur PhysiopatholRespir 1986; 22: 433–436.109. Lebecque P, Spier S, Lapierre JG, Lamarre A, Z<strong>in</strong>man R,Coates AL. Histam<strong>in</strong>e challenge test <strong>in</strong> children us<strong>in</strong>g <strong>forced</strong><strong>oscillation</strong> to measure total respiratory resistance. Chest1987; 92: 313–318.110. Duiverman EJ, Neijens HJ, van Strik R, van der Snee-vanSmaalen M, Kerrebijn KF. Bronchial responsiveness <strong>in</strong>asthmatic children aged 3 to 8 years measured by <strong>forced</strong>pseudo-random noise oscillometry. Bull Eur PhysiopatholRespir 1986; 22: 27–33.111. Wilson NM, Bridge P, Phagoo SB, Silverman M. <strong>The</strong> measurementof methachol<strong>in</strong>e responsiveness <strong>in</strong> 5 year old children:three methods compared. Eur Respir J 1995; 8: 364–370.112. Klug B, Bisgaard H. Measurement of lung function <strong>in</strong> awake2–4-year-old asthmatic children dur<strong>in</strong>g methachol<strong>in</strong>e challengeand acute asthma: a comparison of the impulse<strong>oscillation</strong> <strong>technique</strong>, the <strong>in</strong>terrupter <strong>technique</strong>, and transcutaneousmeasurement of oxygen versus whole-body plethysmography.Pediatr Pulmonol 1996; 21: 290–300.113. Bisgaard H, Klug B. Lung function measurement <strong>in</strong> awakeyoung children. Eur Respir J 1995; 8: 2067–2075.114. Bouaziz N, Beyaert C, Gauthier R, Mon<strong>in</strong> P, Pesl<strong>in</strong> R,Marchal F. Respiratory system reactance as an <strong>in</strong>dicator ofthe <strong>in</strong>trathoracic airway response to methachol<strong>in</strong>e <strong>in</strong>children. Pediatr Pulmonol 1996; 22: 7–13.115. Gaultier C, Fletcher ME, Beardsmore C, England S,Motoyama E. Respiratory function measurements <strong>in</strong> <strong>in</strong>fants:measurement conditions. Eur Respir J 1995; 8: 1057–1066.116. Desager KN, Marchal F, Van de Woestijne KP. Forced<strong>oscillation</strong> <strong>technique</strong>. In: Stocks J, Sly PD, Tepper RS,Morgan WJ, eds. Infant respiratory function test<strong>in</strong>g. NewYork, Wiley-Liss, 1996; pp. 355–378.
1040 E. OOSTVEEN ET AL.117. Farré R, Navajas D, Pesl<strong>in</strong> R, Rotger M, Duvivier C. Acorrection procedure for the asymmetry of differentialpressure transducers <strong>in</strong> respiratory impedance measurements.IEEE Trans Biomed Eng 1989; 36: 1137–1140.118. Desager KN, Buhr W, Willemen M, et al. Measurement oftotal respiratory impedance <strong>in</strong> <strong>in</strong>fants by the <strong>forced</strong><strong>oscillation</strong> <strong>technique</strong>. J Appl Physiol 1991; 71: 770–776.119. Desager KN, Cauberghs M, Van de Woestijne KP. Twopo<strong>in</strong>tcalibration procedure of the <strong>forced</strong> <strong>oscillation</strong> <strong>technique</strong>.Med Biol Eng Comput 1997; 35: 752–756.120. Marchal F, Pesl<strong>in</strong> R, Duvivier C, Gall<strong>in</strong>a C, Crance JP.Mechanics of the ventilatory system <strong>in</strong> sedated <strong>in</strong>fants:Forced <strong>oscillation</strong>s versus s<strong>in</strong>glebreath method. PediatrPulmonol 1988; 5: 19–26.121. Marchal F, Pesl<strong>in</strong> R, Duvivier C, Gall<strong>in</strong>a C, Crance JP.Measurement of ventilatory mechanical impedance <strong>in</strong> <strong>in</strong>fantsus<strong>in</strong>g a head pressure generator. Pediatr Pulmonol 1989; 7:209–216.122. Desager KN, Cauberghs M, Naudts J, van de Woestijne KP.Influence of upper airway shunt on total respiratoryimpedance <strong>in</strong> <strong>in</strong>fants. J Appl Physiol 1999; 87: 902–909.123. Desager KN, Willemen M, Van Bever HP, De Backer W,Vermeire PA. Evaluation of nasal impedance us<strong>in</strong>g the<strong>forced</strong> <strong>oscillation</strong> <strong>technique</strong> <strong>in</strong> <strong>in</strong>fants. Pediatr Pulmonol1991; 11: 1–7.124. Dork<strong>in</strong> HL, Stark AR, Werthammer JW, Strieder DJ,Fredberg JJ, Frantz IDR. Respiratory system impedancefrom 4 to 40 Hz <strong>in</strong> paralyzed <strong>in</strong>tubated <strong>in</strong>fants withrespiratory disease. J Cl<strong>in</strong> Invest 1983; 72: 903–910.125. Gauthier R, Beyaert C, Feillet F, Mon<strong>in</strong> P, Marchal F.Respiratory <strong>oscillation</strong> mechanics <strong>in</strong> <strong>in</strong>fants with bronchiolitisdur<strong>in</strong>g mechanical ventilation. Pediatr Pulmonol 1998;25: 18–31.126. Mart<strong>in</strong>ez FD, Morgan WJ, Wright AL, Holberg CJ, TaussigLM. Dim<strong>in</strong>ished lung function as a predispos<strong>in</strong>g factor forwheez<strong>in</strong>g respiratory illness <strong>in</strong> <strong>in</strong>fants. New Engl J Med 1988;319: 1112–1117.127. Desager KN, Van Bever HP, Willemen M, De Backer W,Vermeire PA. Functional residual capacity and totalrespiratory system impedance <strong>in</strong> wheez<strong>in</strong>g <strong>in</strong>fants. PediatrPulmonol 1994; 17: 354–358.128. Soto ME, Sly PD, Uren E, Taussig LM, Landau LI.Bronchodilator response dur<strong>in</strong>g acute viral bronchiolitis <strong>in</strong><strong>in</strong>fancy. Pediatr Pulmonol 1985; 2: 85–90.129. van Bever HP, Desager KN, Pauwels JH, Wojciechowski M,Vermeire PA. Aerosolised furosemide <strong>in</strong> wheezy <strong>in</strong>fants: anegative report. Pediatr Pulmonol 1995; 20: 16–20.130. Pesl<strong>in</strong> R, Felicio da Silva J, Duvivier C, Chabot F.Respiratory mechanics studied by <strong>forced</strong> <strong>oscillation</strong>s dur<strong>in</strong>gartificial ventilation. Eur Respir J 1993; 6: 772–784.131. Lanteri CJ, Kano S, Duncan AW, Sly PD. Changes <strong>in</strong>respiratory mechanics <strong>in</strong> children undergo<strong>in</strong>g cardiopulmonarybypass. Am J Respir Crit Care Med 1995; 152:1893–1900.132. Farré R, Ferrer M, Rotger M, Torres A, Navajas D.Respiratory mechanics <strong>in</strong> ventilated COPD patients: <strong>forced</strong><strong>oscillation</strong> versus occlusion <strong>technique</strong>s. Eur Respir J 1998; 12:170–176.133. Farré R, Manc<strong>in</strong>i M, Rotger M, Ferrer M, Roca J, NavajasD. Oscillatory resístance measured dur<strong>in</strong>g non<strong>in</strong>vasiveproportional assist ventilation. Am J Respir Crit Care Med2001; 164: 790–794.134. Beydon L, Malass<strong>in</strong>e P, Lor<strong>in</strong>o AM, et al. Respiratoryresistance by end-<strong>in</strong>spiratory occlusion and <strong>forced</strong> <strong>oscillation</strong>s<strong>in</strong> <strong>in</strong>tubated patients. J Appl Physiol 1996; 80: 1105–1111.135. Babik B, Peták F, Asztalos T, Deák ZI, Bogáts G, Hantos Z.Components of respiratory resistance monitored <strong>in</strong> mechanicallyventilated patients. Eur Respir J 2002; 20: 1538–1544.136. Badia JR, Farre R, Montserrat JM, et al. Forced <strong>oscillation</strong><strong>technique</strong> for the evaluation of severe sleep apnoea/hypopnoeasyndrome: a pilot study. Eur Respir J 1998; 11: 1128–1134.137. Lor<strong>in</strong>o AM, Lofaso F, Duizabo D, et al. Respiratoryresistive impedance as an <strong>in</strong>dex of airway obstruction dur<strong>in</strong>gnasal cont<strong>in</strong>uous positive airway pressure titration. AmJ Respir Crit Care Med 1998; 158: 1465–1470.138. Navajas D, Farré R, Rotger M, Badia R, Puig-de-MoralesM, Montserrat JM. Assessment of airflow obstructiondur<strong>in</strong>g CPAP by means of <strong>forced</strong> <strong>oscillation</strong> <strong>in</strong> patientswith sleep apnea. Am J Respir Crit Care Med 1998; 157:1526–1530.139. Randerath WJ, Parys K, Feldmeyer F, Sanner B, Ruhle KH.Self-adjust<strong>in</strong>g nasal cont<strong>in</strong>uous positive airway pressuretherapy based on measurement of impedance: A comparisonof two different maximum pressure levels. Chest 1999; 116:991–999.140. Montserrat JM, Badia JR, Farré R, Ballester E, HernandezL, Navajas D. Rout<strong>in</strong>e application of the <strong>forced</strong> <strong>oscillation</strong><strong>technique</strong> (FOT) for CPAP titration <strong>in</strong> the sleep apnea/hypopnea syndrome. Am J Respir Crit Care Med 1999; 160:1550–1554.141. Jensen A, Atileh H, Suki B, Ingenito EP, Lutchen KR.Airway caliber <strong>in</strong> healthy and asthmatic subjects: effects ofbronchial challenge and deep <strong>in</strong>spirations. J Appl Physiol2001; 91: 506–515.142. Schweitzer C, Moreau-Colson C, Marchal F. Respiratoryimpedance response to a deep <strong>in</strong>halation <strong>in</strong> asthmaticchildren with spontaneous airway obstruction. Eur Respir J2002; 19: 1020–1025.143. Farré R, Ferrer M, Rotger M, Navajas D. Servocontrolledgenerator to measure respiratory impedance from 0.25 to26 Hz <strong>in</strong> ventilated patients at different PEEP levels. EurRespir J 1995; 8: 1222–1227.144. Lutchen KR, Yang K, Kaczka DW, Suki B. Optimalventilation waveforms for estimat<strong>in</strong>g low-frequency respiratoryimpedance. J Appl Physiol 1993; 75: 478–488.145. Farré R, Rotger M, Montserrat JM, Navajas D. A system togenerate simultaneous <strong>forced</strong> <strong>oscillation</strong> and cont<strong>in</strong>uouspositive airway pressure. Eur Respir J 1997; 10: 1349–1353.146. Navajas D, Farré R, Canet J, Rotger M, Sanchis J.Respiratory <strong>in</strong>put impedance <strong>in</strong> anesthetized paralyzedpatients. J Appl Physiol 1990; 69: 1372–1379.147. Hantos Z, Daróczy B, Suki B, Galgóczy G, Csendes T.Forced oscillatory impedance of the respiratory system atlow frequencies. J Appl Physiol 1986; 60: 123–132.148. Hantos Z, Daróczy B, Suki B, Nagy S, Fredberg JJ. Inputimpedance and peripheral <strong>in</strong>homogeneity of dog lungs.J Appl Physiol 1992; 72: 168–178.149. Sly PD, Hayden MJ, Peták F, Hantos Z. Measurement oflow-frequency respiratory impedance <strong>in</strong> healthy <strong>in</strong>fants. AmJ Respir Crit Care Med 1996; 154: 161–166.150. Peták F, Hayden MJ, Hantos Z, Sly PD. Volume dependenceof respiratory impedance <strong>in</strong> <strong>in</strong>fants. Am J Respir CritCare Med 1997; 156: 1172–1177.151. Hall GL, Hantos Z, Peták F, et al. Airway and respiratorytissue mechanics <strong>in</strong> normal <strong>in</strong>fants. Am J Respir Crit CareMed 2000; 162: 1397–1402.152. Hayden MJ, Petak F, Hantos Z, Hall G, Sly PD. Us<strong>in</strong>glow-frequency <strong>oscillation</strong> to detect bronchodilator responsiveness<strong>in</strong> <strong>in</strong>fants. Am J Respir Crit Care Med 1998; 157:574–579.153. Hall GL, Hantos Z, Sly PD. Altered respiratory tissuemechanics <strong>in</strong> asymptomatic wheezy <strong>in</strong>fants. Am J Respir CritCare Med 2001; 164: 1387–1391.154. Hall GL, Hantos Z, Wildhaber JH, Peták F, Sly PD.Methachol<strong>in</strong>e responsiveness <strong>in</strong> <strong>in</strong>fants assessed with lowfrequency<strong>forced</strong> <strong>oscillation</strong> and <strong>forced</strong> expiration <strong>technique</strong>s.Thorax 2001; 56: 42–47.155. Hall GL, Hantos Z, Wildhaber JH, Sly PD. Contribution ofnasal pathways to low-frequency respiratory impedance <strong>in</strong><strong>in</strong>fants. Thorax 2002; 57: 396–399.156. Kaczka DW, Ingenito EP, Suki B, Lutchen KR. Partition<strong>in</strong>gairway and lung tissue resistances <strong>in</strong> humans: effects ofbronchoconstriction. J Appl Physiol 1997; 82: 1531–1541.157. Kaczka DW, Ingenito EP, Israel E, Lutchen KR. Airway
CLINICAL APPLICATION OF FOT1041and lung tissue mechanics <strong>in</strong> asthma. Effects of albuterol.Am J Respir Crit Care Med 1999; 159: 169–178.158. Kaczka DW, Ingenito EP, Lutchen KR. Technique todeterm<strong>in</strong>e <strong>in</strong>spiratory impedance dur<strong>in</strong>g mechanical ventilation:implications for flow limited patients. Ann Biomed Eng1999; 27: 340–355.159. Frey U, Suki B, Kraemer R, Jackson AC. Humanrespiratory <strong>in</strong>put impedance between 32 and 800 Hz,measured by <strong>in</strong>terrupter <strong>technique</strong> and <strong>forced</strong> <strong>oscillation</strong>s.J Appl Physiol 1997; 82: 1018–1023.160. Frey U, Silverman M, Kraemer R, Jackson AC. Highfrequencyrespiratory impedance measured by <strong>forced</strong>-<strong>oscillation</strong><strong>technique</strong> <strong>in</strong> <strong>in</strong>fants. Am J Respir Crit Care Med 1998; 158:363–370.161. Frey U, Jackson AC, Silverman M. Differences <strong>in</strong> airwaywall compliance as a possible mechanism for wheez<strong>in</strong>gdisorders <strong>in</strong> <strong>in</strong>fants. Eur Respir J 1998; 12: 136–142.162. Frey U, Silverman M, Kraemer R, Jackson AC. Highfrequency <strong>in</strong>put impedance <strong>in</strong> <strong>in</strong>fants assessed with the highspeed <strong>in</strong>terrupter <strong>technique</strong>. Eur Respir J 1998; 12: 148–158.163. Chalker RB, Celli BR, Habib RH, Jackson AC. Respiratory<strong>in</strong>put impedance from 4 to 256 Hz <strong>in</strong> normals and chronicairflow obstruction: comparisons and correlations withspirometry. Am Rev Respir Dis 1992; 146: 570–576.