Prescribed Drugs Provider Manual - Iowa Department of Human ...
Prescribed Drugs Provider Manual - Iowa Department of Human ...
Prescribed Drugs Provider Manual - Iowa Department of Human ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Prescribed</strong> <strong>Drugs</strong><strong>Provider</strong> <strong>Manual</strong>
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Page1DateSeptember 1, 2011TABLE OF CONTENTSChapter I. General Program PoliciesChapter II. Member EligibilityChapter III. <strong>Provider</strong>-Specific PoliciesAppendix
III. <strong>Provider</strong>-Specific Policies
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Page1DateAugust 1, 2013TABLE OF CONTENTSPageCHAPTER III. PROVIDER-SPECIFIC POLICIES .................................................. 1A. GENERAL PHARMACY GUIDELINES ............................................................... 11. Definitions ......................................................................................... 12. Entities Involved in Developing Medicaid Drug Policies ............................. 5a. Drug Utilization Review Commission ............................................... 5b. Pharmaceutical and Therapeutics Committee ................................... 63. Pharmacies Eligible to Participate .......................................................... 7a. Licensure .................................................................................... 7b. Survey Participation ..................................................................... 74. Pharmacist Responsibilities................................................................... 8a. Prospective Drug Utilization Review ................................................ 8b. Dispensing Requirements .............................................................. 8c. Patient Counseling ....................................................................... 8d. Reason for Denial ........................................................................ 95. Drug Use Review ............................................................................... 10B. COVERAGE OF SERVICES ........................................................................... 111. Prescription Requirements ................................................................... 11a. Prescriber Qualifications .............................................................. 11b. Prescriber Guidelines ................................................................... 122. <strong>Drugs</strong> Excluded From Coverage ........................................................... 123. <strong>Drugs</strong> for Medicare Eligibles ................................................................ 134. Preferred or Recommended <strong>Drugs</strong> ........................................................ 135. Nonpreferred <strong>Drugs</strong> ........................................................................... 146. Newly Released <strong>Drugs</strong> ........................................................................ 14a. New Drug Entities ....................................................................... 14b. Exceptions to the Nonpreferred Default Policy for New PDL <strong>Drugs</strong> ...... 15c. Existing PDL <strong>Drugs</strong> With Supplemental Rebates .............................. 157. Nonprescription <strong>Drugs</strong> ........................................................................ 168. Medical Supplies ................................................................................ 18C. PRIOR AUTHORIZATION REQUIREMENTS ..................................................... 181. Completing a Prior Authorization Request .............................................. 212. Submitting a Prior Authorization Request .............................................. 233. Prior Authorization Response ............................................................... 244. ADD/ADHD/Narcolepsy Agents............................................................. 255. Alpha 2 Agonists, Extended-Release ....................................................... 26
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Page2DateAugust 1, 2013Page6. Alpha 1 Proteinase Inhibitor Enzymes ..................................................... 267. Amylino Mimetic (Symlin ® ) ................................................................. 278. Angiotensin Receptor Blocker (ARB) ..................................................... 279. Anti-Acne Products ............................................................................. 2810. Antiemetic-5HT3 Receptor Antagonists/Substance P Neurokinin Products ... 2811. Antifungal Therapy ............................................................................. 3012. Antihistamines .................................................................................. 3013. Anti-Thrombotics ............................................................................... 3114. Becaplermin (Regranex ® ) ................................................................... 3115. Benzodiazepines ................................................................................ 3216. Biologicals for Ankylosing Spondylitis .................................................... 3217. Biologicals for Arthritis ........................................................................ 3318. Biologicals for Inflammatory Bowel Disease ........................................... 3419. Biologicals for Plaque Psoriasis ............................................................. 3520. Buprenorphine (Butrans) Transdermal System .................................... 3521. Buprenorphine/Naloxone (Suboxone ® ).................................................. 3522. Chronic Pain Syndrome Agents ............................................................ 3723. Colchicine (Colcrys ® ).......................................................................... 3824. Concurrent IM/PO Antipsychotic Use ..................................................... 3825. Crizotinib (Xalkori ® ) ........................................................................... 3926. Dalfampridine (Ampyra)................................................................... 3927. Dextromethorphan and Quinidine (Nuedexta)...................................... 3928. Digestive Enzymes ............................................................................. 4029. Dipeptidyl Peptidase-4 (DPP-4) Inhibitors .............................................. 4030. Dornase Alfa (Pulmozyme ® ) ................................................................ 4131. Eplerenone (Inspra ® ) ......................................................................... 4132. Erythropoiesis Stimulating Agents ........................................................ 4133. Extended-Release Formulations ........................................................... 4234. Febuxostat (Uloric ® )........................................................................... 4235. Fentanyl, Short-Acting Oral Products .................................................... 4236. Fingolimod (Gilenya) ....................................................................... 4337. Granulocyte Colony Stimulating Factor Agents ....................................... 4338. Growth Hormones .............................................................................. 4439. Hepatitis C Protease Inhibitors-Oral (Incivek and Victrelis ) ................... 4540. Immunomodulators – Topical .............................................................. 4641. Incretin Mimetic (Byetta ® and Victoza ® ) ................................................ 4642. Insulin Pens, Pre-filled ........................................................................ 4743. Isotretinoin (Oral).............................................................................. 4744. Ivacaftor (Kalydeco )......................................................................... 4845. Ketorolac Tromethamine (Toradol ® ) ..................................................... 4846. Lidocaine Patch (Lidoderm ® ) ............................................................... 49
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Page3DateAugust 1, 2013Page47. Linezolid (Zyvox ® ) ............................................................................. 4948. Mifepristone (Korlym ® )....................................................................... 5049. Modified Formulations ........................................................................ 5050. Muscle Relaxants ............................................................................... 5151. Narcotic Agonist-Antagonist Nasal Sprays .............................................. 5152. Nebivolol (Bystolic ® ) .......................................................................... 5253. Nicotine Replacement Products ............................................................ 5254. Nonparenteral Vasopressin Derivatives <strong>of</strong> Posterior Pituitary HormoneProducts ........................................................................................... 5355. Nonpreferred <strong>Drugs</strong> ........................................................................... 5456. Nonsteroidal Anti-Inflammatory <strong>Drugs</strong> .................................................. 5457. Omalizumab (Xolair ® ) ........................................................................ 5558. Oxycodone ER/CR (OxyContin ® ) .......................................................... 5659. Palivizumab (Synagis ® ) ...................................................................... 5660. Proton Pump Inhibitors ....................................................................... 5861. Pulmonary Arterial Hypertension Agents ................................................ 5962. Quantity Limit Override ...................................................................... 60a. Initial 15-Day Limit ..................................................................... 60b. Monthly Limits ............................................................................ 6063. R<strong>of</strong>lumilast (Daliresp) ...................................................................... 8164. Sedative/Hypnotics-Non-Benzodiazepine ............................................... 8265. Selected Brand-Name <strong>Drugs</strong> ................................................................ 8266. Serotonin 5-HT1 Receptor Agonists ...................................................... 8367. Short-Acting Narcotics ........................................................................ 8468. Smoking Cessation Therapy-Oral ......................................................... 8469. Sodium Oxybate (Xyrem ® ).................................................................. 8570. Thrombopoietin Receptor Agonists ....................................................... 8571. Topical Retinoids ............................................................................... 8672. Vemurafenib (Zelboraf).................................................................... 8773. Vilazodone (Viibryd ) ......................................................................... 8774. Vitamins, Minerals and Multiple Vitamins ............................................... 8875. Vusion Ointment ............................................................................. 88D. BASIS OF PAYMENT FOR DRUGS AND SUPPLIES ............................................ 891. Reimbursement Effective February 1, 2013 ........................................... 90a. Generic and Nonprescription <strong>Drugs</strong> ............................................... 90b. Brand-Name <strong>Drugs</strong> ..................................................................... 902. <strong>Drugs</strong> Subject to Federal Upper Limit (FUL) ........................................... 90a. FUL Development ....................................................................... 90b. Reimbursement for FUL <strong>Drugs</strong> ...................................................... 913. Reimbursement for Unit-Dose Packaging ............................................... 914. Reimbursement for Vaccinations .......................................................... 92
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Page4DateAugust 1, 2013PageE. BILLING SYSTEM ...................................................................................... 941. Point <strong>of</strong> Sale Claim Submission ............................................................ 94a. Claims Rejected Due to Other Insurance Coverage .......................... 95b. Correction <strong>of</strong> Insurance Information .............................................. 962. Claiming Payment for Retroactively Eligible Member ............................... 963. Claim Attachment Control, Form 470-3969 ............................................ 974. Paper Claim Submission ...................................................................... 97F. EDITS AND SPECIAL BILLING INFORMATION .............................................. 1051. Claims for Deceased Members ........................................................... 1052. Common Billing Errors ...................................................................... 1053. Compounded Prescriptions ................................................................ 1074. Coverage <strong>of</strong> Non-Drug Products ......................................................... 1075. Date <strong>of</strong> Birth Verification ................................................................... 1096. Override Codes ................................................................................ 1107. Proper Reporting <strong>of</strong> NDCs ................................................................. 1108. Prospective Drug Utilization Review (Pro-DUR)..................................... 111a. Age Edits ................................................................................. 113b. Cost Effectiveness Edit .............................................................. 115c. Dosage Form Edits .................................................................... 116d. Excessive Days Supply .............................................................. 116e. High-Dollar Claims .................................................................... 116f. Refill Too Soon ......................................................................... 117g. Step Therapy Edits.................................................................... 117h. Tablet Splitting ......................................................................... 117i. Therapeutic Duplication ............................................................. 1189. Status Change for Preferred Brand Name <strong>Drugs</strong> ................................... 11810. Travel or Vacation Supplies <strong>of</strong> Medication ............................................ 11811. 340B Drug Pricing Program ............................................................... 119a. Covered Entity (CE) .................................................................. 119b. <strong>Iowa</strong> Medicaid Billing/Reimbursement for CE Outpatient In-HousePharmacy or Contracted Pharmacy .............................................. 12012. Interpreter Services ......................................................................... 120a. Documentation <strong>of</strong> the Service ..................................................... 121b. Qualifications ........................................................................... 121G. REMITTANCE ADVICE AND FIELD DESCRIPTIONS ........................................ 1221. Remittance Advice Explanation .......................................................... 1222. Remittance Advice Field Descriptions .................................................. 123
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage1DateAugust 1, 2013CHAPTER III. PROVIDER-SPECIFIC POLICIESA. GENERAL PHARMACY GUIDELINESThis manual gives general information about Medicaid drug coverage and billingpolicies. For more detailed information, see the following web sites:www.iadur.orgwww.ime.state.ia.uswww.iowamedicaidpdl.comwww.mslciowa.comwww.iowamedicaidpos.comDrug Utilization Review (DUR) Commission<strong>Iowa</strong> Medicaid Enterprise (IME)Pharmaceutical and Therapuetics (P&T) Committeeand Preferred Drug List (PDL)Pharmacy ReimbursementPoint <strong>of</strong> Sale (POS) system for pharmacy claims1. Definitions340B Program means the federal 340B Drug Pricing program managed byHealth Resources and Services Administration (HRSA) Office <strong>of</strong> PharmacyAffairs (OPA). The program allows certain designated facilities to purchaseprescription medications at discounts, so these facilities can <strong>of</strong>fer somemedications to their patients at reduced prices.340B Actual acquisition cost (340B AAC) means the net cost <strong>of</strong> a drugpaid by a pharmacy for drugs purchased through the 340B drug pricingprogram. A drug’s 340B AAC includes discounts, rebates, chargebacks andother adjustments to the price <strong>of</strong> the drug, but excludes dispensing fees.Averge actual acquisition cost (average AAC) means the average pricesthat retail pharmacies paid to acquire drug products.Compendium <strong>of</strong> drug information means one <strong>of</strong> the following:♦ The American Hospital Formulary Service Drug Information (AHFS);♦ The United States Pharmacopeia Drug Information (USP-DI); or♦ DRUGDEX Information System.Contract pharmacy means a pharmacy under contract with a covered entitythat lacks its own pharmacy whereby the contract pharmacy is authorized todispense 340B-discounted drugs on behalf <strong>of</strong> the covered entity.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage2DateAugust 1, 2013Covered entity means a provider that meets eligibility criteria forparticipating in the 340B Program as set forth in Section 340B(a)(4) <strong>of</strong> thePublic Health Service Act.DESI drugs means drug products identified by the federal Food and DrugAdministration, in the Drug Efficacy Study Implementation Program, aslacking substantial evidence <strong>of</strong> effectiveness.Drug rebates means payments provided by pharmaceutical manufacturersto state Medicaid programs under the terms <strong>of</strong> the manufacturers’agreements with the <strong>Department</strong> <strong>of</strong> Health and <strong>Human</strong> Services or with theindividual state.Drug utilization review (DUR) means a quality review <strong>of</strong> coveredoutpatient drugs that assures that prescriptions are appropriate, medicallynecessary, and not likely to result in adverse medical outcomes.Drug Utilization Review Commission means a quality assurance body <strong>of</strong>nine members that seeks to improve the quality <strong>of</strong> pharmacy services andensure rational, cost-effective medication therapy for Medicaid members in<strong>Iowa</strong>. The web site for the Commission is www.iadur.org.Equivalent products means those products that meet therapeuticequivalence standards as published in the federal Food and DrugAdministration document, Approved Prescription Drug Products withTherapeutic Equivalence Evaluations.Federal upper limit (FUL) means the maximum allowable reimbursementset by the Centers for Medicare and Medicaid Services for a multiple-sourcedrug. The list is available at the federal pharmacy reimbursement web site:http://www.cms.hhs.gov/Reimbursement/Grandfather clause means a clause creating an exemption based onpreviously existing circumstances. The Pharmaceutical and TherapeuticsCommittee considered select therapeutic classes for grandfathering existingdrug regimens. For claims processing, “drug history” means the most recent90-day period. If a patient has a history with a specific drug within theseclasses, the prescriber is not required to obtain prior authorization even if thedrug has a nonpreferred status on the Preferred Drug List.Legend drugs are drugs that bear the federal caution: “Federal LawProhibits Dispensing a Drug Without a Prescription.”
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage3DateAugust 1, 2013Less than effective drug or DESI drug means a drug for which:♦ The Food and Drug Administration (FDA) has withdrawn approval <strong>of</strong> thedrug application for safety or efficacy reasons as a result <strong>of</strong> the drugefficacy study implementation (DESI) review; or♦ The secretary <strong>of</strong> the U.S. <strong>Department</strong> <strong>of</strong> Health and <strong>Human</strong> Services hasissued a notice <strong>of</strong> a hearing under section 505(e) <strong>of</strong> the federal Food,Drug, and Cosmetic Act on a proposed order to withdraw approval <strong>of</strong> thedrug application because the secretary has determined that the drug isless than effective for some or all <strong>of</strong> the conditions <strong>of</strong> use prescribed,recommended, or suggested in the drug’s labeling.♦ Medicaid Carve-Out is a billing mechanism available to covered entitiesthat implements the 340B requirement protecting manufacturers fromgiving a 340B discount and paying a Medicaid rebate on the same drug.If a covered entity implements the carve-out option, the covered entityonly purchases through the 340B Program drugs dispensed to non-Medicaid patients. <strong>Drugs</strong> dispensed to Medicaid patients are purchasedoutside the 340B Program.Medically accepted indication means any use for a covered outpatientdrug which is approved under the federal Food, Drug, and Cosmetic Act, orthe use <strong>of</strong> which is supported by one or more citations included or approvedfor inclusion in any <strong>of</strong> the compendia described in section 1927(g)(1)(B)(i) <strong>of</strong>the Social Security Act.National drug code (NDC) means the eleven-digit number themanufacturer or labeler assigns to a pharmaceutical product and attaches tothe product container at the time <strong>of</strong> packaging that identifies the product’smanufacturer, dose form and strength, and package size.Nonpreferred drug means a drug on the Preferred Drug List that requiresprior authorization, with the primary criteria being failure on the preferredagents rather than clinical guidelines. A nonpreferred drug is designated “N”on the Preferred Drug List.Nonprescription drugs or over-the-counter (OTC) drugs means drugsthat may be lawfully sold without a prescription.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage4DateAugust 1, 2013Nonrecommended drug means a drug placed on a voluntary list (designedto inform prescribers <strong>of</strong> cost-effective alternatives) that does not require aprior authorization but if used will be more costly to the Medicaid program. Anonrecommended drug is designated “NR” on the recommended drug list.Pharmaceutical and Therapeutics (P&T) Committee means a committee<strong>of</strong> nine members appointed by the Governor that is charged with developingand providing ongoing review <strong>of</strong> the Preferred Drug List pursuant to <strong>Iowa</strong>Code section 249A.20A.Preferred drug means a drug on the Preferred Drug List that providesmedical equivalency to the Medicaid member in a cost-effective manner (byvirtue <strong>of</strong> OBRA ’90 and Supplemental Rebate) and does not require a priorauthorization. A preferred drug is designated “P” on the Preferred Drug List.Preferred Drug List (PDL) means a list comprised <strong>of</strong> drugs recommendedto the <strong>Iowa</strong> <strong>Department</strong> <strong>of</strong> <strong>Human</strong> Services by the <strong>Iowa</strong> MedicaidPharmaceutical and Therapeutics Committee that have been identified asbeing therapeutically equivalent within a drug class and that provide costbenefit to the Medicaid program.Preferred drug with conditions means a drug has “preferred” agents butbefore getting the drug a patient must meet medical criteria and guidelinesthat coincide with current prior authorization guidelines. A preferred drugwith conditions is designated “P” on the Preferred Drug List and has a numberin the comments column to indicate a prior authorization is required, asdefined on the first page <strong>of</strong> the Preferred Drug List (PDL).Prior authorization (PA) means obtaining approval for a drug before thedrug is provided to a member, as a precondition for provider reimbursement.Prior authorization is requested at the prescriber level and is a prescriber faxonlysystem using the forms provided by the <strong>Iowa</strong> Medicaid Enterprise.Pr<strong>of</strong>essional dispensing fee means payment provided for the costsincurred by a pharmacy to dispense a drug. The fee reflects the pharmacist’spr<strong>of</strong>essional services and costs associated with ensuring that possession <strong>of</strong>the appropriate covered outpatient drug is transferred to a Medicaid member.Prospective drug utilization review (Pro-DUR) means a process in whicha request for a drug product for a particular patient is screened for potentialdrug therapy problems before the product is dispensed.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage5DateAugust 1, 2013Recommended drug means a drug placed on a voluntary list designed toinform prescribers <strong>of</strong> cost-effective alternatives that does not require a priorauthorization and if used will result in a cost savings to the Medicaidprogram. A recommended drug is designated “R” on the Preferred Drug List.Recommended drug list (RDL) means a voluntary list <strong>of</strong> drugsrecommended to the <strong>Department</strong> <strong>of</strong> <strong>Human</strong> Services by the <strong>Iowa</strong> MedicaidPharmaceutical and Therapeutics Committee that informs prescribers <strong>of</strong> costeffectivealternatives that do not require a prior authorization.Retrospective drug utilization review (Retro-DUR) means the process inwhich patient drug utilization is periodically reviewed to identify patterns <strong>of</strong>fraud, abuse, gross overuse, or inappropriate or unnecessary care.Usual and customary charge means the fee that the provider typicallycharges the general public for the product or service.Wholesale Acquisition Cost (WAC) represents the cost reported to Medi-Span by a manufacturer (updated in a number <strong>of</strong> ways) at which wholesalerspurchase drug products from that manufacturer.2. Entities Involved in Developing Medicaid Drug Policiesa. Drug Utilization Review CommissionThe <strong>Iowa</strong> Medicaid Drug Utilization Review (DUR) Commission,established pursuant to <strong>Iowa</strong> Code section 249A.24, is a qualityassurance body <strong>of</strong> nine members that seeks to improve the quality <strong>of</strong>pharmacy services and ensure rational, cost-effective medicationtherapy for Medicaid members in <strong>Iowa</strong>.This Commission meets six times a year in a public forum. TheCommission discusses potential medications or therapeutic classeswhere prior authorization may be beneficial, and discusses existingcriteria to determine if the criteria continue to be therapeutically valid.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage6DateAugust 1, 2013b. Pharmaceutical and Therapeutics CommitteeThe Pharmaceutical and Therapeutics (P&T) Committee was establishedpursuant to <strong>Iowa</strong> Code section 249A.20A. The P&T Committee has ninemembers appointed by the Governor for a two-year term. TheCommittee meets three times a year in a public forum.The P&T Committee is charged with developing and providing ongoingreview <strong>of</strong> the Preferred Drug List (PDL). The PDL is a list <strong>of</strong> drugs thathave been identified as being therapeutically equivalent within a drugclass and that provide cost benefit to the Medicaid program.The PDL was created in an effort to select medications for use by themembers <strong>of</strong> <strong>Iowa</strong> Medicaid that are both clinically sound and costeffective.The <strong>Department</strong> <strong>of</strong> <strong>Human</strong> Services is attempting to containMedicaid drug expenditures while ensuring that members’ access toeffective drug solutions are preserved.The P&T Committee’s focus is maximizing the initial utilization <strong>of</strong> themost cost-effective clinical choices available. All drug manufacturershave been given the opportunity to state the therapeutic benefit <strong>of</strong> theirdrugs and to reduce the net cost to the state through a supplementalrebate program. The Committee has:♦ Reviewed each product within a therapeutic class for:• Pharmacology,• Indications,• Comparative clinical trials, and• Adverse effects and safety.♦ Evaluated relative cost <strong>of</strong> each product.♦ Compared products within the same class to identify the mostclinically effective, cost efficient product in each class.By first considering the therapeutics and then the cost, the P&TCommittee ultimately decides which drugs to recommend to the <strong>Iowa</strong>Medicaid program as “preferred.”The P&T Committee holds public meetings, with public notice <strong>of</strong> itsagenda and opportunity for public comment. The web site for theCommittee is www.iowamedicaidpdl.com.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage7DateAugust 1, 20133. Pharmacies Eligible to ParticipateUnder the <strong>Iowa</strong> Medicaid program, drugs must be furnished by a licensedpharmacy. (The Board <strong>of</strong> Pharmacy Examiners issues these licenses.)a. LicensureParticipating retail pharmacies must be licensed in the state <strong>of</strong> <strong>Iowa</strong> orduly licensed in another state. Out-<strong>of</strong>-state retail pharmacies delivering,dispensing, or distributing drugs by any method to an ultimate userphysically located in <strong>Iowa</strong> must be duly licensed by <strong>Iowa</strong> as anonresident pharmacy for that purpose.b. Survey ParticipationAs a condition <strong>of</strong> participation, retail pharmacies are required to makeavailable drug acquisition cost invoice information, product availabilityinformation if known, dispensing cost information, and any otherinformation deemed necessary by the <strong>Department</strong> to assist inmonitoring and revising reimbursement rates pursuant to 441 IAC79.1(8) or for the efficient operation <strong>of</strong> the pharmacy benefit.♦ A pharmacy shall produce and submit all requested information inthe manner and format requested by the <strong>Department</strong> or its designeeat no cost to the <strong>Department</strong> or its designee.♦ A pharmacy shall submit information to the <strong>Department</strong> or itsdesignee within the time frame indicated following receipt <strong>of</strong> arequest for information unless the <strong>Department</strong> or its designee grantsan extension upon written request <strong>of</strong> the pharmacy.♦ Any dispensing or acquisition cost information submitted to the<strong>Department</strong> that specifically identifies a pharmacy’s individual costsshall be held confidential.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage9DateAugust 1, 2013♦ Proper storage♦ Prescription refill information, including the approximate date whenrefill will be allowed (generally, 90% <strong>of</strong> the prescription is used)♦ Actions to be taken in the event <strong>of</strong> a missed dose♦ Comments relevant to the patient’s drug therapy, including any otherinformation peculiar to the specific patient or drugPatient counseling is required in accordance with federal law at 42 USCSection 1396r(g)(2)(A)(ii)(l) and state rules at 657 <strong>Iowa</strong> AdministrativeCode 8.20(1)-(2).d. Reason for DenialThe pharmacist should explain the reason for any denial <strong>of</strong> a requesteddrug or item to the member or caregiver. For example, denial could bedue to one <strong>of</strong> the following:♦ Noncovered drug or item. Explain why the drug or item is notcovered and suggest alternatives to the member, caregiver, orpractitioner.♦ Prior authorization requirement. Explain the prior authorizationprocess and requirements to the member or caregiver.When a patient presents a prescription for nonpreferred drug at apharmacy and it is denied, contact the prescriber and ask if theprescriber wishes to choose a preferred drug.• If the prescriber wishes to change to a preferred drug, theprescriber may dictate the new prescription order.• If the prescriber views that the nonpreferred drug is medicallynecessary, the prescriber must obtain prior authorization.♦ Refill too soon. Inform the member or caregiver <strong>of</strong> an approximatedate the prescription can be refilled (after 90% <strong>of</strong> the previoussupply is used).In special circumstances, such as a change in dose, travel, or lost,stolen or destroyed medication, that result in an early refill, contactthe IME Pharmacy Point <strong>of</strong> Sale (POS) Unit at (515) 256-4608 (localcalls) or 877-463-7671 with the information. This information will bereviewed to determine if an override can be given to allow payment.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage10DateAugust 1, 2013♦ Plan limits exceeded. Refer to the limits list posted on the website, www.iowamedicaidpdl.com, under “Billing/Quantity Limits.” Thenumber <strong>of</strong> doses should be reduced to meet the quantity limit.If there are special circumstances where adherence to the quantitylimit is not possible, the prescriber should complete form 470-4556,Quantity Limit Override, or form 470-5038, Request for Fifteen DayInitial Prescription Supply Override, and fax it to 1-800-574-2515.The clinical staff will review the information submitted and determineif an override can be given to allow payment.If the member or caregiver is not satisfied with the explanation <strong>of</strong> thereason for a denial, refer the person to the member’s DHS worker forassistance in filing an appeal or requesting an exception to policy.Appeal and exception requests may be filed on line through thefollowing web site: http://www.dhs.state.ia.us/dhs/appeals/.5. Drug Use ReviewThe drug use review (DUR) process was established to fulfill a federalrequirement established by the federal Omnibus Budget Reconciliation Act <strong>of</strong>1990. <strong>Iowa</strong> Medicaid has implemented both <strong>of</strong> the required DUR types:♦ Prospective drug utilization review occurs when the pharmacist doesthe review <strong>of</strong> patient drug therapy at the point <strong>of</strong> sale. See PharmacistResponsibilities.♦ Retrospective drug utilization review occurs when the review takesplace after the point <strong>of</strong> sale.The retrospective DUR program provides ongoing periodic examination <strong>of</strong>claims data and other records in order to identify patterns <strong>of</strong> fraud, abuse,gross overuse, or inappropriate or medically unnecessary care amongphysicians, pharmacists, and members, or associated with specific drugs.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage11DateAugust 1, 2013B. COVERAGE OF SERVICESPayment will be made for legend and nonprescription drugs when prescribed by apractitioner who is legally qualified to prescribe the item, subject to the limitationsdescribed in this manual.1. Prescription RequirementsPrescription records are required for all drugs as specified in <strong>Iowa</strong> pharmacyand drug laws, including <strong>Iowa</strong> Code sections 124.308, 155A.27, and 155A.29.For Medicaid purposes, prescriptions are required for nonprescription drugsand are subject to the same provisions. This includes the record-keepingrequirements on refills. Maintain prescriptions on file in such a manner thatthey will be readily available for audit by the <strong>Department</strong>.Prescriptions executed in writing (nonelectronic) for prescription drugs mustbe presented on a tamper-resistant pad, as required by Section 1903(i)(23)<strong>of</strong> the Social Security Act (42 U.S.C. Section 1396b(i)(23)).a. Prescriber QualificationsPayment is made for drugs prescribed by a legally qualified practitioner(physician, dentist, podiatrist, therapeutically certified optometrist,physician assistant, or advanced registered nurse practitioner) withinthe limits prescribed by law and in policies established by the<strong>Department</strong>.Prescriptions by a therapeutically certified optometrist are limited to thefollowing:♦ Topical and oral antimicrobial agents♦ Topical and oral antihistamines♦ Topical and oral antiglaucoma agents♦ Topical and oral analgesic agents, including controlled substances♦ Topical anesthetic agents♦ Topical anti-inflammatory agents
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage12DateAugust 1, 2013b. Prescriber GuidelinesPrescribers should review the therapy <strong>of</strong> their Medicaid patients forutilization <strong>of</strong> nonpreferred drugs and wherever medically appropriate,change patients to preferred drugs. New therapy should be initiated ona preferred drug unless a nonpreferred drug is medically necessary.When a nonpreferred drug is medically necessary, the prescriber shouldrequest a prior authorization. See PRIOR AUTHORIZATIONREQUIREMENTS for information on criteria for prior authorization andprocedures.In writing prescriptions, the practitioner shall prescribe up to a 31-daysupply, unless therapeutically contraindicated. EXCEPTION: Oralcontraceptives may be prescribed in 90-day quantities.2. <strong>Drugs</strong> Excluded From CoverageMedicaid payment will not be made for:♦ <strong>Drugs</strong> used to cause anorexia, weight gain or weight loss.♦ <strong>Drugs</strong> used for cosmetic purposes or hair growth.♦ <strong>Drugs</strong> used for symptomatic relief <strong>of</strong> cough and colds, except fornonprescription drugs listed in section B.7.♦ <strong>Drugs</strong> used for fertility purposes or for male sexual enhancement.♦ <strong>Drugs</strong> prescribed for a use other than the drug’s medically accepted use.♦ <strong>Drugs</strong> classified as less than effective by the Centers for Medicare andMedicaid Services.♦ <strong>Drugs</strong> marketed by manufacturers that have not signed a Medicaid rebateagreement.♦ Covered outpatient drugs for which the manufacturer seeks to require asa condition <strong>of</strong> sale that associated tests or monitoring services bepurchased exclusively from the manufacturer or designee.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage13DateAugust 1, 20133. <strong>Drugs</strong> for Medicare EligiblesPrescription drugs for Medicaid members who also qualify for Medicare(referred to as “dual eligibles”) are paid through Medicare Part D effectiveJanuary 1, 2006. Medicaid does not cover any drugs covered under MedicarePart D for these members.<strong>Iowa</strong> Medicaid covers drugs in the following categories for dual eligiblemembers:♦ Barbiturates (except when used in the treatment <strong>of</strong> epilepsy, cancer, orchronic mental health disorder diagnoses)♦ Over-the-counter drugs (list posted at www.iowamedicaidpdl.com)♦ Prescription vitamin and minerals, except prenatal vitamins and fluoridepreparations<strong>Iowa</strong> Medicaid will accept only secondary claims for these drugs. Medicaidshould be listed as the secondary insurance for all dual eligibles. All claimsshould be submitted first to the primary insurance (Medicare Part D PDP).<strong>Iowa</strong> Medicaid will not pay for any Medicare Part B drugs, such as:♦ Oral immunosuppressant drugs,♦ Inhalation drugs when used with a nebulizer,♦ Oral chemotherapy drugs,♦ Oral anti-emetic drugs,♦ Blood clotting factors, or♦ Epoetin.A drug for which coverage is available to a dual eligible under Medicare Part Aor Part B must be billed to Medicare Part A or Part B.4. Preferred or Recommended <strong>Drugs</strong>Drug products designated on the Preferred Drug List as “P” (preferred) or “R”(recommended) do not require prior authorization unless the drug has anumber in the comments column to indicate a prior authorization is required,as defined on the first page <strong>of</strong> the Preferred Drug List. Seewww.iowamedicaidpdl.com for the current designations.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage14DateAugust 1, 2013A preferred drug with conditions has “preferred” agents but must meetcertain medical criteria and guidelines that coincide with current priorauthorization guidelines.5. Nonpreferred <strong>Drugs</strong>Drug products designated “N” (nonpreferred) on the Preferred Drug Listrequire prior authorization, with the primary criteria being failure on thepreferred agents rather than clinical guidelines. Seewww.iowamedicaidpdl.com for the current designations.Drug products within a therapeutic class that are not selected as preferredwill be denied for payment unless the prescriber obtains prior authorization.Payment for drugs requiring a prior authorization will be made only when:♦ The drugs are prescribed for treatment <strong>of</strong> one or more conditions set forthfor each, and♦ The <strong>Iowa</strong> Medicaid prior authorization criteria have been met, and♦ Approval is obtained through the prior authorization process.EXCEPTION: In the event <strong>of</strong> an emergency when the prescriber cannot submita prior authorization request, the pharmacist may dispense a 72-hour supply<strong>of</strong> the drug and reimbursement will be made.6. Newly Released <strong>Drugs</strong>a. New Drug EntitiesNew drug entities (including new generic drugs) and new drug productdosage forms <strong>of</strong> existing drug entities will be identified weekly andimmediately be coded as “Nonpreferred – Prior authorization required”until presented at the next quarterly scheduled P&T Committee meeting.These prior authorization restrictions will continue through the reviewprocess, including while committee recommendations are being made,and lasting until DHS makes a final determination.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage15DateAugust 1, 2013b. Exceptions to the Nonpreferred Default Policy for New PDL <strong>Drugs</strong>There are two major potential exceptions to the nonpreferred defaultpolicy for new PDL drugs:♦ If the FDA classifies a new medication as a priority drug, the statemay indicate that such a drug is preferred until the P&T Committeereviews the drug at its next scheduled meeting.♦ The state may decide to designate a new drug as “draft preferred”and provide immediate access and increased therapeutic choice tophysicians until the P&T Committee reviews the drug at its nextscheduled meeting if:• A new drug is therapeutically equivalent or superior to existingpreferred or nonpreferred choices, and• Is as safe or safer than existing preferred or nonpreferredchoices, and• The net cost, adjusted for all rebates, is less expensive than allexisting preferred choices.c. Existing PDL <strong>Drugs</strong> With Supplemental RebatesAlthough the state discourages supplemental rebate <strong>of</strong>fers on existingPDL drugs between annual bidding periods, it may entertain such bidsand may accept them if they:♦ Are determined to represent significant additional savings, or♦ Would replace a delinquent manufacturer’s product or a preferreddrug pulled from the marketplace or significantly restricted by theFDA.This interim preferred status will remain in effect until the P&TCommittee reviews the drug at its next scheduled meeting.Supplemental rebates will be invoiced only for approved drugs undercontract. Draft preferred drugs with supplemental rebates will not beinvoiced until approved by the Committee and accepted by the state. Atthat time, the supplemental rebates will be invoiced back to the effectivedate <strong>of</strong> the agreement, which is the date the drug began to benefit frompreferred status.
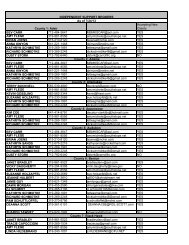
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage16DateAugust 1, 20137. Nonprescription <strong>Drugs</strong>Payment will be made for the following listed nonprescription drugs with aprescription, subject to prior authorization requirements as indicated belowand specified in the preferred drug list.Payment will be made in the same manner as for prescription drugs.Drug√ = PriorAuthorizationRequiredAcetaminophen tablets, 325 mgAcetaminophen tablets, 500 mgAcetaminophen elixir, 160 mg/5 mlAcetaminophen solution, 100 mg/mlAcetaminophen suppositories, 120 mgArtificial tears ophthalmic solutionArtificial tears ophthalmic ointmentAspirin, 81 mg (chewable)Aspirin, 81 mg (plain, enteric-coated)Aspirin tablets, 325 mgAspirin tablets, 650 mgAspirin tablets, enteric-coated, 325 mgAspirin tablets, enteric-coated, 650 mgAspirin tablets, buffered, 325 mgBacitracin ointment, 500 units/gmBenzoyl peroxide 5% gelBenzoyl peroxide 5% lotionBenzoyl peroxide 10% gelBenzoyl peroxide 10% lotionCetirizine 1 mg/ml liquidCetirizine 5 mg tabletsCetirizine 10 mg tabletsChlorpheniramine maleate tablets, 4 mgClotrimazole vaginal cream 1%Diphenhydramine hydrochloride capsules, 25 mgDiphenhydramine hydrochloride elixir, 12.5 mg/5 mlDiphenhydramine hydrochloride liquid, 12.5 mg/5 mlDiphenhydramine hydrochloride syrup, 12.5 mg/5 mlEpinephrine, racemic solution 2.25%Guaifenesin, 100 mg/5 ml with dextromethorphan liquid, 10 mg/5 ml
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage17DateAugust 1, 2013DrugIbupr<strong>of</strong>en suspension 100 mg/5 mlIbupr<strong>of</strong>en tablets, 200 mgLoperamide HCl liquid, 1 mg/5 mlLoperamide HCl tablets, 2 mgLoratadine tablets, 10 mgLoratadine syrup, 5 mg/5 mlMagnesium hydroxide suspension, 400 mg/5 mlMeclizine hydrochloride tablets, 12.5 mgMeclizine hydrochloride tablets, 25 mgMeclizine hydrochloride chewable tablets, 25 mgMiconazole nitrate cream, 2% topicalMiconazole nitrate cream, 2% vaginalMiconazole nitrate vaginal suppositories, 100 mgNeomycin-bacitracin-polymyxin ointmentNicoderm transdermal patch, 7 mg/24 hrNicotine transdermal patch, 7 mg/24 hrNicoderm transdermal patch, 14 mg/24 hrNicotine transdermal patch, 14 mg/24 hrNicoderm transdermal patch, 21 mg/24 hrNicotine transdermal patch, 21 mg/24 hrNicorette gum, 2 mgNicotine gum, 2 mgNicorette gum, 4 mgNicotine gum, 4 mgCommit lozenge, 2 mgNicotine polacrilex lozenge, 2 mgCommit lozenge, 4 mgNicotine polacrilex lozenge, 4 mgPermethrin lotion, 1%√ = PriorAuthorizationRequiredPolyethylene glycol 3350 powder 119 grams √ for ages 13-18Polyethylene glycol 3350 powder 238 grams √ for ages 13-18Polyethylene glycol 3350 powder 510 grams √ for ages 13-18Pseudoephedrine syrup, 30 mg/5 mlPseudoephedrine tablets, 30 mgPseudoephedrine tablets, 60 mgPyrethrins-piperonyl butoxide liquid, 0.33-4%Pyrethrins-piperonyl butoxide shampoo, 0.3-3%Pyrethrins-piperonyl butoxide shampoo, 0.33-4%Salicylic acid liquid 17%Sennosides-docusate sodium tablets, 8.6-50 mgSennosides syrup, 8.8 mg/5 mlSennosides tablets, 8.6 mg√√√√√√√√√√√√√√
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage18DateAugust 1, 2013Drug√ = PriorAuthorizationRequiredSenna tablets, 187 mgSodium chloride hypertonic ophthalmic ointment, 5%Sodium chloride hypertonic ophthalmic solution, 5%Tolnaftate 1% creamTolnaftate 1% powderTolnaftate 1% solutionNonprescription multiple vitamins and minerals may also be payable underconditions specified under PRIOR AUTHORIZATION REQUIREMENTS.Oral solid forms <strong>of</strong> these items shall be prescribed and dispensed in aminimum quantity <strong>of</strong> 100 units per prescription, except when dispensed via aunit-dose system.8. Medical SuppliesPharmacies that dispense medical equipment and supplies should follow theMEDICAL EQUIPMENT AND SUPPLY DEALER PROVIDER MANUAL and purchasea supply <strong>of</strong> CMS-1500 claim forms from any supplier.C. PRIOR AUTHORIZATION REQUIREMENTSPrior approval is required for the following:♦ ADD/ADHD/narcolepsy agents♦ Alpha 2 agonists, extended release♦ Alpha 1 -proteinase inhibitor enzymes♦ Amylino mimetic (Symlin ® )♦ Angiotensin receptor blockers♦ Anti-acne♦ Antiemetic-5HT3 receptor antagonists/substance P neurokinin products♦ Antifungal♦ Antihistamines♦ Anti-thrombotics (injectable)♦ Becaplermin (Regranex ® )♦ Benzodiazepines♦ Biologicals for ankylosing spondylitis♦ Biologicals for arthritis♦ Biologicals for inflammatory bowel disease♦ Biologicals for plaque psoriasis
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage19DateAugust 1, 2013♦ Buprenorphine (Butrans ) transdermal system♦ Buprenorphine/Naloxone (Suboxone ® )♦ Chronic pain syndrome agents♦ Colchicine (Colcrys ® )♦ Concurrent IM/PO antipsychotic use♦ Crizotinib (Xalkori ® )♦ Dalfampridine (Ampyra)♦ Dextromethorphan and Quinidine (Nuedexta)♦ Digestive enzymes♦ Dipeptidyl peptidase-4 (DPP-4) inhibitors♦ Dornase alfa (Pulmozyme ® )♦ Eplerenone (Inspra ® )♦ Erythropoiesis stimulating agents♦ Extended release formulations♦ Febuxostat (Uloric ® )♦ Fentanyl, short-acting oral products♦ Fingolimod (Gilenya)♦ Granulocyte colony stimulating factor agents♦ Growth hormones♦ Hepatitis C Protease Inhibitors-Oral♦ Immunomodulators, topical♦ Incretin mimetic♦ Insulin, pre-filled pens♦ Isotretinoin (oral)♦ Ivacaftor (Kalydeco)♦ Ketorolac tromethamine (Toradol ® )♦ Lidocaine patch (Lidoderm ® )♦ Linezolid (Zyvox ® )♦ Mifepristone (Korlym ® )♦ Modified formulations♦ Muscle relaxants♦ Narcotic agonist-antagonist nasal sprays♦ Nebivolol (Bystolic ® )♦ Nicotine replacement products♦ Nonparenteral vasopressin derivatives <strong>of</strong> posterior pituitary hormone products♦ Nonpreferred drugs♦ Nonsteroidal anti-inflammatory drugs♦ Omalizumab (Xolair ® )
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage20DateAugust 1, 2013♦ Oxycodone CR/ER (OxyContin ® )♦ Palivizumab (Synagis ® )♦ Proton pump inhibitors♦ Pulmonary arterial hypertension agents♦ Quantity limit override♦ R<strong>of</strong>lumilast (Daliresp)♦ Sedative/hypnotics-non-benzodiazepine♦ Selected brand name drugs♦ Serotonin 5-HT1 receptor agonists♦ Short-acting narcotics♦ Smoking cessation therapy (oral)♦ Sodium ozybate (Xyrem ® )♦ Thrombopoietin receptor agonists♦ Topical Retinoids for Acne♦ Vemurafenib (Zelboraf)♦ Vilazodone (Viibryd)♦ Vitamins, minerals and multiple vitamins♦ Vusion ointmentThe prescriber requests prior authorizations, not the pharmacy. The process is aprescriber fax-only system using the forms provided by the <strong>Iowa</strong> MedicaidEnterprise. The prescriber must request prior authorization by faxing thedesignated Request for Prior Authorization form to 800-574-2515.The specific criteria for approval <strong>of</strong> a prior authorization request are defined in thesubsections that follow. The prior authorization criteria are also available in chartformat on the web site www.iowamedicaidpdl.com.Requests require the information on the applicable Request for Prior Authorizationform, as noted in each subsection. Prior authorization forms may be obtained:♦ From the web site https://www.iowamedicaidpdl.com/pa_forms or♦ By calling the drug prior authorization help desk at (515) 256-4607 (local calls)or 877-776-1567. (Requests for prior authorizations will not be taken at thisnumber.)The IME Drug Prior Authorization Unit will consider other conditions as listed in thecompendia on an individual basis after reviewing documentation submittedregarding the medical necessity.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage21DateAugust 1, 20131. Completing a Prior Authorization RequestEach category <strong>of</strong> prior authorization uses a specific request form to reflect thecriteria for approval. The following instructions refer to items common to allRequests for Prior Authorization.IA MEDICAID MEMBER ID #: Copy this number directly from the member’sMedical Assistance Eligibility Card. This number must be eight positions inlength (seven numeric digits and one alphabetical character).PATIENT NAME: Provide the first and last name <strong>of</strong> the member. Use theMedical Assistance Eligibility Card for verification.DATE OF BIRTH (DOB): Copy the member’s date <strong>of</strong> birth directly from theMedical Assistance Eligibility Card. Use two digits for each: month, day, year(i.e., 04/11/67).PATIENT ADDRESS: Enter the member’s home address.PRESCRIBER NUMBER: Enter the national provider identifier (NPI) <strong>of</strong> theprescribing practitioner.PRESCRIBER NAME: Enter the name <strong>of</strong> the prescribing practitioner.PRESCRIBER PHONE NUMBEr: Enter the prescriber’s <strong>of</strong>fice phone number.PRESCRIBER ADDRESS: Enter the prescriber’s <strong>of</strong>fice address.PRESCRIBER FAX NUMBER: Enter the prescribing practitioner’s <strong>of</strong>fice FAXnumber.PHARMACY NAME: Enter the name <strong>of</strong> the pharmacy where the prescriptionwill be filled.PHARMACY ADDRESS: Enter the street address and city <strong>of</strong> the pharmacy.PHARMACY PHONE NUMBER: Enter the phone number <strong>of</strong> the pharmacy.PHARMACY NPI: Enter the pharmacy national provider identifier (NPI)number.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage22DateAugust 1, 2013NDC: If available, enter the National Drug Code <strong>of</strong> the product beingrequested.DRUG NAME: Provide the complete drug name <strong>of</strong> the product beingrequested.STRENGTH: Enter the strength <strong>of</strong> the drug being requested.DOSAGE INSTRUCTIONS: Enter the instructions for use for the requestedproduct.QUANTITY: Enter the quantity on the prescription (cannot exceed a onemonthsupply).DAYS SUPPLY: Enter the number <strong>of</strong> days’ supply requested (cannot exceed aone-month supply).LENGTH OF THERAPY ON PRESCRIPTION (DATE RANGE): Provide an estimate <strong>of</strong>the duration <strong>of</strong> therapy. The prior authorization period granted will besubject to adjustment by the reviewer according to established criteria andindividual consideration.DIAGNOSIS: Enter the patient’s diagnosis relevant to the requested product.PREVIOUS THERAPY: Enter drug names, strengths, dosage instructions, andexact date ranges <strong>of</strong> other medications that have previously been tried andfailed by patient.PERTINENT LAB DATA: Enter any laboratory 909 data that may affect theoutcome <strong>of</strong> this request.OTHER MEDICAL CONDITIONS TO CONSIDER: Enter any other medicalconditions the patient has that may help the Prior Authorization Unit make adecision.POSSIBLE DRUG INTERACTIONS/CONFLICTING DRUG THERAPIES: If the patientis taking any other medications that may negatively affect the requestedproduct, list them here.PRESCRIBER SIGNATURE: The prescriber must sign the form and the signaturemust match the prescriber name listed at the top <strong>of</strong> the request form.DATE OF SUBMISSION: Enter the date the prior authorization request wassubmitted.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage23DateAugust 1, 20132. Submitting a Prior Authorization RequestCompleted drug prior authorization requests must be submitted via FAX tothe IME Drug Prior Authorization Unit at 800-574-2515.Regular working hours for the provider help desk are Monday through Friday,8:00 a.m. to 5:00 p.m.After-hours calls for emergency requests and emergency requests on staterecognizedholidays are routed to the pharmacy pager voicemail system,where an on-call pharmacist is available for assistance.State-recognized holidays are as follows:♦ New Year’s Day♦ Martin Luther King Jr.’s birthday♦ Memorial Day♦ Independence Day♦ Labor Day♦ Veterans’ Day♦ Thanksgiving Day♦ The Friday following Thanksgiving♦ Christmas DayUnder the Health Insurance Portability and Accountability Act, there is anelectronic transaction for prior authorization requests (278 transaction).However, there is no standard to use in submitting additional documentationelectronically.Therefore, if you submit a prior authorization request electronically, you mustsubmit the additional documentation on paper using the following procedure:♦ Complete form 470-3970, Prior Authorization Attachment Control. Toview a sample <strong>of</strong> this form on line, click here.Complete the “attachment control number” with the same numbersubmitted on the electronic prior authorization request. IME will acceptup to 20 characters (letters or digits) in this number. If you do not knowthe attachment control number for the request, please contact the personin your facility responsible for electronic claims billing.♦ Staple the additional information to the Prior Authorization AttachmentControl.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage24DateAugust 1, 2013♦ Fax the form with attachments to the Prior Authorization Unit at800-574-2515 or mail the information to:<strong>Iowa</strong> Medicaid EnterprisePO Box 36478Des Moines, IA 50315Once IME receives the paper attachment, it will manually be matched up tothe electronic claim using the attachment control number and thenprocessed.3. Prior Authorization ResponseThe pharmacist reviewer will make a decision and respond within 24 hours <strong>of</strong>the request. In evaluating requests for prior authorization, the reviewer willconsider the drug from the standpoint <strong>of</strong> published criteria only.If a prior authorization request is denied, a letter <strong>of</strong> denial will be faxed toboth the prescriber and the pharmacist. A letter <strong>of</strong> denial will be mailed tothe member.Upon approval <strong>of</strong> a prior authorization request, a letter <strong>of</strong> approval will befaxed to the prescriber and the pharmacy indicating the prior authorizationnumber and dates <strong>of</strong> authorization.NOTE: When approval <strong>of</strong> a request is granted, this does not indicate validity<strong>of</strong> the prescription, nor does it indicate that the member continues to beeligible for Medicaid. If you are not billing on the point-<strong>of</strong>-sale system, it isyour responsibility to establish that the member continues to be eligible forMedicaid, either by:♦ Calling the eligibility verification system (ELVS) at (515) 323-9639 (localcalls) or 800-338-7752; or♦ Checking the IME web portal;http://www.edissweb.com
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage25DateAugust 1, 20134. ADD/ADHD/Narcolepsy AgentsPrior authorization (PA) is required for ADD/ADHD/narcolepsy agents forpatients 21 years <strong>of</strong> age or older under the following conditions:♦ Attention deficit disorder (ADD) or attention deficit hyperactivity disorder(ADHD) meeting the DSM-IV criteria confirmed by a standardized ratingscale (such as Conners, Vanderbilt, Brown, Snap-IV). Symptoms musthave been present before 12 years <strong>of</strong> age and there must be clearevidence <strong>of</strong> clinically significant impairment in two ore more environments(social, academic, or occupational).♦ Narcolepsy with diagnosis confirmed with a recent sleep study (ESS,MSLT, PSG).♦ Excessive sleepiness from obstructive sleep apnea/hypopnea syndrome(OSAHS) with documentation <strong>of</strong> non-pharmacological therapies tried(weight loss, position therapy, CPAP at maximum titration, BiPAP atmaximum titration, or surgery) and results from a recent sleep study(ESS, MSLT, PSG) with the diagnosis confirmed by a sleep specialist.Payment for a nonpreferred agent will be authorized only for cases in whichthere is documentation <strong>of</strong> previous trial and therapy failure with a preferredagent.If a nonpreferred long-acting medication is requested, a trial <strong>of</strong> thepreferred immediate-release and extended release product <strong>of</strong> the samechemical entity is required.The required trials may be overridden when documented evidence is providedthat the use <strong>of</strong> these agents would be medically contraindicated.Use form 470-4116, Request for Prior Authorization: ADD/ADHD/NarcolepsyAgents, to request prior authorization. Click here to see a sample <strong>of</strong> theform.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage27DateAugust 1, 20137. Amylino Mimetic (Symlin ® )Prior authorization is required for amylino mimetics (Symlin ® ). Payment willbe considered under the following conditions:♦ Diagnosis <strong>of</strong> Type 1 or Type 2 diabetes mellitus,♦ Concurrent use <strong>of</strong> insulin therapy,♦ Documentation <strong>of</strong> blood glucose monitoring three or more times daily,♦ Inadequate reduction in HbgA1C despite multiple titration with basal/bolusinsulin-dosing regiments.Initial authorizations will be approved for six months. Additional priorauthorizations will be considered on an individual basis after review <strong>of</strong>medical necessity and documented improvement in HbgA1C since thebeginning <strong>of</strong> the initial prior authorization period.Use form 470-4406, Request for Prior Authorization: Amylino Mimetic(Symlin ® ), to request prior authorization. Click here to see a sample <strong>of</strong> theform.8. Angiotensin Receptor Blocker (ARB)Payment for ARB and ARB combinations will be considered only for cases inwhich there is a contraindication or therapy failure with at least one ACE-I orACE-I combination.A completed prior authorization form will need to be submitted if:♦ A trial with an ACE-I or ACE-I combination <strong>of</strong> at least 30 days in length isnot found in the point-<strong>of</strong>-sale system, or♦ Evidence is provided that use <strong>of</strong> an ACE-I or ACE-I combination would bemedically contraindicated.Prior authorization is required for all nonpreferred ARBs and ARBcombinations beginning the first day <strong>of</strong> therapy.Payment for nonpreferred ARB or ARB combinations will be consideredfollowing documentation <strong>of</strong> recent trials and therapy failures with a preferredACE-I or ACE-I combination and a preferred ARB or ARB combination.Use form 470-4593, Request for Prior Authorization: Angiotensin ReceptorBlocker Before ACE Inhibitor, to request prior authorization. Click here to seea sample <strong>of</strong> the form.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage28DateAugust 1, 20139. Anti-Acne ProductsPrior authorization is required for all prescription topical acne products.Payment for the treatment <strong>of</strong> mild to moderate acne vulgaris will beconsidered under the following conditions:♦ The patient has has had previous trial and therapy failure with a preferredover-the-counter benzoyl peroxide product (covered without priorauthorization).♦ Requests for nonpreferred topical acne products will be authorized only forcases in which there is documentation <strong>of</strong> previous trials and therapyfailures with two preferred topical agents <strong>of</strong> a different chemical entity.♦ Requests for nonpreferred combination products will be considered onlyafter documented separate trials and therapy failures with the individualingredients.♦ The required trials may be overridden when documented evidence isprovided that the use <strong>of</strong> these agents would be medically contraindicated.♦ Form 470-4093, Request for Prior Authorization: Anti-Acne Products -Topical, is submitted to request prior authorization. Click here to see asample <strong>of</strong> the form.If the patient presents with a preponderance <strong>of</strong> comedonal acne, topicalretinoid products may be used as first-line agents with prior authorization.See Topical Retinoids for conditions specific to retinoid products.10. Antiemetic-5HT3 Receptor Antagonists/Substance P NeurokininProductsPrior authorization is required for preferred antiemetic-5HT3 receptorantagonists/substance P neurokinin medications for quantities exceeding thefollowing dosage limits per month.♦ Aprepitant/Emend ® :• Four 125 mg capsules• Eight 80 mg capsules♦ Dolasetron/Anzemet ® :• Five 50 mg tablets• Five 100 mg tablets
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage29DateAugust 1, 2013♦ Granisetron/Kytril ® :• Eight 1 mg tablets• 30 ml oral solution (1 mg/5 ml)• Eight vials (1 mg/ml)• Two vials (4 mg/ml)♦ Ondansetron ODT/Z<strong>of</strong>ran ODT ® :• Twelve 4 mg tablets• Twelve 8 mg tablets♦ Ondansetron/Z<strong>of</strong>ran ® :• Twelve 4 mg tablets• Twelve 8 mg tablets• Four 24 mg tablets• 50 ml/month oral solution (4 mg/5 ml)• Four 20 ml vials (2 mg/ml)• Eight 2 ml vials (2 mg/ml)♦ Palonosetron/Aloxi ® : Four vials (0.25 mg/ml)Payment for antiemetic-5HT3 receptor antagonists/substance P neurokininagents beyond these limits will be considered on an individual basis afterreview <strong>of</strong> submitted documentation.NOTE: Aprepitant (Emend ® ) is payable only when used in combination withother antiemetic agents (5-HT3 medication and dexamethasone) for patientsreceiving highly emetogenic cancer chemotherapy.Prior authorization is required for all nonpreferred antiemetic-5HT3 receptorantagonists/substance P neurokinin medications beginning the first day <strong>of</strong>therapy.Payment for nonpreferred medications will be authorized only for cases inwhich there is documentation <strong>of</strong> previous trials and therapy failure with apreferred agent in this class.Use form 470-4410, Request for Prior Authorization: Antiemetic-5HT3Receptor Antagonists/Substance P Neurokinin Products, to request priorauthorization. Click here to see a sample <strong>of</strong> the form.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage30DateAugust 1, 201311. Antifungal TherapyPrior authorization is not required for preferred oral antifungal therapy for acumulative 90 days <strong>of</strong> therapy per 12-month period per patient.Payment for any oral antifungal therapy beyond this limit will be authorized incases where the patient has a diagnosis <strong>of</strong> an immunocompromised conditionor a systemic fungal infection. This prior authorization requirement does notapply to nystatin.Prior authorization is required for all nonpreferred oral antifungal therapybeginning the first day <strong>of</strong> therapy. Payment for a nonpreferred oralantifungal agent will be authorized only for cases with documentation <strong>of</strong>previous trial and therapy failure with a preferred agent.Use form 470-4094, Request for Prior Authorization: Antifungal <strong>Drugs</strong>, torequest prior authorization. Click here to see a sample <strong>of</strong> the form.12. AntihistaminesPrior authorization is required for all nonpreferred antihistamines andpreferred second-generation prescription antihistamines.♦ Members aged 21 or older must have three unsuccessful trials with oralantihistamines that do not require prior authorization prior to the approval<strong>of</strong> a nonpreferred oral antihistamine. Two <strong>of</strong> the trials must be withcetirizine and loratadine.♦ Members aged 20 or younger must have unsuccessful trials <strong>of</strong> cetirizineand loratadine prior to the approval <strong>of</strong> a nonpreferred oral antihistamine.The required trials may be overridden when documentation is provided thatthe use <strong>of</strong> these agents would be medically contraindicated.Use form 470-4095, Request for Prior Authorization: Antihistamines, torequest prior authorization. Click here to see a sample <strong>of</strong> the form.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage31DateAugust 1, 201313. Anti-ThromboticsPrior authorization will be required for all nonpreferred injectable antithromboticagents beginning the first day <strong>of</strong> therapy. Payment fornonpreferred anti-thrombotic injectable agents will be authorized only forcases in which there is documentation <strong>of</strong> previous trial and therapy failurewith a preferred agent.Prior authorization is required for use <strong>of</strong> any preferred injectable antithromboticagent longer than 10 consecutive days. Payment for usage <strong>of</strong>injectable anti-thrombotic agents beyond this limit will be authorized forcases in which there is a clinical diagnosis <strong>of</strong>:♦ Pregnancy or planned pregnancy♦ Cancer-associated thromboembolic disease♦ History <strong>of</strong> thrombotic event while on anticoagulant therapy♦ Anti-thrombin III deficiency♦ Total hip arthroplasty♦ Warfarin allergyUse form 470-4096, Request for Prior Authorization: Anti-ThromboticInjectables, to request prior authorization. Click here to see a sample <strong>of</strong> theform.14. Becaplermin (Regranex ® )Prior authorization is required for Regranex ® . Payment for new prescriptionswill be authorized for ten weeks for patients who meet the following criteria:♦ Diagnosis <strong>of</strong> lower extremity diabetic neuropathic ulcers that extend intothe subcutaneous tissue or beyond.♦ Inadequate response to two weeks <strong>of</strong> wound debridement and topicalmoist wound dressing.Authorization will be approved beyond ten weeks for patients whose woundhas decreased in size by 30% after ten weeks.Use form 470-4276, Request for Prior Authorization: Becaplermin(Regranex ® ), to request prior authorization. Click here to see a sample <strong>of</strong>the form.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage32DateAugust 1, 201315. BenzodiazepinesPrior authorization is required for nonpreferred benzodiazepines. Payment fornonpreferred benzodiazepines will be authorized in cases with documentation<strong>of</strong> previous trial and therapy failure with two preferred products. Requestsfor clobazam (Onfi) will be considered for a diagnosis <strong>of</strong> seizures associatedwith Lennox-Gastaut syndrome (LGS) in patients two years <strong>of</strong> age and olderwhen used as an adjunctive treatment. If a long-acting medication isrequested, one <strong>of</strong> the therapeutic trials must include the immediate-releaseform <strong>of</strong> the requested benzodiazepine.Prior authorization will be approved for up to 12 months for documented:♦ Generalized anxiety disorder♦ Panic attack with or without agoraphobia♦ Seizure♦ Nonprogressive motor disorder♦ DystoniaPrior authorization requests will be approved for up to a three-month periodfor all other diagnoses related to the use <strong>of</strong> benzodiazepines.The required trials may be overridden when documented evidence is providedthat use <strong>of</strong> these agents would be medically contraindicated.Use form 470-4117, Request for Prior Authorization: Benzodiazepines, torequest prior authorization. Click here to see a sample <strong>of</strong> the form.16. Biologicals for Ankylosing SpondylitisPrior authorization is required for biologicals used for ankylosing spondylitis.Payment will be considered following inadequate responses to two preferrednon-steroidal anti-inflammatories (NSAIDs) at maximum therapeutic dosesunless there are documented adverse responses or contraindications toNSAID use. Trials should be at least three months in duration.Patients with symptoms <strong>of</strong> peripheral arthritis must also have failed a 30-daytrial with at least one conventional disease-modifying antirheumatic drug(DMARD), unless there is a documented adverse response or contraindicationto DMARD use. DMARDs include sulfasalazine and methotrexate.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage33DateAugust 1, 2013Payment for nonpreferred biologicals for ankylosing spondylitis will beconsidered only for cases in which there is documentation <strong>of</strong> a previous trialsand therapy failures with two preferred biological agents.Use form 470-4521, Request for Prior Authorization: Biologicals forAnkylosing Spondylitis, to request prior authorization. Click here to see asample <strong>of</strong> the form.17. Biologicals for ArthritisPrior authorization is required for biologicals used for arthritis. Patientsinitiating therapy with a biological agent must:♦ Be screened for hepatitis B and C. Patients with active hepatitis B will notbe considered for coverage.♦ Not have been treated for solid malignancies, nonmelanoma skin cancer,or lymphoproliferative malignancy within the last five years <strong>of</strong> starting orresuming treatment with a biological agent.♦ Not have a diagnosis <strong>of</strong> congestive heart failure (CHF) that is New YorkHeart Association (NYHA) class lll or lV with an ejection fraction <strong>of</strong> 50% orless.♦ Be screened for latent TB infection. Patients with latent TB infection willonly be considered after one month <strong>of</strong> TB treatment. Patients with activeTB will only be considered upon completion <strong>of</strong> TB treatment.Payment will be considered under the following conditions:♦ A diagnosis <strong>of</strong> rheumatoid arthritis (RA). A trial and inadequate responseto two preferred disease-modifying antirheumatic drugs (DMARD) usedconcurrently. The combination must include methotrexate plus anotherpreferred oral DMARD (hydroxychloroquine, sulfasalazine, leflunomide, orminocycline). Upon an unsuccessful methotrexate trial in patients withestablished RA, the combination trial with a second DMARD may beoverridden if there is evidence <strong>of</strong> severe disease documented byradiographic erosions.♦ A diagnosis <strong>of</strong> moderate to severe psoriatic arthritis. A trial andinadequate response to the preferred oral DMARD, methotrexate(leflunomide or sulfasalazine may be used if methotrexate iscontraindicated).
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage34DateAugust 1, 2013♦ A diagnosis <strong>of</strong> moderate to severe juvenile idiopathic arthritis. A trial andinadequate response to intraarticular glucocorticoid injections and thepreferred oral DMARD, methotrexate (leflunomide or sulfasalazine may beused if methotrexate is contraindicated).The required trials may be overridden when documented evidence is providedthat the use <strong>of</strong> these agents would be medically contraindicated.Payment for nonpreferred biologicals for arthritis will be considered only forcases in which there is documentation <strong>of</strong> a previous trials and therapy failureswith two preferred biological agents.Use form 470-4522, Request for Prior Authorization: Biologicals for Arthritis,to request prior authorization. Click here to see a sample <strong>of</strong> the form.18. Biologicals for Inflammatory Bowel DiseasePrior authorization is required for biologicals used for inflammatory boweldisease.Payment for nonpreferred biologicals for inflammatory bowel disease will beconsidered only for cases in which there is documentation <strong>of</strong> a previous trialand therapy failure with a preferred agent.♦ Crohn’s disease. Payment will be considered following an inadequateresponse to two preferred conventional therapies, such asaminosalicylates (mesalamine, sulfasalazine), corticosteroids,azathioprine/6-mercaptopurine, or methotrexate.♦ Ulcerative colitis (moderate to severe). Payment will be consideredfollowing an inadequate response to two preferred conventional therapiesincluding aminosalicylates and azathioprine/6-mercaptopurine.Use form 470-4523, Request for Prior Authorization: Biologicals forInflammatory Bowel Disease, to request prior authorization. Click here to seea sample <strong>of</strong> the form.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage35DateAugust 1, 201319. Biologicals for Plaque PsoriasisPrior authorization is required for biologicals used for plaque psoriasis.Payment will be considered following an inadequate response tophototherapy, systemic retinoids (oral isotretinoin), methotrexate, orcyclosporine.Payment for nonpreferred biologicals for plaque psoriasis will be consideredonly for cases in which there is documentation <strong>of</strong> previous trials and therapyfailures with two preferred biological agents.Use form 470-4524, Request for Prior Authorization: Biologicals for PlaquePsoriasis, to request prior authorization. Click here to see a sample <strong>of</strong> theform.20. Buprenorphine (Butrans) Transdermal SystemPrior authorization is required for Butrans. Payment will be consideredwhen the following criteria are met:♦ Previous trials and therapy failures at a therapeutic dose with twopreferred long-acting opioids. The preferred trials must allow foradequate dose titration and show use <strong>of</strong> a short-acting narcotic forbreakthrough pain.♦ A trial and therapy failure with fentanyl patch at maximum tolerated dose.The required trials may be overridden when documented evidence is providedthat the use <strong>of</strong> these agents would be medically contraindicated.Use form 470-5017, Request for Prior Authorization: Buprenorphine(Butrans ) Transdermal System, to request prior authorization. Click here tosee a sample <strong>of</strong> the form.21. Buprenorphine/Naloxone (Suboxone ® )Prior authorization is required for buprenorphine or buprenorphine/naloxone(Suboxone ® ). Requests for doses above 24mg per day or greater than oncedaily dosing will not be considered. Initial requests will be considered for upto three months. Requests for maintenance doses above 16mg per day willnot be considered on a long-term basis.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage36DateAugust 1, 2013Concomitant use with opioids, tramadol, and hypnotics will be prohibited.Benzodiazepines will be allowed up to a cumulative 30 days per 12 monthperiod. Payment will be considered for patients when the following is met:♦ Patient has a diagnosis <strong>of</strong> opioid dependence and is 16 years <strong>of</strong> age orolder; AND♦ Prescriber meets qualification criteria to prescribe buprenorphine/naloxone(Suboxone ® ) for opioid dependence and has an “X” DEA number; AND♦ Patient is participating in and compliant with formal substance abusecounseling or psychosocial therapy; AND♦ A projected treatment plan is provided, including:• Anticipated induction and stabilization dose,• Anticipated maintenance dose,• Expected frequency <strong>of</strong> <strong>of</strong>fice visits, and• Expected frequency <strong>of</strong> counseling or psychosocial therapy visits♦ Requests for renewal must include:• An updated treatment plan, including consideration <strong>of</strong> a medical taperto the lowest effective dose based on a self-assessment scale,• Documentation the <strong>Iowa</strong> Prescription Monitoring Program website hasbeen reviewed for the patient’s use <strong>of</strong> controlled substances since thelast prior authorization request,• Documentation <strong>of</strong> a current, negative drug screen,• Documentation the patient has been compliant with <strong>of</strong>fice visits andcounseling or psychosocial therapy visits.Requests for buprenorphine will only be considered for pregnant patients.Use form 470-5142, Request for Prior Authorization: Buprenorphine/Naloxone (Suboxone ® ), to request prior authorization. Click here to see asample <strong>of</strong> the form.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage37DateAugust 1, 201322. Chronic Pain Syndrome AgentsPrior authorization is required for duloxetine (Cymbalta ® ), pregabalin(Lyrica ® ), and milnacipran (Savella ). Payment will be considered under thefollowing conditions:♦ A diagnosis <strong>of</strong> fibromyalgia (Cymbalta ® , Lyrica ® , and Savella ) with:• A trial and therapy failure at a therapeutic dose with three drugs fromthree distinct therapeutic classes from the following: tricyclicantidepressant, muscle relaxant, SSRI/SNRI, tramadol, or gabapentin,and• Documented non-pharmacologic therapies (cognitive behaviortherapies, exercise, etc.), and• Documentation <strong>of</strong> a previous trial and therapy failure at a therapeuticdose with Savella when Cymbalta ® and Lyrica ® are requested.♦ A diagnosis <strong>of</strong> postherpetic neuralgia (Lyrica ® ) with a trial and therapyfailure at a therapeutic dose with at least two drugs from two distincttherapeutic classes from the following: tricyclic antidepressant, topicallidocaine, valproate, carbamazepine, or gabapentin♦ A diagnosis <strong>of</strong> diabetic peripheral neuropathy (Cymbalta ® and Lyrica ® )with a trial and therapy failure at a therapeutic dose with at least twodrugs from two distinct therapeutic classes from the following: tricyclicantidepressant, topical lidocaine, tramadol, or gabapentin♦ A diagnosis <strong>of</strong> partial onset seizures, as adjunct therapy (Lyrica ® )♦ A diagnosis <strong>of</strong> major depressive disorder or generalized anxiety disorder(Cymbalta ® )♦ A diagnosis <strong>of</strong> chronic musculoskeletal pain (Cymbalta ® ) with a trialand therapy failure at a therapeutic dose with at least three drugs fromthree distinct therapeutic classes from the following: NSAIDs, opioids,tramadol, or tricyclic antidepressants.Requests for concomitant use <strong>of</strong> these agents for an indicated chronic paindiagnosis may only be considered once each agent has been tried atmaximum tolerated dose separately. Duplicate use <strong>of</strong> drugs from the sametherapeutic category will not be considered.Use form 470-4551, Request for Prior Authorization: Chronic Pain Syndrome,to request prior authorization. Click here to see a sample <strong>of</strong> the form.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage38DateAugust 1, 201323. Colchicine (Colcrys ® )Prior authorization is not required for colchicine (Colcrys ® ) for the treatment<strong>of</strong> acute gout for 3 tablets per 60-day period. Prior authorization is requiredfor colchicine (Colcrys ® ) for the treatment <strong>of</strong> chronic hyperuricemia/goutprophylaxis or Familial Mediterranean fever. Payment will be consideredunder the following conditions:♦ Chronic hyperuricemia/gout prophylaxis following a trial and therapyfailure at a therapeutic dose with allopurinol or probenecid. A quantitylimit <strong>of</strong> 60 tablets per 30 days will be applied, when criteria for coverageare met.♦ Familial Mediterranean fever. A maximum quantity limit <strong>of</strong> 120 tabletsper 30 days will be applied for this diagnosis.The required trials may be overridden when documented evidence is providedthat the use <strong>of</strong> these agents would be medically contraindicated.Use form 470-5059, Request for Prior Authorization: Colchicine (Colcrys ® ),to request prior authorization. Click here to see a sample <strong>of</strong> the form.24. Concurrent IM/PO Antipsychotic UsePrior authorization is required for concurrent long-acting injectable and oralantipsychotic medications after 12 weeks (84 days) <strong>of</strong> concomitanttreatment. Consideration <strong>of</strong> concomitant therapy beyond 12 weeks (84 days)will require documentation <strong>of</strong> medical necessity.Prior authorization is required for all nonpreferred antipsychotics as indicatedon the <strong>Iowa</strong> Medicaid Preferred Drug List beginning the first day <strong>of</strong> therapy.Payment for nonpreferred antipsychotics will be considered only for cases inwhich there is documentation <strong>of</strong> previous trials and therapy failures with apreferred agent.Use form 470-4594, Request for Prior Authorization: Concurrent IM/POAntipsychotic Utilization, to request prior authorization. Click here to see asample <strong>of</strong> the form.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage39DateAugust 1, 201325. Crizotinib (Xalkori ® )Prior authorization is required for Xalkori ® (Crizotinib). Payment will beconsidered for patients when the following is met:♦ Diagnosis <strong>of</strong> locally advanced or metastatic non-small cell lung cancer(NSCLC) that is anaplastic lymphoma kinase (ALK)-positive as detected byan FDA-approved test (attach copy <strong>of</strong> results); and♦ Is prescribed by an oncologist.Use form 470-5118, Request for Prior Authorization: Crizotinib (Xalkori ® ), torequest prior authorization. Click here to see a sample <strong>of</strong> the form.26. Dalfampridine (Ampyra)Prior authorization is required for dalfampridine (Ampyra). Payment will beconsidered under the following conditions:♦ For patients that have a gait disorder associated with MS.♦ Initial authorizations will be approved for 12 weeks with a baseline timed25-foot walk (T25FW) assessment.♦ Additional prior authorizations will be considered at six-month intervalsafter assessing the benefit to the patient as measured by a 20%improvement in T25FW from baseline. Renewal will not be approved ifthe 20% improvement is not maintained.♦ Prior authorizations will not be considered for patients with a seizurediagnosis or in patients with moderate or severe renal impairment.Use form 470-5015, Request for Prior Authorization: Dalfampridine(Ampyra), to request prior authorization. Click here to see a sample <strong>of</strong> theform.27. Dextromethorphan and Quinidine (Nuedexta)Prior authorization is required for Nuedexta. Payment will be consideredunder the following conditions:♦ Patients must have a diagnosis <strong>of</strong> pseudobulbar affect (PBA) secondary toamyotrophic lateral sclerosis (ALS) or multiple sclerosis (MS).♦ A trial and therapy failure at a therapeutic dose with amitriptyline or anSSRI.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage40DateAugust 1, 2013♦ Initial authorizations will be approved for 12 weeks with a baseline Centerfor Neurologic Studies Lability Scale (CNS-LS) questionnaire.♦ Subsequent prior authorizations will be considered at six month intervalswith documented efficacy as seen in an improvement in the CNS-LSquestionnaire.Use form 470-5084, Request for Prior Authorization: Dextromethorphan andQuinidine (Nuedexta), to request prior authorization. Click here to see asample <strong>of</strong> the form.28. Digestive EnzymesPrior authorization is required for all digestive enzymes.Payment for preferred digestive enzymes will be authorized only for cases inwhich there is a clinical diagnosis <strong>of</strong> malabsorption due to pancreaticinsufficiency.Payment for nonpreferred digestive enzymes will be authorized only forcases in which there is documentation <strong>of</strong> previous trial and therapy failurewith a preferred agent.Use form 470-4104, Request for Prior Authorization: Miscellaneous, torequest prior authorization. Click here to see a sample <strong>of</strong> the form.29. Dipeptidyl Peptidase-4 (DPP-4) InhibitorsPrior authorization is required for dipeptidyl peptidase-4 (DPP-4) inhibitorsand DPP-4 inhibitor combinations. Payment will be considered under thefollowing conditions:♦ The patient has a diagnosis <strong>of</strong> Type 2 diabetes mellitus;♦ The patient is 18 years <strong>of</strong> age or older; and♦ The patient has not achieved HbgA1C goals using a combination <strong>of</strong> two ormore antidiabetic medications (metformin, sulfonylurea, thiazolidinedione,or insulin) at maximum tolerated doses unless otherwise contraindicated.Payment for a nonpreferred agent will be authorized only for cases in whichthere is documentation <strong>of</strong> a previous trial and therapy failure with a preferredagent, unless evidence is provided that use <strong>of</strong> these agents would bemedically contraindicated.Use form 470-4897, Request for Prior Authorization: DPP-4 Inhibitors, torequest prior authorization. Click here to see a sample <strong>of</strong> the form.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage41DateAugust 1, 201330. Dornase Alfa (Pulmozyme ® )Prior authorization is required for Pulmozyme ® . Payment will be authorizedonly for cases in which there is a diagnosis <strong>of</strong> cystic fibrosis.Use form 470-4104, Request for Prior Authorization: Miscellaneous, torequest prior authorization. Click here to see a sample <strong>of</strong> the form.31. Eplerenone (Inspra ® )Prior authorization is required for Inspra ® . Payment will be authorized only incases where there is documented trial and therapy failure on Aldactone ® ordocumented cases <strong>of</strong> gynecomastia from Aldactone ® therapy.Use form 470-4104, Request for Prior Authorization: Miscellaneous, torequest prior authorization. Click here to see a sample <strong>of</strong> the form.32. Erythropoiesis Stimulating AgentsPrior authorization is required for erythropoiesis stimulating agents prescribedfor outpatients for the treatment <strong>of</strong> anemia.Payment for nonpreferred erythropoiesis stimulating agents will beauthorized only for cases in which there is documentation <strong>of</strong> previous trialand therapy failure with a preferred agent.Patients who meet all <strong>of</strong> the following criteria may receive prior authorizationfor the use <strong>of</strong> erythropoiesis stimulating agents:♦ Hemoglobin less than 10g/dL. If renewal <strong>of</strong> prior authorization is beingrequested, a hemoglobin less than 11g/dL (or less than 10g/dL forpatients with Chronic Kidney Disease (CKD) not on dialysis) will berequired for continued treatment. Hemoglobin laboratory values must bedated within four weeks <strong>of</strong> the prior authorization request.♦ Transferrin saturation greater than or equal to 20 percent (transferrinsaturation is calculated by dividing serum iron by the total iron bindingcapacity), ferritin levels greater than or equal to 100 mg/ml, or onconcurrent therapeutic iron therapy.Transferrin saturation or ferritin levels must be dated within three months<strong>of</strong> the prior authorization request.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage42DateAugust 1, 2013♦ For HIV-infected patients, the endogenous serum erythropoietin levelmust be less than or equal to 500 mU/ml to initiate therapy.♦ No evidence <strong>of</strong> untreated GI bleeding, hemolysis, or vitamin B-12, iron orfolate deficiency.Use form 470-4098, Request for Prior Authorization: ErythropoiesisStimulating Agents, to request prior authorization. Click here to see a sample<strong>of</strong> the form.33. Extended-Release FormulationsPayment for a nonpreferred extended-release formulation will be consideredwhen both <strong>of</strong> the following criteria are met:♦ Previous trial with the preferred immediate-release product <strong>of</strong> the samechemical entity at a therapeutic dose that resulted in a partial responsewith a documented intolerance, and♦ Previous trial and therapy failure at a therapeutic dose with a preferreddrug <strong>of</strong> a different chemical entity that is indicated to treat the submitteddiagnosis.Use form 470-4550, Request for Prior Authorization: Extended ReleaseFormulations, to request prior authorization. Click here to see a sample <strong>of</strong>the form.34. Febuxostat (Uloric ® )Prior authorization is required for febuxostat (Uloric ® ). Payment forfebuxostat (Uloric ® ) will only be considered for cases in which there is adiagnosis <strong>of</strong> gout still persistent while currently using 300 mg per day <strong>of</strong> apreferred allopurinol product unless documentation is provided that such astrial would be medically contraindicated.Use form 470-4849, Request for Prior Authorization: Febuxostat (Uloric ® ), torequest prior authorization. Click here to see a sample <strong>of</strong> the form.35. Fentanyl, Short-Acting Oral ProductsPrior authorization is required for short-acting oral fentanyl products.Payment will be authorized only if the diagnosis is for breakthrough cancerpain in opioid-tolerant patients. This product carries a Black Box Warning.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage43DateAugust 1, 2013Actiq ® , Fentora ® , and Onsolis are indicated only for the management <strong>of</strong>breakthrough cancer pain in patients with malignancies who are alreadyreceiving and tolerant to opioid therapy for their underlying persistent cancerpain.Actiq ® , Fentora ® , and Onsolis are contraindicated in the management <strong>of</strong>acute or postoperative pain. Because life-threatening hypoventilation couldoccur at any dose in patients not taking chronic opiates, do not use theseproducts for patients who are not opioid-tolerant.Use form 470-4092, Request for Prior Authorization: Fentanyl, Short ActingOral Products, to request prior authorization. Click here to see a sample <strong>of</strong>the form.36. Fingolimod (Gilenya)A prior authorization is required for Fingolimod (Gilenya ). Payment will beconsidered under the following conditions:♦ A diagnosis <strong>of</strong> relapsing forms <strong>of</strong> multiple sclerosis, and♦ A previous trial and therapy failure with a preferred interferon or noninterferonused to treat multiple sclerosis.The required trial may be overridden when documented evidence is providedthat the use <strong>of</strong> these agents would be medically contraindicated.Use form 470-5060, Request for Prior Authorization: Fingolimod (Gilenya ),to request prior authorization. Click here to see a sample <strong>of</strong> the form.37. Granulocyte Colony Stimulating Factor AgentsPrior authorization is required for therapy with granulocyte colony stimulatingfactor agents.Payment for nonpreferred granulocyte colony stimulating factor agents willbe authorized only for cases in which there is documentation <strong>of</strong> previous trialand therapy failure with a preferred agent. Laboratory values for completeblood and platelet count must be obtained as directed by the manufacturer’sinstructions.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage46DateAugust 1, 201340. Immunomodulators – TopicalPrior authorization is required for topical immunomodulators. When there isan adequate trial and therapy failure with two preferred topicalcorticosteroids, payment will be considered:♦ For pimecrolimus (Elidel ® ) or tacrolimus (Protopic ® ) 0.03% for nonimmunocompromisedpatients two years <strong>of</strong> age and older; and♦ For tacrolimus (Protopic ® ) 0.1% for patients 16 years <strong>of</strong> age and olderThe required trials may be overridden when documented evidence is providedthat use <strong>of</strong> these agents would be medically contraindicated.Use form 470-5040, Request for Prior Authorization: Immunomodulators –Topical, to request prior authorization. Click here to see a sample <strong>of</strong> theform.If criteria for coverage are met, requests will be approved for one tube per 90days to ensure appropriate short-term and intermittent utilization <strong>of</strong> themedication. Quantities will be limited to 30 grams for use on the face, neck,and groin, and 60 grams or 100 grams for all other areas.41. Incretin Mimetic (Byetta ® and Victoza ® )Prior authorization is required for incretin mimetics (Byetta ® and Victoza ® ).Payment will be considered under the following conditions:♦ The member has a diagnosis <strong>of</strong> type 2 diabetes mellitus.♦ The member has not achieved glycemic goals using a combination <strong>of</strong> twoor more antidiabetic medications (metformin, sulfonylurea, orthiazolidinedione) at maximum tolerated doses unless otherwisecontraindicated.An initial authorization will be approved for six months. Additional priorauthorizations will be considered on an individual basis after review <strong>of</strong>medical necessity and documented improvement in glycemic control since theinitial prior authorization.Use form 470-4407, Request for Prior Authorization: Incretin Mimetic(Byetta ® and Victoza ® ), to request prior authorization. Click here to see asample <strong>of</strong> the form.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage47DateAugust 1, 201342. Insulin Pens, Pre-filledPrior authorization is required for pre-filled insulin pens. Prior authorization isgranted when documentation indicates:♦ The member’s visual or motor skills are impaired to such that the membercannot accurately draw up the insulin, and♦ There is no caregiver available to provide assistance.Prior authorization for nonpreferred insulin pens will be granted only forcases in which there is documentation <strong>of</strong> previous trial and therapy failurewith a preferred agent.Use form 470-4111, Request for Prior Authorization: Insulin, Pre-Filled Pens,to request prior authorization. Click here to see a sample <strong>of</strong> the form.43. Isotretinoin (Oral)Prior authorization is required for oral isotretinoin therapy. Payment will beapproved for preferred oral isotretinoin products for acne under the followingconditions:♦ There are documented trials and therapy failures <strong>of</strong> systemic antibiotictherapy and topical tretinoin therapy. Trials and failures <strong>of</strong> systemicantibiotic therapy and topical tretinoin therapy are not required forapproval for treatment <strong>of</strong> acne conglobata.♦ Patients and providers must be registered in, and meet all requirements<strong>of</strong>, the iPLEDGE (https://www.ipledgeprogram.com/) risk managementprogram.Payment for nonpreferred oral isotretinoin products will be authorized only forcases in which there is documentation <strong>of</strong> trials and therapy failure with apreferred agent. Initial authorization will be granted for up to 20 weeks. Aminimum <strong>of</strong> two months without therapy is required to consider subsequentauthorizations.Use form 470-4101, Request for Prior Authorization: Isotretinoin (Oral), torequest prior authorization. Click here to see a sample <strong>of</strong> the form.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage48DateAugust 1, 201344. Ivacaftor (Kalydeco )Prior authorization is required for Kalydeco (Ivacaftor). Payment will beconsidered for patients when the following criteria are met:♦ Patient is six years <strong>of</strong> age or older; and♦ Has a diagnosis <strong>of</strong> cystic fibrosis with a G551D mutation in the CFTR geneas detected by an FDA-cleared cystic fibrosis mutation test; and♦ Prescriber is a cystic fibrosis specialist or pulmonologist; and♦ Patient does not have one <strong>of</strong> the following infections: Burkholderiacenecepacia, dolosa, or Mycobacterium abcessus.Use form 470-5117, Request for Prior Authorization: Ivacaftor (Kalydeco ),to request prior authorization. Click here to see a sample <strong>of</strong> the form.45. Ketorolac Tromethamine (Toradol ® )Prior authorization is required for ketorolac tromethamine, a nonsteroidalanti-inflammatory drug indicated for short-term management <strong>of</strong> moderatelysevere, acute pain (up to five days). It is not indicated for minor or chronicconditions. This product carries a Black Box Warning.Initiate therapy with IV/IM and use oral ketorolac tromethamine only as acontinuation therapy to ketorolac tromethamine IV/IM. The combinedduration <strong>of</strong> use <strong>of</strong> IV/IM and oral is not to exceed five days. Payment will beapproved for the preferred product under the following conditions:♦ For oral therapy, documentation <strong>of</strong> recent IM/IV ketorolac tromethamineinjection including administration date and time, and the total number <strong>of</strong>injections given.♦ Request falls within the manufacturer’s dosing guidelines. Maximum oraldose is 40 mg/day. Maximum IV/IM dose is 120 mg/day. Maximumintranasal dose is 126 mg/day. Maximum duration <strong>of</strong> therapy is 5 daysper month.♦ Diagnosis indicating moderately severe, acute pain.Requests for IV/IM and intranasal ketorolac must document previous trialsand therapy failures with at least two preferred nonsteroidal antiinflammatorydrugs at therapeutic doses.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage49DateAugust 1, 2013Use form 470-4102, Request for Prior Authorization: KetorolacTromethamine (Toradol ® ), to request prior authorization. Click here to see asample <strong>of</strong> the form.46. Lidocaine Patch (Lidoderm ® )Prior authorization is required for topical lidocaine patches (Lidoderm ® ).Payment will be considered for a diagnosis <strong>of</strong> pain associated with postherpeticneuralgia following a previous treatment failure with a preferredagent at therapeutic dose from two <strong>of</strong> the following: tricyclic antidepressant,opioid, gabapentin, carbamazepine, or valproic acid.A maximum <strong>of</strong> 30 patches may be dispensed with the initial prescription todetermine efficacy.Use form 470-4898, Request for Prior Authorization: Lidocaine Patch(Lidoderm ® ), to request prior authorization. Click here to see a sample <strong>of</strong> theform.47. Linezolid (Zyvox ® )Prior authorization is required for linezolid (Zyvox ® ). Payment for Zyvox ® willbe authorized when there is documentation that:♦ The prescriber is an infectious disease physician or has consulted aninfectious disease physician. (Telephone consultation is acceptable.)♦ The member has an active infection that meets one <strong>of</strong> the followingdiagnostic criteria:• Vancomycin-resistant enterococcus (VRE) when no alternativeregimens with documented efficacy are available and VRE is not inlower urinary tract.• VRE in the lower urinary tract if severe renal insufficiency exists or thepatient is receiving hemodialysis or has known hypersensitivity tonitr<strong>of</strong>urantoin.• Methicillin-resistant staphylococcus aureus (MRSA) when the patient isintolerant to vancomycin.*• Methicillin-resistant staphylococcus epidermis (MRSE) when the patientis intolerant to vancomycin.*
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage50DateAugust 1, 2013* Severe intolerance to vancomycin is defined as:• Severe rash, immune-complex-mediated, determined to be directlyrelated to vancomycin administration.• Red-man’s syndrome (histamine-mediated), refractory to traditionalcountermeasures (e.g., prolonged IV infusion, premedicated withdiphenhydramine).Use form 470-4275, Request for Prior Authorization: Linezolid (Zyvox ® ), torequest prior authorization. Click here to see a sample <strong>of</strong> the form.48. Mifepristone (Korlym ® )Prior authorization is required for mifepristone (Korlym ® ). Payment will beconsidered for patients when the following is met:♦ The patient is 18 years <strong>of</strong> age or older; and♦ Has a diagnosis <strong>of</strong> endogenous Cushing’s Syndrome with hyperglycemiasecondary to hypercortisolism in patients with Type 2 Diabetes or glucoseintolerance; and♦ Patient must have failure surgery or is not a candidate for surgery; and♦ Prescriber is an endocrinologist.♦ Female patients <strong>of</strong> reproductive age must have a negative pregnancy testconfirmed within the last seven days and must use a non-hormonalmethod <strong>of</strong> contraception during treatment and for one month afterstopping treatment.Use form 470-5141, Request for Prior Authorization: Mifepristone (Korlym ® ),to request prior authorization. Click here to see a sample <strong>of</strong> the form.49. Modified FormulationsPayment for a nonpreferred isomer, pro-drug, or metabolite will beconsidered when the following criteria are met:♦ Previous trial with a preferred parent drug <strong>of</strong> the same chemical entity ata therapeutic dose that resulted in a partial response with a documentedintolerance; and♦ Previous trial and therapy failure at a therapeutic dose with a preferreddrug <strong>of</strong> a different chemical entity indicated to treat the submitteddiagnosis if available.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage51DateAugust 1, 2013The required trials may be overridden when documented evidence is providedthat use <strong>of</strong> these preferred agents would be medically contraindicated.Payment for a nonpreferred alternative delivery system will be consideredonly for cases in which the use <strong>of</strong> an alternative delivery system is deemedmedically necessary and there is a previous trial and therapy failure with apreferred alternative delivery system if available.Use form 470-4705, Request for Prior Authorization: Modified Formulations,to request prior authorization. Click here to see a sample <strong>of</strong> the form.50. Muscle RelaxantsPrior authorization is required for nonpreferred muscle relaxants. Paymentfor nonpreferred muscle relaxants will be authorized only for cases in whichthere is documentation <strong>of</strong> previous trials and therapy failure with at leastthree preferred muscle relaxants.Requests for carisoprodol will be approved for a maximum <strong>of</strong> 120 tablets per180 days at a maximum <strong>of</strong> 4 tablets per day when the criteria for coverageare met.If a nonpreferred long-acting medication is requested, one trial must includethe preferred immediate-release product <strong>of</strong> the same chemical entity at atherapeutic dose, unless evidence is provided that use <strong>of</strong> these productswould be medically contraindicated.Use form 470-4105, Request for Prior Authorization: Muscle Relaxants, torequest prior authorization. Click here to see a sample <strong>of</strong> the form.51. Narcotic Agonist-Antagonist Nasal SpraysPrior authorization is required for narcotic agonist-antagonist nasal sprays.The member’s diagnosis must be supplied for consideration.If the use is for the treatment <strong>of</strong> migraine headaches, documentation <strong>of</strong>current prophylactic therapy or documentation <strong>of</strong> previous trials and therapyfailures with two different prophylactic medications must be provided. Theremust also be documented treatment failure or contraindication to triptans forthe acute treatment <strong>of</strong> migraines.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage52DateAugust 1, 2013For other pain conditions, there must be documentation <strong>of</strong> treatment failureor contraindication to oral administration.Payment for nonpreferred narcotic agonist-antagonist nasal sprays will beauthorized only for cases in which there is documentation <strong>of</strong> previous trialand therapy failure with a preferred agent.Quantities are limited to 2 bottles or 5 milliliters per 30 days. Payment fornarcotic agonist-antagonist nasal sprays beyond this limit will be consideredon an individual basis after review <strong>of</strong> submitted documentation.Use form 470-4106, Request for Prior Authorization: Narcotic Agonist/Antagonist Nasal Sprays, to request prior authorization. Click here to see asample <strong>of</strong> the form.52. Nebivolol (Bystolic ® )Prior authorization is required for Bystolic ® . Payment will be considered incases where there are documented trials and therapy failures with twopreferred cardio-selective beta-blockers <strong>of</strong> a different chemical entity at atherapeutic dose. The required trials may be overridden when documentedevidence is provided that the use <strong>of</strong> these agents would be medicallycontraindicated.Use form 470-5099, Request for Prior Authorization: Nebivolol (Bystolic ® ), torequest prior authorization. Click here to see a sample <strong>of</strong> the form.53. Nicotine Replacement ProductsPrior authorization is required for over-the-counter nicotine replacementpatches, gum or lozenges, and prescription nicotine nasal spray or inhaler.Requests for authorization must include:♦ Diagnosis <strong>of</strong> nicotine dependence and referral to the Quitline <strong>Iowa</strong>program for counseling.♦ Confirmation <strong>of</strong> enrollment in the Quitline <strong>Iowa</strong> counseling program isrequired for approval. Continuation therapy is available only withdocumentation <strong>of</strong> ongoing participation in the Quitline <strong>Iowa</strong> program.♦ Approvals will be granted only for patients 18 years <strong>of</strong> age and older.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage53DateAugust 1, 2013♦ The maximum allowed duration <strong>of</strong> therapy is 12 weeks total combinedtherapy within a 12-month period.♦ Patients may receive nicotine replacement patches in combination with anoral nicotine replacement product (gum or lozenges).♦ A maximum quantity <strong>of</strong> 14 nicotine replacement patches and 110 pieces<strong>of</strong> nicotine gum or 144 nicotine lozenges may be dispensed with the initialprescription. Subsequent prescription refills will be allowed for a fourweeksupply at one unit per day <strong>of</strong> nicotine replacement patches and 330pieces <strong>of</strong> nicotine gum or 288 nicotine lozenges.♦ Requests for nonpreferred nicotine replacement products will beconsidered after documentation <strong>of</strong> previous trials and intolerance with apreferred oral and preferred topical nicotine replacement product. Amaximum quantity <strong>of</strong> 168 nicotine inhalers or 40ml nicotine nasal spraymay be dispensed with the initial prescription. Subsequent prescriptionrefills will be allowed to be dispensed as a four-week supply at 336nicotine inhalers or 80ml <strong>of</strong> nicotine nasal spray.♦ The 72-hour emergency supply rule does not apply for drugs used for thetreatment <strong>of</strong> smoking cessation.Use form 470-4421, Request for Prior Authorization: Nicotine ReplacementTherapy, to request prior authorization. Click here to see a sample <strong>of</strong> theform.54. Nonparenteral Vasopressin Derivatives <strong>of</strong> Posterior PituitaryHormone ProductsPrior authorization is required for nonparenteral vasopressin derivatives <strong>of</strong>posterior pituitary hormone products. Payment for nonparenteral vasopressinderivatives <strong>of</strong> posterior pituitary hormone products will be authorized for thefollowing diagnoses:♦ Diabetes insipidus♦ Hemophilia A♦ Von Willebrand’s DiseasePayment for oral vasopressin derivatives <strong>of</strong> posterior pituitary hormoneproducts used in the treatment <strong>of</strong> primary nocturnal enuresis will beauthorized for patients who are six years <strong>of</strong> age or older for periods <strong>of</strong> sixmonths.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage54DateAugust 1, 2013Approvals will be granted for subsequent six-month periods only after a drugfreeinterval to assess the need for continued therapy.Payment for nonpreferred nonparenteral vasopressin derivatives will beauthorized only for cases in which there is documentation <strong>of</strong> trial and therapyfailure with a preferred agent.Use form 470-4107, Request for Prior Authorization: NonparenteralVasopressin Derivatives <strong>of</strong> Posterior Pituitary Hormone Products, to requestprior authorization. Click here to see a sample <strong>of</strong> the form.55. Nonpreferred <strong>Drugs</strong>Prior authorization is required for nonpreferred drugs as specified on the <strong>Iowa</strong>Medicaid Preferred Drug List.Payment for a nonpreferred medication will be authorized only for cases inwhich there is documentation <strong>of</strong> previous trial and therapy failure with apreferred agent, unless evidence is provided that use <strong>of</strong> these agents ismedically contraindicated.Use form 470-4108, Request for Prior Authorization: Non-Preferred Drug, torequest prior authorization. Click here to see a sample <strong>of</strong> the form.56. Nonsteroidal Anti-Inflammatory <strong>Drugs</strong>Prior authorization is required for all nonpreferred nonsteroidal antiinflammatorydrugs (NSAIDs) and COX-2 inhibitors. Prior authorization is notrequired for preferred nonsteroidal anti-inflammatory drugs or COX-2inhibitors.♦ Requests for a nonpreferred NSAID must document previous trials andtherapy failures with at least three preferred NSAIDs.♦ Requests for a nonpreferred COX-2 inhibitor must document previoustrials and therapy failures with three preferred NSAIDs, two <strong>of</strong> which mustbe a preferred COX-2 preferentially selective NSAID.♦ Requests for a nonpreferred topical NSAID must document previous trialsand therapy failures with three preferred NSAIDs. The trials must includetwo preferred COX-2 preferentially selective NSAIDs and the oral drug <strong>of</strong>the same chemical entity. In addition, the use <strong>of</strong> a topical deliverysystem must be deemed medically necessary.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage55DateAugust 1, 2013♦ Requests for a nonpreferred extended release NSAID must documentprevious trials and therapy failures with three preferred NSAIDs, one <strong>of</strong>which must be the preferred.The required trials may be overridden when documented evidence is providedthat use <strong>of</strong> these agents would be medically contraindicated.Use form 470-4109, Request for Prior Authorization: Nonsteroidal Anti-Inflammatory <strong>Drugs</strong>, to request prior authorization. Click here to see asample <strong>of</strong> the form.57. Omalizumab (Xolair ® )Prior authorization is required for omalizumab (Xolair ® ). Payment for Xolair ®will be authorized when the following criteria are met:♦ Patient has a diagnosis <strong>of</strong> moderate to severe persistent asthma for atleast one year; and♦ Patient is 12 years <strong>of</strong> age or older; and♦ Pretreatment IgE level is between 30 IU/ml and 700 IU/ml; and♦ Patient’s weight is between 30 kg and 150 kg; and♦ History <strong>of</strong> a positive skin or RAST test to a perennial aeroallergen; and♦ Prescriber is an allergist, immunologist, or pulmonologist; and♦ Patient is currently using a high dose inhaled corticosteroid and longactingbeta-agonist, is compliant with therapy and asthma symptoms arenot adequately controlled after at least three months <strong>of</strong> therapy.♦ Patient must have access to an EpiPen to treat allergic reactions that mayoccur after administration <strong>of</strong> Xolair ® .If the criteria for coverage are met, the initial authorization will be given for16 weeks to assess the need for continued therapy. Requests forcontinuation <strong>of</strong> therapy will not be granted for patients who have not shownadequate response to Xolair ® therapy and for patients who do not continueconcurrent use with a high dose inhaled corticosteroid and long-acting betaagonist.The required trials may be overridden when documented evidence is providedthat the use <strong>of</strong> these agents would be medically contraindicated.Use form 470-4279, Request for Prior Authorization: Omalizumab (Xolair ® ),to request prior authorization. Click here to see a sample <strong>of</strong> the form.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage56DateAugust 1, 201358. Oxycodone ER/CR (OxyContin ® )Extended release oxycodone/OxyContin ® is nonpreferred except for membersbeing treated for cancer related pain. Prior authorization at any dose twicedaily for cancer related pain will be approved. For all other diagnoses,payment will be considered under the following conditions:♦ There is documentation <strong>of</strong> previous trials and therapy failures with twochemically distinct preferred long-acting narcotics (such as morphinesulfate ER, Opana ER, and methadone) at therapeutic doses, and♦ A trial and therapy failure with fentanyl patch at maximum tolerated dose,and♦ A signed chronic opioid therapy management plan between the prescriberand patient must be included with the prior authorization.♦ The prescriber must review the patient’s use <strong>of</strong> controlled substanceson the <strong>Iowa</strong> Prescription Monitoring program website athttps://pmp.iowa.gov/IAPMPWebCenter/ prior to requesting theprior authorization.♦ Requests will only be considered for 12 hour dosing.The required trials may be overridden when documented evidence is providedthat use <strong>of</strong> these agents would be medically contraindicated.Use form 470-4409, Request for Prior Authorization: Oxycodone ER/CR(OxyContin ® ), to request prior authorization. Click here to see a sample <strong>of</strong>the form.59. Palivizumab (Synagis ® )Respiratory Syncytial Virus (RSV) season is defined by the centers for diseasecontrol and prevention <strong>of</strong> the United States <strong>Department</strong> <strong>of</strong> Health and <strong>Human</strong>Services and described in the RSV surveillance reports published annually inthe Morbidity and Mortality Weekly Report (MMWR) and available athttp://www.cdc.gov/surveillance/nrevss/rsv/reports.html.♦ Medicaid will use virology data provided by the <strong>Iowa</strong> <strong>Department</strong> <strong>of</strong> PublicHealth (IDPH) to prospectively estimate the start <strong>of</strong> the RSV season andfollow the virology data to the end <strong>of</strong> the season.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage57DateAugust 1, 2013♦ Medicaid will provide coverage <strong>of</strong> prescription drugs that protect againstRSV consistent with the American Academy <strong>of</strong> Pediatrics (AAP) Guidelinesfor Infants and Children at Risk for Severe Illness due to RSV Infection.♦ The start date will begin two weeks before the expected season start datefor the state <strong>of</strong> <strong>Iowa</strong>. The start date will be adjusted to an earlier date byMedicaid if indicated by the virological data. The expected season startdate shall be derived from the median start date <strong>of</strong> the past five seasonsusing <strong>Iowa</strong> virological data.Prior authorization is required for therapy with palivizumab. Priorauthorizations will be approved for a maximum <strong>of</strong> five doses per patient. Noallowances will be made for a sixth dose. Payment for palivizumab will beconsidered for patients who meet one <strong>of</strong> the following criteria:♦ Chronic lung disease (CLD):The patient is less than 24 months <strong>of</strong> age at start <strong>of</strong> therapy and haschronic lung disease <strong>of</strong> prematurity (i.e. bronchopulmonary dysplasia)requiring medication (bronchodilator, corticosteroid, or diuretic therapy)or oxygen within six months before the anticipated start <strong>of</strong> RSV season.♦ Prematurity:• The patient is less than 12 months <strong>of</strong> age at start <strong>of</strong> therapy with agestational age <strong>of</strong> less than 29 weeks.• The patient is less than 6 months <strong>of</strong> age at start <strong>of</strong> therapy with agestational age between 29 weeks through 31 weeks.• The patient is less than 3 months <strong>of</strong> age at start <strong>of</strong> therapy or bornduring the RSV season with a gestational age <strong>of</strong> 32 weeks through 34weeks and has one <strong>of</strong> two risk factors. Risk factors include: day careattendance or siblings less than five years <strong>of</strong> age in household. Doseswill be limited to a maximum <strong>of</strong> 3 doses or until patient reaches 90days <strong>of</strong> age, whichever comes first.♦ Severe neuromuscular disease or congenital abnormalities:Patient is 12 months <strong>of</strong> age or younger at the start <strong>of</strong> therapy and haseither severe neuromuscular disease or congenital abnormalities <strong>of</strong> theairway that compromises handling <strong>of</strong> respiratory secretions.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage58DateAugust 1, 2013♦ Congenital heart disease (CHD):The patient is less than 24 months <strong>of</strong> age at start <strong>of</strong> therapy and hashemodynamically significant congenital heart disease further defined byany <strong>of</strong> the following:• Receiving medication to control congestive heart failure,• Moderate to severe pulmonary hypertension, or• Cyanotic congenital heart disease.♦ Severe immunodeficiency:The patient is less than 24 months <strong>of</strong> age at start <strong>of</strong> therapy and hassevere immunodeficiencies (e.g., severe combined immunodeficiency oradvanced acquired immunodeficiency syndrome).Use form 470-4110, Request for Prior Authorization: Palivizumab (Synagis ® ),to request prior authorization. Click here to see a sample <strong>of</strong> the form.60. Proton Pump InhibitorsPrior authorization is not required for the preferred proton pump inhibitors(PPI) for a cumulative 60 days <strong>of</strong> therapy per 12-month period.Prior authorization will be required beginning the first day <strong>of</strong> therapy for allnonpreferred proton pump inhibitors as indicated on the <strong>Iowa</strong> MedicaidPreferred Drug List. Payment for a nonpreferred proton pump inhibitor willbe authorized only for cases with documentation <strong>of</strong> previous trial and therapyfailure with three preferred products.Prior authorization is required for any PPI usage longer than 60 days or morefrequently than one 60-day course per 12-month period. The 12-monthperiod is patient-specific and begins 12 months before the requested date <strong>of</strong>prior authorization.Payment for usage beyond these limits will be authorized for cases in whichthere is a diagnosis <strong>of</strong>:♦ Specific hypersecretory conditions (Zollinger-Ellison syndrome, systemicmastocytosis, multiple endocrine adenomas).♦ Barrett’s esophagus.♦ Erosive esophagitis.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage59DateAugust 1, 2013♦ Symptomatic gastroesophageal reflux after documentation <strong>of</strong> previoustrials and therapy failure with at least one histamine H2-receptorantagonist at full therapeutic doses.Requests for PPIs exceeding one unit per day will be considered afterdocumentation <strong>of</strong> a therapeutic trial and therapy failure with concomitantuse <strong>of</strong> once daily PPI dosing and a bedtime dose <strong>of</strong> a histamineH2-receptor antagonist. Upon failure <strong>of</strong> the combination therapy,subsequent requests for PPIs exceeding one unit per day will beconsidered on a short term basis (up to three months).After the three-month period, a retrial <strong>of</strong> the recommended once dailydosing will be required. A trial <strong>of</strong> the recommended once daily dosing willbe required on an annual basis for those patients continuing to needdoses beyond one unit per day.♦ Recurrent peptic ulcer disease after documentation <strong>of</strong>:• Previous trials and therapy failure with at least one histamineH2-receptor antagonist at full therapeutic doses, and• Either failure <strong>of</strong> Helicobacter pylori treatment or a negativeHelicobacter pylori test result.Use form 470-4112, Request for Prior Authorization: Proton Pump Inhibitors,to request prior authorization. Click here to see a sample <strong>of</strong> the form.61. Pulmonary Arterial Hypertension AgentsPrior authorization is required for agents used to treat pulmonaryhypertension. Payment will be approved for the diagnosis <strong>of</strong> pulmonaryarterial hypertension.Use form 470-4327, Request for Prior Authorization: Pulmonary ArterialHypertension Agents, to request prior authorization. Click here to see asample <strong>of</strong> the form.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage60DateAugust 1, 201362. Quantity Limit Overridea. Initial 15-Day Limit<strong>Drugs</strong> that have been identified with high side effect pr<strong>of</strong>iles, highdiscontinuations rates, or frequent dose adjustments are limited to a15-day initial supply. The initial prescription supply limit ensures costeffectiveness without waste <strong>of</strong> unused medications.These drugs are identified on the Fifteen Day Initial Prescription SupplyLimit list located on the website www.iowamedicaidpdl.com under thePreferred Drug Lists tab and the Billing/Quantity Limits tab.To request authorization for an initial supply longer than 15 days,submit form 470-5038, Request for Fifteen Day Initial PrescriptionSupply Override, for consideration. Click here for a sample <strong>of</strong> the form.The form is located at www.iowamedicaidpdl.com under PA Forms.Documentation <strong>of</strong> medical necessity, excluding patient convenience, isrequired for consideration <strong>of</strong> the 15-day initial supply override.b. Monthly LimitsDesignated drugs have specific quantity limitations. These drugs areidentified on the <strong>Iowa</strong> Medicaid Quantity Limit Chart posted on thewebsite www.iowamedicaidpdl.com under the Billing/Quantity Limits tab.Medication doses that use multiple, lower-strength tablets should beconsolidated to the higher-strength tablet. Quantity limits based on thecompendia are also enforced. Please view the current list atwww.iowamedicaidpdl.com under Quantity Limits.Prior authorization is required if there is a reason the higher tabletstrength cannot be used or a medical rationale for use <strong>of</strong> higher thanrecommended dosing.<strong>Provider</strong>s should submit a Prior Authorization request for overrideconsideration. Use form 470-4556, Request for Prior Authorization:Request for Quantity Limit Override, to request prior authorization.Click here to see a sample <strong>of</strong> the form. The form is located atwww.iowamedicaidpdl.com under PA Forms.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage61DateAugust 1, 2013Drug ProductQuantityDays’SupplyAbilify 2 mg (aripiprazole) 15 30Abilify 5 mg (aripiprazole) 15 30Abilify 10 mg (aripiprazole) 15 30Abilify 15 mg (aripiprazole) 15 30Abilify 20 mg (aripiprazole) 15 30Abilify 30 mg (aripiprazole) 15 30Aceon 2 mg (perindopril) 30 30Aceon 4 mg (perindopril) 30 30Aceon 8 mg (perindopril) 60 30Aciphex 20 mg (rabeprazole) 60 30Actonel 5 mg (risedronate) 30 30Actonel 30 mg (risedronate) 30 30Actonel 35 mg (risedronate) 4 30Actoplus Met 15-500 mg60 30(metformin/pioglitazone)Actoplus Met 15-850 mg60 30(metformin/pioglitazone)Actos 15 mg (pioglitazone) 30 30Actos 30 mg (pioglitazone) 30 30Actos 45 mg (pioglitazone) 30 30Adalat CC 30 mg (nifedipine ER) 30 30Adalat CC 60 mg (nifedipine ER) 30 30Adalat CC 90 mg (nifedipine ER) 30 30Adderall 5 mg (amphetamine salt 90 30combo)Adderall 7.5 mg (amphetamine salt 90 30combo)Adderall 10 mg (amphetamine salt 90 30combo)Adderall 12.5 mg (amphetamine 120 30salt combo)Adderall 15 mg (amphetamine salt 90 30combo)Adderall 20 mg (amphetamine salt 120 30combo)Adderall 30 mg (amphetamine salt 60 30combo)Adderall XR 5 mg(amphetamine ER)30 30Comments
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage62DateAugust 1, 2013Drug ProductAdderall XR 10 mg(amphetamine combo)Adderall XR 15 mg(amphetamine combo)Adderall XR 20 mg(amphetamine ER)Adderall XR 25 mg(amphetamine ER)Adderall XR 30 mg(amphetamine ER)Advair 100/50 diskus(fluticasone/salmeterol)Advair 250/50 diskus(fluticasone/salmeterol)Advair 500/50 diskus(fluticasone/salmeterol)Advair HFA (fluticasone/salmeterol)Days’Quantity Supply30 3030 3060 3060 3060 3060 3060 3060 301 inhaler(12 gm)30CommentsAerobid (flunisolide) 21 30Aerobid-M (flunisolide) 21 30Afinitor 2.5 mg (everolimus) 30 30Afinitor 5 mg (everolimus) 30 30Afinitor 7.5 mg (everolimus) 30 30Afinitor 10 mg (everolimus) 30 30Aldara (imiquimod) 12 pkts 28 Max 48 pkts/16 weeksAllegra 30 mg (fex<strong>of</strong>enadine) 60 30Allegra 60 mg (fex<strong>of</strong>enadine) 60 30Allegra 180 mg (fex<strong>of</strong>enadine) 30 30Alphagan P (brimonidine tartrate) 15 ml 30Alprazolam intensol 1 mg/ml180 ml 30(alprazolam)Altace 1.25 mg (ramipril) 30 30Altace 2.5 mg (ramipril) 30 30Altace 5 mg (ramipril) 30 30Altace 10 mg (ramipril) 60 30Amaryl 1 mg (glimepiride) 30 30Amaryl 2 mg (glimepiride) 30 30Amaryl 4 mg (glimepiride) 60 30Ambien 5 mg (zolpidem) 30 30Ambien 10 mg (zolpidem) 30 30Ambien CR 6.25 mg (zolpidem) 30 30Ambien CR 12.5 mg (zolpidem) 30 30
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage63DateAugust 1, 2013Drug ProductQuantityDays’SupplyAmpyra 10 mg (dalfampridine) 60 30Androgel 1% (25 mg) gel30 pkts 30(testosterone)Androgel 1% (50 mg) gel60 pkts 30(testosterone)Androgel 1% pump (testosterone) 300 gm 30Androgel 1.62% pump150 gm 30(testosterone)Arava 10 mg (leflunomide) 30 30Arava 20 mg (leflunomide) 30 30Arava 100 mg (leflunomide) 3 30Aricept ODT 5 mg (donepezil) 30 30Aricept ODT 10 mg (donepezil) 30 30Aricept 5 mg (donepezil) 30 30Aricept 10 mg (donepezil) 30 30Aricept 23 mg (donepezil) 30 30Astelin nasal spray (azelastine) 30 ml 30Atacand 4 mg (candesartan) 30 30Atacand 8 mg (candesartan) 30 30Atacand 16 mg (candesartan) 30 30Atacand 32 mg (candesartan) 30 30Atacand HCT 16-12.5 mg30 30(candesartan/HCTZ)Atacand HCT 32-12.5 mg30 30(candesartan/HCTZ)Ativan 0.5mg tablet (lorazepam) 150 30Ativan 1 mg tablet (lorazepam) 150 30Ativan 2 mg tablet (lorazepam) 150 30Atrovent HFA (ipratropium)2 bottles 30(25.8 gm)Atrovent inhaler (ipratropium) 2 inhalers 30(28 gm)Atrovent 0.03% nasal spray2 bottles 30(ipratropium)Atrovent 0.06% nasal spray2 bottles 30(ipratropium)Auvi-Q (epinephrine) 2 units 30Comments
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage64DateAugust 1, 2013Drug ProductAvalide 150-12.5 mg(irbesartan/HCTZ)Avalide 300-12.5 mg(irbesartan/HCTZ)Avalide 300-25 mg(irbesartan/HCTZ)Avandaryl 4 mg/1 mg(glimepiride/rosiglitazone)Avandaryl 4 mg/2 mg(glimepiride/rosiglitazone)Avandaryl 4 mg/4 mg(glimepiride/rosiglitazone)Days’Quantity Supply30 3030 3030 3060 3060 3060 30Avandia 8 mg (rosiglitazone) 30 30Avapro 75 mg (irbesartan) 30 30Avapro 150 mg (irbesartan) 30 30Avapro 300 mg (irbesartan) 30 30Avinza 30 mg (morphine ER) 30 30Avinza 45 mg (morphine ER) 30 30Avinza 60 mg (morphine ER) 30 30Avinza 75 mg (morphine ER) 30 30Avinza 90 mg (morphine ER) 30 30Avinza 120 mg (morphine ER) 150 30Bactroban nasal ointment 10 grams 30Bactroban ointment (mupirocin) 44 grams 30Beconase AQ (beclomethasonedipropionate)2 inhalers(50 gm)Benicar 5 mg (olmesartan) 30 30Benicar 20 mg (olmesartan) 30 30Benicar 40 mg (olmesartan) 30 30Benicar HCT 20-12.5 mg30 30(olmesartan/HCTZ)Benicar HCT 40-12.5 mg30 30(olmesartan/HCTZ)Benicar HCT 40-25 mg30 30(olmesartan/HCTZ)Boniva 2.5 mg (ibandronate) 30 30Boniva 150 mg (ibandronate) 1 tablet 30Boniva syr (ibandronate) 1 syringe 9030Comments
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage65DateAugust 1, 2013Drug ProductCaduet 2.5-20 mg(amlodipine/atorvastatin)Caduet 2.5-40 mg(amlodipine/atorvastatin)Caduet 2.5-100 mg(amlodipine/atorvastatin)Caduet 5-10 mg(amlodipine/atorvastatin)Caduet 5-20 mg(amlodipine/atorvastatin)Caduet 5-40 mg(amlodipine/atorvastatin)Caduet 5-80 mg(amlodipine/atorvastatin)Caduet 10-10 mg(amlodipine/atorvastatin)Caduet 10-20 mg(amlodipine/atorvastatin)Caduet 10-40 mg(amlodipine/atorvastatin)Caduet 10-80 mg(amlodipine/atorvastatin)Days’Quantity Supply30 3030 3030 3030 3030 3030 3030 3030 3030 3030 3030 30Catapres 0.1 mg (clonidine) 120 30Catapres 0.2 mg (clonidine) 90 30Catapres 0.3 mg (clonidine) 60 30Celebrex 100 mg (celecoxib) 60 30Celebrex 200 mg (celecoxib) 30 30Celebrex 400 mg (celecoxib) 30 30Celexa 10 mg (citalopram) 45 30Celexa 20 mg (citalopram) 45 30Claritin OTC 10 mg (loratadine) 30 30Clindesse 2% vaginal cream40 gm 30(clindamycin phosphate)Cocet (acetaminophen/codeine) 180 30Codeine Sulfate 15 mg 180 30Codeine Sulfate 30 mg 180 30Codeine Sulfate 60 mg 180 30Combunox (oxycodone/ibupr<strong>of</strong>en) 28 30Complera (emtricitabine/rilpivirine/ten<strong>of</strong>ovir disoproxil fumarate)30 30Comments
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage66DateAugust 1, 2013Drug ProductConcerta SA 18 mg(methylphenidate ER)Concerta SA 27 mg(methylphenidate ER)Concerta SA 36 mg(methylphenidate ER)Concerta SA 54 mg(methylphenidate ER)Cosopt (dorzolamide hydrochloride/timolol maleate)Days’Quantity Supply60 3060 3060 3060 3010 ml 30Cozaar 25 mg (losartan) 60 30Cozaar 50 mg (losartan) 60 30Cozaar 100 mg (losartan) 30 30Crestor 5 mg (rosuvastatin) 30 30Crestor 10 mg (rosuvastatin) 30 30Crestor 20 mg (rosuvastatin) 30 30Crestor 40 mg (rosuvastatin) 30 30Cymbalta 20 mg (duloxetine) 60 30Cymbalta 30 mg (duloxetine) 60 30Cymbalta 60 mg (duloxetine) 60 30Dalmane 15 mg (flurazepam) 30 30Dalmane 30 mg (flurazepam) 30 30Darvocet-N 50 (propoxyphene-n/ 180 30acetaminophen)Darvocet-N 100 (propoxyphenen/acetaminophen)180 30Daytrana 10 mg/9-hour patch30 30(methylphenidate)Daytrana 15 mg/9-hour patch30 30(methylphenidate)Daytrana 20 mg/9-hour patch30 30(methylphenidate)Daytrana 30 mg/9-hour patch30 30(methylphenidate)Detrol LA 2 mg (tolterodine) 30 30Detrol LA 4 mg (tolterodine) 30 30Dexedrine 5 mg SR60 30(dextroamphetamine SR)Dexedrine 10 mg SR60 30(dextroamphetamine SR)Dexedrine 15 mg SR(dextroamphetamine SR)120 30Comments
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage67DateAugust 1, 2013Drug ProductQuantityDays’SupplyDexilant 30 mg (dexlansoprazole) 30 30Dexilant 60 mg (dexlansoprazole) 30 30Diastat (diazepem) 6 30Diazepam syringes 15 30syringesDiazepam intensol 5 mg/ml240 ml 30(diazepam)Diazepam oral solution 1 mg/ml 1200 ml 30(diazepam)Differin 0.1% cream (adapalene) 45 30Differin 0.1% gel (adapalene) 45 30Diovan 40 mg (valsartan) 30 30Diovan 80 mg (valsartan) 30 30Diovan 160 mg (valsartan) 30 30Diovan 320 mg (valsartan) 30 30Diovan HCT 80-12.5 mg30 30(valsartan/HCTZ)Diovan HCT 160-12.5 mg30 30(valsartan/HCTZ)Diovan HCT 160-25 mg30 30(valsartan/HCTZ)Diovan HCT 320-12.5 mg30 30(valsartan/HCTZ)Diovan HCT 320-25 mg30 30(valsartan/HCTZ)Ditropan XL 5 mg (oxybutynin ER) 30 30Ditropan XL 10 mg (oxybutynin ER) 60 30Ditropan XL 15 mg (oxybutynin ER) 60 30Doral 7.5 mg (quazepam) 30 30Doral 15 mg (quazepam) 30 30Duoneb 3 ml vial620 ml 30(albuterol/ipratropium)Edurant 25 mg (rilpivirine) 30 30Effexor XR 37.5 mg (venlafaxine) 30 30Effexor XR 75 mg (venlafaxine) 30 30Effexor XR 150 mg (venlafaxine) 90 30EMLA (lidocaine-prilocaine) 30 grams 30Emsam 6 mg/24-hour patch30 30(selegiline)Emsam 9 mg/24-hour patch30 30(selegiline)Emsam 12 mg/24-hour patch(selegiline)30 30Comments
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage68DateAugust 1, 2013Drug ProductQuantityDays’SupplyEnablex 7.5 mg (darifenacin) 30 30Enablex 15 mg (darifenacin) 30 30Epinephrine, racemic solution30 152.25% (racepinephrine)Epipen (epinephrine) 2 units 30Epipen, Jr (epinephrine) 2 units 30Estraderm (estradiol) 8 patches 30Exelon 1.5 mg (rivastigmine) 60 30Exelon 2 mg/ml oral solution180 ml 30(rivastigmine)Exelon 3 mg (rivastigmine) 60 30Exelon 4.5 mg (rivastigmine) 60 30Exelon 6 mg (rivastigmine) 60 30Fanapt 1 mg (iloperidone) 60 30Fanapt 2 mg (iloperidone) 60 30Fanapt 4 mg (iloperidone) 60 30Fanapt 6 mg (iloperidone) 60 30Fanapt 8 mg (iloperidone) 60 30Fanapt 10 mg (iloperidone) 60 30Fanapt 12 mg (iloperidone) 60 30Fioricet (butalbital-acetaminophencaffeine)360 30Fioricet/codeine (butalbitalacetaminophen-caffeine-codeine)180 30Flomax 0.4 mg (tamsulosin) 60 30Flonase (fluticasone propionate) 2 inhalers(32grams)30Flovent HFA 44 mcg (fluticasonepropionate)Flovent HFA 110 mcg (fluticasonepropionate)Flovent HFA 220 mcg (fluticasonepropionate)Focalin XR 5 mg(dexmethylphenidate)Focalin XR 10 mg(dexmethylphenidate)Focalin XR 15 mg(dexmethylphenidate)Focalin XR 20 mg(dexmethylphenidate)1 inhaler 30(10.6 gm)1 inhaler 30(12 gm)2 inhalers 30(24 gm)60 3060 3090 3060 30Comments
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage69DateAugust 1, 2013Drug ProductFocalin XR 25 mg(dexmethylphenidate)Focalin XR 30 mg(dexmethylphenidate)Focalin XR 35 mg(dexmethylphenidate)Focalin XR 40 mg(dexmethylphenidate)Days’Quantity Supply60 3060 3030 3030 30Foradil aerolizer (formoterol) 60 30Fosamax 5 mg (alendronate) 30 30Fosamax 10 mg (alendronate) 30 30Fosamax 40 mg(alendronate) 30 30Fosamax 70 mg (alendronate) 4 30Geodon 20 mg (ziprasidone) 60 30Geodon 40 mg (ziprasidone) 60 30Geodon 60 mg (ziprasidone) 60 30Geodon 80 mg (ziprasidone) 60 30Glucagen emergency kit (glucagon) 5 30Glucagon emergency kit 5 30Haldol decanoate 50 mg/ml-1 ml 1 ml 30vial (haloperidol decanoate)Haldol decanoate 50 mg/ml-5 ml 10 ml 30vial (haloperidol decanoate)Haldol decanoate 100 mg/ml-1 ml 1 ml 30vial (haloperidol decanoate)Haldol decanoate 100 mg/ml-5 ml 5 ml 30vial (haloperidol decanoate)Hycet solution (hydrocodone/ 3600 ml 30acetaminophen)Hytrin 1 mg (terazosin) 30 30Hytrin 2 mg (terazosin) 60 30Hytrin 5 mg (terazosin) 30 30Hytrin 10 mg (terazosin) 60 30Hyzaar 50-12.5 mg (HCTZ/losartan) 30 30Hyzaar 100-12.5 mg30 30(HCTZ/losartan)Hyzaar 100-25 mg (HCTZ/losartan) 30 30Innopran XL 80 mg (propranolol 30 30ER)Intal inhaler (cromolyn sodium) 3 inhalers(42.6 gm)30Comments
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage70DateAugust 1, 2013Drug ProductQuantityDays’SupplyCommentsIntuniv 1 mg (guanfacine ER) 30 30Intuniv 2 mg (guanfacine ER) 30 30Intuniv 3 mg (guanfacine ER) 30 30Intuniv 4 mg (guanfacine ER) 30 30Invega 3 mg (paliperidone) 30 30Invega 6 mg (paliperidone) 60 30Invega 9 mg (paliperidone) 30 30Invega Sustenna 39 mg syringe 1 syringe 30(paliperidone palmitate)Invega Sustenna 78 mg syringe 1 syringe 30(paliperidone palmitate)Invega Sustenna 117 mg syringe 1 syringe 30(paliperidone palmitate)Invega Sustenna 156 mg syringe 1 syringe 30(paliperidone palmitate)Invega Sustenna 234 mg syringe 1 syringe 30(paliperidone palmitate)Kalydeco (ivacaftor) 60 30Korlym (mifepristone) 120 30Latuda 20 mg (lurasidone) 30 30Latuda 40 mg (lurasidone) 30 30Latuda 80 mg (lurasidone) 60 30Latuda 120 mg (lurasidone) 30 30Lescol 20 mg (fluvastatin) 30 30Lexapro 5 mg (escitalopram) 15 30Lexapro 10 mg (escitalopram) 15 30Lexapro 20 mg (escitalopram) 60 30Lidoderm patch (lidocaine) 90 30 Maximum <strong>of</strong> 30 patchesallowed for initial fillLipitor 10 mg (atorvastatin) 30 30Lipitor 20 mg (atorvastatin) 30 30Lipitor 40 mg (atorvastatin) 45 30Liquicet (hydrocodone/2700 ml 30acetaminophen)Lorazepam intensol 2 mg/ml150 ml 30(lorazepam)Lorcet 10/650 mg (hydrocodone/ 180 30acetaminophen)Lorcet Plus (hydrocodone/acetaminophen)180 30
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage71DateAugust 1, 2013Drug ProductLortab elixir (hydrocodone/acetaminophen)Lortab 5/500 mg (hydrocodone/acetaminophen)Lortab 7.5/500 mg (hydrocodone/acetaminophen)Lortab 10/500 mg (hydrocodone/acetaminophen)Days’Quantity Supply2700 ml 30240 30180 30180 30Lunesta 1 mg (eszopiclone) 30 30Lunesta 2 mg (eszopiclone) 30 30Lunesta 3 mg (eszopiclone) 30 30Luvox 25 mg (fluvoxamine) 30 30Luvox 50 mg (fluvoxamine) 30 30Lyrica 25 mg (pregabalin) 90 30Lyrica 50 mg (pregabalin) 90 30Lyrica 75 mg (pregabalin) 90 30Lyrica 100 mg (pregabalin) 90 30Lyrica 150 mg (pregabalin) 90 30Lyrica 200 mg (pregabalin) 90 30Lyrica 225 mg (pregabalin) 60 30Lyrica 300 mg (pregabalin) 60 30Mavik 1 mg (trandolapril) 30 30Mavik 2 mg (trandolapril) 30 30Mavik 4 mg (trandolapril) 60 30Maxair autoinhaler 14 g (pirbuterolacetate)Maxidone (hydrocodone/acetaminophen)Metadate CD 10 mg(methylphenidate ER)Metadate CD 20 mg(methylphenidate ER)Metadate CD 30 mg(methylphenidate ER)Metadate CD 40 mg(methylphenidate ER)Metadate CD 50 mg(methylphenidate ER)Metadate CD 60 mg(methylphenidate ER)2 inhalers 30(28 gm)150 3060 3090 3060 3060 3060 3060 30Metadate ER 10 mg (methylin ER) 90 30Metadate ER 20 mg (methylin ER) 90 30Comments
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage72DateAugust 1, 2013Drug ProductMetrogel vaginal (metronidazolevaginal gel 0.75%)Days’Quantity Supply70 gm 30Mevacor 10 mg (lovastatin) 30 30Mevacor 20 mg (lovastatin) 30 30Mevacor 40 mg (lovastatin) 60 30Miacalcin nasal 200 U/dose4 ml 30(calcitonin)Mobic 7.5 mg (meloxicam) 30 30Mobic 15 mg (meloxicam) 30 30Monopril 10 mg (fosinopril) 60 30Monopril 20 mg (fosinopril) 60 30Monopril 40 mg (fosinopril) 60 30Mscontin 15 mg (morphine sulfate 90 30SA)Mscontin 30 mg (morphine sulfate 90 30SA)Mscontin 60 mg (morphine sulfate 90 30SA)Mscontin 100 mg (morphine sulfateSA)300 30Namenda 2 mg/1 ml oral solution(memantine)Namenda 5 mg (memantine) 60 30Namenda 10 mg (memantine) 60 30Nasacort AQ (triamcinoloneacetonide)Nasarel (flunisolide)Nasonex 50 mcg nasal spray(mometasone furoate)Comments300 ml 30 Comes in 360 mlcontainers2 bottles(33 gm)3 bottles(75 ml)2 bottles(34 gm)Nexium 20 mg (esomeprazole) 30 30Nexium 40 mg (esomeprazole) 60 30Niaspan 500 mg (niacin) 30 30Niaspan 750 mg (niacin) 60 30Niaspan 1000 mg (niacin) 60 30Norco 5/325 mg (hydrocodone/ 360 30acetaminophen)Norco 7.5/325 mg (hydrocodone/ 240 30acetaminophen)Norco 10/325 mg (hydrocodone/acetaminophen)180 30303030
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage73DateAugust 1, 2013Drug ProductQuantityDays’SupplyNorvasc 2.5 mg (amlodipine) 30 30Norvasc 5 mg (amlodipine) 30 30Nucynta 50 mg (tapentadol) 180 30Nucynta 75 mg (tapentadol) 180 30Nucynta 100 mg (tapentadol) 180 30Onfi 5 mg (clobazam) 60 30Onfi 10 mg (clobazam) 60 30Onfi 20 mg (clobazam) 60 30Opana ER 5 mg (oxymorphone) 60 30Opana ER 7.5 mg (oxymorphone) 60 30Opana ER 10 mg (oxymorphone) 60 30Opana ER 15 mg (oxymorphone) 60 30Opana ER 20 mg (oxymorphone) 60 30Opana ER 30 mg (oxymorphone) 60 30Panlor SS (acetaminophencaffeine-dihyrdocodeine)150 30Paxil 10 mg (paroxetine) 30 30Paxil 20 mg (paroxetine) 30 30Paxil 30 mg (paroxetine) 30 30Paxil 40 mg (paroxetine) 45 30Paxil CR 12.5 mg (paroxetine ER) 30 30Paxil CR 25 mg (paroxetine ER) 60 30Paxil CR 37.5 mg (paroxetine ER) 60 30Pegasys kit (peginterferon1 28alpha-2a)Pegasys syringe (peginterferon 4 ml 28alpha-2a)Percocet 5/325 mg (oxycodone/ 360 30acetaminophen)Percocet 7.5/325 mg (oxycodone/ 240 30acetaminophen)Percocet 7.5/500 mg (oxycodone/ 240 30acetaminophen)Percocet 10/325 mg (oxycodone/ 180 30acetaminophen)Percocet 10/650 mg (oxycodone/ 180 30acetaminophen)Pravachol 10 mg (pravastatin) 30 30Pravachol 20 mg (pravastatin) 30 30Pravachol 40 mg (pravastatin) 30 30Pravachol 80 mg (pravastatin) 30 30Comments
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage74DateAugust 1, 2013Drug ProductPremarin 0.625 mg (conjugatedestrogens)Premarin vaginal cream(conjugated estrogens)Days’Quantity Supply30 301 tube(42.5 gm)30CommentsPrevacid 15 mg (lansoprazole) 30 30 Prior authorizationrequired for more than60 days <strong>of</strong> PPI therapyPrevacid 30 mg (lansoprazole) 30 30 Prior authorizationrequired for more than60 days <strong>of</strong> PPI therapyPrevacid SoluTabs 15 mg30 30(lansoprazole)Prevacid SoluTabs 30 mg30 30(lansoprazole)Prilosec 10 mg (omeprazole) 30 30Prilosec 20 mg (omeprazole) 30 30Prilosec 40 mg (omeprazole) 30 30Pristiq 50 mg (desvenlafaxine) 30 30Pristiq 100 mg (desvenlafaxine) 30 30Proair HFA 8.5 gm (albuterol) 3 inhalers 30(25.5 gm)Procardia XL 30 mg (nifedipine ER) 30 30Procardia XL 60 mg (nifedipine ER) 30 30Procardia XL 90 mg (nifedipine ER) 30 30Procentra 5 mg/5 ml1800 ml 30(dextroamphetamine)Prosom 1 mg (estazolam) 30 30Prosom 2 mg (estazolam) 30 30Protonix 20 mg (pantoprazole) 30 30 Prior authorizationrequired for more than60 days <strong>of</strong> PPI therapyProtonix 40 mg (pantoprazole) 30 30 Prior authorizationrequired for more than60 days <strong>of</strong> PPI therapyProvigil 100 mg (modafinil) 30 30Provigil 200 mg (modafinil) 60 30Prozac 20 mg/5 ml solution600 ml 30(fluoxetine)Prozac 10 mg tablet (fluoxetine) 45 30Prozac 10 mg capsule (fluoxetine) 30 30Prozac 20 mg (fluoxetine) 120 30Prozac 40 mg (fluoxetine) 60 30
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage75DateAugust 1, 2013Drug ProductPulmicort flexhaler 180 mcg/dose(budesonide)Qvar 40 mcg (beclomethasonedipropionate)Qvar 80 mcg (beclomethasonedipropionate)Days’Quantity Supply2 303 inhalers(21.9 gm)3 inhalers(21.9 gm)Remeron 15 mg (mirtazapine) 45 30Remeron 30 mg (mirtazapine) 30 30Remeron 45 mg (mirtazapine) 30 30Remeron SolTab 15 mg45 30(mirtazapine ODT)Remeron SolTab 30 mg30 30(mirtazapine ODT)Remeron SolTab 45 mg30 30(mirtazapine ODT)Restoril 7.5 mg (temazepam) 30 30Restoril 15 mg (temazepam) 30 30Restoril 22.5 mg (temazepam) 30 30Restoril 30 mg (temazepam) 30 30Revlimid 2.5 mg (lenalidomide) 30 30Revlimid 5 mg (lenalidomide) 30 30Revlimid 10 mg (lenalidomide) 60 30Revlimid 15 mg (lenalidomide) 30 30Revlimid 25 mg (lenalidomide) 30 30Rhinocort aqua sus (budesonide) 8.6 gm 30Risperdal 0.5 mg M-tab120 30(risperidone)Risperdal 1 mg M-tab (risperidone) 120 30Risperdal 2 mg M-TAB90 30(risperidone)Risperdal 3 mg M-TAB60 30(risperidone)Risperdal 4 mg M-TAB60 30(risperidone)Risperdal Consta 12.5 mg syringe 2 syringes 28(risperidone)Risperdal Consta 25 mg syringe 2 syringes 28(risperidone)Risperdal Consta 37.5 mg syringe 2 syringes 28(risperidone)Risperdal Consta 50 mg syringe(risperidone)2 syringes 283030Comments
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage76DateAugust 1, 2013Drug ProductQuantityDays’SupplyRisperdal 0.25 mg (risperidone) 120 30Risperdal 0.5 mg (risperidone) 120 30Risperdal 1 mg (risperidone) 120 30Risperidal 2 mg (risperidone) 90 30Risperidal 3 mg (risperidone) 60 30Risperidal 4 mg (risperidone) 60 30Ritalin LA 10 mg (methylphenidate 30 30ER)Ritalin LA 20 mg (methylphenidate 30 30ER)Ritalin LA 30 mg (methylphenidate 60 30ER)Ritalin LA 40 mg (methylphenidate 30 30ER)Ritalin SR 20 mg (methylphenidate 90 30ER)Robinul 1 mg (glycopyrrolate) 90 30Robinul Forte 2 mg (glycopyrrolate) 120 30Robitussin DM Syrup(dextromethorphan-guaifenesin10-100 mg/5 ml)Rozerem 8 mg (ramelteon) 30 30Ryzolt 100 mg (tramadol ER) 30 30Ryzolt 200 mg (tramadol ER) 30 30Ryzolt 300 mg (tramadol ER) 30 30Saphris 5 mg (asenapine) 60 30Saphris 10 mg (asenapine) 60 30Savella 12.5 mg (milnacipran) 60 30Savella 25 mg (milnacipran) 60 30Savella 50 mg (milnacipran) 60 30Savella 100 mg (milnacipran) 60 30Serax 10 mg (oxazepam) 120 30Serax 15 mg (oxazepam) 120 30Serax 30 mg (oxazepam) 120 30Serevent diskus 60 blisters(salmeterol)Comments240 ml 30 Allowed for acumulative 90 days per12 month period1 package(60)Seroquel 25 mg (quetiapine) 90 30Seroquel 50 mg (quetiapine) 90 30Seroquel 100 mg (quetiapine) 90 30Seroquel 200 mg (quetiapine) 90 30Seroquel 300 mg (quetiapine) 60 30Seroquel 400 mg (quetiapine) 60 3030
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage77DateAugust 1, 2013Drug ProductSingulair 4 mg granules(montelukast)Singulair 4 mg chew tablets(montelukast)Singulair 5 mg chew tablets(montelukast)Singulair 10 mg tablets(montelukast)Days’Quantity Supply30 3030 3030 3030 30CommentsSoma 350 mg (carisoprodol) 120 30Sonata 5 mg (zaleplon) 30 30Sonata 10 mg (zaleplon) 60 30Spiriva cap handihaler pkg size 30 30 30(tiotropium bromide)Strattera 10 mg (atomoxetine) 60 30Strattera 18 mg (atomoxetine) 60 30Strattera 25 mg (atomoxetine) 60 30Strattera 40 mg (atomoxetine) 60 30Strattera 60 mg (atomoxetine) 30 30Strattera 80 mg (atomoxetine) 30 30Strattera 100 mg (atomoxetine) 30 30Stribild (elvitegravir/cobicistat/30 30emtricitabine/ten<strong>of</strong>ovir/disoproxilfumarate)Sudafed 30 mg (pseudoephedrine) 72 30 Allowed for acumulative 90 days per12 month periodSudafed 60 mg (pseudoephedrine) 72 30 Allowed for acumulative 90 days per12 month periodSudafed 30 mg/5 ml(pseudoephedrine)Sutent 12.5 mg (sunitinib) 90 30Sutent 25 mg (sunitinib) 30 30Sutent 50 mg (sunitinib) 30 30Talacen (pentazocine/180 30acetaminophen)Tenex 1 mg (guanfacine) 90 30Tenex 2 mg (guanfacine) 90 30Terazol 3 (terconazole vaginal 20 gm 30cream 0.8%)Terazol 7 (terconazole vaginalcream 0.4%)45 gm 30240 ml 30 Allowed for acumulative 90 days per12 month period
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage78DateAugust 1, 2013Drug ProductTilade inhaler (nedocromil sodium)Timoptic ophthalmic solution 0.25%(timolol)Timoptic ophthalmic solution 0.5%(timolol)Timoptic-XE 0.25% (timolol gelforming)Timoptic-XE 0.5% (timolol gelforming)Days’Quantity Supply3 inhalers 30(48.6 gm)15 ml 3015 ml 3015 ml 3015 ml 30Topamax 25 mg (topiramate) 60 30Topamax 50 mg (topiramate) 60 30Topamax 100 mg (topiramate) 60 30Toprol XL 25 mg (metoprolo ER) 45 30Toprol XL 50 mg (metoprolol ER) 45 30Toprol XL 100 mg (metoprolo ER) 45 30Toprol XL 200 mg (metoprolol ER) 60 30Toviaz 4 mg (fesoterodine) 30 30Toviaz 8 mg (fesoterodine) 30 30Transderm Scop 1.5mg10 30(scopolamine)Travatan Z (travoprost) 5 ml 30Tricor 48 mg (fen<strong>of</strong>ibrate) 30 30Tricor 145 mg (fen<strong>of</strong>ibrate) 30 30Triglide 160 mg (fen<strong>of</strong>ibrate) 30 30Twinject (epinephrine) 4 units 30Tylenol w/ codeine elixir2700 ml 30(acetaminophen/codeine)Tylenol with codeine No. 2390 30(acetaminophen/codeine)Tylenol wth codeine No. 3390 30(acetaminophen/codeine)Tylenol wth codeine No. 4390 30(acetaminophen/codeine)Uloric 40 mg (febuxostat) 30 30Ultracet (tramadol/apap) 240 30Ultram 50 mg (tramadol) 240 30Ultram ER 100 mg (tramadol ER) 30 30Ultram ER 200 mg (tramadol ER) 30 30Ultram ER 300 mg (tramadol ER) 30 30Uroxatral (alfuzosin) 30 30Comments
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage79DateAugust 1, 2013Drug ProductQuantityDays’SupplyCommentsValium 2 mg (diazepam) 120 30Valium 5 mg (diazepam) 120 30Valium 10 mg (diazepam) 120 30Valturna 150-160 mg (aliskiren/30 30valsartan)Valturna 300-320 mg (aliskiren/30 30valsartan)Venlafaxine ER 37.5 mg tablet 30 30Venlafaxine ER 75 mg tablet 30 30Venlafaxine ER 150 mg tablet 60 30Venlafaxine ER 225 mg tablet 60 30Veregen (sinecatechins) 15 gm 28 Max 60 gm/16 weeksVicodin 5/500 mg (hydrocodone/ 240 30acetaminophen)Vicodin ES (hydrocodone/150 30acetaminophen)Vicodin HP (hydrocodone/180 30acetaminophen)Vigamox (moxifloxacin) 6 ml 30Viibryd 10 mg (vilazodone) 30 30Viibryd 20 mg (vilazodone) 30 30Viibryd 40 mg (vilazodone) 30 30Vivelle/Vivelle-DOT (estradiol) 8 patches 28Vyvanse 20 mg (lisdexamfetamine) 30 30Vyvanse 30 mg (lisdexamfetamine) 30 30Vyvanse 40 mg (lisdexamfetamine) 30 30Vyvanse 50 mg (lisdexamfetamine) 30 30Vyvanse 60 mg (lisdexamfetamine) 30 30Vyvanse 70 mg (lisdexamfetamine) 30 30Wellbutrin 75 mg (bupropion) 180 30Wellbutrin 100 mg (bupropion) 90 30Wellbutrin SR 100 mg (bupropion 60 30SR)Wellbutrin SR 150 mg (bupropion 60 30SR)Wellbutrin SR 200 mg (bupropion 60 30SR)Wellbutrin XL 150 mg(bupropion 30 30ER)Wellbutrin XL 300 mg (bupropionER)30 30
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage80DateAugust 1, 2013Drug ProductQuantityDays’SupplyXalatan (latanoprost) 5 ml 30Xalkori 200 mg (crizotinib) 60 30Xalkori 250 mg (crizotinib) 60 30Xanax 0.25 mg (alprazolam) 150 30Xanax 0.5 mg (alprazolam) 150 30Xanax 1 mg (alprazolam) 150 30Xanax 2 mg (alprazolam) 150 30Xanax XR 0.5 mg (alprazolam ER) 30 30Xanax XR 1 mg (alprazolam ER) 30 30Xodol 5/300 mg (hydrocodone/ 360 30acetaminophen)Xodol 7.5/300 mg (hydrocodone/ 180 30acetaminophen)Xodol 10/300 mg (hydrocodone/ 180 30acetaminophen)Xolair sol 150 mg (omalizumab) 6 30Xyrem 500 mg/ml (sodium oxybate) 540 ml 30Zamicet (hydrocodone/2700 ml 30acetaminophen)Zavesca (miglustat) 90 30Zebeta 5 mg (bisoprolol) 30 30Zelboraf 250 mg (vemurafenib) 240 30Zetia 10 mg (ezetimibe) 30 30Zocor 5 mg (simvastatin) 30 30Zocor 10 mg (simvastatin) 30 30Zocor 20 mg (simvastatin) 30 30Zocor 40 mg(simvastatin) 30 30Zol<strong>of</strong>t 50 mg (sertraline) 45 30Zonalon 5% cream (doxepin) 45 m 30Zovirax 5% ointment (acyclovir) 30 gm 30Zydone 5/400 mg (hydrocodone/ 240 30acetaminophen)Zydone 7.5/400 mg (hydrocodone/ 240 30acetaminophen)Zydone 10/400 mg (hydrocodone/ 180 30acetaminophen)Zyprexa 2.5 mg (olanzapine) 30 30Zyprexa 5 mg (olanzapine) 30 30Zyprexa 7.5 mg (olanzapine) 30 30Zyprexa 10 mg (olanzapine) 30 30Comments
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage81DateAugust 1, 2013Drug ProductQuantityDays’SupplyZyprexa 15 mg (olanzapine) 60 30Zyprexa 20 mg (olanzapine) 60 30Zyprexa Zydis 5 mg (olanzapine) 30 30Zyprexa Zydis 10 mg (olanzapine) 30 30Zyprexa Zydis 15 mg (olanzapine) 60 30Zyprexa Zydis 20 mg (olanzapine) 60 30Zyrtec 1 mg/ml liquid OTC300 30(cetirizine)Zyrtec 5 mg tablet OTC (cetirizine) 30 30Zyrtec 10 mg tablet OTC (cetirizine) 30 30Comments63. R<strong>of</strong>lumilast (Daliresp)Prior authorization is required for r<strong>of</strong>lumilast (Daliresp ). Payment will beconsidered for patients 18 years <strong>of</strong> age or older when the following is met:♦ A diagnosis <strong>of</strong> severe COPD with chronic bronchitis as documented byspirometry results, and♦ A smoking history <strong>of</strong> ≥ 20 pack-years, and♦ Currently on a long-acting bronchodilator in combination with an inhaledcorticosteroid with documentation <strong>of</strong> inadequate control <strong>of</strong> symptoms, and♦ A history <strong>of</strong> at least one exacerbation in the past year requiring treatmentwith oral glucocorticosteroids.The required trials may be overridden when documented evidence is providedthat the use <strong>of</strong> these agents would be medically contraindicated.Use form 470-5085, Request for Prior Authorization: R<strong>of</strong>lumilast(Daliresp), to request prior authorization. Click here to see a sample <strong>of</strong> theform.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage82DateAugust 1, 201364. Sedative/Hypnotics-Non-BenzodiazepinePreferred agents are available without prior authorization (PA). Althoughintermittent therapy is recommended, quantity limits will allow for 30 tabletsper 30 days supply without PA for preferred medications.Prior authorization is required for all nonpreferred nonbenzodiazepinesedative/hypnotics. Payment for nonpreferred nonbenzodiazepinesedative/hypnotics will be authorized only for cases in which there isdocumentation <strong>of</strong> a previous trial and therapy failure with the preferredagents. Payment for nonpreferred nonbenzodiazepine sedative/hypnotics willbe considered when there is:♦ A diagnosis <strong>of</strong> insomnia.♦ Medications with a side effect <strong>of</strong> insomnia (i.e., stimulants) are decreasedin dose, changed to a short-acting product, or discontinued.♦ Enforcement <strong>of</strong> good sleep hygiene is documented.♦ All medical, neurological, and psychiatric disease states causing chronicinsomnia are being adequately treated with appropriate medication attherapeutic doses.♦ A documented trial and therapy failure with zaleplon.Use form 470-4328, Request for Prior Authorization: Sedative/Hypnotics-Non-Benzodiazepine, to request prior authorization. Click here to see asample <strong>of</strong> the form.65. Selected Brand-Name <strong>Drugs</strong>Prior authorization is required for selected brand-name drugs, as determinedby the <strong>Department</strong>, for which there is available an “A” rated bioequivalentgeneric product, as determined by the federal Food and Drug Administration,unless the brand drug has been designated by the <strong>Department</strong> as preferred(payable) under the <strong>Iowa</strong> Medicaid Preferred Drug List.The list <strong>of</strong> selected brand-name drugs includes the drugs on the FederalUpper Limit (FUL) list at http://www.mslciowa.com/AAC.htm.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage83DateAugust 1, 2013For prior authorization to be considered, the prescriber must submit acompleted Selected Brand Name <strong>Drugs</strong> PA form and <strong>Iowa</strong> Medicaid MedWatchform with:♦ Documentation <strong>of</strong> trials and therapy failures with two different genericmanufacturers <strong>of</strong> the same chemical entity. If an allergy to an inactivecomponent is suspected, the second trial must be with a generic productthat does not contain the allergen, if available.♦ Documentation <strong>of</strong> the failure must include the specific adverse reaction asdefined by the FDA. (See Section B <strong>of</strong> the MedWatch form).Intolerances, such as nausea and vomiting, to the generic drugs will notbe considered as a basis for approval.Trials may be overridden when evidence is provided that use <strong>of</strong> the genericproduct would be medically contraindicated.Use forms 470-5039 and 470-4119, Request for Prior Authorization:Selected Brand Name <strong>Drugs</strong>, to request prior authorization. Click here to seea sample <strong>of</strong> form 470-5039. Click here to see a sample <strong>of</strong> form 470-4119.66. Serotonin 5-HT1 Receptor AgonistsPrior authorization is required for serotonin 5-HT1 receptor agonists forquantities exceeding 12 unit doses <strong>of</strong> tablets, syringes, or sprays per 30days. Payment for serotonin 5-HT1 receptor agonists beyond this limit will beconsidered on an individual basis after review <strong>of</strong> submitted documentation.Prior authorization is required for all nonpreferred serotonin 5-HT1 receptoragonists beginning the first day <strong>of</strong> therapy. Payment for nonpreferredserotonin 5-HT1 receptor agonists will be authorized only for cases in whichthere is documentation <strong>of</strong> previous trials and therapy failures with twopreferred agents.Requests for nonpreferred combination products may be considered onlyafter documented separate trials and therapy failures with the individualingredients.For consideration, the following information must be supplied:♦ The diagnosis requiring therapy.♦ Documentation <strong>of</strong> current prophylactic therapy or documentation <strong>of</strong>previous trials and therapy failures with two different prophylacticmedications.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage84DateAugust 1, 2013Use form 470-4113, Request for Prior Authorization: Serotonin 5-HT1Receptor Agonists, to request prior authorization. Click here to see a sample<strong>of</strong> the form.67. Short-Acting NarcoticsPrior authorization is required for all nonpreferred short-acting narcotics.Payment will be considered for cases in which there is documentation <strong>of</strong>previous trial and therapy failures with three chemically distinct preferredshort-acting narcotics (based on narcotic ingredient only) at therapeuticdoses, unless evidence is provided that use <strong>of</strong> these products would bemedically contraindicated.Use form 470-4899, Request for Prior Authorization: Short Acting Narcotics,to request prior authorization. Click here to see a sample <strong>of</strong> the form.68. Smoking Cessation Therapy-OralPrior authorization is required for varenicline (Chantix) or bupropion SRthat is FDA approved for smoking cessation. Requests for authorization mustinclude:♦ Diagnosis <strong>of</strong> nicotine dependence and referral to the Quitline <strong>Iowa</strong>program for counseling.♦ Confirmation <strong>of</strong> enrollment and ongoing participation in the Quitline <strong>Iowa</strong>counseling program is required for approval and continued coverage.Approvals will be granted only for patients 18 years <strong>of</strong> age or older.♦ The duration <strong>of</strong> therapy is initially limited to 12 weeks within a 12-monthperiod.♦ For patients who have successfully stopped smoking at the end <strong>of</strong> 12weeks, an additional course <strong>of</strong> 12 weeks treatment will be considered witha prior authorization request. The maximum duration <strong>of</strong> approvabletherapy is 24 weeks within a 12-month period.♦ Requests for varenicline to be used in combination with bupropion SR thatis FDA-indicated for smoking cessation or nicotine replacement therapywill not be approved.♦ The 72-hour emergency supply rule does not apply for drugs used for thetreatment <strong>of</strong> smoking cessation.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage85DateAugust 1, 2013Use form 470-4517, Request for Prior Authorization: Smoking CessationTherapy-Oral, to request prior authorization. Click here to see a sample <strong>of</strong>the form.69. Sodium Oxybate (Xyrem ® )Prior authorization is required for sodium oxybate (Xyrem ® ). Payment will beconsidered for patients 16 years <strong>of</strong> age or older under the followingconditions:♦ A diagnosis <strong>of</strong> cataplexy associated with narcolepsy verified by a recentsleep study (including a PSG, MSLT, and ESS0 and previous trial andtherapy failure at a therapeutic dose with one <strong>of</strong> the following tricyclicantidepressants: clomipramine, imipramine, or protriptyline.♦ A diagnosis <strong>of</strong> excessive daytime sleepiness associated with narcolepsyverified by a recent sleep study (including a PSG, MSLT, and ESS) andprevious trials and therapy failures at a therapeutic dose with a preferredamphetamine and non-amphetamine stimulant.Requests for patients with a prior history <strong>of</strong> substance abuse, concurrent usewith a sedative hypnotic, or a semialdehyde dehydrogenase deficiency willnot be considered.The required trials may be overridden when documented evidence is providedthat the use <strong>of</strong> these agents would be medically contraindicated.Use form 470-5016, Request for Prior Authorization: Sodium Oxybate(Xyrem ® ), to request prior authorization. Click here to see a sample <strong>of</strong> theform.70. Thrombopoietin Receptor AgonistsPayment for a preferred thrombopoietin receptor agonist will be consideredonly for cases in which there is a diagnosis <strong>of</strong> chronic immunethrombocytopenic purpura (ITP) including documentation <strong>of</strong> an insufficientresponse to a corticosteroid or an immunoglobulin, or the member hasundergone splenectomy.Payment for a nonpreferred thrombopoietin receptor agonist will beconsidered following documentation <strong>of</strong> a recent trial and therapy failure witha preferred thrombopoietin receptor agonist unless such a trial would bemedically contraindicated.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage86DateAugust 1, 2013Use form 470-4850, Request for Prior Authorization: ThrombopoietinReceptor Agonists, to request prior authorization. Click here to see a sample<strong>of</strong> the form.71. Topical RetinoidsPrior authorization is required for all prescription topical retinoid products.Payment for prescription topical retinoid products will be considered underthe following conditions:♦ Patients with a diagnosis <strong>of</strong> skin cancer, lamellar ichthyosis, or Darier’sdisease will receive automatic approval for lifetime use <strong>of</strong> topical retinoidproducts.♦ Payment will be authorized when the patient has had previous trial andtherapy failure with:• A preferred over-the-counter benzoyl peroxide product, and• Two preferred topical or oral antibiotics for the treatment <strong>of</strong> mild tomoderate acne (noninflammatory and inflammatory) or drug-inducedacne.EXCEPTION: Trials and therapy failure are not required for patientspresenting with a preponderance <strong>of</strong> comedonal acne.♦ Payment for nonpreferred topical retinoid products will be authorized onlyfor cases in which there is documentation <strong>of</strong> previous trial and therapyfailure with a preferred agent.♦ Requests for nonpreferred combination products wil be considered onlyafter documentation <strong>of</strong> separate trials and therapy failures with theindividual ingredients.♦ Trial and therapy failure with a preferred topical antipsoriatic agent willnot be required for tazorac for a psoriasis diagnosis.The required trials may be overridden when documented evidence is providedthat the use <strong>of</strong> these agents would be medically contraindicated.Use form 470-4114, Request for Prior Authorization: Topical Retinoids forAcne, to request prior authorization. Click here to see a sample <strong>of</strong> the form.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage87DateAugust 1, 201372. Vemurafenib (Zelboraf)Prior authorization is required for vemurafenib (Zelboraf). Payment will beconsidered for patients when the following criteria are met:♦ Patient is 18 years <strong>of</strong> age or older; and♦ Has a diagnosis <strong>of</strong> unresectable or metastatic melanoma with BRAFV600Emutation as detected by an FDA-approved test; and♦ Prescriber is an oncologist.If the criteria for coverage are met, authorizations will be given at threemonth intervals. Updates on disease progression must be provided with eachrenewal request. If disease progression is noted, therapy will not becontinued.Use form 470-5136, Request for Prior Authorization: Vemurafenib(Zelboraf), to request prior authorization. Click here to see a sample <strong>of</strong> theform.73. Vilazodone (Viibryd )Prior authorization is required for Viibryd . Requests for doses above themanufacturer recommended dose will not be considered. Payment will beconsidered for patients when the following criteria are met:♦ The patient has a diagnosis <strong>of</strong> Major Depressive Disorder (MDD) and is 18years <strong>of</strong> age and older; and♦ Documentation <strong>of</strong> a previous trial and therapy failure at a therapeuticdose with one preferred generic SSRI; and♦ Documentation <strong>of</strong> a previous trial and therapy failure at a therapeuticdose with one preferred generic SNRI; and♦ Documentation <strong>of</strong> a previous trial and therapy failure at a therapeuticdose with an additional generic antidepressant from any class.The required trials may be overridden when documented evidence is providedthat the use <strong>of</strong> these agents would be medically contraindicated.Use form 470-5098, Request for Prior Authorization: Vilazodone (Viibryd ),to request prior authorization. Click here to see a sample <strong>of</strong> the form.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage88DateAugust 1, 201374. Vitamins, Minerals and Multiple VitaminsPayment for vitamins, minerals, and multiple vitamins for treatment <strong>of</strong>specific conditions will be approved when:♦ A specific vitamin or mineral deficiency disease is diagnosed; or♦ A member aged 20 or under has a diagnosed disease that inhibits thenutrition absorption process as a secondary effect <strong>of</strong> the disease.Prior approval is not required for prescribed multi-vitamins with or withoutiron or vitamin D supplements for patients under 12 months <strong>of</strong> age or aprescription product primarily classified as a blood modifier if that productdoes not contain more than three vitamins and minerals, or for productsprincipally marketed as prenatal vitamin-mineral supplements.Prior authorization is not required for a vitamin and mineral productprincipally marketed for use as a dietary supplement during pregnancy andlactation.Use form 470-4115, Request for Prior Authorization: Vitamins & Minerals, torequest prior authorization. Click here to see a sample <strong>of</strong> the form.75. Vusion OintmentPrior authorization is required for Vusion ointment. Payment will beconsidered only for cases in which there is documentation <strong>of</strong> previous trialsand therapy failures with (1) over-the-counter miconazole 2% cream(payable with a prescription) and (2) nystatin cream or ointment, unlessevidence is provided that use <strong>of</strong> these agents would be medicallycontraindicated.Use form 470-4655, Request for Prior Authorization: Vusion Ointment, torequest prior authorization. Click here to see a sample <strong>of</strong> the form.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage89DateAugust 1, 2013D. BASIS OF PAYMENT FOR DRUGS AND SUPPLIESThe amount <strong>of</strong> payment for drugs and supplies is based on several factors, inaccordance with 441 IAC 79.1(8) and upper limits in 42 CFR 447.500 to 447.520.340B actual acquisition cost (340B AAC) means the net cost <strong>of</strong> a drug paid bya pharmacy for drugs purchased through the 340B drug pricing program. A drug’s340B AAC includes discounts, rebates, chargebacks, and other adjustments to theprice <strong>of</strong> the drug, but excludes dispensing fees.Average actual acquisition cost (average AAC) is defined as retailpharmacies’ average prices paid to acquire drug products.♦ Average AAC is determined by the <strong>Department</strong> based on a survey <strong>of</strong> invoiceprices paid by <strong>Iowa</strong> Medicaid retail pharmacies.♦ Surveys are conducted at least once every six months, or more <strong>of</strong>ten at the<strong>Department</strong>’s discretion.♦ The average AAC is calculated as a statistical mean based on one reported costper drug per pharmacy. The average AAC determined by the <strong>Department</strong> ispublished on the <strong>Iowa</strong> Medicaid Enterprise website.♦ If no current average AAC has been determined for a drug, the wholesaleacquisition cost (WAC) published by Medi-Span is used.Federal upper limit (FUL) is defined as the upper limit for multiple-source drugsestablished in accordance with the methodology <strong>of</strong> the Centers for Medicare andMedicaid Services, as described in 42 CFR 447.514.For drugs with no established FUL, the <strong>Department</strong> determines the allowableaverage actual acquisition cost in accordance with the provisions <strong>of</strong> federal drugregulation 42 CFR 447.512. This basis <strong>of</strong> payment is also applicable tocompounded prescriptions.Pr<strong>of</strong>essional dispensing fee is added to the ingredient cost to cover thepharmacist’s pr<strong>of</strong>essional services and costs associated with transferring the drugto a Medicaid member. The dispensing fee is set based on cost <strong>of</strong> dispensingsurveys <strong>of</strong> <strong>Iowa</strong> Medicaid participating pharmacies.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage90DateAugust 1, 20131. Reimbursement Effective February 1, 2013The Medicaid program relies on information published by Medi-Span toclassify drugs as brand or generic.a. Generic and Nonprescription <strong>Drugs</strong>For covered generic prescription drugs and for coverednonprescription drugs shall be the lowest <strong>of</strong> the following, as <strong>of</strong> thedate <strong>of</strong> dispensing:♦ Average actual acquisition cost (average AAC) plus the pr<strong>of</strong>essionaldispensing fee.♦ The federal upper limit (FUL) plus the pr<strong>of</strong>essional dispensing fee.♦ The submitted charge, representing the provider’s usual andcustomary charge for the drug.b. Brand-Name <strong>Drugs</strong>For covered brand-name prescription drugs shall be the lowest <strong>of</strong> thefollowing, as <strong>of</strong> the date <strong>of</strong> dispensing:♦ Average actual acquisition cost (average AAC) plus the pr<strong>of</strong>essionaldispensing fee.♦ The submitted charge, representing the provider’s usual andcustomary charge for the drug.2. <strong>Drugs</strong> Subject to Federal Upper Limit (FUL)a. FUL DevelopmentThe Centers for Medicare and Medicaid Services (CMS) establishesfederal upper limits (FUL) for reimbursement for multiple-source drugs.These reimbursement levels are updated periodically and are availableon the Centers for Medicare and Medicaid Services web page athttp://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Benefits/Prescription-<strong>Drugs</strong>/Prescription-<strong>Drugs</strong>.html.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage91DateAugust 1, 2013b. Reimbursement for FUL <strong>Drugs</strong>For the drug groups on the Preferred Drug List where brand-nameproducts are preferred over generic products, the FUL rate will continueto apply when the generic version <strong>of</strong> the drug is dispensed.However, the payment for preferred brand name products (which nolonger require prior authorization before dispensing) equals the lower <strong>of</strong>the average acquisition cost (average AAC) or the submitted charges, asopposed to the FUL/SMAC rate.Nonpreferred brand products require prior authorization beforedispensing. If authorized, payment equals the lower <strong>of</strong> the the averageacquisition cost (average AAC) or the submitted charges, as opposed tothe FUL rate with a prior authorization. The DAW=1 is no longerrequired for brand reimbursement.Prior authorization is required for selected brand-name drugs asdetermined by the <strong>Department</strong> for which there is available, an “A” ratedbioequivalent generic product as determined by the federal Food andDrug Administration.For prior authorization to be considered, evidence <strong>of</strong> a treatment failurewith the bioequivalent generic drug must be provided. A copy <strong>of</strong> acompleted form 470-4119, Request for Prior Authorization: SelectedBrand Name <strong>Drugs</strong>, shall be considered as evidence <strong>of</strong> treatment failure.The list <strong>of</strong> selected brand-name drugs includes the drugs on the FederalUpper Limit (FUL) list at http://mslciowa.com/AAC.htm. Priorauthorization is not required for brand name drugs that have beendesignated by the <strong>Department</strong> as preferred (payable) under the <strong>Iowa</strong>Medicaid Preferred Drug List (PDL).3. Reimbursement for Unit-Dose PackagingAdditional reimbursement <strong>of</strong> one cent per dose shall be added to theallowable ingredient cost <strong>of</strong> a prescription for an oral solid if the drug isdispensed to a patient in a nursing home in unit dose packaging prepared bythe pharmacist. Unit-dose reimbursements are permitted only for patientswith Plan 300 eligibility.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage92DateAugust 1, 2013Claim the additional reimbursement by placing a “3” in “Unit Dose Indicator”(field 429-DT) for electronic claims, as explained under Point <strong>of</strong> Sale ClaimSubmission, or a “09” in the Basis Cost (field 14) on the paper claim form, asexplained under Paper Claim Submission. The additional reimbursement willbe automatically added, possibly resulting in reimbursement that is higherthan your submitted charge.Credits: Payment may be made only for unit-dose-packaged drugs that areconsumed by the patient. Any previous charges for intact unit-dosepackages returned to the pharmacy must be credited to the Medicaidprogram. Such credits may be shown on future billings. If no additionalbillings are to be made, direct a refund in the drug cost component.In accordance with state and federal law, proper crediting to <strong>Iowa</strong> Medicaid isrequired for the return <strong>of</strong> unused medications upon therapy discontinuationor a member’s discharge, transfer, or death.Both the long-term-care pharmacy and the nursing facility are subject t<strong>of</strong>inancial review by the state to ensure that medications are being returned tothe pharmacy when permitted by state and federal law and proper credits areapplied to the <strong>Iowa</strong> Medicaid program.4. Reimbursement for VaccinationsVaccines for mass immunizations, such as might occur with nursing homepatients, are payable to a pharmacy. Examples are vaccines such asinfluenza vaccine and pneumonia vaccine.Payment is allowed on a per-dose basis. Reimbursement is limited to thelesser <strong>of</strong> the pharmacist’s usual charge per dose or the cost <strong>of</strong> the dose plusthe current pr<strong>of</strong>essional fee. Each dose must be billed on the billing form <strong>of</strong>the patient receiving the dose. Where available, unit-dose syringes should bedispensed.In 1995, the <strong>Department</strong> implemented the Vaccines for Children (VFC)immunization program. The VFC Program was created to meet thevaccination needs <strong>of</strong> children from birth through 18 years <strong>of</strong> age. Theprogram is intended to help raise childhood immunization levels, especiallyamong infants and young children.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage93DateAugust 1, 2013Under the VFC program, all providers are required to follow the most currentRecommended Immunization Schedule from the Advisory Committee onImmunization Practices (ACIP). The following vaccines may be ordered underthe VFC program:♦ DTaP♦ DTaP/Hep B/IPV(Pediarix)♦ DTaP/IPV/Hib (Pentacel)♦ DTaP/IPV (Kinray)♦ DT (pediatric)♦ Td preservative free♦ Tdap♦ Hib♦ Hib/Hep B♦ Hepatitis A♦ Hepatitis B♦ HPV (Gardasil)♦ Influenza♦ MMR♦ MMR/V (ProQuad)♦ Meningococcal conjugate (Menactra)♦ Pneumococcal conjugate (Prevnar)♦ Polio♦ Rotavirus♦ VaricellaFor more information, see the <strong>Iowa</strong> <strong>Department</strong> <strong>of</strong> Public Health web page:http://www.idph.state.ia.us/ImmTB/Immunization.aspx?prog=Imm&pg=VfcAs a result, pharmacists are not reimbursed for providing these vaccineswhen administered by the practitioner. EXCEPTIONS: Payment forimmunizations administered to these persons will continue:♦ Medicaid members who are enrolled in an HMO that has contracted toprovide specific Medicaid services.♦ When Medicare makes payment, the deductibles, coinsurance, and anyMedicaid-covered services beyond the scope <strong>of</strong> Medicare are consideredfor coverage for Medicaid members who are dually eligible for Medicaidand Medicare.♦ Pharmacies enrolled in the Vaccines for Children (VFC) Program throughthe <strong>Iowa</strong> <strong>Department</strong> <strong>of</strong> Public Health may administer influenza vaccinesfor children age 18 and under. Pharmacies will be paid for administration<strong>of</strong> influenza vaccines when the vaccine is covered under the VFC Program.Pharmacists can be reimbursed for vaccines for patients in an institutionalsetting where facility staff administer the vaccine.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage94DateAugust 1, 2013E. BILLING SYSTEM<strong>Iowa</strong> Medicaid Enterprise provides for on-line, real-time processing <strong>of</strong> Medicaidpharmacy claims. Through electronic submission, you are able to submit claimsmore accurately. You also receive your Medicaid payments sooner than if yousubmitted paper claims.Point-<strong>of</strong>-sale (POS) transactions are handled by the <strong>Iowa</strong> Medicaid EnterprisePharmacy Point <strong>of</strong> Sale (POS) Unit. POS will handle the overrides for prospectivedrug utilization review edits such as high dose, therapeutic duplication, refill toosoon, excessive days supply, dose consolidation, duplicate claim, orimmunosuppressant drugs.<strong>Provider</strong>s that wish to exercise the point <strong>of</strong> sale billing option must complete the<strong>Iowa</strong> DHS Point <strong>of</strong> Sale Agreement. Please visit www.iowamedicaidpos.com tocomplete this agreement. You may call the (Point <strong>of</strong> Sale) POS Helpdesk at877-463-7671 or locally at 515-256-4608.1. Point <strong>of</strong> Sale Claim SubmissionFor point-<strong>of</strong>-sale (POS) submitters, refer to your POS Payer Sheet for claimsubmission instructions explanation <strong>of</strong> the data fields for the electronic billingformat. (To view the instruction on line, click here.)The <strong>Iowa</strong> Medicaid Enterprise eliminated the procedure <strong>of</strong> paying pharmacyclaims and then billing the primary insurance company on behalf <strong>of</strong> themembers (“pay and chase”) effective January 16, 2007, except for childrenunder age 21 and pregnant women.♦ For members under age 21, pharmacy claims may be processedthrough Pharmacy Point <strong>of</strong> Sale System with <strong>Iowa</strong> Medicaid as theprimary insurer.♦ For members who are pregnant, bill claims through the PharmacyPoint <strong>of</strong> Sale System with <strong>Iowa</strong> Medicaid as the primary insurer. To get a$0.00 copayment:• Enter code “2” (medical certification) in the prior authorization typecode field (NCPDP field 461-EU), and• Enter code “4” in the Prior Auth Number Submitted (NCPDP field462-EV).
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage95DateAugust 1, 2013♦ For all other Medicaid members with other prescription insurance, thatinsurance is primary and Medicaid is secondary.• Ask the member for the primary prescription insurance card.• If a member has primary pharmacy insurance, submit the claim to theprimary insurance first and then the copay to Medicaid last, using a “8”in the OTHER COVERAGE CODE field (field 308-C8).• If a member has primary pharmacy insurance and the claim is notcovered by the primary insurance, submit the claim to Medicaid usinga “3” in the OTHER COVERAGE CODE field (field 308-C8).• If a member has <strong>Iowa</strong> Medicaid pharmacy insurance only (or does nothave the primary prescription insurance information), enter a “1” inthe OTHER COVERAGE CODE field (field 308-C8).a. Claims Rejected Due to Other Insurance CoverageWhen a claim is submitted with a blank field or a zero in the OTHERCOVERAGE CODE field but the <strong>Iowa</strong> Medicaid eligibility file has third-partyliability (TPL) information, the Medicaid claim will be denied and you willreceive a rejection code <strong>of</strong> 41, “Submit to Primary Payer.”The Point-<strong>of</strong>-Sale System will give the policy number and the type <strong>of</strong>coverage. Most times the insurance company name is given. However,for the less common companies, a code is given in place <strong>of</strong> the name.Use the primary prescription insurance billing information to bill theprimary insurance. If necessary, you may contact the IME <strong>Provider</strong>Services for the name and address <strong>of</strong> the health insurance company.After billing the other company, resubmit the claim with one <strong>of</strong> thefollowing codes the OTHER COVERAGE CODE field:♦ Use code 1 if the member states that there is no other insurancecoverage. If the claim has already been rejected with a reject code<strong>of</strong> 41 “Submit to Primary Payer,” <strong>Iowa</strong> Medicaid’s eligibility fileconflicts with the primary third-party insurance company’sinformation. See Correction <strong>of</strong> Insurance Information.♦ Use code 3 if other coverage does exist but the drug is not coveredunder the primary insurance plan.♦ Use code 8 when payment is not collected. Example: The primarythird-party insurance is 100% major medical.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage96DateAugust 1, 2013b. Correction <strong>of</strong> Insurance InformationThe <strong>Department</strong> makes every attempt to keep current data regardingother insurance Medicaid members may have. However, if the primaryinsurance is no longer valid or has changed, the <strong>Department</strong>’s recordsneed to be corrected. The pharmacy can facilitate this in one <strong>of</strong> threeways:♦ Instruct the client to notify the <strong>Department</strong>; or♦ Complete form 470-2826, Insurance Questionnaire, available on theIME web site (www.ime.state.ia.us/), under <strong>Provider</strong>s/Forms, andFAX the form to Revenue Collections at (515) 725-1352; or♦ Notify the <strong>Department</strong> by e-mailing Revcoll@dhs.state.ia.us or bycalling (515) 256-4619 (local) or 1-866-810-1206. The minimuminformation necessary for insurance carriers to verify the otherinsurance coverage is the following:• Member last name• Member first name• State identification number or social security number• Date <strong>of</strong> birth• Policy number• Full insurance company nameFor example, if the company is Blue Cross/Blue Shield, include whichstate the policy is from, as most every state has a BC/BS carrier. (In<strong>Iowa</strong>, it’s Wellmark.)2. Claiming Payment for Retroactively Eligible MemberFor <strong>Iowa</strong> Medicaid prescription drug claims involving claims for a memberwhose Medicaid eligibility was determined retroactively, call the IME Point <strong>of</strong>Sale (POS) Unit at (515) 256-4608 (local calls) or 877-463-7671. Have thefollowing information available:♦ The pharmacy’s national provider identifier.♦ The member’s <strong>Iowa</strong> Medicaid number, name, and date <strong>of</strong> birth.♦ The drug’s name, strength, quantity, and dates requested forreimbursement.♦ The date the pharmacy was made aware the member had Medicaidcoverage for the state <strong>of</strong> <strong>Iowa</strong>.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage97DateAugust 1, 2013For medications payable on <strong>Iowa</strong> Medicaid, the POS staff will put an overrideon the point-<strong>of</strong>-sale system for the pharmacy to rebill the claims forreimbursement.3. Claim Attachment Control, Form 470-3969If you want to submit electronically a claim that requires an attachment, youmust submit the attachment on paper using the following procedure:♦ Complete form 470-3969, Claim Attachment Control. To view a sample <strong>of</strong>this form on line, click here.Complete the “attachment control number” with the same numbersubmitted on the electronic claim. IME will accept up to 20 characters(letters or digits) in this number. If you do not know the attachmentcontrol number for the claim, please contact the person in your facilityresponsible for electronic claims billing.♦ Staple the additional information to form 470-3969. Do not attach apaper claim.♦ Mail the Claim Attachment Control with attachments to:Medicaid ClaimsPO Box 150001Des Moines, IA 50315Once IME receives the paper attachment, it will manually be matched upto the electronic claim using the attachment control number and thenprocessed.4. Paper Claim SubmissionTraditional Universal Claim forms are no longer accepted. The new universalclaim forms PUCF-D01PT (VER 1.2) can be ordered by calling CommuniFormat 800-564-8140, or online at http://www.ncpdp.org/Universal-Claim-Forms.aspx.The following table contains information that will aid in the completion <strong>of</strong> thepharmacy claim form. The table follows the form by field name, giving a briefdescription <strong>of</strong> the information to be entered, and whether providinginformation in that field is required, optional, or conditional on the individualmember’s situation.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage98DateAugust 1, 2013FIELD NAME/DESCRIPTIONINSTRUCTIONS1 – CARDHOLDER ID MANDATORY. Enter the member’s Medicaid IDnumber. Copy this directly from the MedicalAssistance Eligibility Card. It consists <strong>of</strong> sevennumeric characters followed by a letter, i.e.,1234567A.2 – GROUP ID NOT USED. Leave blank.3 – LAST NOT USED. Submit information under Patientsegment.4 – FIRST NOT USED. Submit information under Patientsegment.5 – PLAN NAME IAMED6 – BIN NUMBER 0119337 – BIN NUMBER IAPOPPATIENT8 – PATIENT’S LAST NAME REQUIRED. Must be submitted.9 – PATIENT’S FIRST NAME REQUIRED. Must be submitted.10 – PERSON CODE NOT USED.11 – DATE OF BIRTH REQUIRED. Enter the member’s birth date using atwo-digit entry for each <strong>of</strong> the following: month,day, and year.12 – PATIENT GENDER CODE REQUIRED. Enter the gender.13 – RELATIONSHIP TOCARDHOLDERNOT USED.PHARMACY15 – SERVICE PROVIDER ID MANDATORY. Enter the pharmacy’s nationalprovider identifier (NPI).16 – SERVICE PROVIDER IDQUALIFIERMANDATORY. Enter “01” for national provideridentifier (NPI).
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage99DateAugust 1, 2013FIELD NAME/DESCRIPTIONINSTRUCTIONS17 – PHARMACY NAME REQUIRED. Enter the pharmacy’s name.18 – PHONE NUMBER OPTIONAL. Entering the pharmacy’s area code andphone number may expedite processing <strong>of</strong> theclaim.19 – ADDRESS REQUIRED. Enter the pharmacy’s street address.20 – CITY REQUIRED. Enter the pharmacy’s city.21 – STATE REQUIRED. Enter the pharmacy’s state.22 – ZIP REQUIRED. Enter the pharmacy’s zip code.PRESCRIBER25 – PRESCRIBER ID REQUIRED. Enter the national provider identifier(NPI) <strong>of</strong> the prescribing practitioner.26 – ID QUALIFIER 01 = NPI27 – PRESCRIBER LAST NAME REQUIRED.PHARMACIST28 – PHARMACIST ID NOT USED.29 – ID QUALIFIER NOT USED.CLAIM30 – PRESCRIPTION SERV.REF# (RX NUMBER)31 – PRESCRIPTION SERV.REF# (RX NUMBER) QUALIFIERMANDATORY. Enter the prescription number youhave assigned to the prescription being billed. Thisnumber must be all numeric. No alpha charactersare allowed.1 = RX BILLING32 – FILL # REQUIRED. Enter “00” for a new prescription, and01-99 for refills.33 – DATE WRITTEN REQUIRED. Enter the date the prescription waswritten using a two-digit entry for each <strong>of</strong> thefollowing: month, day, and year. CCYYMMDD
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage100DateAugust 1, 2013FIELD NAME/DESCRIPTIONINSTRUCTIONS34 – DATE OF SERVICE MANDATORY. Enter the date the prescription wasfilled using a two-digit entry for each <strong>of</strong> thefollowing: month, day, and year. CCYYMMDD35 – SUBMISSIONCLARIFICATIONOPTIONAL.36 – PRESCRIPTION ORIGIN OPTIONAL.37 – PRODUCT/SERVICE ID MANDATORY. Enter the national drug code (NDC)found on the drug’s label. All <strong>of</strong> the numerals inthe NDC, including the package size, must becurrent and exactly match the NDC <strong>of</strong> the productactually dispensed.Be careful to copy the NDC exactly as it appears,including leading zeros. If the product number isonly three digits long, enter a leading zero.For a compound, “0” must appear in this field. Listeach ingredient, NDC, quantity, and charge in theCOMPOUND section.38 – PRODUCT/SERVICE IDQUALIFIER00 = COMPOUND03 = NDC39 – PRODUCT DESCRIPTION REQUIRED.40 – QUANTITY DISPENSED REQUIRED. Give the number <strong>of</strong> tablets, capsules,etc. or the metric measurement for liquids,creams, etc. Be sure the billed quantity, whendivided by the number <strong>of</strong> days’ supply, is anappropriate amount for that therapeutic class <strong>of</strong>drugs. If the quantity is a fractional amount, use adecimal point.41 – DAYS SUPPLY REQUIRED. Enter the number <strong>of</strong> days theprescription will last.42 – DAW CODE (MACOVERRIDE)43 – PRIOR AUTH #SUBMITTEDLeave blank.CONDITIONAL. Leave blank unless one <strong>of</strong> thefollowing applies:1 = 72 hour supply4 = Pregnant5 = Nursing facility vaccine7 = Mental health drugs
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage101DateAugust 1, 2013FIELD NAME/DESCRIPTIONINSTRUCTIONS44 – PA TYPE CONDITIONAL. Enter code “2” if a number wasentered in the “PRIOR AUTH # SUBMITTED” box.Otherwise, leave blank.45 – OTHER COVERAGE CODE CONDITIONAL. To determine whether the memberhas drug coverage under other insurance, checkthe member’s eligibility using the EligibilityVerification System (ELVS) or the IME web portal.♦♦♦♦If a member has <strong>Iowa</strong> Medicaid pharmacyinsurance only and no other primary insurance,leave this field blank or enter a zero.Enter code “1” if the member states there is noother insurance but the claim has already beenrejected with a reject code <strong>of</strong> 41 “Submit toPrimary Payer.” <strong>Iowa</strong> Medicaid’s eligibility fileconflicts with the primary third-party insurancecompany’s information.Enter code “3” if other coverage does exist andthe drug is not covered under the primaryinsurance plan. NOTE: Also allowed for PartD excluded drugs.Enter code “8” when billing is for patientfinancial responsibility.46 – DELAY REASON NOT USED.47 – LEVEL OF SERVICE NOT USED.48 – PLACE OF SERVICE OPTIONAL.CLINICAL49 – DIAGNOSIS CODE NOT USED.Only the indicator “06 = Patient Pay Amount”will be accepted as an other payer-patientresponsibility amount qualifier.50 – DIAGNOSIS CODEQUALIFIERNOT USED.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage102DateAugust 1, 2013FIELD NAME/DESCRIPTIONINSTRUCTIONSDUR51 – DUR/PPS CODE REASON Leave blank.52 – DUR/PPS CODE SERVICE Leave blank.53 – DUR/PPS CODE RESULT Leave blank.54 – LEVEL OF EFFORT Leave blank.55 – PROCEDURE MODIFIER Leave blank.COB OTHER PAMENTSCOB1 – PRIMARY56 – OTHER PAYER ID REQUIRED FOR COB. Primary payer.57 – OTHER PAYER IDQUALIFIERREQUIRED FOR COB. Primary payer.58 – OTHER PAYER DATE REQUIRED FOR COB. Primary payer.If the patient has other insurance coverage, enterthe date the claim was paid or rejected by theother insurer.59 – OTHER PAYER REJECTCODESCONDITIONAL. If the patient has other insurancecoverage but the claim was rejected, enter therejection codes assigned by the other insurer (ifknown).COB1 – SECONDARY60 – OTHER PAYER ID REQUIRED FOR COB. Payer ID <strong>of</strong> primary payer.61 – OTHER PAYER IDQUALIFIERREQUIRED FOR COB.62 – OTHER PAYER DATE REQUIRED FOR COB.If the patient has other insurance coverage, enterthe date the claim was paid or rejected by theother insurer.63 – OTHER PAYER REJECTCODESCONDITIONAL. If the patient has other insurancecoverage but the claim was rejected, enter therejection codes assigned by the other insurer (ifknown).
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage103DateAugust 1, 2013FIELD NAME/DESCRIPTIONINSTRUCTIONSCOMPOUND64 – DOSAGE FORMDESCRIPTION CODE65 – DISPENSING UNIT FORMINDICATOR66 – ROUTE OFADMINISTRATION67 – INGREDIENT COMPONENTCOUNTMANDATORY.MANDATORY.OPTIONAL.MANDATORY.68 – PRODUCT NAME REQUIRED. Submit for each compound component.69 – PRODUCT ID REQUIRED. Submit for each compound component.70 – PRODUCT ID QUALIFIER REQUIRED. Submit for each compound component.71 – INGREDIENT QTY REQUIRED. Submit for each compound component.72 – INGREDIENT DRUG COST OPTIONAL. Submit for each compound component.73 – BASIS OF COST OPTIONAL. Submit for each compound component.PRICING74 – USUAL & CUSTOMARYCHARGE75 – BASIS OF COSTDETERMINATION76 – INGREDIENT COSTSUBMITTEDREQUIRED. Enter the usual and customary charge.CONDITIONAL. Enter code “09” to indicate unit dosedrug. Otherwise, leave blank.REQUIRED. Enter the pharmacy’s submittedproduct component cost <strong>of</strong> the dispensedprescription. Amount also included in the grossamount due.340B pricing submitted in this field whenapplicable.77 – DISPENSING FEESUBMITTEDREQUIRED. Enter the pharmacy’s usual andcustomary dispensing fee. Enter zeros if nodispensing fee is charged for the prescription.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage104DateAugust 1, 2013FIELD NAME/DESCRIPTION78 – PROFESSIONAL SERVICEFEE SUBMITTED79 – INCENTIVE AMOUNTSUBMITTED80 – OTHER AMOUNTSUBMITTEDINSTRUCTIONSREQUIRED. Enter the pharmacy’s usual andcustomary dispensing fee. Enter zeros if nodispensing fee is charged for the prescription.Leave blank.Leave blank.81 – SALES TAX SUBMITTED NOT USED.82 – GROSS AMOUNT DUE REQUIRED. Enter the total charge for this item.The total claim charge must be equal to the sum <strong>of</strong>the submitted ingredient cost submitted and thesubmitted dispensing fee.83 – PATIENT PAID AMOUNT Leave blank.84 – OTHER PAYER AMOUNTPAID #185 – OTHER PAYER AMOUNTPAID #286 – OTHER PAYER-PATIENTRESPONSIBILITY AMOUNT #187 – OTHER PAYER-PATIENTRESPONSIBILITY AMOUNT #2NOT USED.NOT USED.REQUIRED FOR IA COB CLAIMS.REQUIRED FOR IA COB CLAIMS.88 – NET AMOUNT DUE REQUIRED. Enter the total price less the deductibleamount. NOTE: If resubmitting a claim that is over12 months old, the word “resubmit” must clearlyappear on the claim to avoid denials for timelyfiling. This procedure can be used only if theoriginal submission was within the last 12 months.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage105DateAugust 1, 2013F. EDITS AND SPECIAL BILLING INFORMATION1. Claims for Deceased MembersSubmit claims for all <strong>Iowa</strong> Medicaid members using the dispensing date.Pharmacy claims must be billed before a member’s date <strong>of</strong> death for claimsprocessing. Failure to bill before the date <strong>of</strong> death may result in claimrecoupment for any claims processed after that date <strong>of</strong> death.2. Common Billing ErrorsMedications can <strong>of</strong>ten be described using three measures: each, grams, andmilliliters. It is important to choose the correct unit <strong>of</strong> measure when billing.MedicationBactroban cream(mupirocin)Bactroban ointment(mupirocin)Byetta 5 mcg(exenatide)Byetta 10 mcg(exenatide)Correct Unitfor BillingGramsGramsMl (Submit indecimal format; donot round)Ml (Submit indecimal format; donot round)Days’Quantity SupplyVaries; should be Variesdivisible by 15gramsVaries; should be Variesdivisible by 22grames1.2 ml 302.4 ml 30Copaxone (glatiramer) Each 1 30Diastat ACDL gelEach (kit contains1 Varies(diazepam)2 syringes; bill #<strong>of</strong> kits)Enbrel 25 mg Each 1 1Enbrel 25 mg/0.5 ml(etanercept)Enbrel SureClick(etanercept)Fragmin (dalteparin)Ml (Submit indecimal format; donot round)Ml (Submit indecimal format; donot round )Ml (Submit indecimal format; donot round)Varies claimsshould be divisibleby 0.5 mlVaries should bedivisible by .98 mlVaries3030Varies
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage106DateAugust 1, 2013MedicationGamunex 10% (immuneglobulin)Humira (adalimumab)Influenza vaccinesKineret (anakinra)Lovenox (enoxaparin)Miacalcin NS (calcitonin)Nascobal(cyanocobalamin)Neupogen 400 mcg(filgrastim)Neupogen 600 mcg(filgrastim)Pegasys (peginterferonAlfa-2a)Peranex HC (lidocaine/hydrocortisone)Correct Unitfor BillingMl (Each vial is 10ml)Each (kit contains2 syringes)Ml (Submit indecimal format; donot round)Ml (Submit indecimal format; donot round)Ml (Submit indecimal format; donot round)Ml (Submit indecimal format; donot round)Ml (Submit indecimal format; donot round)Ml (Submit indecimal format; donot round)Ml (Submit indecimal format; donot round)Each (kit contains4 syringes)QuantityVariesDays’SupplyVaries2 300.5 ml 1Varies; should bedivisible by 0.67Varies30Varies3.7 30Varies; claims 30should be divisibleby 2.3 mlVaries; claims 30should be divisibleby 1.6 mlVaries; claims 30should be divisibleby 0.5 ml1 28Each 1 VariesProair HFA (albuterol) Grams 8.5 grams 30Proventil HFA (albuterol) Grams 6.7 grams 30Rebif pack (interferonBeta-1a)Ml (Submit indecimal format; donot round)4.2 ml 30Rebif syringe (interferonBeta-1a)Ml (Submit indecimal format; donot round)6 ml 30Remicade (infliximab) Each 1 VariesRestasis (cyclosporine) Each 32/64 30Risperdal Consta(risperidone)Each 2 28
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage107DateAugust 1, 2013MedicationStadol nasal spray 10mg/ml (butorphanol)Synagis 50 mg(palivizumab)Correct Unitfor BillingMl (Submit indecimal format; donot round)Ml (Submit indecimal format; donot round)Days’Quantity SupplyVaries; claims Variesshould be divisibleby 2.5 ml0.5 ml 30Synagis 100 mgMl 1 ml 30(palivizumab)Ventolin HFA (albuterol) Grams 18 grams 30Xopenex HFA(levalbuterol)3. Compounded PrescriptionsGramsVaries; claimsshould be divisibleby 15 gramsVaries<strong>Iowa</strong> Medicaid will process claims for compounded prescriptions in the NCPDPD.Ø format using the multiple ingredient functionality. All applicable edits,including Preferred Drug List (PDL) rules, apply to each NDC submitted.<strong>Provider</strong>s must submit the NDCs for the active ingredients dispensed tocreate the compound.A dispensing fee will be added to the claim when a drug within the compoundis reimbursed at EAC or State MAC price. There will be no additional fee paidto prepare the compounded prescription. <strong>Provider</strong>s need to submit thequantity <strong>of</strong> the active ingredients used in the compound for reimbursement,not the quantity <strong>of</strong> the total amount <strong>of</strong> the compound made.4. Coverage <strong>of</strong> Non-Drug ProductsProducts not approved as prescription drugs by the Food and DrugAdministration do not meet the definition <strong>of</strong> “covered outpatient drugs” andcannot be covered by Medicaid pharmacy program. Coverage <strong>of</strong> theseproducts is allowed in other coverage areas, such as medical supplies.Medicaid will continue to cover certain non-drug products as listed below.Pharmacies shall continue to provide these products and bill Medicaid throughthe point <strong>of</strong> sale system. Prior authorizations (PA) will be submitted throughthe Pharmacy PA system.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage108DateAugust 1, 2013Product√ IndicatesPA RequiredMAC per Tablet,ML or GMAmmonium lactate lotion 12% 0.0933AquADEKs capsules √ 0.1489AquADEKs tabs √ 0.5306AquADEKs solution √ 0.3678Bacterostatic sodium chloride injection 0.9% 0.0459Bacterostatic water for injection 0.0240Bacterostatic parabens water for injection 0.0420Calcionate syrup 1.8 gm/5 √ 0.0417Calcium carbonate 500 mg chewable tablets √ 0.0205Calcium carbonate 750 mg chewable tablets √ 0.0381Calcium carbonate 1000 mg chewable tablets √ 0.0469Calcium carbonate 1250 mg chewable tablets √ 0.1026Calcium carbonate 1250 mg/5 ml suspension √ 0.0579Calcium carbonate 600 mg tablets √ 0.0440Calcium carbonate-vitamin D 500 mg/200 unit √ 0.0468Calcium carbonate-vitamin D 600 mg/200 unit tablets √ 0.0294Calcium carbonate-vitamin D 600/400 unit tablets √ 0.0516Calcium gluconate 650 mg tablets √ 0.0152Calcium lactate 650 mg tablets √ 0.0232Calvite P&D tablets √ 0.1846Cerovite Jr chewable tablets √ 0.0551Cerovite liquid √ 0.0228Cholecalciferol 400 Unit tablets √ 0.0249Epoprostenolol diluents (Flolan) 0.5 mg 12.72Epoprostenolol diluents (Flolan) 1.5 mg 40.04Ferrex 150 capsules plus √ 1.2769Ferrous fumarate 325 mg tablets 0.0181Ferrous gluconate 325 mg tablets 0.0462Ferrous sulfate 75 mg/0.6 ml drops 0.0388Ferrous sulfate 75 mg/ml drops 0.1629Ferrous sulfate 220 mg/5 ml elixir 0.0127Ferrous sulfate 325 mg tablets 0.0246Mag-delay tablets √ 0.1198Magnesium oxide 400 mg tablets √ 0.0852Magonate 1000 mg/5 ml liquid √ 0.0267Maximum D3 capsules √ 0.9900Metronidazole powder 1.5775Multiple vitamins tablets √ 0.0261Nephro-Vite tablets √ 0.1107Niacin 50 mg tablets 0.0185Niacin 100 mg tablets 0.0239Niacin 250 mg tablets 0.0369Niacin 500 mg tablets 0.0372
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage109DateAugust 1, 2013Product√ IndicatesPA RequiredMAC per Tablet,ML or GMPediatric oral electrolyte solution 0.0054Phos-Nak powder concentrate √ 0.3880Poly-Iron 150 mg capsules √ 0.2750Poly-Vi-Sol drops √ 0.1604Poly-Vi-Sol w/iron drops √ 0.1604Progesterone powder 2.0231Progesterone micronized powder 1.0841Pyridoxine 100 mg tablets √ 0.0399Pyridoxine 25 mg tablets √ 0.0697Pyridoxine 50 mg tablets √ 0.1050Slow-mag tablets √ 0.1708Sodium bicarbonate 325 mg tablets √ 0.0116Sodium bicarbonate 650 mg tablets √ 0.0134Sodium chloride injection 0.9% 0.0030Sodium chloride solution 0.9% for inhalation 0.0451Thera-M enhanced tablets √ 0.0538Tri-Vi-Sol drops √ 0.1887Tri-Vi-Sol w/iron drops √ 0.1400Vitamin A 10000 IU capsules √ 0.0215Vitamin B-1 100 mg tablets √ 0.0425Vitamin B-1 50 mg tablets √ 0.0217Vitamin B-12 1000 mcg CR tablets √ 0.0998Vitamin B-12 1000 mcg tablets √ 0.0541Vitamin C 500 mg chewable tablets √ 0.0547Vitamin C 500 mg tablets √ 0.0447Vitamin C 1000 mg tablets √ 0.0699Vitamin D 400 unit drops √ 0.1440Vitamin D 1000 unit tablets √ 0.0499Vitamin D 2000 unit tablets √ 0.0349Vitamin D 400 unit tablets √ 0.0220Vitamin E 400 unit capsules √ 0.08725. Date <strong>of</strong> Birth VerificationPoint <strong>of</strong> sale edits for the exact date <strong>of</strong> birth from the eligibility file for <strong>Iowa</strong>Medicaid members. Field # 304-C4 (Date <strong>of</strong> Birth) on The National Counselfor Prescription Drug Programs (NCPDP) Payer Sheet is mandatory. TheNCPDP rejection message will state “09-Missing/Invalid Date <strong>of</strong> Birth.”Claims should be resubmitted with the correct date <strong>of</strong> birth for the member.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage110DateAugust 1, 20136. Override CodesA 72-hour emergency supply <strong>of</strong> medication may be dispensed using priorauthorization type code “1” as a point <strong>of</strong> sale override. The provision for a72-hour supply can be used in an emergency situation only one time permember, per drug.A seven-day override <strong>of</strong> the prior authorization requirement will be allowedwhile the prescriber is requesting prior authorization for certain mental healthdrugs. The override applies to drugs that are deemed to have a significantvariation in therapeutic or side effect pr<strong>of</strong>ile from other drugs in the sametherapeutic class. See the Preferred Drug List at: www.iowamedicaidpdl.comThe pharmacy may use a prior authorization type code “7” as a point <strong>of</strong> saleoverride for applicable mental health drugs. The seven-day provision can beused only one time per member, per NDC, per 30 days.7. Proper Reporting <strong>of</strong> NDCsThe <strong>Iowa</strong> Medicaid Program can cover only drugs from manufacturers whohave signed national Medicaid drug rebate agreements with the Centers forMedicare and Medicaid Services (CMS). Drug companies sign the agreementsfor specific drug manufacturer codes called national drug codes (NDC).Since rebates are determined by <strong>Iowa</strong> Medicaid’s utilization data, it isimperative that pharmacies and providers bill <strong>Iowa</strong> Medicaid using the correctNDC number <strong>of</strong> the drug actually dispensed or administered.If a provider is dispensing or administering one drug and billing for an NDCdifferent from the drug being dispensed or administered, it is consideredfraud, which can result in claims being recouped, sanctions, and termination<strong>of</strong> provider agreements. The Program Integrity Unit will be monitoring forthis in their reviews.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage111DateAugust 1, 20138. Prospective Drug Utilization Review (Pro-DUR)The goal <strong>of</strong> Prospective DUR is to identify potential drug therapy concerns toallow the pharmacist to use pr<strong>of</strong>essional judgment regarding the need forintervention, such as whether or not to contact the prescribing physician.The following prospective DUR edits will cause claims to deny:EditNumber andMessageReason for the Denial* OverrideProvidedAge Edits75 - PRIORAUTHORIZATIONREQUIREDCertain medications arepayable only for specificage groups.PA required.CostEffectiveness75 - PRIORAUTHORIZATIONREQUIREDCertain strengths shouldbe substituted withmore cost-effectivestrengths <strong>of</strong> the samemedication.PA required.DosageForm75 - PRIORAUTHORIZATIONREQUIREDAdditional text:NONPREFERREDCertain dosage formsshould be substitutedwith more cost-effectivedosage forms <strong>of</strong> thesame medication.PA required.ExcessiveDaysSupply19 - M/I DAYSSUPPLYAdditional text:EXCEEDS ALLOWABLEDAYS SUPPLYThe supply submitted ismore than 31 days.Request anexception topolicy if there is avalid reason whya supply morethan 31 days isrequired.15-DayInitialPrescriptionSupplyLimit76 - PLAN LIMITSEXCEEDEDThe supply submitted ismore than 15 days onselect drugs.PA required. SeeQuantity LimitOverride.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage112DateAugust 1, 2013EditNumber andMessageReason for the Denial* OverrideProvidedHigh DollarClaims78 - COST EXCEEDSMAXIMUMAdditional text:CLAIM EXCEEDS$10,000.00, PLEASECALL POS HELPDESKAll claims submitted inexcess <strong>of</strong> $10,000 willbe rejected. Afterverifying that thequantity and days’supply <strong>of</strong> the claim arecorrect, contact thePharmacy POS HelpDesk. See below.A one-timeoverride will begranted ifquantity anddays’ supply areaccurate andconsistent.Additional medicaldocumentation isrequired forlonger overrides.QuantityLimits76 - PLAN LIMITSEXCEEDEDIf the quantitysubmitted exceeds theestablished quantitylimit.PA required. SeeQuantity LimitOverride.Refill TooSoon79 - REFILL TOOSOONAdditional text:RX NUMBER/FILLDATE/NPI ORIf less than 90% <strong>of</strong> thepreviously paid claim forthat medication has notbeen used. See RefillToo Soon.If there is achange in dose;lost, stolen ordestroyed drug;or travel.NABP/DATE FOR NEXTFILLStepTherapyEdits75 - PRIORAUTHORIZATIONREQUIREDCertain therapeutic drugclasses are subject tostep therapy edits asdesignated on thePreferred Drug List.PA required.TabletSplitting19 - M/I DAYSSUPPLYAdditional text:MUST SPLIT TABLETSCertain medications thatare scored and easilyhalved should be split t<strong>of</strong>acilitate more costeffectiveuse <strong>of</strong> thedrugs.PA required.TherapeuticDuplication88 - DUR REJECTMESSAGEAdditional text:SITUATIONALIf a second claimsubmitted is atherapeutic duplication<strong>of</strong> a drug alreadysubmitted andreimbursed.PA required.* Always verify that the quantity and days’ supply on the claim are correct;then for an override contact: Pharmacy POS Help Desk at 877-463-7671 or(515) 256-4608 (local)
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage113DateAugust 1, 2013a. Age EditsCertain medications are payable only for specific age groups:Drug Name/Class<strong>Drugs</strong> FDA indicated forthe treatment <strong>of</strong>Alzheimer’s dementia(donepezil, galantamine,memantine, andrivastigmine)Aldara (imiquimod)Asmanex 110 mcgBrovanaAge EditPayable for members40 years <strong>of</strong> age andolderPayable for members12 years <strong>of</strong> age andolderPayable for membersless than 12 years <strong>of</strong>age.Payable for members18 years <strong>of</strong> age andolder.Prior Authorization(PA) RequirementPA is required formembers under 40years <strong>of</strong> age.PA is required formembers under 12years <strong>of</strong> age.PA is required formembers 12 years <strong>of</strong>age and older.PA is required formembers under 18years <strong>of</strong> age.Clorazepate Payable for members 9years <strong>of</strong> age and older.PA is required formembers under 9years <strong>of</strong> age.CompleraDuleraEdurantEligardErivedgePayable for members18 years <strong>of</strong> age andolder.Payable for members12 years <strong>of</strong> age andolder.Payable for members18 years <strong>of</strong> age andolder.Payable for members18 years <strong>of</strong> age andolder.Payable for members18 years <strong>of</strong> age andolder.PA is required formembers under 18years <strong>of</strong> age.PA is required formembers under 12years <strong>of</strong> age.PA is required formembers under 18years <strong>of</strong> age.PA is required formembers under 18years <strong>of</strong> age.PA is required formembers under 18years <strong>of</strong> age.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage114DateAugust 1, 2013Drug Name/ClassFemara (letrozole)FlurazepamAge EditPayable for members50 years <strong>of</strong> age andolder.Payable for members15 years <strong>of</strong> age andolder.Prior Authorization(PA) RequirementPA is required formember under 50years <strong>of</strong> age.PA is required formembers under 15years <strong>of</strong> age.Foradil Payable for members 5years <strong>of</strong> age and older.PA is required formembers under 5years <strong>of</strong> age.InlytaIsentress 25 mg and100 mg chewabletabletsJakafiNuvigil (armodafinil)OTC Polyethylene glycol3350 powderPayable for members18 years <strong>of</strong> age andolder.Payable for membersless than 12 years <strong>of</strong>age.Payable for members18 years <strong>of</strong> age andolder.Payable with a PA formembers 17 years <strong>of</strong>age and olderPayable for members 0to 12 years <strong>of</strong> age. PArequired for members13 to 18 years <strong>of</strong> age.Not covered formembers 19 years <strong>of</strong>age or over.PA is required formembers under 18years <strong>of</strong> age.PA is required formembers 12 years <strong>of</strong>age and older.PA is required formembers under 18years <strong>of</strong> age.PA is required formembers under 17years <strong>of</strong> age.PA is required formembers 13-18 years<strong>of</strong> age.Oxazepam Payable for members 6years <strong>of</strong> age and older.PA is required formembers under 6years <strong>of</strong> age.PerforomistProvigil (modafinil)Payable for members18 years <strong>of</strong> age andolder.Payable for members16 years <strong>of</strong> age andolderPA is required formembers under 18years <strong>of</strong> age.PA is required formembers under 16years <strong>of</strong> age and 21years <strong>of</strong> age andolder
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage115DateAugust 1, 2013Drug Name/ClassRevlimidAge EditPayable for members18 years <strong>of</strong> age andolder.Prior Authorization(PA) RequirementPA is required formembers under 18years <strong>of</strong> age.Serevent Payable for members 4years <strong>of</strong> age and older.PA is required formembers under 4years <strong>of</strong> age.Singulair 4 mg granulesStribildVeregen (sinecatechins)Zytigab. Cost Effectiveness EditPayable for membersless than 2 years <strong>of</strong>agePayable for members18 years <strong>of</strong> age andolder.Payable for members18 years <strong>of</strong> age andolder.Payable for members18 years <strong>of</strong> age andolder.PA is required formembers 2 years <strong>of</strong>age and older.PA is required formembers under 18years <strong>of</strong> age.PA is required formembers under 18years <strong>of</strong> age.PA is required formembers under 18years <strong>of</strong> age.Drug Dosage AlternativeAntivert tablet 50 mg Deny. Use two meclizine HC1 25 mgtablets.Benzonatate capsule 200 mg Deny. Use two benzonatate 100 mgcapsules.Buspirone tablet 30 mg Deny. Use two buspirone 15 mgtablets.Clindamycin capsule 300 mg Deny. Use multiples <strong>of</strong> clindamycin150 mg capsule.Hydroxyzine HC1tabletsHydroxyzine pamoatecapsulesImipramine pamoatecapsulesProzac or fluoxetineHC1 capsulesRheumatrex25 & 50mgDeny. Use hydroxyzine pamoate 25& 50 mg capsules.100 mg Deny. Use hydroxyzine pamoate 50mg capsules.Deny. Use imipramine HCL tablets.40 mg Deny. Use two fluoxetine HC1 20 mgcapsules.Deny. Use methotrexate.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage116DateAugust 1, 2013c. Dosage Form EditsForm Drug Dosage AlternativeProzac tablets fluoxetine 20 mg Deny. Use the capsule dosageform.Norvir tablets ritonavir 100 mg Deny. Use the capsule dosageform.Zantac capsules ranitidine 150 mg Deny. Use the tablet dosageform.Zantac capsules ranitidine 300 mg Deny. Use the tablet dosageform.d. Excessive Days SupplyThe claim will be rejected if the supply submitted is more than 31 days.If there is a valid reason why a supply <strong>of</strong> more than 31 days is required,request an exception to policy.e. High-Dollar ClaimsAll claims in excess <strong>of</strong> $10,000 submitted through the pharmacy point <strong>of</strong>sale system will be rejected with a denial message stating, “Claimexceeds $10,000, please call POS Help Desk at 877-463-7671 or(515) 256-4608 locally.”After verifying that the quantity and days' supply on the claim arecorrect, contact the Pharmacy POS Help Desk for consideration <strong>of</strong> anoverride. A technician or pharmacist will review the informationsubmitted and determine if an override shall be issued.As a part <strong>of</strong> this process, the <strong>Iowa</strong> Medicaid Program Integrity Unit mayrequest additional medical documentation regarding the case from theprescriber or pharmacy. This policy is intended to help ensure thatproper billing procedures are being followed.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage117DateAugust 1, 2013f. Refill Too SoonThe claim will be denied if not enough time has elapsed for the memberto use 90% <strong>of</strong> the supply issued under previously paid claim for thatmedication. An override will be considered if:♦ There is a change in dose;♦ The previously issued supply has been lost, stolen or destroyed; or♦ The member is traveling and will not be able to pick up the next refillat the normal time.g. Step Therapy EditsCertain therapeutic drug classes are subject to step therapy edits asdesignated on the Preferred Drug List. Antipsychotics-Atypicals:Step 1: Preferred generic drugs. No PA required.Step 2: Preferred brand name drugs. No PA required if a preferredgeneric trial is found in the paid claims system in the past 12 months.Step 3: Non-preferred drugs. PA required.h. Tablet SplittingCertain medications that are scored and easily halved should be split t<strong>of</strong>acilitate more cost-effective use <strong>of</strong> the drugs.Drug Product Quantity Days’ Supply CommentsAbilify 2 mg 15 30Abilify 5 mg 15 30 Use 10 mg tablets toobtain 5 mg daily doseAbilify 10 mg 15 30 Use 20 mg tablets toobtain 10 mg daily doseAbilify 15 mg 15 30 Use 30 mg tablets toobtain 15 mg daily doseAbilify 20 mg 15 30Abilify 30 mg 15 30Lexapro 5 mg 15 30 Use 10 mg tablets toobtain 5 mg daily doseLexapro 10 mg 15 30 Use 20 mg tablets toobtain 10 mg daily dose
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage118DateAugust 1, 2013i. Therapeutic DuplicationIf a second claim submitted is a therapeutic duplication <strong>of</strong> a drugalready submitted and reimbursed, overlapping claims will be consideredon an individual basis.Deny regardless <strong>of</strong> prescriberAnti-narcolepsy oranti-hyperkinesisagentsAntipsychoticsBarbituratesCentral nervoussystem stimulantsNonsteroidal antiinflammatorydrugs(NSAIDs)Provide prescriber verified documentation <strong>of</strong> thenecessity <strong>of</strong> the duplication in the treatment plan.After 12 weeks (84 days) <strong>of</strong> concomitant oral andinjectable antipsychotic medication use, provideprescriber verified documentation <strong>of</strong> the necessity inthe treatment plan.Provide prescriber verified documentation <strong>of</strong> thenecessity <strong>of</strong> the duplication in the treatment plan.Provide prescriber verified documentation <strong>of</strong> thenecessity <strong>of</strong> the duplication in the treatment plan.After 60 days <strong>of</strong> concomitant use, provide prescriberverified documentation <strong>of</strong> the necessity <strong>of</strong> theduplication in the treatment plan.9. Status Change for Preferred Brand Name <strong>Drugs</strong>When the status <strong>of</strong> a previously preferred brand-name drug changes tononpreferred, pharmacies are given a transition period <strong>of</strong> up to 30 days toallow utilization <strong>of</strong> existing stock <strong>of</strong> the brand-name product.If additional stock remains beyond this period, pharmacies may call the Point<strong>of</strong> Sale (POS) Helpdesk at 877-463-7671 or 515-256-4608 (local) to requestan override for the nonpreferred brand-name drug with a recent statuschange.10. Travel or Vacation Supplies <strong>of</strong> MedicationRequests <strong>of</strong> medications for travel or vacation should be planned well inadvance <strong>of</strong> the departure date.The pharmacy can process the first month’s prescriptions as usual, and thenmay call the Point <strong>of</strong> Sale (POS) Helpdesk at 877-463-7671 or 515-256-4608(local) to obtain up to a one-month supply <strong>of</strong> medications to total up to a60-day supply <strong>of</strong> medication.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage119DateAugust 1, 2013Exceptions to policy will not be granted if other sources for payment areavailable.11. 340B Drug Pricing ProgramIn order to become eligible to participate in the 340B Program, the providermust submit a request to the Office <strong>of</strong> Pharmacy Affairs (OPA) within theHealth Resources and Services Administration (HRSA). The OPA website ishttp://www.hrsa.gov/opa/. The request form is listed at the following link:ftp://ftp.hrsa.gov/bphc/pdf/opa/PrgmReg.pdf.It is very important that the OPA has accurate and up-to-date information,particularly your exact name and street address. It your responsibility to:♦ Contact the OPA with any changes in your information; and♦ Tell your wholesaler or manufacturer that you are registered for 340Bdiscount prices when you place an order.<strong>Provider</strong>s must enroll with <strong>Iowa</strong> Medicaid in order to bill and receivereimbursement for self-adminsitered drugs purchased through the 340BProgram.a. Covered Entity (CE)The covered entity (CE) has full responsibility and accountability forcompliance with all requirements to prevent diversion <strong>of</strong> covered drugsto individuals other than patients <strong>of</strong> the CE, and to prevent situations inwhich a drug is subject to both the 340B discount and a Medicaid rebateclaim.Use <strong>of</strong> a contract pharmacy arrangement (single or multiple) does notlessen a CE’s duty to ensure that the 340B Program is beingadministered in compliance with the statute and HRSA guidelines.It is imperative that all CEs participating in the 340B Program not onlycomply with program requirements but also be able to documentcompliance with those requirements in the event <strong>of</strong> an audit.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage120DateAugust 1, 2013To prevent duplicate discounts, HRSA requires CEs to indicate on OPAwebsite if they purchase drugs at 340B pricing for Medicaid patients(Medicaid Exclusion File), so Medicaid does not bill for rebates. HRSAdirects CEs to follow state guidelines when billing for 340B drugs. CEsmay not use a contracted pharmacy unless it has reached an agreementwith the state Medicaid agency on a method to prevent duplicatediscounts.b. <strong>Iowa</strong> Medicaid Billing/Reimbursement for CE Outpatient In-House Pharmacy or Contracted PharmacyAny CE or contracted pharmacy filling prescriptions for Medicaidmembers with drugs acquired through the 340B Program are required tobill Medicaid their 340B actual acquisition cost (340B AAC) plus thedispensing fee.If the CE or contracted pharmacy chooses the Medicaid carve-outoption, drugs shall be billed in accordance with existing state Medicaidreimbursement methodologies, allowing rebates to be collected.This is reviewed through a postpayment review. Overbillings are subjectto recoupment.12. Interpreter ServicesTranslation and interpretative services may be covered, whether done orallyor through sign language. Interpreters must provide only interpretationservices for your pharmacy. The services must facilitate access to Medicaidcovered services.In order for translation and interpretation services to be covered by <strong>Iowa</strong>Medicaid, the services must meet the following criteria:♦ Provided by interpreters who provide only interpretive services.♦ Interpreters may be employed or contracted by the billing provider.♦ The interpretive services must facilitate access to Medicaid-coveredservices.<strong>Provider</strong>s may only bill for these services if <strong>of</strong>fered in conjunction with anotherwise Medicaid covered service. Medical staff that are bilingual are notreimbursed for the interpretation but only for their medical services.Reimbursable time may include the interpreter’s travel and wait time.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage121DateAugust 1, 2013a. Documentation <strong>of</strong> the ServiceThe billing provider must document in the patient’s record the:♦ Interpreter’s name or company,♦ Date and time <strong>of</strong> the interpretation,♦ Service duration (time in and time out), and♦ The cost <strong>of</strong> providing the service.b. QualificationsIt is the responsibility <strong>of</strong> the billing provider to determine theinterpreter’s competency. Sign language interpreters should be licensedpursuant to <strong>Iowa</strong> Administrative Code 645 Chapter 361. Oralinterpreters should be guided by the standards developed by theNational Council on Interpreting in Health Care (www.ncihc.org)The following are instructions for billing interpretive services when thatservice is provided by an outside commercial translation service.♦ Bill code T1013 on the pr<strong>of</strong>essional CMS-1500 claim form:• For telephonic interpretive services use modifier “UC” to indicatethat the payment should be made at $1.70 per minute.• The lack <strong>of</strong> the UC modifier will indicate that the charge is beingmade for the 15 minute face-to-face unit.♦ Enter the number <strong>of</strong> minutes actually used for the provision <strong>of</strong> theservice.♦ Special note: Because the same code is being used but a conditionalmodifier may be necessary, any claim where the UC modifier is NOTused and the units exceed 24 will be paid at 24 units.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage122DateAugust 1, 2013G. REMITTANCE ADVICE AND FIELD DESCRIPTIONS1. Remittance Advice ExplanationTo simplify your accounts receivable reconciliation and posting functions, youwill receive a comprehensive Remittance Advice with each Medicaid payment.The Remittance Advice is also available on magnetic computer tape forautomated account receivable posting. To view a sample <strong>of</strong> this form on line,click here.The Remittance Advice is separated into categories indicating the status <strong>of</strong>those claims listed below. Categories <strong>of</strong> the Remittance Advice include paidclaims and denied claims:♦ Paid indicates all processed claims, credits and adjustments for whichthere is full or partial reimbursement.♦ Denied represents all processed claims for which no reimbursement ismade.Note that claim credits or recoupments (reversed) appear as regular claimswith the exception that the transaction control number contains a “1” in thetwelfth position and reimbursement appears as a negative amount.An adjustment to a previously paid claim produces two transactions on theRemittance Advice. The first appears as a credit to negate the claim; thesecond is the replacement or adjusted claim, containing a “2” in the twelfthposition <strong>of</strong> the transaction control number.If the total <strong>of</strong> the credit amounts exceeds that <strong>of</strong> reimbursement made, theresulting difference (amount <strong>of</strong> credit less the amount <strong>of</strong> reimbursement) iscarried forward and no check is issued. Subsequent reimbursement will beapplied to the credit balance, as well, until the credit balance is exhausted.A detailed field-by-field description <strong>of</strong> each informational line follows. It isimportant to study these examples to gain a thorough understanding <strong>of</strong> eachelement as each Remittance Advice contains important information aboutclaims and expected reimbursement.Regardless <strong>of</strong> one’s understanding <strong>of</strong> the Remittance Advice, it is sometimesnecessary to contact IME <strong>Provider</strong> Services with questions. When doing so,keep the Remittance Advice handy and refer to the transaction controlnumber <strong>of</strong> the particular claim. This will result in timely, accurateinformation about the claim in question.
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage123DateAugust 1, 20132. Remittance Advice Field DescriptionsField NameField DescriptionA R.A. No. Remittance Advice numberB Warrant Number Check number (usually zeros). Contact IME forcheck number.C <strong>Provider</strong> Name Name <strong>of</strong> the pay-to provider as registered with IMED <strong>Provider</strong> Address Address registered with IME for the mailing <strong>of</strong>Remittance Advice and paper checksEImportant IMEInformationReminders and updates from IMEF Run Date Date the Remittance Advice was createdG Date Paid Date the Remittance Advice was mailed and checkwas releasedH Prov. Number National provider identifier (NPI) <strong>of</strong> the billing(pay-to) providerI Page Page numberJ Number <strong>of</strong> Claims Number <strong>of</strong> claims processed for each defined statusKBilled Amount <strong>of</strong> AllClaimsTotal dollar amount <strong>of</strong> claims billed for eachdefined statusL Subtotal Amount Paid Amount paid for each defined statusM Amount <strong>of</strong> Deposit Total check amount for claims paid on thisRemittance AdviceN EOB Code Explanation <strong>of</strong> benefits (EOB) code or denial codeO EOB Description Description <strong>of</strong> the denial EOBPNumber <strong>of</strong> ClaimsPosting EOBNumber <strong>of</strong> claims that denied for the EOB codedescribedQ Total Billed Amt. Total amount billed to <strong>Iowa</strong> Medicaid for claims inthis status sectionR Total Other Sources Third party insurance payment or spenddownamount applied for claims in this status sectionS Total Paid by Mcaid Total amount paid by Medicaid for claims in thisstatus sectionT Copay Amt. Members’ copayment amount (applied per date <strong>of</strong>service, when applicable) for claims in this status
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage124DateAugust 1, 2013Field NameField Description1 Patient Name Name <strong>of</strong> the member as shown on the MedicalAssistance Eligibility Card (last name and firstinitial)2 Recipient Ident Num Member identification number (7 digits+letter)3 Trans-Control-Number4 Dispense Date Date <strong>of</strong> service5 National Drug Code 11-digit NDC number6 Sub Units Number <strong>of</strong> units billed7 Rx No. Prescription number17-digit transaction control number assigned toeach claim8 Billed Amt. Total amount billed to <strong>Iowa</strong> Medicaid for this claim9 Other Sources Third party insurance payment or spenddownamount applied to this claim10 Paid by Mcaid Total amount paid by Medicaid on this claim11 Copay Amt. Member’s copay amount (applied per date <strong>of</strong>service, when applicable)12 S Source <strong>of</strong> payment. Allowed charge source codesare as follows:A AnesthesiaB Billed chargeC Percentage <strong>of</strong> chargesD Inpatient per diem rateE EAC priced plus dispense feeF Fee scheduleG FMAC priced plus dispense feeH Encounter rateI Prior authorization rateK DeniedL Maximum suspend ceilingM <strong>Manual</strong>ly pricedN <strong>Provider</strong> charge rateO Pr<strong>of</strong>essional componentP Group therapyQ EPSDT total over 17R EPSDT total under 18S EPSDT partial over 17SP Not yet pricedT EPSDT partial under 18
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage125DateAugust 1, 2013Field NameField DescriptionU Gynecology feeV Obstetrics feeW Child feeX Medicare or coinsurance deductiblesY Immunization replacementZ Batch bill APG0 APG1 No payment APG3 HMO/PHP rate4 System parameter rate5 Statewide per diem6 DRG auth or new7 Inlier/outlier adjust8 DRG ADR inlier9 DRG ADR13 EOB Explanation <strong>of</strong> benefits (EOB) code, if denied. Adescription <strong>of</strong> the code can be found on thesummary page <strong>of</strong> the Remittance Advice (Field O).14 Practitioner Name <strong>of</strong> prescribing provider15 Drug Name Name and dosage <strong>of</strong> drug dispensed16 Adj-R Reason code indicating the reason for theadjustment17 TCN-to-Credit 17-digit TCN number <strong>of</strong> the claim being credited