Prescribed Drugs Provider Manual - Iowa Department of Human ...
Prescribed Drugs Provider Manual - Iowa Department of Human ...
Prescribed Drugs Provider Manual - Iowa Department of Human ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
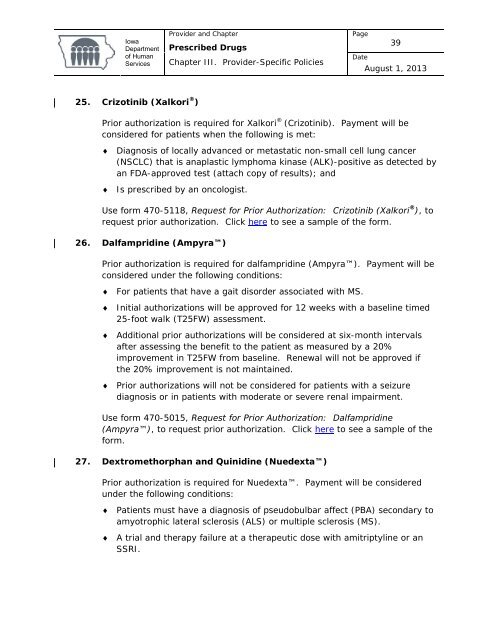
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage39DateAugust 1, 201325. Crizotinib (Xalkori ® )Prior authorization is required for Xalkori ® (Crizotinib). Payment will beconsidered for patients when the following is met:♦ Diagnosis <strong>of</strong> locally advanced or metastatic non-small cell lung cancer(NSCLC) that is anaplastic lymphoma kinase (ALK)-positive as detected byan FDA-approved test (attach copy <strong>of</strong> results); and♦ Is prescribed by an oncologist.Use form 470-5118, Request for Prior Authorization: Crizotinib (Xalkori ® ), torequest prior authorization. Click here to see a sample <strong>of</strong> the form.26. Dalfampridine (Ampyra)Prior authorization is required for dalfampridine (Ampyra). Payment will beconsidered under the following conditions:♦ For patients that have a gait disorder associated with MS.♦ Initial authorizations will be approved for 12 weeks with a baseline timed25-foot walk (T25FW) assessment.♦ Additional prior authorizations will be considered at six-month intervalsafter assessing the benefit to the patient as measured by a 20%improvement in T25FW from baseline. Renewal will not be approved ifthe 20% improvement is not maintained.♦ Prior authorizations will not be considered for patients with a seizurediagnosis or in patients with moderate or severe renal impairment.Use form 470-5015, Request for Prior Authorization: Dalfampridine(Ampyra), to request prior authorization. Click here to see a sample <strong>of</strong> theform.27. Dextromethorphan and Quinidine (Nuedexta)Prior authorization is required for Nuedexta. Payment will be consideredunder the following conditions:♦ Patients must have a diagnosis <strong>of</strong> pseudobulbar affect (PBA) secondary toamyotrophic lateral sclerosis (ALS) or multiple sclerosis (MS).♦ A trial and therapy failure at a therapeutic dose with amitriptyline or anSSRI.