Prescribed Drugs Provider Manual - Iowa Department of Human ...
Prescribed Drugs Provider Manual - Iowa Department of Human ...
Prescribed Drugs Provider Manual - Iowa Department of Human ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
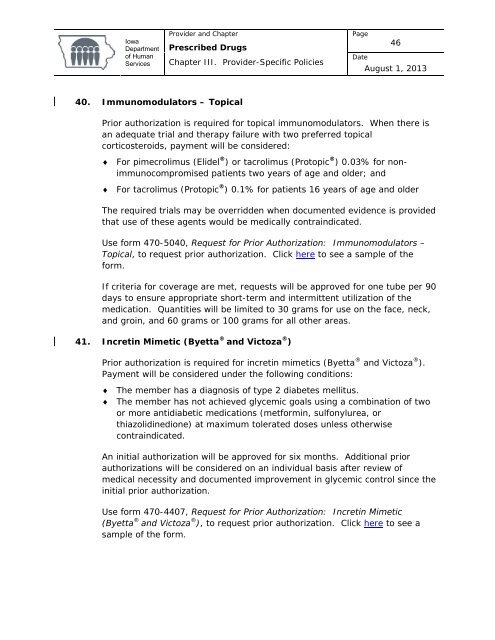
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage46DateAugust 1, 201340. Immunomodulators – TopicalPrior authorization is required for topical immunomodulators. When there isan adequate trial and therapy failure with two preferred topicalcorticosteroids, payment will be considered:♦ For pimecrolimus (Elidel ® ) or tacrolimus (Protopic ® ) 0.03% for nonimmunocompromisedpatients two years <strong>of</strong> age and older; and♦ For tacrolimus (Protopic ® ) 0.1% for patients 16 years <strong>of</strong> age and olderThe required trials may be overridden when documented evidence is providedthat use <strong>of</strong> these agents would be medically contraindicated.Use form 470-5040, Request for Prior Authorization: Immunomodulators –Topical, to request prior authorization. Click here to see a sample <strong>of</strong> theform.If criteria for coverage are met, requests will be approved for one tube per 90days to ensure appropriate short-term and intermittent utilization <strong>of</strong> themedication. Quantities will be limited to 30 grams for use on the face, neck,and groin, and 60 grams or 100 grams for all other areas.41. Incretin Mimetic (Byetta ® and Victoza ® )Prior authorization is required for incretin mimetics (Byetta ® and Victoza ® ).Payment will be considered under the following conditions:♦ The member has a diagnosis <strong>of</strong> type 2 diabetes mellitus.♦ The member has not achieved glycemic goals using a combination <strong>of</strong> twoor more antidiabetic medications (metformin, sulfonylurea, orthiazolidinedione) at maximum tolerated doses unless otherwisecontraindicated.An initial authorization will be approved for six months. Additional priorauthorizations will be considered on an individual basis after review <strong>of</strong>medical necessity and documented improvement in glycemic control since theinitial prior authorization.Use form 470-4407, Request for Prior Authorization: Incretin Mimetic(Byetta ® and Victoza ® ), to request prior authorization. Click here to see asample <strong>of</strong> the form.