Prescribed Drugs Provider Manual - Iowa Department of Human ...
Prescribed Drugs Provider Manual - Iowa Department of Human ...
Prescribed Drugs Provider Manual - Iowa Department of Human ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
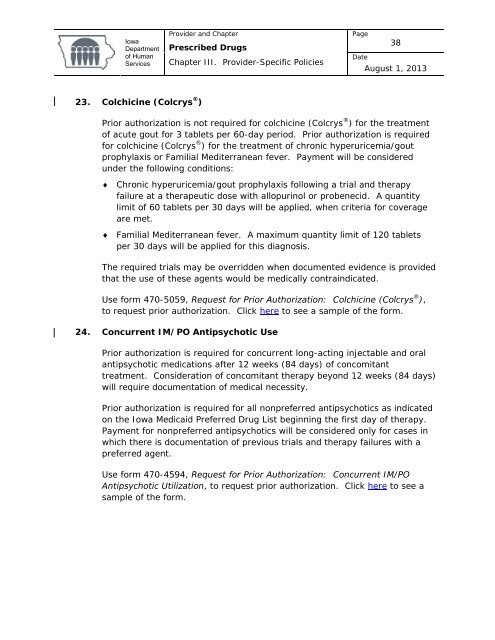
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage38DateAugust 1, 201323. Colchicine (Colcrys ® )Prior authorization is not required for colchicine (Colcrys ® ) for the treatment<strong>of</strong> acute gout for 3 tablets per 60-day period. Prior authorization is requiredfor colchicine (Colcrys ® ) for the treatment <strong>of</strong> chronic hyperuricemia/goutprophylaxis or Familial Mediterranean fever. Payment will be consideredunder the following conditions:♦ Chronic hyperuricemia/gout prophylaxis following a trial and therapyfailure at a therapeutic dose with allopurinol or probenecid. A quantitylimit <strong>of</strong> 60 tablets per 30 days will be applied, when criteria for coverageare met.♦ Familial Mediterranean fever. A maximum quantity limit <strong>of</strong> 120 tabletsper 30 days will be applied for this diagnosis.The required trials may be overridden when documented evidence is providedthat the use <strong>of</strong> these agents would be medically contraindicated.Use form 470-5059, Request for Prior Authorization: Colchicine (Colcrys ® ),to request prior authorization. Click here to see a sample <strong>of</strong> the form.24. Concurrent IM/PO Antipsychotic UsePrior authorization is required for concurrent long-acting injectable and oralantipsychotic medications after 12 weeks (84 days) <strong>of</strong> concomitanttreatment. Consideration <strong>of</strong> concomitant therapy beyond 12 weeks (84 days)will require documentation <strong>of</strong> medical necessity.Prior authorization is required for all nonpreferred antipsychotics as indicatedon the <strong>Iowa</strong> Medicaid Preferred Drug List beginning the first day <strong>of</strong> therapy.Payment for nonpreferred antipsychotics will be considered only for cases inwhich there is documentation <strong>of</strong> previous trials and therapy failures with apreferred agent.Use form 470-4594, Request for Prior Authorization: Concurrent IM/POAntipsychotic Utilization, to request prior authorization. Click here to see asample <strong>of</strong> the form.