Prescribed Drugs Provider Manual - Iowa Department of Human ...
Prescribed Drugs Provider Manual - Iowa Department of Human ...
Prescribed Drugs Provider Manual - Iowa Department of Human ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
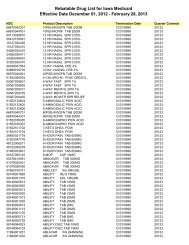
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage110DateAugust 1, 20136. Override CodesA 72-hour emergency supply <strong>of</strong> medication may be dispensed using priorauthorization type code “1” as a point <strong>of</strong> sale override. The provision for a72-hour supply can be used in an emergency situation only one time permember, per drug.A seven-day override <strong>of</strong> the prior authorization requirement will be allowedwhile the prescriber is requesting prior authorization for certain mental healthdrugs. The override applies to drugs that are deemed to have a significantvariation in therapeutic or side effect pr<strong>of</strong>ile from other drugs in the sametherapeutic class. See the Preferred Drug List at: www.iowamedicaidpdl.comThe pharmacy may use a prior authorization type code “7” as a point <strong>of</strong> saleoverride for applicable mental health drugs. The seven-day provision can beused only one time per member, per NDC, per 30 days.7. Proper Reporting <strong>of</strong> NDCsThe <strong>Iowa</strong> Medicaid Program can cover only drugs from manufacturers whohave signed national Medicaid drug rebate agreements with the Centers forMedicare and Medicaid Services (CMS). Drug companies sign the agreementsfor specific drug manufacturer codes called national drug codes (NDC).Since rebates are determined by <strong>Iowa</strong> Medicaid’s utilization data, it isimperative that pharmacies and providers bill <strong>Iowa</strong> Medicaid using the correctNDC number <strong>of</strong> the drug actually dispensed or administered.If a provider is dispensing or administering one drug and billing for an NDCdifferent from the drug being dispensed or administered, it is consideredfraud, which can result in claims being recouped, sanctions, and termination<strong>of</strong> provider agreements. The Program Integrity Unit will be monitoring forthis in their reviews.