Prescribed Drugs Provider Manual - Iowa Department of Human ...
Prescribed Drugs Provider Manual - Iowa Department of Human ...
Prescribed Drugs Provider Manual - Iowa Department of Human ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
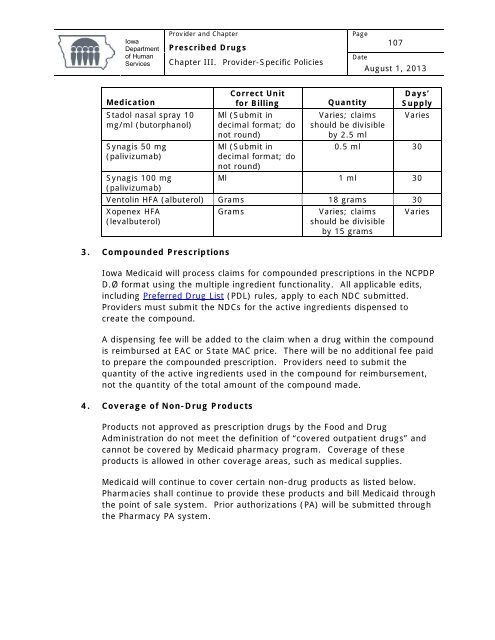
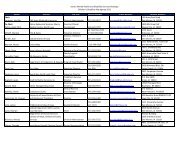
<strong>Iowa</strong><strong>Department</strong><strong>of</strong> <strong>Human</strong>Services<strong>Provider</strong> and Chapter<strong>Prescribed</strong> <strong>Drugs</strong>Chapter III. <strong>Provider</strong>-Specific PoliciesPage107DateAugust 1, 2013MedicationStadol nasal spray 10mg/ml (butorphanol)Synagis 50 mg(palivizumab)Correct Unitfor BillingMl (Submit indecimal format; donot round)Ml (Submit indecimal format; donot round)Days’Quantity SupplyVaries; claims Variesshould be divisibleby 2.5 ml0.5 ml 30Synagis 100 mgMl 1 ml 30(palivizumab)Ventolin HFA (albuterol) Grams 18 grams 30Xopenex HFA(levalbuterol)3. Compounded PrescriptionsGramsVaries; claimsshould be divisibleby 15 gramsVaries<strong>Iowa</strong> Medicaid will process claims for compounded prescriptions in the NCPDPD.Ø format using the multiple ingredient functionality. All applicable edits,including Preferred Drug List (PDL) rules, apply to each NDC submitted.<strong>Provider</strong>s must submit the NDCs for the active ingredients dispensed tocreate the compound.A dispensing fee will be added to the claim when a drug within the compoundis reimbursed at EAC or State MAC price. There will be no additional fee paidto prepare the compounded prescription. <strong>Provider</strong>s need to submit thequantity <strong>of</strong> the active ingredients used in the compound for reimbursement,not the quantity <strong>of</strong> the total amount <strong>of</strong> the compound made.4. Coverage <strong>of</strong> Non-Drug ProductsProducts not approved as prescription drugs by the Food and DrugAdministration do not meet the definition <strong>of</strong> “covered outpatient drugs” andcannot be covered by Medicaid pharmacy program. Coverage <strong>of</strong> theseproducts is allowed in other coverage areas, such as medical supplies.Medicaid will continue to cover certain non-drug products as listed below.Pharmacies shall continue to provide these products and bill Medicaid throughthe point <strong>of</strong> sale system. Prior authorizations (PA) will be submitted throughthe Pharmacy PA system.