Quality control of blood irradiation - ResearchGate
Quality control of blood irradiation - ResearchGate
Quality control of blood irradiation - ResearchGate
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
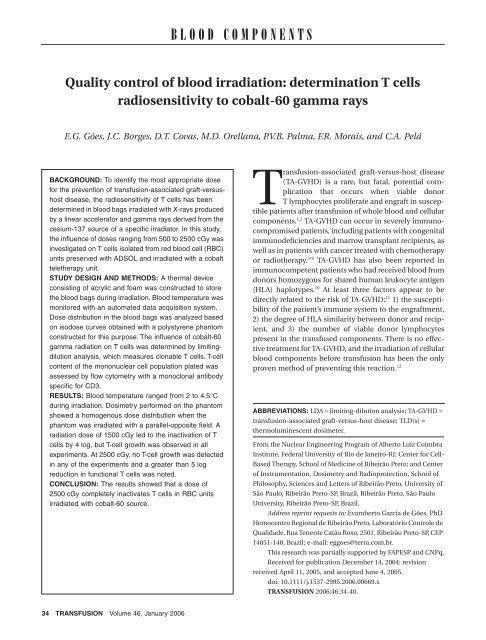
GÓES ET AL.Fig. 4. Isodose curves obtained at the central plane when thephantom was irradiated with parallel-opposed fields.Fig. 6. Reduction in functional T cells, as a function <strong>of</strong> the radiationdose used, represented by a sigmoidal function.DISCUSSIONFig. 5. Percentage <strong>of</strong> viable T cells (CD3+ cells) on Day 0 assessedby flow cytometry.1:46-1:649). At 1000 cGy, the mean T-cell growth was 1 in2372 (range, 1:1056-1:4336). When cells were irradiatedwith a dose <strong>of</strong> 1500 cGy, the mean growth decreased to 1in 128,821 (range, 1:34,175–1:208,017), with T-cell growthbeing observed in all experiments. At 2000 cGy, no T-cellgrowth was observed in wells containing less than 2 × 10 6cells per well in any <strong>of</strong> the three experiments, correspondingto a reduction in the growth potential <strong>of</strong> T cells <strong>of</strong> morethan 5 log. No T-cell growth was observed in any <strong>of</strong> thethree experiments at 2500 cGy. At this dose, the meangrowth was less than 1 in 10 6 plated cells, correspondingto a reduction in the T-cell growth <strong>of</strong> more than 5.4 log.The results <strong>of</strong> T-cell inactivation as a function <strong>of</strong> the doseare summarized in Fig. 6.The prevention <strong>of</strong> TA-GVHD by the <strong>irradiation</strong> <strong>of</strong> <strong>blood</strong>components before transfusion is based on the fact that<strong>irradiation</strong> produces T-cell damage at a magnitude sufficientto inhibit their proliferative abilities and thereforetheir ability to respond to allogeneic cells. The ideal dosenecessary to prevent TA-GVHD while preserving the quality<strong>of</strong> other <strong>blood</strong> cells, excluding the lymphocytes, continuesto be an issue. A dose as little as 500 cGy canattenuate the response <strong>of</strong> lymphocytes to allogeneic cellsin a mixed lymphocyte culture, and 1500 cGy can reducethe response to mitogen-induced stimulation by 90-99 percent, representing a sensitivity lower than 2 log. 27-29In the past, based on data about the elimination <strong>of</strong> allogeneicreactivity in the mixed lymphocyte culture, the use atleast 1500 cGy was recommended. 29 Three cases <strong>of</strong> TA-GVHD have been reported in patients who received <strong>blood</strong>irradiated with doses between 1500 and 2000 cGy by use<strong>of</strong> a specific <strong>blood</strong> irradiator and a linear accelerator. 30-32Dosimetric procedures necessary to verify the dose deliveredin the <strong>blood</strong> bags, however, were not applied in thesecases.Recently, two studies with LDA assay indicated that2500 cGy was the minimal dose necessary for TA-GVHDprevention. 18,19 One <strong>of</strong> those studies tested the effects <strong>of</strong>gamma rays emitted by the 137 Cs source <strong>of</strong> a <strong>blood</strong> irradiator,and X-rays emitted by an linear accelerator, onT cells when delivered in situ to ADSOL-preserved RBCunits in PL-146 and PL-2209 plastic containers. 18 The38 TRANSFUSION Volume 46, January 2006
60Co IRRADIATION INACTIVATES T CELLS IN RBC UNITSother study tested the effect <strong>of</strong> gamma rays emitted by the137Cs source <strong>of</strong> a <strong>blood</strong> irradiator on T cells when deliveredin situ to plateletpheresis units in the PL-732 plasticcontainer. 19In this study, we focused our attention on the determination<strong>of</strong> T-cell radiosensitivity to 60 Co gamma rays tobetter delineate the minimal dose needed to inactivateT cells when irradiating RBC with a cobalt teletherapyunit. We used the LDA assay, which is the most sensitivemethod previously employed to determine functionalT cells after T-cell depletion for the prevention <strong>of</strong> GVHDin the setting <strong>of</strong> marrow transplantation. 20-23 In our studies,the phantom consisting <strong>of</strong> standard material providedinformation regarding the dose distribution in the irradiated<strong>blood</strong> volume and permitted us to establish inadvance the geometry <strong>of</strong> <strong>irradiation</strong> that would minimizedose heterogeneity in the volume irradiated. The minimization<strong>of</strong> dose-distribution heterogeneity is important toavoid subdosage, or overdosage, <strong>of</strong> some <strong>of</strong> the <strong>blood</strong>cells.The present LDA results demonstrated T-cell growthin all experiments for cells irradiated with a dose <strong>of</strong>1500 cGy. As can be seen in Fig. 6, the slope <strong>of</strong> the curveat first increases slowly between 500 and 1000 cGy andthen becomes fairly straight between 1000 and 1500 cGy(i.e., maximal reduction in functional T cells per doserange), and finally decreases at doses higher then2000 cGy. At 2500 cGy, reduction in functional T cellsreached a plateau, suggesting the detection limit <strong>of</strong> theLDA method. We found that a gamma <strong>irradiation</strong> dose <strong>of</strong>2500 cGy may be required to completely inactivate T cellsin RBC units when a 60 Co source is used. The LDA <strong>of</strong> T cellsirradiated with a similar dose delivered either by the 137 Cssource <strong>of</strong> a specific irradiator or by X-rays produced by alinear accelerator has shown that a dose <strong>of</strong> 2500 cGyreduces functional T cells by more than 5 log. 18,19 Thesefindings are in agreement with the present LDA results.Thus, the results obtained in this study on the radiosensitivity<strong>of</strong> T cells to gamma rays delivered by a 60 Co sourcesupport the use <strong>of</strong> 2500 cGy as the appropriate dose toprevent TA-GVHD.When <strong>irradiation</strong> is performed with a specific <strong>blood</strong>irradiator, the dose necessary for TA-GVHD prevention isreleased within a few minutes. When a linear acceleratoror cobalt teletherapy unit is used for this task, however,the entire <strong>irradiation</strong> process is completed within 30 to60 minutes. In such cases, the <strong>blood</strong> components remainat room temperature (approx. 23°C) during the <strong>irradiation</strong>process. A thermal device that provides appropriatestorage conditions during the <strong>irradiation</strong> <strong>of</strong> <strong>blood</strong> componentswith a teletherapy unit has been recently proposed.17 Because <strong>of</strong> the dimensions <strong>of</strong> this device (20 cmin diameter and 20 cm in height), however, the dose distributionin the volume is more heterogeneous, and thereforewe decided to build a more appropriate thermaldevice to store the <strong>blood</strong> bags during the process <strong>of</strong> <strong>irradiation</strong>used in this experiments. The method used tostore the <strong>blood</strong> bags guaranteed that the temperature <strong>of</strong>the RBC units would be kept below 4.5°C during <strong>irradiation</strong>,ensuring that all damage caused to the cells studiedwas exclusively due to the action <strong>of</strong> radiation at the differentdoses applied.ACKNOWLEDGMENTSThe authors thank Thomaz Ghilardi Netto, PhD, Elisa A. Reis,Maria Helena da Silva, Marcos Vasques, José Luiz Aziani, DilmaFreire, and Aurea T. Souza, for their technical assistance.REFERENCES1. Kerman NA, Collins NH, Juliano L, et al. Clonable Tlymphocytes in T cell-depleted bone marrow transplantscorrelate with development <strong>of</strong> graft-v-host disease. Blood1986;68:770-3.2. Przepiorka D, LeParc GF, Stovall MA, et al. Use <strong>of</strong> irradiated<strong>blood</strong> components: practice parameter. Am Clin Pathol1996;106:6-11.3. Thomaz ED, Herman EC, Greenough WB. Irradiation andmarrow infusion in leukemia. Arch Intern Med 1961;107:829-45.4. Parkman R, Mosier D, Umansky I, et al. Graft-versus hostdisease after intrauterine and exchange transfusions forhemolytic disease <strong>of</strong> the newborn. N Engl J Med 1974;290:359-63.5. Von Fliedner V, Higby DJ, Kim U. Graft-versus-host reactionfollowing <strong>blood</strong> transfusion. Am J Med 1982;72:951-9.6. Brubaker DB. Human postransfusion graft-versus-hostdisease. Vox Sang 1983;45:401-20.7. Anderson KC, Weinstein HJ. Transfusion-associated graftversus-hostdisease. N Engl J Med 1990;332:315-21.8. Greenbaum B. Transfusion-associated graft-versus-hostdisease: historical perspectives, incidence, and current use<strong>of</strong> irradiated <strong>blood</strong> products. J Clin Oncol 1991;9:1889-902.9. Jamieson NV, Joysey V, Friend PJ, et al. Graft-versus-hostdisease in solid organ transplantation. Transplant Int1991;4:67-71.10. Thaler M, Shamiss A, Orgad S, et al. The role <strong>of</strong> <strong>blood</strong> fromHLA-homozygous donors in fatal transfusion-associatedgraft-versus-host disease after open heart surgery. N Engl JMed 1989;321:25-8.11. Ferrara JL, Deeg HJ. Graft-versus-host disease. N Engl J Med1991;324:667-74.12. Chapman J, Finney RD, Formam K. Guide on gamma<strong>irradiation</strong> <strong>of</strong> <strong>blood</strong> components for prevention <strong>of</strong>transfusion-associated graft-versus-host disease.Transfusion 1996;6:261-71.13. Anderson KC, Goodnough LT, Sayers M, et al. Variation in<strong>blood</strong> component <strong>irradiation</strong> practice: implication forVolume 46, January 2006 TRANSFUSION 39
GÓES ET AL.prevention <strong>of</strong> transfusion-associated graft-versus-hostdisease. Blood 1991;77:2096-102.14. Mor<strong>of</strong>f G, Luban NLC. The <strong>irradiation</strong> <strong>of</strong> <strong>blood</strong> and <strong>blood</strong>components to prevent graft-versus-host disease: technicalissues and guidelines. Transfus Med 1997;11:15-26.15. Patton GA, Skowronski MG. Implementation <strong>of</strong> a <strong>blood</strong><strong>irradiation</strong> program at a community cancer center.Transfusion 2001;41:1610-4.16. Chen F, Covas DT, Baffa O. Dosimetry <strong>of</strong> <strong>blood</strong> <strong>irradiation</strong>using an alanine/ESR dosimeter. Appl Radiat Isot 2001;55:13-6.17. Góes EG, Covas DT, Haddad R, et al. <strong>Quality</strong> <strong>control</strong> systemfor <strong>blood</strong> <strong>irradiation</strong> using a teletherapy unit. Vox Sang2004;86:105-10.18. Pelszynski MM, Mor<strong>of</strong>f G, Luban NL, et al. Effect <strong>of</strong> gamma<strong>irradiation</strong> <strong>of</strong> red <strong>blood</strong> cell units on T-cell inactivation asassessed by limiting dilution analysis: implication forpreventing transfusion-associated graft-versus-hostdisease. Blood 1994;83:1683-9.19. Luban NL, Drothler D, Mor<strong>of</strong>f G, Quinones R. Irradiation <strong>of</strong>platelet components: inhibition <strong>of</strong> lymphocyte proliferationassessed by limiting-dilution analysis. Transfusion 2000;40:348-52.20. Taswell C. Limiting dilution assays for the determination <strong>of</strong>immunocompetent cell frequencies. I. Data analysis.J Immunol 1981;126:1614-9.21. Kernan NA, Flomenberg N, Collins NH, et al. Quantitation<strong>of</strong> T lymphocytes in human bone marrow by a limitingdilution assay. Transplantation 1985;40:317-22.22. Moretta A, Pantaleo G, Moretta L, et al. Direct demonstration<strong>of</strong> the clonogenic potential <strong>of</strong> every human peripheral <strong>blood</strong>T cell: clonal analysis <strong>of</strong> HLA-DR expression and cytolyticactivity. J Exp Med 1985;157:743-54.23. Quinones RR, Gutierrez RH, Dinndorf PA, et al.Extended-cycle elutriation to adjust T-cell content inHLA-disparate bonne marrow transplantation. Blood1993;82:307-17.24. Andreo P, Cunningham JR, Hohlfeld K, et al. Absorbed dosedetermination in photon and electron beams: aninternational code <strong>of</strong> practice. Technical Reports Series277.Vienna: International Atomic Energy Agency; 1987.25. White DR, Booz J, Griffith RV, et al. Tissue substitute inradiation dosimetry and measurement. Report 44. Bethesda:International Commission on Radiation Units andMeasurements; 1989.26. Press WH, Flannery BP, Teukolsky SA, et al. Numericalrecipes in Pascal: the art <strong>of</strong> scientific computing. New York:Cambridge University Press; 1997.27. Sprent J, Anderson RE, Miller JF. Radiosensitivity <strong>of</strong> T and Blymphocytes. II. Effect <strong>of</strong> <strong>irradiation</strong> on response <strong>of</strong> T cellsto alloantigens. Eur J Imunol 1974;4:204-10.28. Valerius NH, Johansen KS, Nielsen OS, et al. Effect <strong>of</strong> in vitrox-<strong>irradiation</strong> on lymphocyte and granulocyte function.Scand J Haematol 1981;27:9-18.29. Rosen NR, Weidner JG, Boldt HD, et al. Prevention <strong>of</strong>transfusion-associated graft-versus-host disease: selection<strong>of</strong> an adequate dose <strong>of</strong> gamma <strong>irradiation</strong>. Transfusion1993;33:125-7.30. Dobrynski W, Thibodeau S, Truitt RL, et al. Third-partymediatedgraft rejection and graft-versus-host diseaseafter T-cell-depleted bone marrow transplantation asdemonstrated by hypervariable DNA probes and HLA-DRpolymorphism. Blood 1989;74:2285-94.31. Lowenthal RM, Challis DR, Griffiths AE, et al. Transfusionassociatedgraft-versus-host disease: report <strong>of</strong> a casefollowing administration <strong>of</strong> irradiated <strong>blood</strong>. Transfusion1993;33:524-9.32. Sproul AM, Chalmers EA, Mills KI, et al. Third partymediated graft rejection despite <strong>irradiation</strong> <strong>of</strong> <strong>blood</strong>products. Br J Haematol 1992;80:261-2.40 TRANSFUSION Volume 46, January 2006