Serious Untoward Incident Policy - Health Partnerships Learning ...
Serious Untoward Incident Policy - Health Partnerships Learning ...
Serious Untoward Incident Policy - Health Partnerships Learning ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
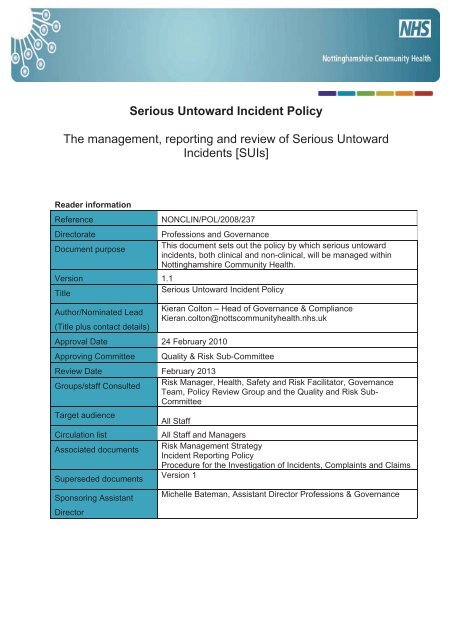
1. <strong>Policy</strong> Statement1.1 This policy determines how serious untoward incidents (hereafter referred to as SUIs),both clinical and non-clinical, will be managed across Nottinghamshire Community <strong>Health</strong>(NCH). The organisation will put in place effective mechanisms for managing and monitoringserious untoward incidents. It is the responsibility of the Governance Committee (NCH) toreceive summary reports from serious incident reviews and to be assured that wherenecessary, new procedures are developed and reviewed to prevent reoccurrence.1.2 This <strong>Policy</strong> is related to the Care Quality Commission registration regulations and alsothe NHS Litigation Authority Risk Management Standards for Primary Care Trusts.1.3 Nottinghamshire Community <strong>Health</strong> has a fair and open culture (Appendix A) and asupportive approach to dealing with serious incidents. Rather than seeking to assign blamethe emphasis is that the occurrence of an incident, however serious, is not in itself evidenceof neglect, carelessness or dereliction of duty. Only if evidence emerges of breaches of law,[Criminal or Civil], professional standards, codes of conduct or repeated poor performancewill disciplinary action be considered.1.4 Nottinghamshire Community <strong>Health</strong> will ensure that as far as reasonably practicableinformation regarding SUIs is provided to patients as soon as possible and also ifappropriate, to relatives and other stakeholders. (Appendix B: Quick Reference Guide toBeing Open)2. <strong>Policy</strong> Scope2.1 The policy covers all NCH employed staff whatever their role or location and isapplicable to others working within NCH premises. The <strong>Policy</strong> outlines the overarchingprinciples associated with the management of SUIs.3. <strong>Policy</strong> Purpose3.1 The purpose of this policy is promote consistent management, reporting, review andlearning from an SUI.3.2 This policy aims to give guidance to staff who are alerted to a SUI and theirresponsibilities. The <strong>Policy</strong> appendices provide specific operational guidance in themanagement of SUIs.3.3 To provide a framework to ensure consistent management of SUIs.4. <strong>Policy</strong> objectives4.1 The objectives of this policy are to ensure: A widely understood definition of a serious untoward incident That a serious untoward incident is declared and reported in a timely manner andappropriately managed There is appropriate reporting both internally and externally when a SUI has takenplace Clear lines of reporting and accountability That a thorough investigation (using root cause analysis techniques) of a SUI iscarried out and actions are implemented to ensure learning.3
An accident occurring on NHS premises that resulted in serious injury, major orpermanent harm or death (or the risk of) to a patient, member of staff, contractoror member of the public.The actions of staff providing NHS funded care that are likely to cause significantpublic concern i.e. serious instances of abuse (physical/sexual/mental).An event that might adversely impact on the delivery of services causing urgentinvocation of the Trusts business continuity plan, initiation of the major incidentpolicy or may reflect a serious breach of standards.NB: Any media issue that is not related to a serious incident must not bereported through STEIS but through relevant communication teams.Any incident which meets the definition of a SUI must be reported via STEIS within 24 hoursof becoming aware of the event. Where it is uncertain whether an incident is a SUI,discussions with the relevant commissioning PCT should take place for clarity.Please refer to Appendix C – Deciding whether an incident is a SUI7. SUI reporting7.1 Once a SUI is considered a possibility, the information must be passed through the linemanagement chain up to and including Managers and Assistant Directors, NCHHeadquarters and the Head of Communications. In all cases where a SUI is reported theAssistant Director of Professions and Governance will be notified as soon as possible. Thereshould be no delay in reporting to the appropriate Assistant Director even if a Line manageris unavailable.7.2 A specific minimum amount of initial data is required for SUI reporting. [Appendix E –Initial Data Set Capturing Immediate Dataset]7.3 All NHS organisations, are required to report all SUIs to East Midlands SHA using thenational reporting system known as STEIS / UNIFY. The SHA provides a central point for thehealth community where information about SUIs will be recorded, monitored, analysed andlearning disseminated. Additionally, the SHA requires this information to be able to supportthe PCTs to appropriately manage the media and brief Ministers accordingly. Depending onthe incident, the SHA may need to work alongside NCH in communicating with otherstakeholders. The SHA may also be able to provide objective advice on a range of issues. InAddition all SUI’s relating to NCH will be reviewed and monitored by NHS NottinghamshireCounty as part of their role as commissioners of our services.7.4 Where the incident has occurred within Nottinghamshire Community <strong>Health</strong> Services theGovernance department will be responsible for reporting the SUI to NHS NottinghamshireCounty and the East Midlands SHA. The responsibility for reporting lies with SeniorManagers and Assistant Directors within the Governance Department.7.5 Where an SUI occurs ‘Out of Hours’ follow on call procedures to immediately contact oncall Managers and Assistant Directors by calling 0115 934 3236.8. Responsibilities8.1 All staff are responsible for adhering to NCH <strong>Policy</strong> and reporting all adverse events,including those regarded as SUIs in an appropriate and timely manner.5
9 Investigating SUIs9.1 See Section A: NCH – <strong>Serious</strong> <strong>Untoward</strong> <strong>Incident</strong> Process (Page 8)10. External stakeholder reporting arrangements10.1 There are a number of external agencies who require information about SUIs andwhere other agencies (e.g. NHS Nottinghamshire County, Social Services, GPs, <strong>Health</strong> andSafety Executive, Police, Home Office, legal advisors, Area Child Protection Committee,NHS Litigation Authority, National Patient Safety Agency) have a legitimate reason to beinformed of a SUI.NCH will comply with the Memorandum of Understanding (Feb 2006) jointly publishedbetween the NHS, Police and HSE when a joint investigation is needed to investigate apatient death or serious incident.10.2 The following events have separate reporting mechanisms but may also need to betreated as a SUI, and reported to other stakeholders by the Managing Director for NCH orone of the Assistant Director’s: Major <strong>Incident</strong> Plans are separate and NCH will work with the lead Trust to manage aMajor <strong>Incident</strong> in which NCH services are involved/required Estates incidents which affect the health, safety and/or welfare of patients, staff andvisitors or which damage NHS property or facilities resulting in disruption to servicese.g. fire, water/power failure, flood. (See Business Continuity Plan and report to NHSEstates via Chief Operating Officer NCH)Reporting of Communicable Diseases. (Discuss with <strong>Health</strong> Protection Agency).Medical Device Adverse <strong>Incident</strong>s which are or have the potential to be a risk topatients, staff, users or other person’s safety (Medicines and <strong>Health</strong>care productsRegulatory Agency MHRA)<strong>Policy</strong> on Public Interest Disclosure (Whistleblowing) <strong>Policy</strong> – guidance on whataction staff should take in the event of discovery or suspicion of fraudulent activity,either by another member of staff or by one of the NCH suppliers is contained in thispolicy.See Appendix F for External Reporting details11. <strong>Learning</strong> from SUIs11.1 The importance of learning from SUIs to ensure they do not reoccur is fundamental todeveloping quality services and minimising risk to patients, staff and the organisation.11.2 The NCH SUI Lead will ensure that any SUI trends are reviewed in the GovernanceTeam and Governance Committee, and reported to the Board where required.Recommendations and changes to practice will be disseminated to the wider NCH throughappropriate channels to enable organisational and clinical improvements to be achieved as aconsequence.11.3 It is particularly important that NCH learns from investigations into serious untowardincidents. NCH needs to ensure that their staff, are genuinely encouraged in performanceimprovement and this culture needs to pervade the review process and be paid specialattention at the conclusion of a review.6
12. Key performance indicators12.1 A high level summary of SUIs will be reported to each of the Governance Committeemeetings and via this mechanism to the NHS Nottinghamshire County – GovernanceCommittee. The Governance Committee will also receive an Annual SUI report based onthemes and outcomes.12.2 SUIs will be a feature of the Annual Risk Management Report and identify the mostsignificant risks facing NCH.12.3 NCH will have in place a means of ‘independent assurance’ through the ManagingBoard and Governance Committee responsible for reviewing NCH’s establishment andmaintenance of an effective system of internal control and risk management of SUIs. Thesecommittee’s will provide verification to the Managing Board that the systems in place areclearly defined and working effectively within the organisation.12.4 A statement from Internal Audit, who undertakes periodic audits of the internal controlmechanisms, will be provided to the Managing Board and the PCT Board on theeffectiveness of the risk management control mechanisms.13. Dissemination13.1 This policy and guidelines will be communicated to all staff through an identified policyratification and dissemination process. It will be cascaded through the organisation throughthe Assistant Directors, General Manager and Locality Service Managers. It will also beplaced on the NCH Intranet Site.14. Conclusion14.1 This policy states and confirms NCH’s commitment to the importance of effectivemanagement of <strong>Serious</strong> <strong>Untoward</strong> <strong>Incident</strong>s. In conjunction with the other Risk ManagementPolicies it sets out the key elements of NCH’s risk management approach to secure effectiveidentification and management of its risks. The Risk Management Strategy sets out theframework and specific systems and processes for implementation for risk management.15. <strong>Policy</strong> ReviewThis policy will be reviewed every three years or as and when organisational change orlegislation determines.16. <strong>Policy</strong> Audit toolThe implementation of this <strong>Policy</strong> will be monitored as part of the NCH Audit cycle using theaudit tool at Appendix K (SUI <strong>Policy</strong> Audit Tool)17. Equality and DiversityNottinghamshire Community <strong>Health</strong> aims to design and implement services, policies andclinical/non clinical procedures with measures that meet the diverse needs of our service,population and workforce, ensuring that none are placed at a disadvantage over others.All policies and clinical/non clinical procedures should be developed in line with the NHSNotts County Equality and Diversity <strong>Policy</strong> (2008), and need to take into account the diverseneeds of the community that is served.7
18. Bibliography Australia/New Zealand Risk Management Standard: AS/NZS 4360:1999 Assurance: The Board Agenda (August 2002) NPSA Seven Steps to Patient Safety 2003 NPSA toolkit at: http://www.npsa.nhs.uk/health/resources/root_cause_analysis] Standards for Better <strong>Health</strong> DoH 2004 NHSLA PCT Risk Management Standards April 20078
MANAGEMENT OF SUIs: SECTION ANCH <strong>Serious</strong> <strong>Untoward</strong> <strong>Incident</strong> Process:1. Immediate Management of a <strong>Serious</strong> <strong>Untoward</strong> <strong>Incident</strong> [SUI]1.1 The situation must be immediately controlled ensuring the health, safety and welfare ofthose specifically involved.1.2 The incident must be immediately reported through the relevant Line Management Chainduring business hours and through on call mechanisms out of hours. In all cases where aSUI is reported the Assistant Director or Professions and Governance (and in their absencethe Head of Governance and Compliance) will be notified as soon as possible.1.3 Some SUIs may not require immediate investigation but most will require immediatemanagement actions urgently to prevent further harm or damage, preserve evidence and togain the facts. The Duty / nominated Lead Assistant Director will be accountable and actionsmay include: Ensuring patients and relatives are appropriately informed of the SUI and theimmediate steps being taken.Ensuring staff are supported as required.Taking a faulty item of equipment out of action. Any allegedly defective piece ofequipment should be withdrawn from use and kept secure (do not change anysettings or dials). Advice on any biohazard can be obtained from the infection controladvisor.Closing a workplace until repairs can be effected.Sealing / preserving an area and equipment or paperwork to ensure evidence ispreserved.Ensuring appropriate internal managers and external agencies are informed.2. Staff present at incident / discovering incident – responsibilities:2.1 The most senior person at the incident will make arrangements to secure the immediatewell being of patients and other staff and the safety of the workplace or clinical area asappropriate. If necessary this will include calling a Duty Doctor or Ambulance, or specificNCH Managers e.g. Estates, <strong>Health</strong>, Safety & Risk Facilitator and / or Head of Governance& Compliance.2.2 It is the responsibility of the senior person present at the incident (or the personidentifying an incident has occurred) to inform their responsible NCH Assistant Director,normally via the local manager or duty manager, immediately that they believe that a SUIhas occurred, and describe what happened and the initial actions taken.2.3 In the case of potential Police or <strong>Health</strong> and Safety Executive involvement or a potentiallegal claim, the senior person will ensure that the scene is secured and left untouched forfurther investigation and that all equipment and associated disposable items are retainedand preserved, and that the Head of Governance & Compliance for NCH is informed.9
5.6 In the event that an external independent investigation is thought appropriate, theDesignated Director will discuss and agree Terms of Reference with the Managing Directorand the Professional Executive Team.5.7 The Assistant Director (Professions & Governance) will monitor performance against SUIaction plans and will ensure STEIS/UNIFY is regularly updated (and root causes, lessonslearnt and actions taken are completed) and SUIs are closed on STEIS/UNIFY within 60days.All SUI action plans will be monitored for full implementation through the Quality and RiskSub-Committee at each of their meetings.6. SUI Investigation Manager – responsibilities:6.1 The designated SUI Investigation Manager will agree their Terms of Reference for theInvestigation with the Designated Director for the SUI and undertake a detailed investigationof the issue designated as a <strong>Serious</strong> <strong>Untoward</strong> <strong>Incident</strong>.6.2 The Investigation Manager will ensure appropriate communication takes place with theindividuals involved, patients, relatives, staff and Assistant Directors, Head ofCommunications to inform them of progress concerning the investigation.6.3 The investigation Manager will ensure that staff are aware of the Mental Capacity Act2005, which took full effect from 1 October 2007 and of the impact this has both from a legaland clinical perspective. [Refer Mental Capacity Act <strong>Policy</strong>]6.4 A fully anonymised report and Root Cause Analysis [RCA] with recommendations and anaction plan will be produced within 60 days styled on the NCH standard Pro-forma.[Appendix J] Except in circumstances where an external investigation has beencommissioned. This will be provided to the Governance Committee and the ProfessionalExecutive Team.7. Communications - general7.1 The NCH Communications Team must be contacted by the Designated Director as soonas a SUI has been declared in hours or out of hours (depending on the scale of incident andlikely media interest). The minimum data set, (Appendix E), should be used to ensureconsistence of reporting. If the NCH Communications Team is unavailable the SHA willgive/arrange interim communications support.7.2 The NCH Communications team through the Head of Communications will notify theSHA Media and Communications team within 12 hours of the SUI occurring7.3 Following any SUI occurring within NCH, the Head of Communications on behalf of theManaging Director will handle media interest and press statements. In the event of a SUIinvolving other agencies joint press statements should be made available wherever possible.In the event of a SUI, which requires major communication links (e.g. major infrastructurefailure) designated ‘help lines’ may be required. (See Section 7.9 Communication –Establishment of “Hotlines”).7.4 The Designated Director and the Head of Communications will maintain close contactwith NHS Nottinghamshire County and the SHA when there is a need for nationalcoordination in the handling of a particular serious incident and will offer advice in handlingincidents including media relations and preparation of press statements. The SHA will also11
ensure that all who need to be alerted to an incident are informed including appropriateDepartment Of <strong>Health</strong> ministers.7.5 The senior person at the incident should gather initial factual details of the incidentincluding details of any injuries and the treatment given and the outcome of the treatment(e.g. admission to hospital). They should ensure additional information is passed toDesignated Director and therefore the Head of Communications as soon as it becomesavailable. If the incident concerns Safeguarding Children or Protection of Vulnerable Adults[POVA] the Senior Manager of the relevant speciality will discuss with the DesignatedDirector then inform Local Authority Safeguarding / POVA Leads who will subsequentlyadvise NCH on the relevant review process.7.6 The senior person at the incident should also ensure an <strong>Incident</strong> Report Form iscompleted for the Datix Database as per the <strong>Incident</strong> Reporting <strong>Policy</strong>, as soon as the initialsituation is under control or at least within 24hrs of the incident occuring.7.7 The Investigating Manager or designated Senior Manager will ensure appropriatecommunications maintained with all those involved with the SUI: Assistant Directors,Patients, Relatives, Staff and the Head of Communications.7.8 The outcome of the SUI investigation / review: recommendations and lessons learnedwill be shared with stakeholders and the broader NHS as appropriate.7.9 Communication – Establishment of “Hotlines”The hotline process will be governed by a strategy for communicating both internallyand externally. The style and approach used will be dependent on the type ofincident. This strategy will be aimed at: -i) Providing informationii) Reducing untoward concerniii) Providing and creating guidance for callers, allowing them to receivefurther information/treatment/assessment.iv) Reducing potential for incorrect information being in the public domainThis strategy will be developed by the Chief Operating Officer in association with theManaging Director and the Head of Communications for NCH.It will include directions as regards: - Those individuals, who are recognised as being actually or potentially involved inthe incident, will need to be contacted by the hotline. Creation of a list of essential staff to assist in the communication process, forexample, Head of Communications, Patient, Carer and Public EngagementManager, Service Manager, Governance Lead external parties, e.g. PCT and SHA Ensuring that care is taken to keep the patients and relatives (if appropriate)informed of events. The Head of Communications and the Patient, Carer andPublic Engagement Manager may be of assistance in this process, withexperience of how to deal sensitively with patients and relatives whilst independentof the NCH process. Ensuring that all records relating to the incident are secure. The need to uphold confidentiality7.10 Action to be taken12
The Chief Operating Officer will contact the Gold On Call Manager to set up thearrangements.The hotlines will be established in the Gold On Call room.A dedicated group of staff will work under the direction of the Gold On CallDirector.The decision as to how long the line will be set up will be taken by the ManagingDirector/Chief Operating Officer in association with partner organisations such asthe PCT and Strategic <strong>Health</strong> Authority. Systems and staffing will be available to provide access to the hotline over a 24hour, 7 day a week period. The decision to provide this level of capacity will bemade by the Managing Director/Chief Operating Officer taking into account: -i) Guidance from the PCT and/or Strategic <strong>Health</strong> Authorityii) Level of initial usageiii) Other support systems/hotlines availableiv) Level of media coveragev) Developments in relation to the management of the incident All calls will be logged – recording advice given and identifying individuals nameswho have used the line.7.11 Equipment providedMultiple phone lines and internal accessExtra mobile phones to allow immediate access to communication facilitiesDocumentation for logging calls in a specific and rigorous wayComputer terminals/fax machines will allow the hotline team to receive andprovide information to people making enquiries as well as statutory agencies.8. Documentation8.1 NCH should protect itself and their staff by initiating a record of events from the time aSUI is reported. The Designated Director will be responsible for setting up and maintainingadequate records. These records should be contemporaneous, legible, signed, time anddated. All records of the incident will be kept securely, meeting both Caldicott and DataProtection Act requirements by the person managing the incident.8.2 Relevant patient records must be secured as soon as the incident has been reported,together with any other relevant information such as duty rotas. Records may need to becopied if they are required for ongoing use. Documentation should include contemporaneouswritten records (witness statements) from all involved staff, which must be legible, dated,timed and signed. [See Appendix G]8.3 The Investigating Manager will ensure that comprehensive information is available forany further investigations, which may occur (e.g. inquests, criminal proceedings, civil claimsor disciplinary hearings) and maintain liaison with the Head of Governance & Compliance.9 Support for those involved with SUIs9.1 It is recognised that SUIs will cause distress to patients, family and carers and staff andas such support will be offered as soon as possible following a SUI.9.2 In the case of a SUI involving a patient, the patient or relatives will be notified by adoctor/nurse or by another appropriate person identified by the Designated Director for theincident as soon as possible referring to the NCH Being Open <strong>Policy</strong> (See guide AppendixB). This should be given prior to any anonymised information about the SUI being sharedwith the media (if appropriate) and recorded. Patient confidentiality will be maintained at all13
times. The staff involved, have a crucial role to play through their professional expertise, inensuring that the distress of patients and carers is acknowledged and handled with care andsensitivity.9.3 The Head of Governance & Compliance will advise on any legal issues and anyrequirement for formal witness statements for the Police or Coroner. He will support staff andshould be involved in the management of relevant SUIs at the earliest opportunity. [AppendixH]9.4 SUIs may cause significant distress to staff involved. The Designated Director andInvestigation Manager reviewing the SUI will be responsible for ensuring that employeesinvolved have access to appropriate support.9.5 Initial session/s with staff to discuss the events should take place as soon as possibleafter the incident as is appropriate. An external facilitator may be appointed and staff shouldbe encouraged to approach their line manager if support is required. Individual members ofstaff can also access the free and confidential counselling service via Human Resources.Staff will be encouraged to liaise with their staff side representative.10 Investigating SUIs10.1 The Designated Lead Director and designated Investigating Manager will agree Termsof Reference for the investigation. All SUIs will be managed and investigated so that thelearning from the incident can be identified and implemented. A short term SUI Managementand Review Group should be set up [sub Group of the Governance Committee] and it isimportant that an investigation is started as soon as possible after the incident. At least onemember of the review team will be trained in the use of NPSA Root Cause Analysis tools.The level of the investigation will depend on the seriousness of the SUI but all will warrantimmediate action to support patients, staff and the public. The process will include: Identifying the events, which led up to the incident? Analysing the reasons (root cause analysis) why the incident happened. Ascertaining whether agreed procedures were properly carried out and/or identifyingany inadequacies in the procedures. Recommending appropriate interventions and an action plan including time scalesand responsibilities. Review process to ensure the action plan is implemented. Consider whether any residual risk remains.10.2 The Designated Lead Director should update the Head of Governance & Complianceand PCT SUI Lead and the Head of Communications weekly by email on the progress of theinvestigation.10.3 The Head of Governance & Compliance will ensure STEIS/UNIFY is regularly updatedto reflect progress on the investigation.10.4 The Investigating Manager should document all the findings of the investigation in areport [Appendix J] (except where an external investigation has been commissioned) and adraft should be forwarded to the Head of Governance & Compliance within 4 weeks andfinalised for the SUI review Group by 8 weeks. The report will also define what actions canbe taken to prevent a similar incident occurring again in the future. The Head of Governance& Compliance will update the STEIS/UNIFY system and ensure the Root Cause andLessons Learnt section are completed.14
10.5 Progress on the investigation and action plan development for all SUIs will bemonitored through the Governance Committee10.6 When an investigation is complete and within 12 weeks a copy of the report outliningthe process, findings and recommendations of the internal review plus action plan should besent to the Managing Director NCH. The final report will be sent to the GovernanceCommittee and the Professional Executive Team and the resulting action plans will bemonitored for their implementation through the Quality & Risk Sub-committee.The PCT as commissioner will review the SUIs reported to the PCT by the ManagingDirector and may externally monitor the action plans. With agreement an anonomised reportcovering the main findings and recommendations will be shared with other providers whereappropriate.11. <strong>Learning</strong> from SUIs11.1 The importance of learning from SUIs to ensure they do not reoccur is fundamental todeveloping quality services and minimising risk to patients, staff and the organisation.11.2 It is the responsibility of the Designated Lead Director to meet with individuals /services/agencies involved to share recommendations so that multi-disciplinary learning from theevent will take place.11.3 The Head of Governance & Compliance will ensure that any SUI trends are reviewed inthe Governance Committee and reported to Managing Board where required.Recommendations and changes to practice will be disseminated to the wider organisationthrough appropriate channels to enable organisational and clinical improvements to beachieved as a consequence.11.4 It is particularly important that NCH learns from investigations into serious untowardincidents. NCH needs to ensure that their staff, are genuinely encouraged in performanceimprovement and this culture needs to pervade the process and be paid special attention atthe conclusion of a review.12. Key performance indicators12.1 All SUIs are reported to relevant parties within NCH within four hours of occurrence.12.2 All SUIs are reported to the Head of Communications and from there verbally to thePCT and SHA Communications Team within twelve hours of occurrence.12.3 All SUIs are reported to STEIS/UNIFY within 48 hours of occurrence.12.4 The Governance Committee will receive a summary report of all SUIs and lessonslearned at each of their meetings.12.5 The Quality and Risk Sub- Committee will monitor the implementation of all SUI actionplans.12.6 Any residual risks are monitored and managed through the NCH Risk Register process.15
Appendix A - Commitment to a Fair and Open CultureA clinical or non-clinical error, accident or adverse event however serious is rarely causedwilfully. It is not, in itself, evidence of carelessness, neglect or a failure to carry out a duty ofcare. Errors are often caused by a number of factors including, process problems, humanerror, individual behaviour and lack of knowledge or skills. <strong>Learning</strong> from such incidents canonly take place when they are reported and investigated in a positive, open and structuredway.Determining safe practice is an important part of successful risk management. Moving awayfrom punishing errors to learning from them will promote a fair and open culture and safepractice throughout the organisation. This will enable Nottinghamshire Community <strong>Health</strong>(NCH) to identify trends and take positive action to prevent the error or adverse incident fromhappening again.To promote a fair and open culture and encourage the reporting of adverse events, NCH willtake a non-punitive approach to those incidents it investigates. Staff remain accountable inlaw and to users, carers, NCH and their professional bodies for their actions, but a nonpunitiveapproach means that disciplinary action will not be taken against a member of stafffor reporting an incident, but in the rare circumstances where there is evidence of: Gross professional or gross personal misconduct Repeated unacceptable behaviour Wilful concealment of errors accidental or otherwise <strong>Incident</strong>s that results in criminal charges or prosecution16
Appendix B - Quick reference guide to “Being Open” for staffThe principles of Being Open are fully supported by a wide range of Royal Colleges andprofessional organisations.Apologising and explaining when patients have been harmed can be very difficult. You mayhave already considered some or all of the recommendations below, but this guide will helpensure that you follow best practice. Do also refer to the NCH Being Open <strong>Policy</strong> beforeproceeding. Patients and/or carers should receive an apology as soon as possible after apatient safety incident has occurred and staff should feel able to apologise on the spot.Saying sorry is not an admission of liability and it is the right thing to do. Patients have a rightto expect openness in their healthcare and answers to any queries that they raise. The initialapology should be made by a senior member of staff with the knowledge and skills todiscuss the situation and answer any immediate questions.The opportunity of a follow up meeting should be made to ensure the patient and carershave any concerns addressed and are assured that an incident review is underway.Stage 1: preliminary meeting with the patient and/or their carersWho should attend? A lead staff member who is normally the most senior person responsible for thepatient’s care and/or someone with experience and expertise in the type of incidentthat has occurred. Ensure that those members of staff who do attend the meetings can continue to doso: continuity is very important in building relationships. The person taking the lead should be supported by at least one other member ofstaff, such as Head of Governance & Compliance, Assistant Director of Professions& Governance or member of the healthcare team treating the patient. Ask the patient and/or their carers who they would like to be present. Consider each team member’s communication skills; they need to be able tocommunicate clearly, sympathetically and effectively. Hold a pre-meeting amongst healthcare professionals so that everyone knows thefacts and understands the aims of the meeting.When should it be held? As soon after the incident as possible. Consider the patient’s and/or their carer’s home and social circumstances. Check that they are happy with the timing. Offer them a choice of times and confirm the chosen date in writing. Do not cancel the meeting unless absolutely necessary.Where should it be held? Use a quiet room where you will not be distracted by work or interrupted. Do not host the meeting near to the place where the incident occurred if this may bedifficult for the patient and/or their carers.Stage 2: discussionHow should you approach the patient and/or their carers? Speak to the patient and/or their carers as you would want someone in the samesituation to communicate with a member of your own family. Do not use jargon or acronyms; use clear, straightforward language. Consider the needs of patients with special circumstances, for example, linguistic orcultural needs, and those with learning disabilities.17
What should be discussed? Introduce and explain the role of everyone present to the patient and/or their carerand ask them if they are happy with those present. Acknowledge what happened and apologise on behalf of the team and theorganisation. Expressing regret is not an admission of liability. Stick to the facts that are known at the time and assure them that if more informationbecomes available, it will be shared with them. Do not speculate or attribute blame. Suggest sources of support and counselling. Check they have understood what you have told them and offer to answer anyquestions. Provide a named contact who they can speak to again. Ensure a record of the meeting is taken.Stage 3: follow-up Clarify in writing the information given, reiterate key points, record action points andassign responsibilities and deadlines. The patient’s notes should contain a complete, accurate record of the discussion(s)including the date and time of each entry, what the patient and/or their carers havebeen told, and a summary of agreed action points. Maintain a dialogue by addressing any new concerns, share new information onceavailable and provide information on counselling, as appropriate.18
Appendix C - Deciding whether an incident is a <strong>Serious</strong> <strong>Untoward</strong><strong>Incident</strong> [SUI]Assessing the severity of an incident will initially lie with local managers but ultimately rely onthe expertise, experience and discretion of the relevant Assistant Director. For example theAssistant Director will need to consider the level of likely media/public interest as well as thecircumstances of the incident itself.The following guidance is provided as an aide to determining severity.The following can be involved in the incident:A patient, service user, member of the public, contractor, NHS staff, locum staff and out ofhours providers, children, young people, prisoners and young offenders, or other providersof healthcare involved in the process of treatment, care or consultation on NHS premises, orin the course of treatment or care that is commissioned by the NHS but may be delivered bya private provider on non-NHS premises. This definition includes patients’ homes.<strong>Incident</strong>s for Consideration<strong>Incident</strong>s that should be considered for reporting as SUIs will most commonly fall within oneor more of the following categories. Whether or not the incident is reported will depend uponthe Assistant Director’s discretion and their assessment of the severity of the incident. Thislist is not exhaustive and is intended as a guide only. Accident in hospital resulting in serious injury Allegation of abuse against a healthcare worker Allegation of Assault against a healthcare worker Allegation of theft / fraud against a healthcare worker Significant assault by other/unknown assailant Significant assault by Patient Bogus healthcare worker Chemical, biological, radiological or Nuclear [CBRN] incident resulting in seriousinjury or major service disruption Child or Adult Abuse (alleged or actual) – instigation of a Local SafeguardingChildren Board (LSCB) <strong>Serious</strong> Case Review or if a <strong>Serious</strong> Case Review isundertaken under Protection of Vulnerable Adults (POVA) guidance. Significant Confidential information leak Damage (serious) to NHS property (e.g. through fire, flood, criminal activity) Death on GP premises Deaths in custody (where the health services are provided by NCH) Drug incident (including controlled drugs and medical gases) Equipment Failure relating in serious injury or service disruption Estate Failure e.g. utilities, lifts, generators, heating etc Fire Communicable disease or significant infection issue <strong>Health</strong>care Associated Infection/Infection control – outbreak of infection > 5 cases in7 days <strong>Health</strong>care Associated Infection – MRSA or C Diff mentioned on part 1 of deathcertificate Pressure Ulcers Grade 3 and 4 Contamination/radiation hazard Screening Issues19
Security threat, including terrorism in a healthcare premises<strong>Serious</strong> disruption to services<strong>Serious</strong> injury to any personSuicide (attempted or actual)Unexpected death (unusual or suspicious circumstances or significant mediainterest)Unplanned ward or service closure20
Appendix D - Essential Contact NumbersContact nameContact NumberMon-Fri 9am to 5pmContact Numberout of normal hoursDirector on Call Non applicable 0115 934 3236Manager on Call Non applicable 0115 934 3236Managing Director 01623 673787 Via on call managerChief Operating Officer 01623 673786 Via on call managerAssistant Director of Professions & Governance 01623 673784 Via on call managerHead of Communications 01623 673824 Via on call managerHead of Governance & Compliance 01623 673768 Via on call managerTel:NHS Nottinghamshire County Contact 0300 300 1234 0115 934 3236East Midlands SHA SUI Hotline - NHS EMDirectorate of Patient Care0115 968 4702 08700 555500Give call groupcodeNHSEM1D.2. Nottinghamshire Community <strong>Health</strong> SUI LeadD2.1 The principal link with East Midlands Strategic <strong>Health</strong> Authority [SHA] concerning<strong>Serious</strong> <strong>Untoward</strong> <strong>Incident</strong>s within NCH and has responsibility for ensuring theSTEIS/UNIFY on line <strong>Serious</strong> <strong>Untoward</strong> <strong>Incident</strong> [SUI] report is completed lies with the Headof Governance or nominated proxy.21
Appendix E - Initial Data Set: Capturing the Immediate Details.Assistant Directors and Managers should use the <strong>Serious</strong> <strong>Untoward</strong> <strong>Incident</strong> Data Form tocapture the information that will initially be needed to brief senior colleagues and inform theHead of Communications, the PCT and the SHA, the Head of Governance& Compliance.[Affected person name not included for reasons of confidentiality but will be required to beshared where appropriate]<strong>Serious</strong> <strong>Untoward</strong> <strong>Incident</strong> Log Form[For initial data collection, does not replace standard incident report]Name of Designated Lead Director:Phone Number:Date of <strong>Incident</strong>:Service, Site & Location of <strong>Incident</strong>:Gender of Patient:Time of <strong>Incident</strong>:Type of Patient:[Inpatient, community, etc.]Ethnic Group (if known):Date of Birth:Type of <strong>Incident</strong>:[Accident, Infection control, Data protection etc.]Actual/Near MissBrief outline of the issue / Description of what happened: (include any equipment, medical devices, medication involvedensure preserved for the incident investigation)Describe Immediate action taken:Further Action being taken: (include action to support and inform patients, relatives and carers)Patient / Relatives informed: ( ‘Being Open’ procedure applied) Date/Time informed, who informed and by whom)Media Interest: Yes/No (If yes please give sufficient information to form basis of press release. What is the initial view of events andthe approach to the investigation?)Principal Staff contact(s) and contact number(s); (initial SUI Lead and other significant contacts)Further information (if relevant):Managing Director informedDate/Time Informed:Assistant Director Professions and Governance Informed Date/Time Informed:Head of Governance & Compliance informedDate/Time Informed:Head of Communications InformedDate/Time Informed:PCT Senior Management TeamDate/Time Informed:(Name of Senior Manager Informed)Signed:Print Name:Designation:Date & Time:22
Appendix F:EXTERNAL REPORTING<strong>Incident</strong> type Recipient Information reportedRIDDOR incidents <strong>Health</strong> & safety executive (HSE) Injuries from work based accidents.Details of incident and personsinvolved.Medicine incidentsMedicines and <strong>Health</strong>care ProductsRegulatory Agency (MHRA)Comprehensive details of incidentsrelated to adverse drugs reactions.Medical device related incidents MHRA Comprehensive details related todevices involved in incidentincluding manufacture date, expirydate.<strong>Serious</strong> Adverse Blood RelatedEvents (SABRE)MHRA / Hospital TransfusionCommittee Via Acute TrustHaematology LaboratoryDetails of incident including initialfindings.Patient safety incidents NPSA All patient safety incidents includingnear-miss events.Communicable disease outbreaksand other public health issuesFire related incidents. Estaterelated incidents<strong>Health</strong> Protection Agency (HPA)NHS Estates (NHSME)Infection control and other publichealth incidents with details ofspread of disease, contact etc.Details of fire incident injuries/deathcause type/quantity loss.Insurance claims and incidents NHSLA Details and cost of loss/claim.Environment related incidents e.g.waste disposalData Protection/CaldicottcontraventionsEnvironment AgencyDept of <strong>Health</strong> through SHAInformation on incidents e.g. type ofwaste and hazards.Description of contravention e.g.patient details disclosedinappropriately.Safeguarding Children Local Safeguarding Children Board Details of child protection relatedincident.Safeguarding vulnerable adults Social Services Details of incident to Protection ofVulnerable Adults Lead [POVA].The Central Alert System (CAS) Department of <strong>Health</strong> Details of actions taken to addressissues contained in alert.<strong>Incident</strong> involving a patient detailedunder the Mental <strong>Health</strong> Act<strong>Incident</strong> involving individual in aregistered residential care homeIf doctor cannot issue a deathcertificateMental <strong>Health</strong> Act CommissionCare Quality CommissionHM CoronerDetails of the individual, type ofsection, occurrence.Details of individual, occurrence.Details about patient and fullcircumstances of death.23
Appendix G - GUIDANCE FOR STAFFREQUESTS FOR REPORTS AND WITNESS STATEMENTS INCORONIAL LAW, LEGAL PROCEEDINGS OR INCIDENTS1 Aim of GuidanceThis document is produced as guidance for staff that are approached for written information instatements or reports in respect of their patients/clients. A witness statement may be required for: The Coroner, after a death has been referred to him/her Following an accident, incident or untoward event and/or SUI In response to a claim against NCHRequests for Coroner’s/Solicitor’s reports should be routed via NCH’s Head of Governance &Compliance; and any request you receive or contact made direct to you should be notified to yourmanager and advice sought from the Head of Governance & Compliance. The reason for this is toensure that all NCH staff representing the organisation are supported through the report-writingprocess and through any subsequent appearance in Court as a witness. The author of a report can berequired to appear as a witness and will summoned to attend. NCH is committed to supporting its staffthrough legal processes as set out above. Any information you provide may be used as evidence inconnection with legal proceedings. These requests may initially be made by telephone but should befollowed by a written request for a written report.DO NOT GIVE INFORMATION BY TELEPHONEIn all cases, the aim of a witness statement is to preserve the information that is not apparent from thecase notes; in a form that can be given in evidence should the witness not be available forinvestigation, inquest or trial.2 Summary: Write down your full name, address (place of work, although you may be asked to provideyour home address by the Coroner/Police) and brief CV details. Remind yourself of the case/incident by referring to the medical/nursing notes (if applicable) Write a narrative of precisely what you recall of the events, what you did and did not do,whom you spoke to, who you contacted and at what stage you ceased to be involved. Useand explain the words that you recorded in the patients notes. UNDER NO CIRCUMSTANCES ALTER THE PATIENT RECORDS/NOTES. Document your reasons for any actions or omissions. Record the facts only, do not include hearsay or opinion. Consider whether sensitive or potentially distressing information is relevant to the inquest, orinvestigation (e.g. allegation of abuse, difficult family relationships) before including suchdetail in the statement. If in doubt contact the Head of Governance & Compliance. It is desirable that your statement is typed, however if this is not possible then a hand writtenstatement will suffice, but it must be legible and written in black pen which assists with anyphotocopying required. Use one side of A4 for each page. Do not use Tippex to delete anentry in your report/statement. Any alterations to a witness statement must be initialled by the person making the statementor by an authorised person (a person able to administer oaths and take affidavits). Contactthe Head of Governance for advice if necessary. You may ask your line manager and the Head of Governance & Compliance to look throughyour statement prior to signing. You may also consult your professional body if you wish.When you have read through your statement and are happy with the contents then sign anddate it. (Some statements need to be signed witnessed and dated at the bottom of eachpage.) UNDER NO CIRCUMSTANCES SHOULD YOUR STATEMENT BE FILED IN THEPATIENTS NOTES. Ensure that you keep a copy of your statement and provide a copy to the Head ofGovernance & Compliance when appropriate. DO NOT USE ABBREVIATIONS.If you have any queries or need assistance please contact: Head of Governance & Compliance viaNCH HQ24
Coronial Law – request for reports for the Coroner and witnessappearances at InquestsCoroners are required to inquire into deaths reports to them, which appear to be violent, unnatural, orof sudden and unknown cause. The Coroner will seek to establish the medical cause of death; if thecause remains in doubt after a post mortem, an inquest will be held. Not all deaths are reported to thecoroner. In many cases a GP or hospital doctor can certify the medical cause of death and the deathcan be registered by the Registrar of Births and Deaths in the usual way. However, these Registrarsmust report deaths to the Coroner in certain circumstances. For example if a doctor cannot give asatisfactory cause of death; if the death occurred during or shortly after an operation; was due toindustrial disease; occurred whilst the person was in custody, or if the death was unnatural or due toviolence or occurred in other suspicious circumstances.An Inquest is an inquiry into who has died and how, when and where the death occurred and morerecently the addition of “and in what circumstances the death occurred” has been added. An inquestis not a trial and does not apportion blame for a death. Possible verdicts include: natural causes,accident, suicide, unlawful or lawful killing, industrial disease and open verdicts (where there isinsufficient evidence for any other verdict) or if death is as a result of neglect. The Coroner may bringa narrative verdict, in which case additional text will be included in the verdict.General Principles: The Coroner will expect a report within a certain timescale, usually within 28 days of thewritten request. If in any doubt about the amount of detail required in a report, contact the Head ofGovernance for advice. The report should be capable of standing on its own. Do not assume that the reader has anybackground knowledge of the case. Several people may have to read the report from theCoroner. A draft of the report should be sent to the Head of Governance before a signed copyis sent to the Coroner. Remember that the Coroner may not be a clinician so the report should be written so that alay person can understand it; i.e. drug names, doses etc in full, what it was prescribed for,when started or stopped and why.Clinical Records:The Coroner may require disclosure of the whole medical record. In any event, take a fullphotocopy set, including the front and back cover of the Lloyd George envelope if appropriate(even if the back has nothing written on it), for your own records before disclosing or returningthe records. Also keep a printout of all information held on computer.You may need to keep copies before destroying them in accordance with NCH Retention andDisposal schedules. (Refer to Records Management Code of Practice part 2)It can be helpful to give the exact dates spanned by the notes because it will not always beobvious from the entries.Style of report: Avoid using any abbreviations in your report, unless the meaning is written out in full on firstusage. If you mention a drug, explain what type of drug it is, give the full generic name,dosage, method of administration, when started or stopped and why it was prescribed orstopped. Write your report in the first person. It is tempting to write in the passive tense because that isthe accepted format in a clinical report. However, it is easier for the Coroner to get the fullpicture of events if the report is written in the first person.First hand evidence: The Coroner is most interested in first hand evidence. Hearsay evidence carries less weight.Concentrate on your observations and understanding of the case, provide factual evidencenot supposition.25
Clearly your understanding of a case, and the interpretation you place on your examination,will be significantly influenced by the history given to you by the patient or from what you haveread, for example, in medical notes, referral letters. Whilst the patient’s description isimportant and provides the context for your interpretation, it is less important than yourobservations and understanding.The involvement of colleagues: Where another clinician has been involved in the care of the deceased you should identifythem with their full name and professional status. You may describe your understanding ofwhat they did and the conclusions they reached purely on a factual basis. It may be necessary for colleagues to write individual reports. If you feel this may be the caseplease discuss with the Head of Governance & Compliance who may need to contact theCoroner.Negative information: Your description of both the history and the examination should enable a third person to relatethem in your place. It is important, therefore, to say not only what you found, but also whatyou looked for, but failed to find.Notes, your memory and your “usual” practice: In your report you should specify which details are based on (1) your memory, (2) thecontemporaneous notes you, or (3) others have written and (4) your “usual” or “normal”practice.Conclusion: Take the necessary time to produce a comprehensive, accurate report, this will minimise theneed of further correspondence with the Coroner. If your report clearly demonstrates that yourhistory and examination were thorough, it may not be necessary for you to be called as awitness to have your evidence tested at Inquest. If you are called to give evidence at an Inquest you may not be able to consult your reportwhilst giving evidence, however, you will be allowed to read your contemporaneous notes. Itis therefore worth rereading your report before you take the witness stand to refresh yourmemory, hence the importance of keeping a copy of your report. You may, if you wish, notify your defence organisation, and, if so please inform the Head ofGovernance that you have done so.Requests for Statements for other purposesMembers of staff may not be obliged to make a written statement in circumstances other than outlinedabove. If staff are prepared to assist, as will sometimes be the case, they should reply that they arerequired to seek the advice of their manager before they respond verbally or in writing. Advice mustbe sought in all cases. Managers may also be expected to be generally co-operative but they willneed to take into account such matters as patient confidentiality, prejudice to the interests of theemployee or Nottinghamshire Community <strong>Health</strong> before making a decision. Managers should takeadvice from the Head of Governance & Compliance when approached to give statements.Requests for Reports for other purposesNottinghamshire Community <strong>Health</strong> would advise that all staff to refrain from agreeing to write reportsor professional witness statements for solicitors without first seeking advice from a manager. Themanager should take advice from the Head of Governance & Compliance when necessary.In the event that a Court of Law requests a statement or report, then the recipient of the Court Ordershould comply with the request, ensuring firstly that they are provided with a copy of the Order if itwas not received with the request. If in doubt, seek the advice of the Head of Governance &Compliance. In the event that a report is used as evidence by Solicitors, staff are reminded that theywould not automatically have the legal or financial support of NCH if NCH were not a party in theparticular legal proceedings or had not agreed to the provision of a statement. All requests fromSolicitors for reports should be referred to the lead professional responsible for the patient’s care.26
It is important to remember that verbal discussions with third parties who are not involved with apatient’s care would breach the patient’s confidentiality unless the patient consented to the disclosure.In exceptional cases disclosure of information may be necessary without the patient’s consent but thisshould first be discussed with the line manager or the Head of Governance & Compliance.Requests for Access to, or Disclosure of <strong>Health</strong> RecordsAll written requests for access to patient’s medical records for anyone other than the patient must beforwarded to the PCT’s Information Governance Manager. (Refer to Records Management Code ofPractice part 1)27
Appendix H:CORONER’S REPORT / WITNESS STATEMENTNOTE: TEMPLATE remove guidance in italics before useCORONER’S REPORT / WITNESS STATEMENT [delete as appropriate] IN THE MATTER OFPatient name (if applicable)<strong>Incident</strong> Date:(e.g. This report relates to the death of ………….. who died on ………….. )NAME:JOB TITLE AND EMPLOYER:ADDRESS:QUALIFICATIONS:SUMMARY OF EXPERIENCE:BODY OF REPORT: (see sections below)STATEMENT OF TRUTH:This report/statement (consisting of …….. page(s) each signed by me) is true to the best of myknowledge and belief and I make it knowing that, if it is tendered in evidence, I shall be liableto prosecution if I have wilfully stated anything in it, which I know to be false, or do not believeto be true.Signature:Date:……………………………………………………………………………………………………………………...Your report should include information about the following:Background Summary Specify the nature of your contact with the patient, e.g. state if you saw the patient on theNHS or privately, for clinical purposes or for forensic purposes or a combination of reasons.Where appropriate state if you saw the patient alone or accompanied by another personduring each and every consultation. Give the name and status of the other person(s) present,e.g. spouse, mother, social worker, ward sister, etc.Documents List all the documents you have relied on in writing your report.Factual Account of Events Set out a chronological description of recent illnesses and/or events leading to death/incident.Give a factual description of events as you saw them using the clinical notes as a framework.Refer to the notes in your report whenever you can. Describe each and every consultation ortelephone contact in turn and this description should include your working diagnosis or yourdifferential diagnosis. Outline any hospital referrals, identifying the name of the relevantpractitioner or consultant. Ensure there are no gaps in the sequence of events or where thereare provide an explanation, e.g. during May I was on annual leave and did not therefore seethe patient.Clinical Record For Coroner’s reports it may be helpful to disclose a photocopy of the contemporaneousclinical notes when requested. Where appropriate it might even be necessary to provide aword for word, line-by-line type written transcript of notes plus abbreviations written out in full.28
Appendix I:- Investigating a <strong>Serious</strong> <strong>Untoward</strong> <strong>Incident</strong> [SUI]This appendix lays out the SUI investigation procedure for SUIs and details theresponsibilities of managers in achieving compliance. The initiation of an investigationfollows the reporting of a SUI by the Designated Lead Director in accordance with the NCHSUI reporting process.Nottinghamshire Community <strong>Health</strong> Internal SUI Review GroupThe group will be a sub group of Governance Committee.Terms of reference to be agreed by the Designated Lead Director, Assistant Director(Professions & Governance) and the Managing Director.Terms of reference should include: Composition of the internal review team including external advisors as required Style and nature of the internal review The job title of the person leading the review A requirement to consider any other relevant factors raised by the incident A remit to investigate the circumstances surrounding the SUI To produce a report on its findings, including recommendations for action Methods of working (confidentiality, conducting interviews, clearing notes andstatements with interviewees) Critical dates (e.g. completion of interim report and final report) Arrangements for subsequent handling and publication of the reportReport content [See Appendix J]The minimum data required to be collected and reported on as part of the investigation is setout below: What happened (event/near miss description, severity of actual or potential harm,people and equipment involved) Where did it happen (exact location and speciality) When did it happen (date and time) How did it happen (immediate or approximate causes) Why did it happen (underlying root cause analysis using NPSA tools) What action was taken or proposed (immediate and longer term) What other agencies were informed of the SUI, when and by whom What impact did the event have (harm to organisation, patients, others) What factors did or could have minimised the impact of the event (mitigating factors) Recommend further action to be taken in the form of an action plan (with timescalesand identified leads)29
Appendix J: - Adverse Event Review Report Template:NOTE: remove guidance text shown in italics before useCONFIDENTIALDraft<strong>Serious</strong> <strong>Untoward</strong><strong>Incident</strong> ReportLocation:[of incident]Date:[of incident]Report Author(s):Contents: Page numbers relevant to each section Pages:Adverse Event Report:Divided into sections under headings as on following page[No patient or staff identifiable information]Acknowledgements:To those participating in review.[Job titles not personal names].References:Full reference to any relevant papers / documentsAppendices:1,2 6 & 7 as standard, plus others as appropriate to the depthof review, where assist in enhancing the report content.[Re-number as necessary]1 Terms of Reference of Review Group2 <strong>Incident</strong> Report Form [Printed from Datix where applicable and dulyanonymised]30
Main report Headings:3 Relevant documentation [anonymised]4 Photographs [where relevant with appropriate consent]5 Personal accounts / statements [anonymised]6 Root Cause Analysis tool used [E.G. Completed Time line / fishbone]7 Action Plan with identified lead individualsFree text narrative of the entire adverse event related to appropriate appendices.1.0 The Adverse Event:Very Brief synopsis of what happened, the headlines:- Adverse Event Report [AER]number (used to link all relevant information) Date, Time, Location.2.0 Background:Factors leading up to the event Clinical history where relevant Setting the context3.0 The occurrence of the event:Detailed Chronology / Factual account / no speculation4.0 Immediate actions:How the event was initially managed: patient / staff safety / preservation of the scene/ who was informed [role / job title not personal names]5.0 Contributory Factors / Root Causes:Describe Root Cause methodology:[See NPSA toolkit at: http://www.npsa.nhs.uk/health/resources/root_cause_analysis]Include as appendix one of completed Time line / fish bone, five whys etc.Use the following headings for narrative: Environment / working conditions: Task / process: Equipment and resources: Patient factors: Staff / Team factors: Communication Factors: Organisation / Strategic / Management factors: Exterior influences: local / national6.0 Potential long-term outcomes:[Future risk: consequences & likelihood]For those involvedFor the organisation7.0 Conclusion:Include principal root causes8.0 Recommendations:To form basis of action plan9.0 Action Plan:What is to be done, by whom and by when.31
Detailed Action Plan Re <strong>Serious</strong> <strong>Untoward</strong> <strong>Incident</strong> SHA STEIS Log Number:Datix Adverse Event Number:Location:Date:ActionPlanRef:Issue /ProblemActionPlanCost £LeadDirectorLeadManagerTargetDateDate oflastreviewProgress[N.B. If noprogressprovideseparateexceptionreport todetailconstraints]32
Appendix K: - <strong>Serious</strong> <strong>Untoward</strong> <strong>Incident</strong> <strong>Policy</strong>: Audit toolThis checklist summarises the requirements of the <strong>Serious</strong> <strong>Untoward</strong> <strong>Incident</strong> [SUI] <strong>Policy</strong>1. Is the procedure for SUI reporting explained to all new staff as part of their CorporateInduction?YES/NO2. Have all Nottinghamshire Community <strong>Health</strong>’s SUI’s been reported to an AssistantDirector within 4 hours of their occurrence?YES/NO3. Have patients and relatives where appropriate been informed of SUIs under ‘Being Open’procedures and in all cases before any information disclosed to the media? YES/NO4. Have all NCH SUIs been reported to the PCT within one week of their occurrence?YES/NO5. Have all SUIs been appropriately recorded onto the <strong>Incident</strong> Reporting Database Datixand signed off when completed?YES/NO6. Has a Risk Assessment [Consequence and likelihood] been undertaken regarding thespecific type of SUI that has been reviewed?YES/NO7. Have all SUIs been appropriately recorded onto STEIS/UNIFY and signed off whencompleted?YES/NO8. Have all SUIs had a formal report completed within 60 days of the index event?YES/NO9. Have all SUIs had an action plan developed, implemented and monitored? YES/NO10. Have lessons learned from SUIs been shared across NCH and with stakeholders?YES/NO11. Has a summary report regarding SUI’s been submitted to Governance Committee atleast quarterly?YES/NO12. Have SUIs been included as part of the Annual Risk Management Report? YES/NOWhere .NO’ is a response an action plan should be devised to implement improvements.33
Appendix LEquality Impact Assessment ToolTo be completed and attached to any procedural document when submitted to theappropriate committee for consideration and approval.PROCEDURE NAME<strong>Serious</strong> <strong>Untoward</strong> <strong>Incident</strong> <strong>Policy</strong>Yes/NoComments1. Does the policy/guidance affect onegroup less or more favourably thananother on the basis of: Race Ethnic origins (including gypsies andtravellers) Nationality Gender Culture Religion or belief Sexual orientation including lesbian,gay and bisexual people Age Disability - learning disabilities, physicaldisability, sensory impairment andmental health problems2. Is there any evidence that some groupsare affected differently?3. If you have identified potentialdiscrimination, are any exceptionsvalid, legal and/or justifiable?4. Is the impact of the policy/guidancelikely to be negative?NoNoNoNoNoNoNoNoNoNoNoNo5. If so can the impact be avoided? No6. What alternatives are there to achievingthe policy/guidance without the impact?7. Can we reduce the impact by takingdifferent action?NoNo34
If you have identified a potential discriminatory impact of this procedural document, pleaserefer it to the sponsoring director, together with any suggestions as to the action required toavoid/reduce this impact.For further advice in respect of answering the above questions, please contact the Equalityand Diversity Lead for NCH Associate Director of Workforce.35