Session 3 - Incident Reporting Policy - Health Partnerships Learning ...
Session 3 - Incident Reporting Policy - Health Partnerships Learning ...
Session 3 - Incident Reporting Policy - Health Partnerships Learning ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
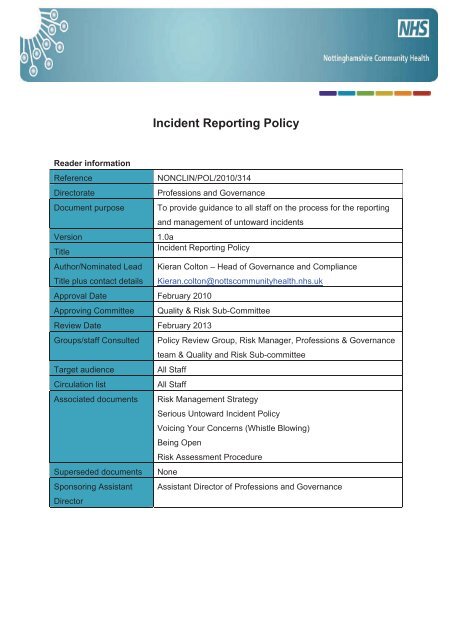
<strong>Incident</strong> <strong>Reporting</strong> <strong>Policy</strong><br />
Reader information<br />
Reference<br />
NONCLIN/POL/2010/314<br />
Directorate<br />
Professions and Governance<br />
Document purpose To provide guidance to all staff on the process for the reporting<br />
and management of untoward incidents<br />
Version 1.0a<br />
Title<br />
<strong>Incident</strong> <strong>Reporting</strong> <strong>Policy</strong><br />
Author/Nominated Lead<br />
Title plus contact details<br />
Kieran Colton – Head of Governance and Compliance<br />
Kieran.colton@nottscommunityhealth.nhs.uk<br />
Approval Date February 2010<br />
Approving Committee Quality & Risk Sub-Committee<br />
Review Date February 2013<br />
Groups/staff Consulted <strong>Policy</strong> Review Group, Risk Manager, Professions & Governance<br />
team & Quality and Risk Sub-committee<br />
Target audience All Staff<br />
Circulation list<br />
All Staff<br />
Associated documents Risk Management Strategy<br />
Serious Untoward <strong>Incident</strong> <strong>Policy</strong><br />
Voicing Your Concerns (Whistle Blowing)<br />
Being Open<br />
Risk Assessment Procedure<br />
Superseded documents None<br />
Sponsoring Assistant Assistant Director of Professions and Governance<br />
Director
Contents<br />
Section<br />
Page<br />
1 Introduction 3<br />
2 Purpose 3<br />
3 Definitions 4<br />
4 Duties 5<br />
5 Communication and Notification 8<br />
6 <strong>Reporting</strong> to External Agencies 9<br />
7 How to Report an <strong>Incident</strong> or Near Miss 10<br />
8 <strong>Incident</strong> <strong>Reporting</strong> and Investigation 12<br />
9 Approval and Monitoring 12<br />
10 <strong>Learning</strong> and Sharing Safety Lessons 13<br />
11 Training 13<br />
12 Equality Impact Assessment 13<br />
13 Monitoring Compliance with the Document 14<br />
14 References 14<br />
15 Associated Documentation 15<br />
Appendices<br />
Appendix A How to Report an <strong>Incident</strong> or Near Miss (<strong>Reporting</strong> Procedure) 16<br />
Appendix B Risk Grading Matrix 20<br />
Appendix C List of External Stakeholders 22<br />
Appendix D Definitions of Serious Untoward <strong>Incident</strong>s (SUI’s) 23<br />
Appendix E Senior Manager On-Call Arrangements 25<br />
Appendix F Equality Impact Assessment Tool 26<br />
Appendix G Plan for Dissemination of Policies or Procedural Documents 27<br />
Appendix H Employee Record of Having Read the <strong>Policy</strong>/Procedure/Guidance 28
1 Introduction<br />
The effective reporting of patient safety and staff related incidents, accidents, near misses and<br />
hazards is an essential component to patient safety and quality improvement within<br />
Nottinghamshire Community <strong>Health</strong> (NCH). It is vital to the delivery of high quality, safe patient<br />
care and to facilitate organisational learning in preventing recurrence of adverse events.<br />
Effective reporting works to improve patient safety and the well being of staff and visitors to<br />
NCH premises.<br />
This document details the standard requirements for incident reporting. The <strong>Policy</strong> does not<br />
provide comprehensive details on <strong>Incident</strong> Investigation and Root Cause Analysis (RCA)<br />
processes used by NCH in the investigation of all incidents, including Serious Untoward<br />
<strong>Incident</strong>s (SUI’s). Further information on these processes is available in the<br />
<br />
<br />
Investigation of <strong>Incident</strong>s, Claims & Complaints <strong>Policy</strong><br />
Serious Untoward <strong>Incident</strong> <strong>Policy</strong><br />
The key principles and benefits of the organisations’ <strong>Incident</strong> <strong>Reporting</strong> <strong>Policy</strong> are to:<br />
<br />
<br />
<br />
<br />
<br />
<br />
Safeguard patient care;<br />
Identify trends and potential risk areas for patient safety and quality<br />
improvement;<br />
Maximise organisational learning from the investigation of the incident;<br />
Ensure incidents, where required, are reported to relevant statutory agencies<br />
and external bodies;<br />
Develop a culture of reporting is nurtured through a fair blame approach to<br />
incident reporting and investigation; and<br />
Ensure damage to NCH’s reputation and assets is minimised.<br />
The over-riding purpose of incident reporting is to maximise learning from incidents<br />
and not to apportion inappropriate blame.<br />
Accurate and effective reporting can only occur in a non-punitive environment. <strong>Incident</strong>s are<br />
therefore managed positively as a way to increase patient safety and improve quality and will<br />
only imply the need for disciplinary action in exceptional circumstances, such as criminal,<br />
reckless or malicious acts and omissions, or gross professional misconduct. All staff are<br />
therefore required to report incidents and to be actively involved in their investigation in a<br />
climate of openness and shared learning.<br />
This <strong>Policy</strong> has been developed to ensure that NCH has procedures in place to meet Standard<br />
1.5.1 of the NHSLA Risk Management Standards for PCT’s dated April 2009/10 which<br />
describes the process for managing the risks associated with the reporting of all internally and<br />
externally reportable incidents.<br />
2 Purpose<br />
The purpose of this policy is to minimise injury or incident to all, by ensuring that any lessons<br />
learned from any accident, incident, near miss, disease or dangerous occurrence are acted on<br />
so that a similar recurrence is either avoided or the possibility of recurrence is reduced.<br />
It also ensures that required information is passed on to prescribed authorities and affected<br />
person(s) in a proper and prompt manner.
3 Definitions<br />
Accident: Anything that happens without apparent cause<br />
Breach of confidentiality which includes: Finding a computer printout with a header and a<br />
person’s information on it at location outside of any NCH premises/building. Finding any paper<br />
records about a patient/member of staff or business of the organisation in any location outside<br />
of the NCH premises/buildings. Being able to view patient records in the back (or front) of an<br />
employees car (e.g. Doctors and Nurses). Discussing, in person or on the phone, patient or<br />
staff personal information with someone else in an open area where the conversation can be<br />
overheard. A fax, email or letter being received by the incorrect recipient.<br />
Breach of Security:<br />
<br />
<br />
<br />
<br />
<br />
Loss of computer equipment due to crime or an individual’s carelessness<br />
Loss of computer media e.g. floppy disc, CD due to an individual’s carelessness<br />
Accessing any part of a database using someone else’s authorisation either<br />
fraudulently or by accident<br />
Trying to access a secure part of the organisation using someone else’s PIN number,<br />
swipe card<br />
Finding the doors and/or windows have been broken and forced entry gained to a<br />
secure room/building<br />
Information Security <strong>Incident</strong>: any event that has resulted or could result in;<br />
<br />
<br />
<br />
<br />
The disclosure of confidential information to any unauthorised person<br />
The integrity of the system or data being put at risk<br />
The availability of the system or information being put at risk<br />
An adverse impact e.g.<br />
o Embarrassment to the NHS<br />
o Threat to personal safety or privacy<br />
o Legal obligation or penalty<br />
o Financial loss<br />
o Disruption of activities<br />
Hazard: ‘a situation with the potential to cause harm or damage’<br />
<br />
<br />
<br />
Hazards are situations with the potential to cause harm or damage. They could include<br />
faulty equipment, worn or loose floor coverings, irritant chemicals etc.<br />
<strong>Incident</strong> Report Forms must be completed for all hazards<br />
Staff are responsible for not only completing the <strong>Incident</strong> Report Form but also taking<br />
reasonable steps at the time to minimise the risk of injury from the identified action<br />
Near Miss: ‘any patient safety incident that had the potential to cause harm but was<br />
prevented, resulting in no harm’<br />
<br />
<br />
<br />
A Near Miss is when any incident that had the potential to cause harm but was<br />
prevented, resulting in no harm<br />
It is important Near Misses are reported to identify and effectively manage the risk of<br />
reoccurrence<br />
Research has shown that for every serious incident, there will have been many more<br />
similar Near Misses which were not reported because no harm resulted<br />
Page 4 of 28
Other incidents: Some incidents may impact on other parts of the NHS e.g. a computer virus<br />
and if this is the case the incident should be reported to the IT Helpdesk (01623 410310 Ext<br />
4040). All Information Security <strong>Incident</strong>s will be reported to the Risk Management Team.<br />
Other <strong>Incident</strong> Categories<br />
Patient safety incidents<br />
Accidental injuries<br />
Slips, Trips and Falls<br />
Work related ill-health<br />
Unusual or dangerous occurrences<br />
Medication errors<br />
Adverse drug reactions<br />
Patient safety incidents<br />
Missing health records<br />
Violence or damage to property<br />
Equipment failures<br />
Fraud etc.<br />
This list is not exhaustive but gives some examples of the wide range of adverse events that<br />
are categorised as reportable incidents.<br />
Patient Safety <strong>Incident</strong>: ‘an unintended or unexpected incident that did lead to harm for one<br />
or more persons receiving NHS-funded care’<br />
Reportable <strong>Incident</strong>s: any event which contains one or more of the following components:<br />
<br />
<br />
<br />
<br />
Standards of patient care full below those expected to deliver good patient care<br />
An incident that places patients, staff or visitors at unnecessary risk<br />
An incident that may attract adverse legal or media attention<br />
There is risk or damage to property<br />
<strong>Reporting</strong> of Injuries, Diseases and Dangerous Occurrences Regulations 1995 (RIDDOR<br />
95)<br />
A number of incidents and accidents must be reported to the <strong>Health</strong> and Safety Executive<br />
under the RIDDOR regulations as defined below:<br />
Dangerous Occurrences: A ‘dangerous occurrence’ is a term used in RIDDOR 95,<br />
which specifically denotes types of incidents that are reportable under these<br />
regulations<br />
Major Injury: RIDDOR regulations do not define a major injury; the list in Appendix A<br />
of the <strong>Incident</strong> <strong>Reporting</strong> Procedure identifies the types of injuries that are reportable<br />
Further details can be obtained from the RIDDOR web site: http://www.riddor.gov.uk/<br />
Serious Untoward <strong>Incident</strong>s (SUIs) involve the occurrence of the most serious incidents,<br />
examples include (See Appendix D and also Serious Untoward <strong>Incident</strong> <strong>Policy</strong>)<br />
<br />
<br />
<br />
<br />
<br />
<br />
Significant harm<br />
Unexpected death<br />
Death directly related to an adverse event<br />
Substantial damage or loss to NCH assets<br />
Adverse media interest<br />
Death of a prisoner in receipt of care<br />
Page 5 of 28
Ward closure<br />
Child death<br />
Serious sexual assault<br />
Risk to NCH’s reputation; and Infection outbreaks<br />
Significant loss of confidential information or patient identifiable information<br />
Staff: ‘Staff, volunteers, students and sub-contractors working for Nottinghamshire<br />
Community <strong>Health</strong> and independent contractors commissioned by NCH.<br />
4 Duties<br />
Managing Director:<br />
<br />
The Managing Director has overall responsibility for risk management within NCH<br />
Assistant Directors/Associate Directors<br />
<br />
<br />
<br />
<br />
<br />
Ensure all staff in their Directorate are informed of the need to report incidents<br />
which arise out of the activities of the Directorate<br />
Ensure all directly employed staff understand the incident reporting system and<br />
receive feedback from incidents reported<br />
Ensure contractors and volunteers are aware of the <strong>Incident</strong> <strong>Reporting</strong> <strong>Policy</strong><br />
Allocate sufficient resources (both financial and human) for incident investigation<br />
and follow up<br />
Ensure any recommendations made as a result of investigations are put into place<br />
Locality Service Managers/Heads of Service<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Ensure all staff, bank staff, agency workers and contractors under their control<br />
understand and follow this policy accordingly<br />
Ensure that all incidents within their sphere of responsibility are reported<br />
Grading all accidents as soon as possible in accordance with the Matrix in this<br />
policy. (See How to Report an <strong>Incident</strong> or Near Miss Appendix A)<br />
Liaise with Occupational <strong>Health</strong> team regarding any health issues related to the<br />
health of the injured person<br />
Report intentional assault on staff to the Risk Management Team; who will report to<br />
the Local Security Management Specialist (LSMS) Officer<br />
Ensure that all incidents classified as Major or above are reported immediately to<br />
the Risk Management Team based at Ransom Hall<br />
Ensure that all other incidents are reported to the Risk Management Team within<br />
24 hours of the incident occurring or 1 working day<br />
Undertake investigation as appropriate and completion of the manager’s action<br />
section of the incident report form and returned to the Risk Management team<br />
based at Ransom Hall within 2 weeks from the date of the incident.<br />
Ensure recommendations and actions are carried out as a result of any<br />
investigation<br />
Monitor information reported on the incident forms for accuracy and completeness<br />
Ensure that any procedures within their area take account of incidents which have<br />
been brought to their attention<br />
Ensure that serious incidents are brought to the immediate attention of their Line<br />
Manager or Assistant Director<br />
Where appropriate obtain witness statements<br />
Make safe any area or equipment following an accident and retaining equipment for<br />
inspection where required<br />
Page 6 of 28
Ensure that risk assessments are reviewed or carried out on all significant identified<br />
hazards and appropriate action plans put in place to reduce risks to an acceptable<br />
level. The results of those risk assessments must be communicated to all those<br />
who may be at risk<br />
Provide feedback to directly employed staff on trends, serious incidents, results of<br />
investigations, recommendations and any learning opportunities<br />
Risk Manager/<strong>Health</strong>, Safety & Risk Facilitator/Risk Management Team must:<br />
Collate, review and support managers with incidents reported<br />
Support local managers in the investigation process (to be decided case by case)<br />
on incidents<br />
Compile quarterly summary reports on incidents and review recorded incidents to<br />
identify trends<br />
Ensure that all reports are anonymised so that patients cannot be identified from<br />
them<br />
Bring any incidents or trends of particular importance or giving rise to immediate<br />
concern to the attention of the Assistant Director of Professions and Governance,<br />
Head of Governance & Compliance and/or the appropriate Assistant Director<br />
Ensure lessons learned are cascaded and embedded in practice. This will be done<br />
through discussion in team meetings, training, newsletter, posters and intranet<br />
Highlight NCH wide incident trends to the staff and Committees as required on a<br />
quarterly basis, or more frequently if required<br />
Ensure aggregated qualitative and quantitative data on incidents is produced within<br />
the quarterly incident reports. The qualitative data will include types and number of<br />
incidents, service affected, risk severity comparison with previous quarter<br />
Ensure that all reports do not contain any information that would allow the patient to<br />
be identified<br />
Ensure any risk discovered from trends and themes in the aggregated data is<br />
transferred into the appropriate risk register.<br />
Ensure the NCH audit program is informed of risks to enable adaptation to<br />
encompass auditing of learning within the agreed timeframe to ensure staff alter<br />
their practice in response to lessons learnt<br />
Ensure information related to NCH performance in relation to numbers of incidents<br />
and trend analysis are presented to the appropriate Committee, raise awareness of<br />
activity and to engage in the processes of organisation wide learning and<br />
development<br />
Ensure that lessons learnt from trend analysis result in a change in organisational<br />
culture and practice through a robust risk register process<br />
Ensure lessons learned are cascaded and embedded in practice. This will be done<br />
through discussion in team meetings, training, newsletter, posters and internet and<br />
the National Patient Safety Agency (NPSA)<br />
<strong>Reporting</strong> of Injuries, Diseases and Dangerous Occurrences Regulations 1995<br />
(RIDDOR) accidents/incidents to the <strong>Health</strong> and Safety Executive (HSE)<br />
Ensure that accidents/incidents are appropriately investigated, and where<br />
necessary remedial measures taken<br />
Maintain an appropriate filing system for hard copy incident report forms<br />
Produce collated reports on incidents for the <strong>Health</strong> and Safety Group<br />
Forward all incidents of intentional assault and verbal abuse to the Local Security<br />
Management Specialist (LSMS)<br />
Report details of patient related incidents to the NPSA under the National<br />
<strong>Reporting</strong> and <strong>Learning</strong> System (NRLS)<br />
Page 7 of 28
Report details of other incidents to the statutory agencies as necessary (See How<br />
to Report an <strong>Incident</strong> or Near Miss Appendix A)<br />
All Employees<br />
All employees (including placement students, sub-contractor staff, and volunteers) are<br />
responsible for:<br />
Verbally reporting all incidents and near misses (including violence and verbal<br />
abuse) to their manager as soon as possible<br />
Ensure that all reports of incidents which are categorised as Major or above are<br />
reported immediately to their Line Manager/Service Lead/Risk Management Team<br />
Completing the NCH <strong>Incident</strong> Report Form within 24 hours of the incident<br />
occurring, either by them or if incapacitated, by a nominee and fax to the Risk<br />
Management Team at Ransom Hall 01623 781747 and then hand original form to<br />
their line Manager<br />
Bringing to the attention of their manager or supervisor any incidents which<br />
resulted in, or had the potential to result in injury, loss or damage (i.e. near misses)<br />
Co-operating in any investigation and providing relevant information to assist in<br />
identifying the cause of the harm<br />
Immediate action must be taken to ensure the safety of staff, patients and other<br />
members of the public before an <strong>Incident</strong> Form is completed<br />
Role of the Quality & Risk Sub-Committee<br />
The NCH Managing Board has devolved to the Quality and Risk Sub-committee responsibility<br />
for risk management. The Terms of Reference for the Quality & Risk Sub-Committee<br />
(Q&RSC) are included in the Risk Management Strategy.<br />
The Q&RSC receives regular incident reports demonstrating trend analysis and any actions<br />
taken to mitigate the risks.<br />
The responsibility for the completion of action plans, developed in response to incidents record<br />
as Major or above, SUI’s incident investigations, and the effectiveness of any risk reduction<br />
measures will be reported to and co-ordinated by the Q&RSC with the support of the relevant<br />
service (Clinical or Corporate) or groups for specific incident types.<br />
5 Communication and Notification<br />
The Locality Service Manager/Head of Department/Senior Manager as appropriate has a<br />
responsibility to ensure that staff or other persons involved in the incident have received a full<br />
explanation and are made aware of any further implications concerning what has happened.<br />
Those involved in the incident should be kept up-to-date with progress on investigating the<br />
incident.<br />
Communication with and Support for Staff<br />
Nottinghamshire Community <strong>Health</strong> is committed to developing a culture which allows staff to<br />
raise concerns through appropriate channels, particularly in relation to patient safety. The<br />
systems and processes for reporting incidents and raising concerns will be clearly<br />
communicated to staff and staff will be proactively encouraged to raise concerns. Staff will<br />
also be advised of and have access to the <strong>Policy</strong> for Voicing Your Concerns (Whistle<br />
blowing). Although NCH would expect that this would only be required in exceptional<br />
circumstances as all senior managers will be responsible for ensuring staff have access to<br />
more appropriate routes.<br />
Page 8 of 28
Following a reported incident, regardless of severity level it is essential that the staff are:<br />
appropriately supported by line managers, involved in any subsequent investigation and<br />
advised of the investigation outcomes and recommended changes to practice.<br />
Communication with and Support for Victims, Perpetrators, Families and Carers<br />
Following an <strong>Incident</strong><br />
Nottinghamshire Community <strong>Health</strong> will expect that following any incident those involved in the<br />
incident both staff and patients will be offered information and support commensurate with the<br />
level of the incident.<br />
It is also important to ensure that where an incident has occurred involving a patient(s), the<br />
patient is kept informed as to the progress and outcome of any investigation and /or outcome.<br />
Subject to confidentiality provisions, family and carers should also be informed. Such<br />
communication should be clearly recorded within the incident record. Communication should<br />
be maintained with the patient /carer or family for as long as this is necessary.<br />
Communication with the patients and/or the relatives, staff or visitors may need to be both pre<br />
and post investigation dependant on the incident grading and investigation.<br />
Any information given to patients, staff or family and carers needs to be documented by the<br />
person who has provided the information in the incident record. This communication needs to<br />
follow the principles of ‘being open’ as described in the Being Open <strong>Policy</strong>.<br />
Media Involvement<br />
The Head of Department/Service has a responsibility to ensure that staff affected by or<br />
involved in an incident are informed before any media are involved. The investigating manager<br />
should work closely with the Head of Communications to ensure that this is guaranteed. It is<br />
also important that all staff ensure that no information is given to the media; all media<br />
requested must be referred immediately to their appropriate Assistant Director and/or the<br />
Head of Communications who are based at Ransom Hall.<br />
6. <strong>Reporting</strong> to External Agencies<br />
NHS Nottinghamshire County and East Midlands SHA<br />
All serious untoward incidents, both clinical and non-clinical will be reported via STEIS by the<br />
Head of Governance and Compliance.<br />
National <strong>Reporting</strong> <strong>Learning</strong> System (NRLS)<br />
All patient safety incidents for NCH will be reported, electronically via DATIX, to the NRLS by<br />
the Risk Manager. This contributes to national learning about patient safety. Reports will be<br />
received from the NRLS and distributed through the organisation, which can be used to<br />
benchmark incident reporting with other organisations and identify areas for improvement.<br />
<strong>Health</strong> and Safety Executive – RIDDOR<br />
The <strong>Reporting</strong> of Injuries, Diseases and Dangerous Occurrences Regulations 1995 came into<br />
force on 1st April 1996. NCH must report deaths, major injuries, and accidents resulting in<br />
over 3 day injury, diseases, dangerous occurrences and gas incidents. The Service<br />
Managers/Heads of Service/Team Leaders will carry out RIDDOR reporting, to the HSE, for<br />
NCH. When an incident has been identified as RIDDOR reportable, the <strong>Health</strong>, Safety & Risk<br />
Facilitator should be notified as soon as possible. In serious incidents resulting in major injury<br />
Page 9 of 28
or death, the <strong>Health</strong> and Safety Executive need to be alerted immediately<br />
(www.riddor.gov.uk). Outside of normal working hours the senior manager on-call should do<br />
this. If there is an accident connected with work (including an act of physical violence)<br />
resulting in an employee suffering an over-three-day injury it must be reported in compliance<br />
with the above regulations within 10 days. An over-3-day injury is one which is not ‘major’ but<br />
results in the injured person being away from work OR unable to do their full range of their<br />
normal duties for more than three days. It is the manager’s responsibility to ensure that<br />
the <strong>Health</strong>, Safety & Risk Facilitator is contacted within 24 hours.<br />
The <strong>Health</strong> and Safety Executive will require the following information: -<br />
Date and time of incident<br />
Location of incident<br />
Name, home address, gender and status of persons involved / affected<br />
Details of any injuries<br />
Confirmation as to whether the situation is under control or whether assistance<br />
is required<br />
Brief outline of the circumstances of the incident<br />
Details of any witnesses.<br />
Medicines and <strong>Health</strong>care Products Regulatory Agency (MHRA)<br />
Where a serious incident involves a medical device the NCH nominated liaison officer with the<br />
Medicines and <strong>Health</strong>care Products Regulatory Agency (MHRA) must be contacted within 24<br />
hours. The liaison officer for NCH is the <strong>Health</strong>, Safety and Risk Facilitator. An appropriate<br />
senior manager will be responsible for ensuring that the material evidence is labelled and kept<br />
secure. The Senior Medicines Management Advisor will report adverse reactions to<br />
medication to the MHRA.<br />
Communicable Diseases<br />
The Consultant in Communicable Disease Control (<strong>Health</strong> Protection Agency) should be<br />
contacted in the event of an infectious disease outbreak defined as two or more cases<br />
connected by time and place and any serious single infection with public health implications.<br />
The most senior manager on duty should notify the HPA as soon as an outbreak has been<br />
identified.<br />
Other External Agencies<br />
A list of other external agencies to which incidents and near misses may require reporting to<br />
are set out in Appendix C. <strong>Reporting</strong> to these agencies will be undertaken by the Risk<br />
Manager with support from the Risk Management Team and relevant information provided<br />
from service teams.<br />
7. How to Report an <strong>Incident</strong> or Near Miss<br />
All incidents and near misses should be reported to the line manager as soon as possible after<br />
the event. If the line manager is not available report to the next available senior member of<br />
staff.<br />
Out of hours contact the Senior Manager on call by telephoning 0115 934 3236 (See Appendix<br />
E –Senior Manager On-Call Arrangements)<br />
All incidents, near misses and serious untoward incidents must also be recorded on the NCH<br />
<strong>Incident</strong> Report Form which are available in all departments and clinical areas within the<br />
Page 10 of 28
<strong>Incident</strong> <strong>Reporting</strong> Folders (a complete list of all the locations is available on the NCH Intranet<br />
site).<br />
Wherever possible the <strong>Incident</strong> Report form should be completed and faxed to the Risk<br />
Management Team at Ransom Hall (Save Haven Fax 01623 781747) immediately or as a<br />
minimum within 24 hours of the incident occurring. The original <strong>Incident</strong> Report (Part 1)<br />
and Part 2 should be sent immediately to their Line Manager for grading and further<br />
investigation (See also Appendix A).<br />
The person involved in or identifying the incident should complete the incident report.<br />
In instances where a member of staff is unable to complete the form due to illness or injury,<br />
the senior person on duty should complete the incident report form.<br />
Where an incident results in an absence from work of more than three consecutive days<br />
(excluding the day of the incident, but including week-ends, bank holidays or days off) then the<br />
Line Manager must notify the <strong>Health</strong>, Safety & Risk Facilitator as soon as possible, in order<br />
that the <strong>Health</strong> and Safety Executive can be informed within ten days of the accident or<br />
incident. This is a legal requirement under RIDDOR.<br />
Describing the <strong>Incident</strong> or Near Miss<br />
A description of the <strong>Incident</strong> or Near Miss should include:<br />
<br />
<br />
<br />
<br />
<br />
<br />
a full, clear and accurate description of the incident and relevant circumstances<br />
recording facts and not subjective opinions<br />
an outline of what was happening immediately prior to the incident occurring and<br />
the exact location of the incident<br />
a clear description of any relevant equipment involved, including asset inventory<br />
ref. serial number, make, model etc<br />
environmental details such as weather and lighting where relevant, and details of<br />
any protective equipment, clothing or footwear<br />
sketch(s)/or photographs should be attached if it assists in making the report<br />
clearer<br />
details of the identity of any witnesses to the event.<br />
Special Actions Relating to Serious Untoward <strong>Incident</strong>s:<br />
In addition to reading this section all staff should make themselves aware of the<br />
Serious Untoward <strong>Incident</strong> <strong>Policy</strong><br />
<strong>Reporting</strong> Process in Hours<br />
Where it becomes apparent that the incident is serious (Appendix D gives examples of<br />
incidents that should be reported as a SUI) it must be reported immediately to the appropriate<br />
Assistant Director/General Manager/Head of Governance & Compliance in addition to<br />
completion of the usual incident report form.<br />
The SUI lead (Assistant Director of Professions and Governance) must also be informed and<br />
is responsible for ensuring that the incident is reported on the STEIS system (Strategic<br />
Executive information System ) within 24 hours.<br />
Page 11 of 28
Out of Hours<br />
If the incident has occurred out of hours telephone the call handling service on 0115 934 3236<br />
who will notify the Senior Manager on call. (See Appendix E)<br />
8. <strong>Incident</strong> <strong>Reporting</strong> and Investigating<br />
The timely reporting and investigating of incidents is essential in order to improve patient<br />
safety. Through the identification of actual or potential (near miss) incidents, the subsequent<br />
investigation to identify what, how and why it happened and the implementation of change<br />
should reduce or prevent the recurrence of similar incidents. The process for reporting and<br />
investigating incidents will vary depending on the severity of the incident, the details of which<br />
are provided in the NCH Guidance Document for the Investigation of Complaints, <strong>Incident</strong>s<br />
and Claims.<br />
<strong>Incident</strong> Grading and Appropriate Levels of Investigations<br />
All incidents should be graded using the grading matrix set out on Appendix B of this<br />
document. The basic principle is to multiply the consequence by the likelihood. The resulting<br />
number is the risk grade.<br />
Level of Investigation<br />
The level of investigation is dependent on the outcome of the risk grade of the incident.<br />
Level of risk<br />
Risk score 0 to 10<br />
Level of Investigation<br />
Investigated by service with advice and guidance from Risk<br />
Management Team and includes outcome on Part 2 of the<br />
<strong>Incident</strong> report form<br />
12 to 20 Investigated by Service with direct input and review by Risk<br />
Management Team – outcome record on Part 2 of the <strong>Incident</strong><br />
Report Form.<br />
Mangers should adopt the Investigation tools identified within the<br />
document “Guidance on Conducting Investigations of Complaints,<br />
<strong>Incident</strong>s and Claims”<br />
SUI’s<br />
Some incidents graded between 16 and 25 will require a more<br />
detailed report. Guidance should be sought from the Risk<br />
Management Team<br />
Investigated in line with the Serious Untoward <strong>Incident</strong> <strong>Policy</strong><br />
9. Approval and Monitoring<br />
To ensure appropriate change is made to reduce the likelihood of an incident recurring there<br />
needs to be a system for the approval and monitoring of action plans. It is expected that<br />
remedial action will be taken in response to all incidents and near misses but that the level of<br />
approval and monitoring will be dependent upon the severity. All incidents with a severity<br />
rating below Major will have their actions plans/learning points agreed locally and with<br />
appropriate input from the NCH Risk Management team. Those plans will then be monitored<br />
through the DATIX risk management system by the NCH Risk Management Team.<br />
Page 12 of 28
All Action Plans relating to incidents or near misses grade Major or above will be approved<br />
and monitored by the Q&RSC.<br />
10. <strong>Learning</strong> and Sharing Safety Lessons<br />
The reporting, reviewing, investigating and acting upon incidents is critical to the delivery of<br />
safe and effective services. This is essential for all incident types ranging from near misses to<br />
serious untoward incidents. To ensure that NCH learns lessons from reported incidents the<br />
following will be undertaken -<br />
<br />
<br />
<br />
<br />
<br />
<br />
Analysis of trends emerging from high numbers of incidents involving either a<br />
specific type of incident, an individual member of staff, a individual patient or<br />
particular service.<br />
<strong>Incident</strong> review which will incorporate a root cause analysis of all incidents<br />
classified as Catastrophic or a SUI.<br />
Analysis of all reported incidents quarterly.<br />
The <strong>Learning</strong> Form Patient Experience Group will review the learning form a variety<br />
of sources such as <strong>Incident</strong>s, Complaints, Claims, Patient Experience and<br />
identified good practice. Such learning and good practice will be shared via team<br />
meetings, training events, newsletters and the usual service structures.<br />
Lessons requiring instant dissemination will be cascaded through the NCH Safety<br />
Alert Broadcast System.<br />
Improvement will be monitored via the Q&RSC.<br />
The reporting of incident analysis and lessons learnt to Managing Board will be through the<br />
Q&RSC and the Governance Committee following analysis by the various relevant working<br />
groups.<br />
11. Training<br />
Nottinghamshire Community <strong>Health</strong> will ensure that all staff will have access to induction and<br />
ongoing training in the reporting and handling of <strong>Incident</strong> Report and investigation.<br />
Staff Group Type Frequency<br />
All Staff Groups<br />
General Risk Management<br />
including <strong>Incident</strong> Reports,<br />
Induction<br />
3 years<br />
General Principles Risk<br />
Assessment<br />
Band 6 and above<br />
<strong>Incident</strong> Investigation and Managers Induction<br />
Associates/Directors<br />
General Managers<br />
Service Managers<br />
Governance 6 and above<br />
Band 8 and above<br />
Governance Team and<br />
where required Role Specific<br />
Risk Assessment<br />
SUI Investigation<br />
(Including learning<br />
lessons)<br />
Risk Management<br />
Risk Register/Assurance<br />
Framework<br />
Risk Management<br />
DATIX<br />
NRLS<br />
STEIS<br />
3 years<br />
3 years<br />
3 years<br />
2 years<br />
12. Equality Impact Assessment<br />
Page 13 of 28
Nottinghamshire Community <strong>Health</strong> aims to design and implement services, policies and<br />
clinical/non clinical procedures with measures that meet the diverse needs of our service,<br />
population and workforce, ensuring that none are placed at a disadvantage over others.<br />
All policies and clinical/non clinical procedures should be developed in line with the NHS Notts<br />
County Equality and Diversity <strong>Policy</strong> (2008), and need to take into account the diverse needs<br />
of the community that is served. The Equality Impact Assessment tool is designed to help<br />
consider the needs and assess the impact of the policy and clinical/non clinical procedure<br />
being developed (See Appendix F), and must be completed before approval/ratification can<br />
take place.<br />
13. Monitoring Compliance with the Document<br />
Nottinghamshire Community <strong>Health</strong> (through the Risk Management Team) will monitor the<br />
effectiveness of this policy through key performance indicators (KPIs) which will include an<br />
annual review.<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
The process for involving and communicating with internal and external<br />
stakeholders to share safety lessons<br />
The process for following up relevant action plans; through reports from DATIX for<br />
low level risk and the work of the Q&RSC for higher level risks.<br />
NCH regularly uploads to the NPSA National <strong>Reporting</strong> <strong>Learning</strong> (NRLS) system<br />
Lessons learnt from analysis result in change<br />
Process for reducing risk identified through incident reports<br />
75% of incidents have a completed management action section within 2 weeks of<br />
the incident occurring<br />
Quarterly incident risk management reports contain incident and causal factors<br />
trend analysis<br />
At least 2 Lessons Learnt reports (Shared Experience Newsletters) are produced<br />
and disseminated each year<br />
An annual risk management report containing results of the audit and improvement<br />
actions is produced for the Q&RSC responsible for overseeing risk management<br />
14. References<br />
<strong>Health</strong> & Safety Executive. (1995). <strong>Reporting</strong> of Injuries, Diseases and Dangerous<br />
Occurrences Regulations (RIDDOR Explained, Version 6), Suffolk: <strong>Health</strong> and Safety<br />
Executive. Available at: http://www.hse.gov.uk/riddor/index.htm.<br />
<strong>Health</strong> and Safety (Consultation with Employees) Regulations 1996. (Statutory Instrument<br />
1996 No. 1513). London: The Stationery Office. Available at: www.opsi.gov.uk<br />
<strong>Health</strong> & Safety Executive. (1996). A guide to the <strong>Health</strong> and Safety (Consultation with<br />
Employees) Regulations 1996 (L95). Suffolk: <strong>Health</strong> and Safety Executive. Available at:<br />
www.hsebooks.com/<br />
Public Interest Disclosure Act 1998, Chapter 23. London: The Stationery Office. Available at:<br />
www.opsi.gov.uk<br />
Department of <strong>Health</strong>. (1998). <strong>Health</strong> Service Circular 1999/198, The Public Interest<br />
Disclosure Act 1998: Whistle blowing in the NHS. London: Department of <strong>Health</strong>. Available at<br />
www.dh.gov.uk/<br />
Page 14 of 28
Department of <strong>Health</strong>. (2000). An Organisation with a Memory: Report of an Expert Group on<br />
<strong>Learning</strong> from Adverse Events in the NHS. London: Department of <strong>Health</strong>. Available at<br />
www.dh.gov.uk/<br />
Department of <strong>Health</strong>. (2001). Building a Safer NHS for Patients: Implementing an<br />
Organisation with a Memory. London: Department of <strong>Health</strong>. Available at www.dh.gov.uk/<br />
National Patient Safety Agency. (2004). Seven Steps to Patient Safety. London: National<br />
Patient Safety Agency. Available at: www.npsa.nhs.uk/<br />
National Patient Safety Agency. (2005). Building a Memory: Preventing Harm, Reducing Risks<br />
and Protecting Patient Safety London: National Patient Safety Agency. Available at:<br />
www.npsa.nhs.uk.<br />
National Patient Safety Agency. (2005). Patient Briefing - Saying Sorry When Things Go<br />
Wrong. London: National Patient Safety Agency. Available at: www.npsa.nhs.uk/<br />
National Patient Safety Agency. (2005). Safer Practice Notice - Being Open When Patients<br />
are Harmed. London: National Patient Safety Agency. Available at: www.npsa.nhs.uk/<br />
<strong>Health</strong>care Commission. (2008). The annual health check 2008/09 Assessing and rating the<br />
NHS. London: <strong>Health</strong>care Commission. Available at:<br />
http://www.healthcarecommission.org.uk/publicationslibrary.<br />
Department of <strong>Health</strong>. (2008). High Quality Care For All NHS Next Stage Review Final Report.<br />
London: Department of <strong>Health</strong>. Available at: http://www.dh.gov.uk<br />
National Patient Safety Agency (NPSA). (2009). Never Events – Framework for 2009/10:<br />
Process and action for Primary Care Trusts 2009/10. London: NPSA. Available at:<br />
http://www.npsa.nhs.uk<br />
15. Associated Documentation<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
All Information Governance Policies<br />
Safeguarding Children <strong>Policy</strong><br />
Being Open <strong>Policy</strong><br />
<strong>Health</strong> and Safety <strong>Policy</strong><br />
<strong>Incident</strong> <strong>Reporting</strong> Procedure<br />
Slips, Trips and Falls <strong>Policy</strong><br />
Guidance on the Investigation of Claims, <strong>Incident</strong>s and Complaints<br />
<strong>Policy</strong> for the Management of Violence and Aggression (Zero<br />
Tolerance)<br />
Risk Management Strategy<br />
Risk Assessment Procedure<br />
Risk Register <strong>Policy</strong><br />
Patient Identification <strong>Policy</strong><br />
Safeguarding Adults <strong>Policy</strong><br />
Serious Untoward <strong>Incident</strong> <strong>Policy</strong><br />
Medical Devices Procedure<br />
Raising Concerns “Whistle Blowing' <strong>Policy</strong><br />
Page 15 of 28
Appendix A<br />
HOW TO REPORT AN INCIDENT OR NEAR MISS<br />
The following is operational guidance on when and how to report an incident or near miss. For full<br />
guidance on untoward incident reporting you should refer to the Nottinghamshire Community <strong>Health</strong><br />
Procedure for the <strong>Reporting</strong> of <strong>Incident</strong>s and Near Misses.<br />
All incidents and near misses should be reported to the line manager as soon as possible after the<br />
event. If the line manager is not available report to the next available senior member of staff.<br />
Out of hours contact the Senior Manager on call by telephoning 0115 934 3236.<br />
All incidents, near misses and serious untoward incidents must also be recorded on the<br />
Nottinghamshire Community <strong>Health</strong> <strong>Incident</strong> Report Form (Example Section 3)<br />
<br />
Hard copies of the <strong>Incident</strong> Report forms are available across the organisation and<br />
the nearest pack of forms to you is identified in Section 1 of this folder.<br />
In all cases the <strong>Incident</strong> Report form should be completed and submitted within 24 hours of the<br />
incident occurring:<br />
Hard copy <strong>Incident</strong> Reports: Should be faxed to the Risk Management Team (Ransom<br />
Hall) on 01623 781747<br />
<br />
Where the service, team and/or department have the capability to scan the <strong>Incident</strong> Report<br />
(part1) then they can also email the electronic PDF of the <strong>Incident</strong> Report to:<br />
professions.governance@nottscommunityhealth.nhs.uk<br />
DEFINITIONS<br />
<strong>Incident</strong>: – Any event or circumstance involving patients, staff, visitors or contractors that could<br />
have, or did lead to unintended or unexpected harm, loss or damage.<br />
Near Miss: – Any event or omission where an incident almost occurred which had the potential<br />
to cause harm, injury, damage or loss but failed to develop, whether or not as a result of<br />
compensating action.<br />
ROLES AND RESPONSIBILITIES<br />
Employees: - All Employees of NCH have a duty to ensure incidents and near misses are<br />
reported as soon as possible and their manager notified so that the event can be<br />
investigated and measures taken to minimise the risk of a recurrence of the situation.<br />
Managers: - Managers have a responsibility for ensuring that incidents and near misses are<br />
graded and investigated as soon as possible after the event and that measures are taken<br />
to minimise the risk of a recurrence of the situation.<br />
Page 16 of 28
Guidance on completing an <strong>Incident</strong> Report Form<br />
The <strong>Incident</strong> <strong>Reporting</strong> Form MUST be used to record ALL incidents<br />
Record known FACTS only – do not give opinions<br />
The form must be completed within 24 hours of the incident occurring<br />
All staff are required to complete part 1<br />
SECTION ONE (S1)<br />
From the categories stated clearly tick what type of incident has occurred<br />
Date of incident should be noted in the following format: 01 11 08<br />
Time to be shown as the 24 hour clock e.g. 13:45<br />
SECTION TWO (S2)<br />
The exact location of where the incident occurred needs to be given in detail<br />
Examples:<br />
Stapleford Care Centre Consulting room 3<br />
Ransom Hall<br />
External fire escape stairs<br />
Mansfield Community Hospital Inpatients Ward<br />
Clearly tick the relevant box if equipment, medication or violence and aggression was involved or a<br />
contributory factor in the incident<br />
SECTION THREE (S3)<br />
1) Give a brief overview of the actual incident.<br />
2) Write clearly avoiding the use of abbreviations<br />
3) Give brief details of the events leading up to the incident<br />
4) Give details of any person(s) involved - do not name them<br />
5) If medication or equipment was involved, give details e.g. Drug name and dose and/or serial<br />
number of equipment<br />
6) Do not attach any statements or further information to the form (Do not attach patients<br />
clinical records)<br />
It is important that you only state FACT and not opinion<br />
If the incident relates to poor discharge arrangements (Section 5 - Poor Discharge Form) or a<br />
Pressure Ulcer Grade 3 or 4 (Section 6 - Supplementary Information for Pressure Ulcer <strong>Incident</strong><br />
Forms) then the appropriate form identified at section 5 and 6 MUST be completed. Guidance on<br />
completing both forms is outlined in Section 4 of the <strong>Incident</strong> <strong>Reporting</strong> Folder<br />
SECTION FOUR (S4)<br />
Give names of any witnesses and indicate what status they are e.g. staff, patient, contractor<br />
Give a contact number including the std code e.g. 01623 414114 Ext 4656 etc<br />
Page 17 of 28
SECTION FIVE (S5)<br />
Describe in all stages any actions that have been taken following the accident.<br />
E.g. removed faulty equipment out of use/Reported to Estates/Reported to Police/Referred to Staff<br />
<strong>Health</strong><br />
SECTIONS SIX & SEVEN (S6 & S7)<br />
The individual affected by the incident is the person that suffers or could have suffered injury, ill health<br />
or loss.<br />
If the individual affected is a member of staff then section seven must also be completed. The<br />
member of staff must give their actual job title e.g. District Nurse, Pharmacist, Administrator.<br />
Give a contact number and give the full workplace address not just the name of the premises.<br />
The table below has a list of ethnicity groups all coded. The relevant code should be added in section<br />
6.<br />
Asian or Asian<br />
British<br />
Mixed Black or Black British White Other ethnic<br />
group<br />
01 – Bangladeshi<br />
02 – Indian<br />
03 – Pakistani<br />
04 – Other Asian<br />
background<br />
05 – White & Asian<br />
06 – White & Black African<br />
07 – White & Black Caribbean<br />
08 – Other mixed background<br />
09 – African<br />
10 – Caribbean<br />
11 – Other black<br />
background<br />
12 – British<br />
13 – Irish<br />
14 –Other White<br />
background<br />
15 – Chinese<br />
16 – Other ethnic<br />
group<br />
SECTION EIGHT & NINE (S8 & S9)<br />
The person completing the form should enter all details in block capitals. Details of full workplace<br />
address must be given not just the name of the premises. Enter the date you complete the form.<br />
Give full details as stated of their line manager’s details.<br />
ON COMPLETION OF THE FORM<br />
Check the form to ensure all details are correct<br />
Do not attach any further information with the form<br />
Fax the BLUE copy (Part 1) of the form to the Risk Management Team on 01623 781747 or e-<br />
mail an electronic copy to professions.governance@nottscommunityhealth.nhs.uk<br />
Send the blue copy of the form to line manager for completion of part 2 - clearly mark the<br />
envelope e.g. Tanya Jones, District Nurse Team Leader<br />
Remove the white copy out of the incident reporting pad and retain and file in a safe place<br />
Page 18 of 28
SECTION 10 (S10)<br />
PART 2 IS TO BE COMPLETED BY A LINE MANAGER<br />
Consider the incident and look at the initial actions already taken to prevent the incident from re<br />
occurring (actions in part 1, section 5).<br />
<br />
<br />
<br />
<br />
<br />
Assess the incident using the risk matrix<br />
When scoring the incident think about the potential severity if the incident were to happen<br />
again<br />
Think about how likely it is that the incident could occur again<br />
If the overall risk score is below 8, and the actions in part 1 - section 5 are sufficient then no<br />
further investigation is required<br />
If the overall risk score is between 8 and 12 then further investigation must be carried out.<br />
The rest of this form should be used to record the findings.<br />
If the overall risk score is over 12 than the incident must be reported to the Risk Management<br />
Team immediately on 01623 673847<br />
SECTION 11 (S11)<br />
1) Give full details of the investigation you have undertaken<br />
2) Do not attach any further documents (statements, clinical records etc)<br />
3) Identify how and why the incident happened.<br />
4) Give details of any person(s) involved in the investigation process and identify what role they<br />
played e.g. partners from other agencies, estates manager<br />
5) Give details of any policies/procedures that have been referred to during the investigation<br />
SECTION 12 (S12)<br />
From the investigation note down stage by stage the lessons learnt.<br />
Give simple, clear facts. Each sentence should contain one specific fact.<br />
Example: Lessons learnt from the loss of a data stick.<br />
1) Never put personal information on the data stick<br />
2) Use encrypted data sticks only<br />
SECTION 13 (S13)<br />
Write down stage by stage all the actions that have been has been taken from the lessons learnt.<br />
Example:<br />
1) Purchased encrypted data sticks<br />
2) Ensured all staff have read and understood the <strong>Policy</strong> for Use of Portable Data Storage devices<br />
Complete SECTION this 14 section (S14) using block capitals<br />
Enter date the investigation completed<br />
Enter full job title e.g. General Manager, Locality Service Manager, <strong>Health</strong> Visitor Team Lead<br />
Enter full workplace address.<br />
Once completed return the original Part 1 and Part 2 (Blue form) to the Risk Management team; you<br />
should retain a copy for your own records.<br />
The form must be returned to the Risk Management team within two weeks of the date of the<br />
original incident occurring<br />
Page 19 of 28
Appendix B<br />
Risk Grading Matrix<br />
Severity<br />
LIKELIHOOD<br />
1<br />
Insignificant<br />
2<br />
Minor<br />
3<br />
Moderate<br />
4<br />
Major<br />
5<br />
Catastrophic<br />
1 - Rare<br />
2 - Unlikely<br />
3 - Possible<br />
4 - Likely<br />
5 - Almost<br />
Certain<br />
1 2 3 4 5<br />
2 4 6 8 10<br />
3 6 9 12 15<br />
4 8 12 16 20<br />
5 10 15 20 25<br />
Risk<br />
High (H)<br />
Moderate<br />
(M)<br />
Low (L)<br />
Further Action<br />
Risk Priority<br />
Significant Risk. As below plus:<br />
Report to Managing Board identifying treatment options<br />
Quarterly report to the Managing Board monitoring progress on<br />
treatment action plans<br />
Unacceptable Risk. As below plus:<br />
(12 and above) Report to the Governance Committee identifying<br />
treatment options<br />
(12 and above) report to the Q&RSC monitoring progress on<br />
treatment action plans<br />
Acceptable Risk. As below plus:<br />
discuss whether any further action should be taken to reduce<br />
future risk<br />
By Whom<br />
Governance<br />
Committee<br />
Q&RSC<br />
Team Meetings<br />
Risk Matrix – Likelihood<br />
Likelihood rating Description<br />
5 Almost Certain this type of event will happen frequently<br />
4 Likely this type of event will happen, but its not a persistent concern<br />
3 Possible this type of event may well happen (e.g. 50/50 chance)<br />
2 Unlikely unlikely that this type of event will happen<br />
1 Rare cannot believe that an event of this type will occur in the foreseeable future<br />
Page 20 of 28
Risk Matrix – Severity<br />
1 2 3 4 5<br />
Descriptor Insignificant Minor Moderate Major Catastrophic<br />
Over three days off Major injuries, or<br />
Injury<br />
Minor injury or “sick” = RIDDOR long term Death or major<br />
Minor injury not<br />
illness, first aid reportable. 10 days incapacity / permanent<br />
requiring first aid<br />
treatment needed to report to the disability (loss of incapacity<br />
HSE.<br />
limb)<br />
Patient<br />
Experience<br />
Unsatisfactory<br />
patient experience<br />
not directly related<br />
to patient care<br />
Unsatisfactory<br />
patient experience<br />
- readily resolvable<br />
Mismanagement of<br />
patient care – short<br />
term effects<br />
Mismanagement of<br />
patient care – long<br />
term effects<br />
Totally<br />
unsatisfactory<br />
patient outcome or<br />
experience<br />
Complaint/<br />
Claim Potential<br />
Locally resolved<br />
complaint<br />
Justified complaint<br />
peripheral to<br />
clinical care<br />
Justified complaint<br />
involving lack of<br />
appropriate care<br />
Multiple justified<br />
complaints<br />
Multiple claims or<br />
single major claim<br />
Objectives/<br />
Projects<br />
Service/<br />
Business<br />
Interruption<br />
Human<br />
Resources/<br />
Organisational<br />
Development<br />
Insignificant cost<br />
increase/schedule<br />
slippage. Barely<br />
noticeable<br />
reduction in scope<br />
or quality<br />
Loss/interruption ><br />
1 hour<br />
Short term low<br />
staffing level<br />
temporarily<br />
reduces service<br />
quality (< 1 day)<br />
< 5% over<br />
budget/schedule<br />
slippage. Minor<br />
reduction in<br />
quality/scope<br />
Loss/interruption ><br />
8 hours<br />
Ongoing low<br />
staffing level<br />
reduces service<br />
quality<br />
5 -10% over<br />
budget/schedule<br />
slippage.<br />
Reduction in scope<br />
or quality requiring<br />
client approval<br />
Loss/interruption ><br />
1 day<br />
Late delivery of key<br />
objective/service<br />
due to lack of staff<br />
(recruitment,<br />
retention or<br />
sickness). Minor<br />
error due to<br />
insufficient training.<br />
Ongoing unsafe<br />
staffing level<br />
10 - 25% over<br />
budget/schedule<br />
slippage. Doesn't<br />
meet secondary<br />
objectives<br />
Loss/interruption ><br />
1 week<br />
Uncertain delivery<br />
of key objective/<br />
service due to lack<br />
of staff. Serious<br />
error due to<br />
insufficient training<br />
> 25% over<br />
budget/schedule<br />
slippage. Doesn't<br />
meet primary<br />
objectives<br />
Permanent loss of<br />
service or facility<br />
Non-delivery of key<br />
objective/ service<br />
due to lack of staff.<br />
Loss of key staff.<br />
Very high turnover.<br />
Critical error due to<br />
insufficient training<br />
Financial Small loss (> £100) Loss > £1,000 Loss > £10,000 Loss > £100,000 Loss > £1,000,000<br />
Inspection/ Audit<br />
Adverse<br />
Publicity/<br />
Reputation<br />
Minor<br />
recommendations.<br />
Minor noncompliance<br />
with<br />
standards<br />
Rumours<br />
Recommendations<br />
given. Noncompliance<br />
with<br />
standards<br />
Local Media - short<br />
term<br />
Reduced rating.<br />
Challenging<br />
recommendations.<br />
Non-compliance<br />
with core<br />
standards<br />
Local Media - long<br />
term<br />
Enforcement<br />
Action. Low rating.<br />
Critical report.<br />
Multiple<br />
challenging<br />
recommendations.<br />
Major noncompliance<br />
with<br />
core standards<br />
National Media < 3<br />
Days<br />
Prosecution. Zero<br />
Rating. Severely<br />
critical report<br />
National Media > 3<br />
Days. MP Concern<br />
(Questions in<br />
House)<br />
Page 21 of 28
Appendix C<br />
List of External Stakeholders<br />
<strong>Incident</strong> type Recipient Information reported<br />
RIDDOR incidents <strong>Health</strong> & safety executive (HSE) Injuries from work based accidents.<br />
Details of incident and persons<br />
involved.<br />
Medicine incidents<br />
Medicines and <strong>Health</strong>care Products<br />
Regulatory Agency (MHRA)<br />
Comprehensive details of incidents<br />
related to adverse drugs reactions.<br />
Medical device related incidents MHRA Comprehensive details related to<br />
devices involved in incident<br />
including manufacture date, expiry<br />
date.<br />
Serious Adverse Blood Related<br />
Events (SABRE)<br />
MHRA / Hospital Transfusion<br />
Committee Via Acute Trust<br />
Haematology Laboratory<br />
Details of incident including initial<br />
findings.<br />
Patient safety incidents NPSA All patient safety incidents including<br />
near-miss events.<br />
Communicable disease outbreaks<br />
and other public health issues<br />
Fire related incidents. Estate<br />
related incidents<br />
<strong>Health</strong> Protection Agency (HPA)<br />
NHS Estates (NHSME)<br />
Infection control and other public<br />
health incidents with details of<br />
spread of disease, contact etc.<br />
Details of fire incident injuries/death<br />
cause type/quantity loss.<br />
Insurance claims and incidents NHSLA Details and cost of loss/claim.<br />
Environment related incidents e.g<br />
.waste disposal<br />
Data Protection/Caldicott<br />
contraventions<br />
Environment Agency<br />
Dept of <strong>Health</strong> through SHA<br />
Information on incidents e.g. type of<br />
waste and hazards.<br />
Description of contravention e.g.<br />
patient details disclosed<br />
inappropriately.<br />
Safeguarding Children Local Safeguarding Children Board Details of child protection related<br />
incident.<br />
Safeguarding vulnerable adults Social Services Details of incident to Protection of<br />
Vulnerable Adults Lead [POVA].<br />
The Central Alerting System (CAS) Department of <strong>Health</strong> Details of actions taken to address<br />
issues contained in alert.<br />
<strong>Incident</strong> involving a patient detailed<br />
under the Mental <strong>Health</strong> Act<br />
<strong>Incident</strong> involving individual in a<br />
registered residential care home<br />
If doctor cannot issue a death<br />
certificate<br />
Mental <strong>Health</strong> Act Commission<br />
Care Quality Commission<br />
HM Coroner<br />
Details of the individual, type of<br />
section, occurrence.<br />
Details of individual, occurrence.<br />
Details about patient and full<br />
circumstances of death.<br />
Page 22 of 28
Appendix D<br />
DEFINITIONS OF SERIOUS UNTOWARD INCIDENTS (SUIS)<br />
The following are criteria for reporting Serious Untoward incidents to NHS Nottinghamshire<br />
County and the Strategic <strong>Health</strong> Authority and by implication will be deemed items reportable<br />
under this policy as part of serious incident reporting.<br />
These definitions are currently under review as part of the revised East Midlands SHA<br />
<strong>Policy</strong> for the <strong>Reporting</strong> and Handling of Serious <strong>Incident</strong>s in the East Midlands.<br />
Major <strong>Incident</strong>s:<br />
<br />
Any circumstance which necessitates the activation of the NCHs’ or wider community<br />
Emergency Plan.<br />
Medico-legal incidents:<br />
<br />
<br />
Suspicion of large scale theft or any incident which may give rise to serious criminal<br />
charges.<br />
Impending court hearing or out of court settlement in cases of large scale litigation<br />
(including negligence claims)<br />
<strong>Incident</strong>s involving staff:<br />
All incidents where suspension from duty is contemplated and there is likely to be public<br />
interest or the issue is of a serious nature as defined within the following list:<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Serious complaints about a member of staff<br />
Suspicion of a serious error or errors by a member of staff<br />
A serious drug error resulting in harm to a patient<br />
A serious breach of confidentiality<br />
Serious verbal and / or physical aggression<br />
Requests for the issue of an Alert letter.<br />
Problems that may have a serious impact on public health or there is a perceived threat<br />
to the health of individual patients<br />
Significant threats to public safety<br />
If referral to the relevant statutory body is contemplated<br />
Suggestions of significant inappropriate conduct, sexual or otherwise<br />
Definite criminal activity or the involvement of the police<br />
Significant inappropriate use of or prescription of controlled drugs<br />
Strong likelihood of stories reaching the media<br />
Mortality / morbidity incidents:<br />
<br />
<br />
Clusters of unexpected or unexplained deaths<br />
Maternal deaths<br />
Page 23 of 28
The suicide of any person currently in receipt of NHS services including those provided<br />
by primary care practitioners on or off NHS premise, or who have been discharged<br />
within the last 12 months. Suicide is defined as death:<br />
where there is obvious evidence or strong suspicion of self harm, or,<br />
where the above does not apply initially but emerges later from a clinical review or<br />
other review of the case, or,<br />
where the Coroner’s verdict is suicide (or open verdict)<br />
Death or injury where foul play is suspected.<br />
The accidental death of or serious injury to a patient, member of staff or visitor to NHS<br />
premises or involving NHS staff or equipment.<br />
Significant harm to children where reported under child protection arrangements or an<br />
adverse event which results in a serious case review.<br />
Significant harm to adults where reported under vulnerable adult arrangements.<br />
<strong>Health</strong>care associated infection / infection control:<br />
<br />
<br />
<br />
<strong>Incident</strong>s which result in significant morbidity or mortality and/or<br />
Involve highly virulent and transmissible organisms and/or<br />
Require control measures that have an impact on the care of other patients, including<br />
limitation of access to healthcare services.<br />
These incidents are divided into two bands:<br />
<br />
<br />
Outbreaks that are sufficiently serious to require the convening of an incident<br />
team and/or<br />
Outbreaks that significantly disrupt services and/or highly virulent and<br />
transmissible with an impact on staff, patients or the community.<br />
<br />
<br />
Infected healthcare worker or patient incidents necessitating consideration of look back<br />
investigations (e.g. TB, vCJD, blood borne infections)<br />
Significant breakdown of infection control procedures with actual or potential for cross<br />
infection (e.g. release of products from a failed sterilisation cycle, contaminated blood<br />
transfusion).<br />
Premises / equipment incidents:<br />
<br />
<br />
<br />
<br />
Serious damage that occurs of NHS premises, or to NHS property, or any incident that<br />
results in serious injury to any individual or serious disruption to services (e.g.<br />
evacuation of patients due to fire)<br />
Failure of equipment so serious as to endanger life, whether or not injury results<br />
Suspicion of malicious activity e.g. tampering with equipment<br />
Circumstances that lead to the provider no longer being able to provide an element of<br />
service.<br />
Page 24 of 28
Appendix E<br />
SENIOR MANAGER ON-CALL ARRANGEMENTS<br />
From 6 April 2008 CNCS (Central Nottinghamshire Clinical Services) provides a single call<br />
handling service for both the County PCT and Nottinghamshire Community <strong>Health</strong> Senior<br />
Manager on-call rotas.<br />
The contact telephone number is 0115 934 3236<br />
This will access the CNCS call centre who will contact the relevant Senior Manager on-call.<br />
The CNCS team will endeavour to answer all calls within one minute as part of the partner service<br />
agreement with the PCT.<br />
Process for contacting the Senior Manager On-call<br />
1. If there are any urgent security issues, such as a suspected intruder, please phone the<br />
Police straight away as well as making a call to CNCS to contact the relevant On-call Senior<br />
Manager.<br />
2. Please identify to the call handler whether the incident relates to the County PCT or County<br />
Provider services (Nottinghamshire Community <strong>Health</strong>).<br />
3. CNCS will ask you for the following information:<br />
<br />
<br />
brief details of the incident<br />
contact details to include:<br />
Your name<br />
Your role<br />
Your team/base<br />
Where you are currently e.g. home, work base etc<br />
Contact telephone numbers<br />
4. CNCS will contact the PCT or NCH Senior Manager on-call.<br />
If the call relates to reporting a Major <strong>Incident</strong> which requires the PCT input, CNCS will<br />
contact the On Call Director to enable them to escalate the issue to the PCT Chief<br />
Executive.<br />
5. If for any reason you have not heard from the On-Call Manager, please phone again e.g.<br />
after 15 minutes if urgent or half an hour if non-urgent.<br />
6. If CNCS do not receive an answer to calls made to the mobile and home contact numbers<br />
provided for the manager they will leave a message asking them to contact CNCS regarding<br />
an on-call matter and will record the time and date of the call.<br />
7. If not successful in making contact with the senior manager and the matter is urgent, CNCS<br />
will contact the on-call Director. If it is a non-urgent matter they will wait up to half an hour<br />
for the call to be returned.<br />
8. Please ensure the NCH on-call incident log form is completed in full. Completed forms<br />
should be forwarded to the Operations Team at Ransom Hall as soon as possible, certainly<br />
by the next working day.<br />
Page 25 of 28
Appendix F<br />
Equality Impact Assessment Tool<br />
To be completed and attached to any procedural document when submitted to the<br />
appropriate committee for consideration and approval.<br />
PROCEDURE NAME<br />
<strong>Incident</strong> <strong>Reporting</strong> <strong>Policy</strong><br />
Yes/No<br />
Comments<br />
1. Does the policy/guidance affect one<br />
group less or more favourably than<br />
another on the basis of:<br />
Race<br />
Ethnic origins (including gypsies and<br />
travellers)<br />
Nationality<br />
Gender<br />
Culture<br />
Religion or belief<br />
Sexual orientation including lesbian,<br />
gay and bisexual people<br />
Age<br />
Disability - learning disabilities, physical<br />
disability, sensory impairment and<br />
mental health problems<br />
2. Is there any evidence that some groups<br />
are affected differently?<br />
3. If you have identified potential<br />
discrimination, are any exceptions<br />
valid, legal and/or justifiable?<br />
4. Is the impact of the policy/guidance<br />
likely to be negative?<br />
No<br />
No<br />
No<br />
No<br />
No<br />
No<br />
No<br />
No<br />
No<br />
No<br />
No<br />
No<br />
5. If so can the impact be avoided? No<br />
6. What alternatives are there to achieving<br />
the policy/guidance without the impact?<br />
No<br />
7. Can we reduce the impact by taking<br />
different action?<br />
If you have identified a potential discriminatory impact of this procedural document, please<br />
refer it to the sponsoring director, together with any suggestions as to the action required to<br />
avoid/reduce this impact.<br />
For further advice in respect of answering the above questions, please contact the Equality<br />
and Diversity Lead for NCH the Associate Director of Workforce<br />
No<br />
Page 26 of 28
Appendix G<br />
Plan for Dissemination of Policies or Procedural Documents<br />
To be completed and attached to any document which guides practice when submitted to the<br />
appropriate committee for consideration and approval.<br />
Acknowledgement: University Hospitals of Leicester NHS Trust.<br />
Title of<br />
document:<br />
<strong>Incident</strong> <strong>Reporting</strong> <strong>Policy</strong><br />
Date finalised: Feb 2010<br />
Previous<br />
document<br />
already being<br />
used?<br />
No<br />
(Please delete<br />
as appropriate)<br />
Dissemination lead:<br />
Print name and<br />
contact details<br />
Kieran Colton<br />
Head of<br />
Governance &<br />
Compliance<br />
If yes, in what<br />
format and<br />
where?<br />
N/A<br />
Proposed action<br />
to retrieve outof-date<br />
copies of<br />
the document:<br />
N/A<br />
To be<br />
disseminated to:<br />
How will it be<br />
disseminated, who<br />
will do it and<br />
when?<br />
Paper<br />
or<br />
Electronic<br />
Comments<br />
Dissemination Record - to be used once document is approved.<br />
Date put on intranet<br />
Date due to be reviewed<br />
Disseminated to:<br />
(either directly or<br />
via meetings, etc)<br />
Format (i.e.<br />
paper or<br />
electronic)<br />
Date<br />
Disseminate<br />
d<br />
No. of<br />
Copies<br />
Sent<br />
Contact Details /<br />
Comments<br />
Page 27 of 28
Appendix H<br />
Employee Record of Having Read the <strong>Policy</strong>/Procedure/Guidance<br />
Title of <strong>Policy</strong>/Procedure/Guidance:<br />
<strong>Incident</strong> <strong>Reporting</strong> <strong>Policy</strong><br />
I have read and understand the principles contained in the named policy.<br />
PRINT FULL NAME SIGNATURE DATE<br />
Page 28 of 28