BCN Referral and Clinical Review Program - e-Referral
BCN Referral and Clinical Review Program - e-Referral
BCN Referral and Clinical Review Program - e-Referral
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
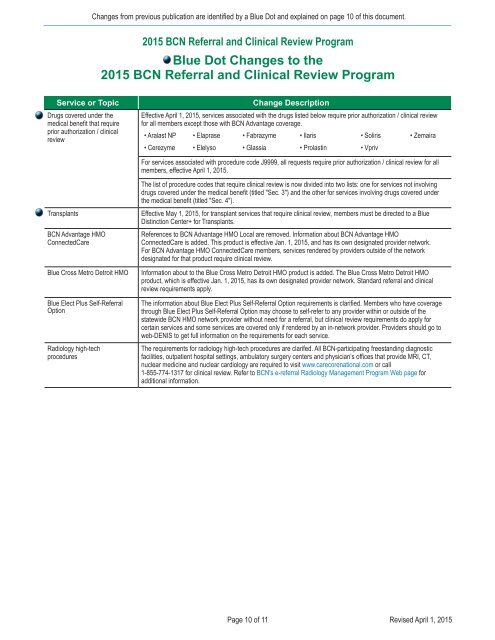
Changes from previous publication are identified by a Blue Dot <strong>and</strong> explained on page 10 of this document.2015 <strong>BCN</strong> <strong>Referral</strong> <strong>and</strong> <strong>Clinical</strong> <strong>Review</strong> <strong>Program</strong>Blue Dot Changes to the2015 <strong>BCN</strong> <strong>Referral</strong> <strong>and</strong> <strong>Clinical</strong> <strong>Review</strong> <strong>Program</strong>Service or TopicDrugs covered under themedical benefit that requireprior authorization / clinicalreviewChange DescriptionEffective April 1, 2015, services associated with the drugs listed below require prior authorization / clinical reviewfor all members except those with <strong>BCN</strong> Advantage coverage.• Aralast NP • Elaprase • Fabrazyme • Ilaris • Soliris • Zemaira• Cerezyme • Elelyso • Glassia • Prolastin • VprivFor services associated with procedure code J9999, all requests require prior authorization / clinical review for allmembers, effective April 1, 2015.Transplants<strong>BCN</strong> Advantage HMOConnectedCareBlue Cross Metro Detroit HMOBlue Elect Plus Self-<strong>Referral</strong>OptionRadiology high-techproceduresThe list of procedure codes that require clinical review is now divided into two lists: one for services not involvingdrugs covered under the medical benefit (titled "Sec. 3") <strong>and</strong> the other for services involving drugs covered underthe medical benefit (titled "Sec. 4").Effective May 1, 2015, for transplant services that require clinical review, members must be directed to a BlueDistinction Center+ for Transplants.References to <strong>BCN</strong> Advantage HMO Local are removed. Information about <strong>BCN</strong> Advantage HMOConnectedCare is added. This product is effective Jan. 1, 2015, <strong>and</strong> has its own designated provider network.For <strong>BCN</strong> Advantage HMO ConnectedCare members, services rendered by providers outside of the networkdesignated for that product require clinical review.Information about to the Blue Cross Metro Detroit HMO product is added. The Blue Cross Metro Detroit HMOproduct, which is effective Jan. 1, 2015, has its own designated provider network. St<strong>and</strong>ard referral <strong>and</strong> clinicalreview requirements apply.The information about Blue Elect Plus Self-<strong>Referral</strong> Option requirements is clarified. Members who have coveragethrough Blue Elect Plus Self-<strong>Referral</strong> Option may choose to self-refer to any provider within or outside of thestatewide <strong>BCN</strong> HMO network provider without need for a referral, but clinical review requirements do apply forcertain services <strong>and</strong> some services are covered only if rendered by an in-network provider. Providers should go toweb-DENIS to get full information on the requirements for each service.The requirements for radiology high-tech procedures are clarifed. All <strong>BCN</strong>-participating freest<strong>and</strong>ing diagnosticfacilities, outpatient hospital settings, ambulatory surgery centers <strong>and</strong> physician’s offices that provide MRI, CT,nuclear medicine <strong>and</strong> nuclear cardiology are required to visit www.carecorenational.com or call1-855-774-1317 for clinical review. Refer to <strong>BCN</strong>'s e-referral Radiology Management <strong>Program</strong> Web page foradditional information.Page 10 of 11Revised April 1, 2015