BCN Referral and Clinical Review Program - e-Referral
BCN Referral and Clinical Review Program - e-Referral
BCN Referral and Clinical Review Program - e-Referral
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
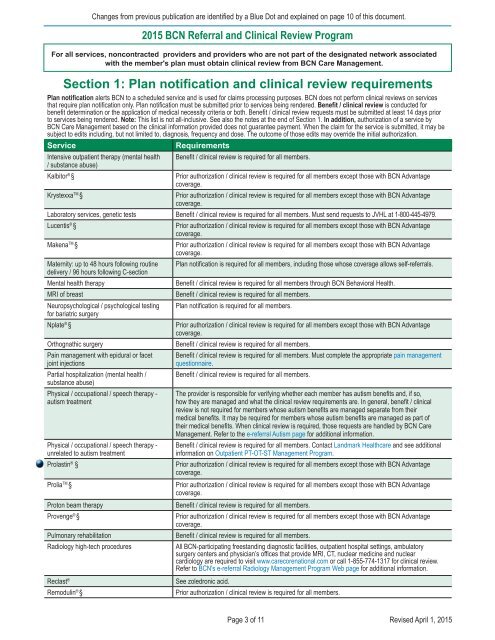
Changes from previous publication are identified by a Blue Dot <strong>and</strong> explained on page 10 of this document.Section 1: Plan notification <strong>and</strong> clinical review requirementsPlan notification alerts <strong>BCN</strong> to a scheduled service <strong>and</strong> is used for claims processing purposes. <strong>BCN</strong> does not perform clinical reviews on servicesthat require plan notification only. Plan notification must be submitted prior to services being rendered. Benefit / clinical review is conducted forbenefit determination or the application of medical necessity criteria or both. Benefit / clinical review requests must be submitted at least 14 days priorto services being rendered. Note: This list is not all-inclusive. See also the notes at the end of Section 1. In addition, authorization of a service by<strong>BCN</strong> Care Management based on the clinical information provided does not guarantee payment. When the claim for the service is submitted, it may besubject to edits including, but not limited to, diagnosis, frequency <strong>and</strong> dose. The outcome of those edits may override the initial authorization.ServiceIntensive outpatient therapy (mental health/ substance abuse)Kalbitor ® §Krystexxa TM §RequirementsBenefit / clinical review is required for all members.Prior authorization / clinical review is required for all members except those with <strong>BCN</strong> Advantagecoverage.Prior authorization / clinical review is required for all members except those with <strong>BCN</strong> Advantagecoverage.Laboratory services, genetic tests Benefit / clinical review is required for all members. Must send requests to JVHL at 1-800-445-4979.Lucentis ® §Makena TM §Maternity: up to 48 hours following routinedelivery / 96 hours following C-sectionMental health therapyMRI of breastNeuropsychological / psychological testingfor bariatric surgeryNplate ® §Orthognathic surgeryPain management with epidural or facetjoint injectionsPartial hospitalization (mental health /substance abuse)Physical / occupational / speech therapy -autism treatmentPhysical / occupational / speech therapy -unrelated to autism treatmentProlastin ® §Prolia TM §Proton beam therapyProvenge ® §Pulmonary rehabilitationRadiology high-tech procedures2015 <strong>BCN</strong> <strong>Referral</strong> <strong>and</strong> <strong>Clinical</strong> <strong>Review</strong> <strong>Program</strong>For all services, noncontracted providers <strong>and</strong> providers who are not part of the designated network associatedwith the member's plan must obtain clinical review from <strong>BCN</strong> Care Management.Prior authorization / clinical review is required for all members except those with <strong>BCN</strong> Advantagecoverage.Prior authorization / clinical review is required for all members except those with <strong>BCN</strong> Advantagecoverage.Plan notification is required for all members, including those whose coverage allows self-referrals.Benefit / clinical review is required for all members through <strong>BCN</strong> Behavioral Health.Benefit / clinical review is required for all members.Plan notification is required for all members.Prior authorization / clinical review is required for all members except those with <strong>BCN</strong> Advantagecoverage.Benefit / clinical review is required for all members.Benefit / clinical review is required for all members. Must complete the appropriate pain managementquestionnaire.Benefit / clinical review is required for all members.The provider is responsible for verifying whether each member has autism benefits <strong>and</strong>, if so,how they are managed <strong>and</strong> what the clinical review requirements are. In general, benefit / clinicalreview is not required for members whose autism benefits are managed separate from theirmedical benefits. It may be required for members whose autism benefits are managed as part oftheir medical benefits. When clinical review is required, those requests are h<strong>and</strong>led by <strong>BCN</strong> CareManagement. Refer to the e-referral Autism page for additional information.Benefit / clinical review is required for all members. Contact L<strong>and</strong>mark Healthcare <strong>and</strong> see additionalinformation on Outpatient PT-OT-ST Management <strong>Program</strong>.Prior authorization / clinical review is required for all members except those with <strong>BCN</strong> Advantagecoverage.Prior authorization / clinical review is required for all members except those with <strong>BCN</strong> Advantagecoverage.Benefit / clinical review is required for all members.Prior authorization / clinical review is required for all members except those with <strong>BCN</strong> Advantagecoverage.Benefit / clinical review is required for all members.All <strong>BCN</strong>-participating freest<strong>and</strong>ing diagnostic facilities, outpatient hospital settings, ambulatorysurgery centers <strong>and</strong> physician’s offices that provide MRI, CT, nuclear medicine <strong>and</strong> nuclearcardiology are required to visit www.carecorenational.com or call 1-855-774-1317 for clinical review.Refer to <strong>BCN</strong>'s e-referral Radiology Management <strong>Program</strong> Web page for additional information.Reclast ®Remodulin ® §See zoledronic acid.Prior authorization / clinical review is required for all members.Page 3 of 11Revised April 1, 2015