BCN Referral and Clinical Review Program - e-Referral
BCN Referral and Clinical Review Program - e-Referral
BCN Referral and Clinical Review Program - e-Referral
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
DATE : 20/11/2012NORTH TIPP COUNTY COUNCILTIME : 12:13:04 PAGE : 1P L A N N I N G A P P L I C A T I O N SPLANNING APPLICATIONS RECEIVED FROM 12/11/12 TO 16/11/12under section 34 of the Act the applications for permission may be granted permission, subject to or without conditions, or refused;The use of the personal details of planning applicants, including for marketing purposes, maybe unlawful under the Data ProtectionActs 1988 - 2003 <strong>and</strong> may result in action by the Data Protection Commissioner, against the sender, including prosecutionFILENUMBER12/510384APPLICANTS NAMEAPP.TYPEDATERECEIVEDDEVELOPMENT DESCRIPTION AND LOCATIONCiaran Cowan E 13/11/2012 traditional single storey split level house, domesticgarage, septic tank percolation area <strong>and</strong> entrance(07/51/1277)LismakeeveBorrisoleighThurlesEISRECD.PROT.STRUIPC WASTELIC. LIC.12/510385 ABO Wind Irel<strong>and</strong> Ltd., P 13/11/2012 wind energy project comprising of five wind turbineseach with a maximum tip height of 126 metres.construction of new access tracks <strong>and</strong> the upgradingof existing tracks, an electrical substation, a borrowpit <strong>and</strong> associated works. The application is for a10 year permission; an E.I.S. accompanies theapplicationKnockcurraghbola CommonsKnockcurraghbola Crownl<strong>and</strong>sGraniera <strong>and</strong> ShevryY12/510386Benny Fogarty & Emily Lewis P 14/11/2012 dwelling, entrance, garage, with packagedwastewater treatment system <strong>and</strong> polishing filtersystem <strong>and</strong> with all associated site worksClonmoreTemplemoreCo. Tipperary
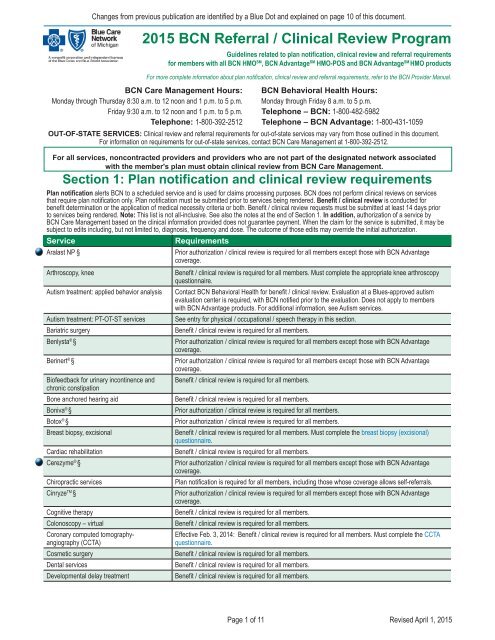
Changes from previous publication are identified by a Blue Dot <strong>and</strong> explained on page 10 of this document.Section 1: Plan notification <strong>and</strong> clinical review requirementsPlan notification alerts <strong>BCN</strong> to a scheduled service <strong>and</strong> is used for claims processing purposes. <strong>BCN</strong> does not perform clinical reviews on servicesthat require plan notification only. Plan notification must be submitted prior to services being rendered. Benefit / clinical review is conducted forbenefit determination or the application of medical necessity criteria or both. Benefit / clinical review requests must be submitted at least 14 days priorto services being rendered. Note: This list is not all-inclusive. See also the notes at the end of Section 1. In addition, authorization of a service by<strong>BCN</strong> Care Management based on the clinical information provided does not guarantee payment. When the claim for the service is submitted, it may besubject to edits including, but not limited to, diagnosis, frequency <strong>and</strong> dose. The outcome of those edits may override the initial authorization.ServiceIntensive outpatient therapy (mental health/ substance abuse)Kalbitor ® §Krystexxa TM §RequirementsBenefit / clinical review is required for all members.Prior authorization / clinical review is required for all members except those with <strong>BCN</strong> Advantagecoverage.Prior authorization / clinical review is required for all members except those with <strong>BCN</strong> Advantagecoverage.Laboratory services, genetic tests Benefit / clinical review is required for all members. Must send requests to JVHL at 1-800-445-4979.Lucentis ® §Makena TM §Maternity: up to 48 hours following routinedelivery / 96 hours following C-sectionMental health therapyMRI of breastNeuropsychological / psychological testingfor bariatric surgeryNplate ® §Orthognathic surgeryPain management with epidural or facetjoint injectionsPartial hospitalization (mental health /substance abuse)Physical / occupational / speech therapy -autism treatmentPhysical / occupational / speech therapy -unrelated to autism treatmentProlastin ® §Prolia TM §Proton beam therapyProvenge ® §Pulmonary rehabilitationRadiology high-tech procedures2015 <strong>BCN</strong> <strong>Referral</strong> <strong>and</strong> <strong>Clinical</strong> <strong>Review</strong> <strong>Program</strong>For all services, noncontracted providers <strong>and</strong> providers who are not part of the designated network associatedwith the member's plan must obtain clinical review from <strong>BCN</strong> Care Management.Prior authorization / clinical review is required for all members except those with <strong>BCN</strong> Advantagecoverage.Prior authorization / clinical review is required for all members except those with <strong>BCN</strong> Advantagecoverage.Plan notification is required for all members, including those whose coverage allows self-referrals.Benefit / clinical review is required for all members through <strong>BCN</strong> Behavioral Health.Benefit / clinical review is required for all members.Plan notification is required for all members.Prior authorization / clinical review is required for all members except those with <strong>BCN</strong> Advantagecoverage.Benefit / clinical review is required for all members.Benefit / clinical review is required for all members. Must complete the appropriate pain managementquestionnaire.Benefit / clinical review is required for all members.The provider is responsible for verifying whether each member has autism benefits <strong>and</strong>, if so,how they are managed <strong>and</strong> what the clinical review requirements are. In general, benefit / clinicalreview is not required for members whose autism benefits are managed separate from theirmedical benefits. It may be required for members whose autism benefits are managed as part oftheir medical benefits. When clinical review is required, those requests are h<strong>and</strong>led by <strong>BCN</strong> CareManagement. Refer to the e-referral Autism page for additional information.Benefit / clinical review is required for all members. Contact L<strong>and</strong>mark Healthcare <strong>and</strong> see additionalinformation on Outpatient PT-OT-ST Management <strong>Program</strong>.Prior authorization / clinical review is required for all members except those with <strong>BCN</strong> Advantagecoverage.Prior authorization / clinical review is required for all members except those with <strong>BCN</strong> Advantagecoverage.Benefit / clinical review is required for all members.Prior authorization / clinical review is required for all members except those with <strong>BCN</strong> Advantagecoverage.Benefit / clinical review is required for all members.All <strong>BCN</strong>-participating freest<strong>and</strong>ing diagnostic facilities, outpatient hospital settings, ambulatorysurgery centers <strong>and</strong> physician’s offices that provide MRI, CT, nuclear medicine <strong>and</strong> nuclearcardiology are required to visit www.carecorenational.com or call 1-855-774-1317 for clinical review.Refer to <strong>BCN</strong>'s e-referral Radiology Management <strong>Program</strong> Web page for additional information.Reclast ®Remodulin ® §See zoledronic acid.Prior authorization / clinical review is required for all members.Page 3 of 11Revised April 1, 2015
Changes from previous publication are identified by a Blue Dot <strong>and</strong> explained on page 10 of this document.2015 <strong>BCN</strong> <strong>Referral</strong> <strong>and</strong> <strong>Clinical</strong> <strong>Review</strong> <strong>Program</strong>Section 2: <strong>Referral</strong> requirementsGENERAL RULE. When members need specialty care, their primary care physician must submit a global referral to <strong>BCN</strong> for a contracted provider.A global referral allows the specialist to perform necessary services to diagnose <strong>and</strong> treat a member in the office, with the exception of services thatrequire benefit / clinical review. Specialists may not refer patients to other specialists. If the specialist determines services are needed outside thosespecified by a global referral, including further diagnosis or treatment in an alternate treatment setting (either outpatient or inpatient), the specialist isresponsible for submitting all required plan notifications or clinical review requests to <strong>BCN</strong>.EXCEPTIONS TO THE GENERAL RULE. The following are exceptions to the requirement for a global referral.• Global referrals cannot be used for chiropractic services or for physical, occupational or speech therapy; see Section 1 for those requirements.• <strong>BCN</strong>’s referral requirements vary based on the region assigned to the medical care group the member’s primary care physician is associated with.(See the Blue Care Network Provider Consultant Regions map at the end of this document.) For <strong>BCN</strong> HMO members not assigned to a U-M primarycare physician <strong>and</strong> living in the Mid, West or Upper Peninsula region, no global referral is required as long as the specialist is located in one of thoseregions. For <strong>BCN</strong> HMO members not assigned to a U-M primary care physician <strong>and</strong> living in the East or Southeast region, a referral is required.• For University of Michigan Premier Care, Premier Care 65 <strong>and</strong> GradCare members assigned to a non-U-M primary care physician <strong>and</strong> referred to anyspecialist (U-M or non-U-M), a referral is required. This guideline applies regardless of where the member lives or where the practitioners are located.• For <strong>BCN</strong> Advantage HMO-POS members in any region, no global referral is required as long as the specialist is part of the <strong>BCN</strong> Advantage HMO-POSnetwork.• For Blue Cross Partnered, <strong>BCN</strong> Advantage HMO ConnectedCare <strong>and</strong> <strong>BCN</strong> Advantage MyChoice Wellness members, services rendered by providersoutside of the network designated for each of those products require clinical review.• Blue Cross Metro Detroit HMO members must choose their primary care physician from within the Blue Cross Metro Detroit HMO provider network.That physician coordinates services within the Blue Cross Metro Detroit HMO provider network. St<strong>and</strong>ard referral <strong>and</strong> clinical review requirementsapply.• Members who have coverage through Blue Elect Plus Self-<strong>Referral</strong> Option may choose to self-refer to any provider within or outside of the statewide<strong>BCN</strong> HMO network provider without need for a referral, but clinical review requirements do apply for certain services <strong>and</strong> some services are coveredonly if rendered by an in-network provider. Providers should go to web-DENIS to get full information on the requirements for each service.• For members who have coverage through self-funded or other products that allow members to refer themselves directly to a specialist within adesignated provider network, no referral is required from the primary care physician in order to access specialist services within that network. However,benefit/clinical review requirements apply. Providers should always check Section 1 of this document for benefit/clinical review requirements.• Some services do not require a referral as long as the service is performed by a contracted provider. The table below provides a list of services that donot require a referral for ANY member. Note: This list is not all-inclusive.Note: When a referral does not need to be submitted to <strong>BCN</strong>, the primary care physician can "refer" the member to the specialist using any method thatcan be documented by both the primary care physician <strong>and</strong> the specialist -- for example, a written request, fax or prescription, or telephone notes.Office / outpatient / ancillary servicesPacemaker adjustmentsPediatric Choice services<strong>Referral</strong> is not required for any member.See <strong>BCN</strong> Requirements for Pediatric Choice <strong>Program</strong>.Radiology - routine (procedure codes other than those identified as high-tech) <strong>Referral</strong> is not required for any member. Also see Section 1.Specialist office visits <strong>and</strong> treatment See Section 1.Sterilization procedures (with appropriate benefit)Surgical procedures, routine See Section 1.Urgent careWoman's Choice services<strong>Referral</strong> is not required for any member.<strong>Referral</strong> is not required for any member.See Woman's Choice <strong>Referral</strong> <strong>and</strong> <strong>Clinical</strong> <strong>Review</strong> Guidelines.VENDOR CONTACT INFORMATIONVendor name Services Contact informationCareCore National <strong>Review</strong>s requests for select high-tech radiology procedures. www.carecorenational.com1-855-774-1317J&B Medical Supply <strong>Review</strong>s all requests for outpatient diabetic <strong>and</strong> insulin pump supplies 1-888-896-6233JVHL Provides statewide network <strong>and</strong> third-party administration for outpatient laboratory services 1-800-445-4979L<strong>and</strong>mark HealthcareProvides care management for members receiving physical, occupational <strong>and</strong> speech therapyservices in office <strong>and</strong> outpatient settings, including outpatient hospital settingsLMhealthcare.comNorthwood <strong>Review</strong>s all requests for outpatient nondiabetic DME, medical supplies <strong>and</strong> P&O 1-800-667-8496Page 7 of 11Revised April 1, 2015
Changes from previous publication are identified by a Blue Dot <strong>and</strong> explained on page 10 of this document.2015 <strong>BCN</strong> <strong>Referral</strong> <strong>and</strong> <strong>Clinical</strong> <strong>Review</strong> <strong>Program</strong>SEC. 3: For services not involving medications covered under the medical benefitProcedures That Require <strong>Clinical</strong> <strong>Review</strong>Procedure codes* (Note: This list is not all inclusive.)Note: ALL procedures with "not otherwise classified (NOC)," "unclassified," "unlisted" or "unspecified" codes require clinical review.00170 193400295T-0298T21208-2121019342 212150318T 19350 2123011920-1192215780-1578315786-1578915792-1579315819-1583015832-1583919355 212352987029873-2987729879-2988329885-2988719357 21240 304001936121242-2124940842-408455826041800 5827541805-4180641820-4182341825-4182830410 4183058291583535835658541-5854464479-6448064483-6448464490-6449567900-6790969710-697187032874160 78496 74170 74176-74178 74181-74183 7426375571-7557419364 21255 30420 41850 58550 70336 7638019366-1937121270 30430 4187058552-5855419380 21280 30435 41872 58563 70460 15847 19396 21282 30450 4187415876-158792101021295-2129617340 21050 2148017360 21060 2148517380 21070 2149019101 211161912019125-1912619300193161931819324-193251932821120-2112721141-2114721150-2115121154-2115521159-2116021493-21494225332255830620 4212031660-3166133361-3336933990-3399336468-3647136475-3647636478-3647943644-4364543770-4377543842-4384843886-438884413059840-5984159850-5985259855-5985762281-6228270450 7700377058-7705970470 7752070486-70488 70551-70553 71250 62287 71260 62310-6231162318-6231955970 6300522612 37718 55980 6301222630 37722 56805 6301727332-2733337765-3776657335 6303021188 27425 37780 58150 6304221193-2119929800 37785 58152 6304771270 72131-72133 72141-72142 72146-72149 72156-72158 72192-72194 73218-73223 73718-73723 77522-775237752578201-78202 78205-78206 78215-78216 78226-78227 78451-78454 90867-9086997112-97113S0190-S019197116 S019990901 97124 S208390911 97140 S220292507-9250892521-9252493797-9379895782-9578395800-9580195805-958119610597001-9700478466 9702278468-78469 78472-78473 971509753097532-9753397535975379754297545-975469775097010 9775597012 9918397014 A457597016 C130097018 G028997024G0398-G0400G0422-G042497026 L803978481 97028 L860078483 97032-9703619330 21206 29804 40840 58180 63056 74150 78494 97110 Q4100L8692S9472-S9473*CPT codes, descriptions <strong>and</strong> two-digit numeric modifiers only are copyright 2014 American Medical Association. All rights reserved. Effective July 1, 2014, clinical review requests for these procedures must be reviewed by CareCore National. Refer to <strong>BCN</strong>'s e-referral RadiologyManagement <strong>Program</strong> Web page for information on the CareCore National review process.Note: Additional details are provided about the services represented by these codes in the tables found earlier in this document.Page 8 of 11Revised April 1, 2015
Changes from previous publication are identified by a Blue Dot <strong>and</strong> explained on page 10 of this document.2015 <strong>BCN</strong> <strong>Referral</strong> <strong>and</strong> <strong>Clinical</strong> <strong>Review</strong> <strong>Program</strong>SEC. 4: For services involving medications covered under the medical benefitProcedures That Require <strong>Clinical</strong> <strong>Review</strong> §Procedure codes (Note: This list is not all inclusive.)Note: ALL procedures with "not otherwise classified (NOC)," "unclassified," "unlisted" or "unspecified" codes require clinical review.C9269-C9270J0215J0597-J0598J0897 J1459 J1566 J1740 J2778 J3357 J3590C9272-C9273J0256-J0257J0638 J1290 J1557J1568-J1569J1743 J2796 J3385 J9999J0178 J0490 J0641 J1300 J1559 J1572 J1786 J3060 J3489 Q2040J0180J0585-J0588J0800 J1325 J1561 J1725 J2507 J3285 J3490§ For medications covered under the medical benefit that require prior authorization / clinical review, providers are encouraged to submit requestsusing the e-referral system by including the necessary information in the e-referral Comments section. The requests may also be called in to <strong>BCN</strong>Care Management at 1-800-392-2512 or submitted using the Medical Benefit Drug Request Form. This form can be accessed on the e-referralForms Web page. In addition, see <strong>Clinical</strong> Information for Drugs Covered under the Medical Benefit That Require Medical Necessity <strong>Review</strong>, whichshows the clinical information <strong>and</strong> criteria for each drug.Note: Additional details are provided about the services represented by these codes in the tables found earlier in this document.Q2042-Q2044Page 9 of 11Revised April 1, 2015
Changes from previous publication are identified by a Blue Dot <strong>and</strong> explained on page 10 of this document.2015 <strong>BCN</strong> <strong>Referral</strong> <strong>and</strong> <strong>Clinical</strong> <strong>Review</strong> <strong>Program</strong>Blue Dot Changes to the2015 <strong>BCN</strong> <strong>Referral</strong> <strong>and</strong> <strong>Clinical</strong> <strong>Review</strong> <strong>Program</strong>Service or TopicDrugs covered under themedical benefit that requireprior authorization / clinicalreviewChange DescriptionEffective April 1, 2015, services associated with the drugs listed below require prior authorization / clinical reviewfor all members except those with <strong>BCN</strong> Advantage coverage.• Aralast NP • Elaprase • Fabrazyme • Ilaris • Soliris • Zemaira• Cerezyme • Elelyso • Glassia • Prolastin • VprivFor services associated with procedure code J9999, all requests require prior authorization / clinical review for allmembers, effective April 1, 2015.Transplants<strong>BCN</strong> Advantage HMOConnectedCareBlue Cross Metro Detroit HMOBlue Elect Plus Self-<strong>Referral</strong>OptionRadiology high-techproceduresThe list of procedure codes that require clinical review is now divided into two lists: one for services not involvingdrugs covered under the medical benefit (titled "Sec. 3") <strong>and</strong> the other for services involving drugs covered underthe medical benefit (titled "Sec. 4").Effective May 1, 2015, for transplant services that require clinical review, members must be directed to a BlueDistinction Center+ for Transplants.References to <strong>BCN</strong> Advantage HMO Local are removed. Information about <strong>BCN</strong> Advantage HMOConnectedCare is added. This product is effective Jan. 1, 2015, <strong>and</strong> has its own designated provider network.For <strong>BCN</strong> Advantage HMO ConnectedCare members, services rendered by providers outside of the networkdesignated for that product require clinical review.Information about to the Blue Cross Metro Detroit HMO product is added. The Blue Cross Metro Detroit HMOproduct, which is effective Jan. 1, 2015, has its own designated provider network. St<strong>and</strong>ard referral <strong>and</strong> clinicalreview requirements apply.The information about Blue Elect Plus Self-<strong>Referral</strong> Option requirements is clarified. Members who have coveragethrough Blue Elect Plus Self-<strong>Referral</strong> Option may choose to self-refer to any provider within or outside of thestatewide <strong>BCN</strong> HMO network provider without need for a referral, but clinical review requirements do apply forcertain services <strong>and</strong> some services are covered only if rendered by an in-network provider. Providers should go toweb-DENIS to get full information on the requirements for each service.The requirements for radiology high-tech procedures are clarifed. All <strong>BCN</strong>-participating freest<strong>and</strong>ing diagnosticfacilities, outpatient hospital settings, ambulatory surgery centers <strong>and</strong> physician’s offices that provide MRI, CT,nuclear medicine <strong>and</strong> nuclear cardiology are required to visit www.carecorenational.com or call1-855-774-1317 for clinical review. Refer to <strong>BCN</strong>'s e-referral Radiology Management <strong>Program</strong> Web page foradditional information.Page 10 of 11Revised April 1, 2015
Blue Cross Blue Shield of Michigan<strong>and</strong> Blue Care NetworkProvider Consultant Regionsbcbsm.comKeweenawHoughtonOntonagonBaragaGogebicIronDickinsonMarquetteAlgerDeltaSchoolcraftLuceMackinacChippewaMenomineeEmmetUpper PeninsulaCharlevoixCheboyganPresqueIsleWest regionAntrim Otsego MontmorencyAlpenaEast regionProvider consultantregional toll-free numbers:Upper Peninsula1-866-497-7647West Michigan1-800-968-2583East Michigan1-800-527-1906Mid Michigan1-877-258-0168Southeast1-866-299-4667MasonOceanaBenzieManisteeMuskegonLeelanauOttawaAlleganVan BurenLakeNewaygoGr<strong>and</strong>TraverseWexford Missaukee Roscommon Ogemaw IoscoKentOsceolaMecostaKalamazooMontcalmBarryKalkaska Crawford Oscoda AlconaIoniaClareIsabellaCalhounEatonGratiotClintonGladwinMidl<strong>and</strong>InghamJacksonArenacSaginawShiawasseeBayLivingstonGeneseeWashtenawTuscolaOakl<strong>and</strong>LapeerWayneHuronSanilacMacombSt. ClairMid regionSoutheast regionBerrien Cass St. JosephBranchHillsdaleLenaweeMonroeHere’s how to find more comprehensive contact information:1 Log in at bcbsm.com/provider. 2 Click on web-DENIS. 3 Click either BCBSM Contact Us or<strong>BCN</strong> Contact Us.Updated June 2014R011579