emt-basic curriculum module 4
emt-basic curriculum module 4
emt-basic curriculum module 4
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationMODULE 4Medical/BehavioralandObstetrics/GynecologyLesson 4-1General PharmacologyModule 4-1
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationOBJECTIVES LEGENDC=Cognitive P=Psychomotor A=Affective1 = Knowledge level2 = Application level3 = Problem-solving levelOBJECTIVESCOGNITIVE OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:4-1.1 Identify which medications are carried on board an ambulance licensedat the EMT-Basic level in Wisconsin. (C-1)4-1.2 Identify the medications with which the EMT-Basic may assist thepatient with administration at the EMT-Basic level in Wisconsin. (C-1)4-1.3 List the components of a drug profile. (C-1)4-1.4 Identify the different forms in which medications are found. (C-1)4-1.5 Summarize the “6 R’s” in the administration of a medication. ((C-1)4-1.6 Explain the importance of medical control involvement and medicationadministration. (C-1)4-1.7 Describe how allergies to medications can affect patients. (C-1)4-1.8 State the importance of determining the preexistence of a medicationallergy. (C-1)4-1.9 Differentiate between what is meant by a medication allergy versusmedication intolerance. (C-2)4-1.10 Identify the general steps in administering a medication to a patient.(C-2)4-1.11 State the rationale for administering most medications to pediatricpatients based upon weight. (C-1)4-1.12 Define the concept of polypharmacy as it relates to geriatric patients.(C-1)AFFECTIVE OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:4-1.13 Examine the importance of correctly administering medications tospecific patients. (C-3)PSYCHOMOTOR OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:4-1.14 Demonstrate general steps for assisting patient with self-administrationof medications. (P-2)4-1.15 Demonstrate general steps involved in administering a medication to apatient. (P-2)Module 4-2
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education4-1.16 Read the labels and inspect each type of medication that can beadministered by the EMT-Basic. (P-2)4-1.17 Create a drug profile for each of the medications that can beadministered by the EMT-Basic. (P-1)PREPARATIONMotivation:Later in this course the EMT-Basic student will belearning specific medications which may be administeredto a patient, for a specific medical condition.Administering medications is an important responsibilityof the EMT. Giving medications to pediatric and geriatricpatients requires special consideration. They must onlybe given following thorough evaluation and permissionfrom medical control.Prerequisites:AV Equipment:EMS Equipment:Primary Instructor:Assistant Instructor:BLS, Preparatory, Airway and Patient Assessment.MATERIALSUtilize various audio-visual materials relating to generalpharmacology. The continuous design and developmentof new audio-visual materials relating to EMS requirescareful review to determine which best meet the needs ofthe program. Materials should be edited to assuremeeting the objectives of the <strong>curriculum</strong>.NonePERSONNELAdvanced-level provider who has administeredmedications.The instructor-to-student ratio should be 1:6 forpsychomotor skill practice. Individuals used as assistantinstructors should be knowledgeable in generalpharmacology.PRESENTATIONDeclarative (What)I. Overview - the importance of medications and the concerns associated withtheir administrationModule 4-3
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationII.III.IV.Medications carried on board (*may be carried on board the EMT-BasicService in Wisconsin, with required additional training and approval)A. Activated CharcoalB. Oral GlucoseC. *GlucagonD. OxygenE. Albuterol, nebulizedF. *Atrovent, nebulizedG. AspirinH. *Epinephrine, auto-injectorI. MARK 1 Kit (Atropine and 2-PAM Chloride)Medications that are prescribed by a physician and the patient has in his/herpossession. May assist patients, with approval by medical direction.A. Metered Dose Inhalers – Albuterol, AtroventB. NitroglycerinC. Epinephrine, auto-injectorDrug Profile - information about medications that every EMT-Basic should beaware of prior to administering any medicationA. Drug names-generic and tradeB. Mechanism of actionC. IndicationsD. ContraindicationsE. Medication formsF. DoseG. RouteH. Side effectsV. Medication namesA. Generic1. The name listed in the U.S. Pharmacopedia, a governmentalpublication listing all drugs in the U.S2. Name assigned to drug before it becomes officially listed.Usually a simple form of the chemical name.3. Not capitalized4. Examples include activated charcoal, albuterol, aspirin, glucose,epinephrineB. Trade1. Brand name is the name a manufacturer uses in marketing thedrug2. Capitalized3. Examples include Super Char, Proventil, Bayer, Insta-glucose,Epi-pen Auto-injectorVI.VII.Mechanism of Action-the desired effect that a particular medication has uponbody systems and their function.Indications - the indication for a drug's use includes the most common uses ofthe drug in treating a specific illnessModule 4-4
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationVIII. Contraindications - situations in which a drug should not be used because itmay cause harm to the patient or offer no effect in improving the patient'scondition or illnessIX. Medication FormA. Types:1. Compressed powders or tablets - nitroglycerin2. Liquids for injection – epinephrine and glucagon3. Gels – glucose4. Suspensions - activated charcoal5. Fine powder for inhalation – metered-dose inhaler6. Gases - oxygen7. Sublingual spray - nitroglycerin8. Liquid/vaporized nebulizers – alubterol and AtroventB. Each drug is in a specific medication form to allow properly controlledconcentrations of the drug to enter into the blood stream where it hasan effect on the target body systemX. Dose - state how much of the drug should be givenXI. Routes of Administration - state route by which the medication is administeredasA. Oral – swallowedB. Sublingual - absorbed through mucous membranesC. Intramuscular injection - injected into muscleD. Subcutaneous injection - injected into subcutaneous tissueE. Intravenous - administered into veins (not an EMT B skill)F. Endotrachial - administered into an ET tube (not an EMT B skill)XII. Side EffectsA. Actions of a drug other than those desiredB. Some side effects may be predictableC. Intolerance - the severity of side effects may outweigh expectedbenefits of the medicationD. Allergy1. Can occur with medication administration if patient ishypersensitive to that medication2. If severe, may cause swelling of airway tissues3. Be alert for signs and symptoms of severe allergic reaction (seesection on Severe Allergic Reactions)4. Identify preexisting allergies during patient history to avoidpotentially adverse or fatal response to medicationsE. Involve medical control in medication administration1. Adequate consideration of indications and contraindications2. Adequate consideration of potential medication interaction3. Possible adjustment of usual dose based on age, weight andrelative contraindicationsXIII. The “6 Rs” of medication administrationA. Right patientB. Right drugModule 4-5
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationKinesthetic (Do)1. The student will practice inspecting and reading the labels of each type ofmedication they will use on the EMS unit.2. The student will create a drug profile for each medication discussed for use atthe EMT-Basic level.INSTRUCTOR ACTIVITIES1. Supervise student practice.2. Reinforce student progress in cognitive, affective, and psychomotor domains.3. Redirect students having difficulty with content (complete remediation forms).EVALUATIONWritten:Practical:Develop evaluation instruments, e.g., quizzes, verbal reviews,handouts, to determine if the students have met the cognitiveand affective objectives of this lesson.Evaluate the actions of the EMT-Basic students during role play,practice or other skill stations to determine their compliance withthe cognitive and affective objectives and their mastery of thepsychomotor objectives of this lesson.REMEDIATIONIdentify students or groups of students who are having difficulty with this subjectcontent. Complete remediation sheet from the instructor's course guide.ENRICHMENTWhat is unique in the local area concerning this topic? Complete enrichment sheetsfrom the instructor's course guide and attach with lesson plan.Module 4-7
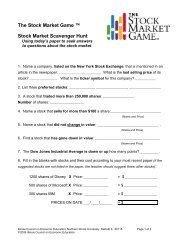
HBF-TWN Trade & Gender Briefs5Table 1: The Shift from WTO to FTAs by Provisions/ Chapters and Associated Gender ImplicationsArea/ Provision WTO FTAs Gender ImplicationsPrincipleDevelopmentConcessionReciprocityOften adverse as SP concessions are not allowedCommodity Trade:TariffsFrom BoundRates, losesflexibilityActual Applied Rates,loses full protectionDeveloping countries lose more under both. FTAs create realcompetition for all groups, small producers may lose as they are notbacked by big capitalNTBs: Standards,TBTsAgreementAffirmation of WTOlevels or often moreWomen producers may find it more difficult to meet higherstandards and technical process requirementsNAMA: Anticoncentrationclause and sectoralsYes (beingnegotiated)May be includedUnder the anti-concentration clause, entire sectors cannot beprotected, a problem where women dominate. Under ‘sectorals’stiff competition opens up in sectors covered with immediate effectLabour standards Not Included May be included inFTAs with developedcountriesMay be good for women workers but inclusion in trade agreementsis controversialInvestmentOnly traderelatedinvestment isdiscussedYes, throughinvestment chaptersMay allow significant market access and protection for foreigninvestors which may increase competition for womenentrepreneurs. Women may get more jobs in foreign enterprises butFDI is also often labour saving and targets women’s labourIntellectualProperty RightsYes, but TRIPSunder WTO offersmany flexibilitiesTRIPS plus provisionsare coming in throughFTAsWomen can lose as they are weaker in terms of access toknowledge and technology and at registering IP instruments suchas patents, copyrights, trademarks, etc.Publicprocurement,competition policyNot included onmandatory basisMay be included inFTAs with developedcountriesCan take away certain benefits for women producers in publicprocurement and certain state subsidiesReferencesGhosh, Jayati (2006) “Note on Gender and Macroeconomics”, Paper submitted and presented at session on 'Integration of GenderPerspectives in Macroeconomics', Commission on the Status of Women, Forty-ninth session, United Nations, 28 February-11March, New York.Hirway, Indira and Seeta Prabhu (2009) Global Economic Crisis: Impact on the Poor in India – A Synthesis of Sector Studies,UNDP.Jhabvala, Renana (2003) Globalization, Liberalization and Women in the Informal Economy” in Veena Jha (ed.) Trade,Globalisation, and Gender: Evidence from South Asia, UNIFEM in collaboration with UNCTAD, New DelhiNational Commission for Enterprises in the Unorganised Sector (2007): Report on Conditions of Work and Promotion ofLivelihoods in the Unorganised Sector, Government of India, August, New Delhi.Sengupta, Ranja and Abhilash Gopinath (2009) The Current Trade Framework and Gender Linkages in Developing Economies:An Introductory Survey of Issues with Special Reference to India’, Trade and Gender Series, Paper I, Centad and Heinrich BollFoundation, DecemberTran-Nguyen, A-N and A Beviglia Zampetti (2004) Trade and Gender: Opportunities and Challenges for Developing Countries,UNCTAD, GenevaVan Staveren, Irene, Diane Elson, Caren Grown and Nilufer Cagatay (eds.) (2007) The Feminist Economics of Trade, Colchest:Francis Taylor Group, 2007. ISBN 978 0 415 43637 38This Brief is the fifth of the ‘Trade and Gender Briefs’ Series published by the Third World Network (TWN) andHeinrich Boell Foundation (HBF) India. The series is published for information dissemination on issues related to thegender specific impacts of trade liberalisation in India and other developing economies.Author: Ranja Sengupta Date of Publication: August 2012 Printed by: InditeGlobal, New DelhiFor More Information: Contact Ranja Sengupta at ranja.sengupta@gmail.comDisclaimer: The views analysis and conclusions are of the authors only and may not necessarily reflect the views or position ofTWN & HBF. Readers are encouraged to quote or cite this Brief with due acknowledgement to the authors, TWN & HBF.Copyright: This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 License.Acknowledgement: Shalini Yog, Santhosh M.R., and to Centad for including this brief in its “Trade and Gender AdvocacyProjects, August 2012.
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationOBJECTIVES LEGENDC=Cognitive P=Psychomotor A=Affective1 = Knowledge level2 = Application level3 = Problem-solving levelOBJECTIVESCOGNITIVE OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:4-2.1 List the key structures, and their function, of the respiratory system.(C-1)4-2.2 List signs and symptoms of adequate air exchange. (C-1)4-2.3 List signs and symptoms of inadequate air exchange. (C-1)4.2-4 Differentiate between upper airway obstruction and a lower airwaydisease in the adult patient. (C-3)4-2.5 Differentiate between upper airway obstruction and airway diseases inthe pediatric patient. (C-3)4-2.6 Recognize the need for medical direction to assist in the emergencymedical care of the patient with breathing difficulty. (C-3)4-2.7 Establish the relationship between airway management and the patientwith breathing difficulty. (C-3)4-2.8 Identify appropriate treatment and management for the adult patient inrespiratory distress due to a common respiratory disease. (C-1)4-2.9 Identify appropriate treatment and management for the pediatricpatient in respiratory distress due to a common respiratory disease.(C-1)4-2.10 List common trade names, action, indications, contraindications, forms,dose, route and side effects of albuterol. (C-1)4-2.11 List common trade names, action, indications, contraindications, forms,dose, route and side effects of ipratropium bromide (Atrovent). (C-1)4-2.12 Distinguish between the emergency medical care of the infant, childand adult patient with signs of respiratory distress.(C-3)4-2.13 Identify common respiratory diseases of the adult patient. (C-1)4-2.14 Identify common respiratory diseases of the pediatric patient. (C-1)AFFECTIVE OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:4-2.15 Defend EMT-Basic treatment regimens for various respiratoryemergencies.(A-1)4-2.16 Explain the rationale for administering albuterol.(A-3)4-2.17 Explain the rationale for administering Atrovent. (A-3)PSYCHOMOTOR OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:Module 4-9
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education4-2.18 Demonstrate the emergency medical care for a patient in respiratorydistress. (P-2)4-2.19 Perform the steps in assisting a patient with the use of their metereddose inhaler. (P-2)4-2.20 Perform the steps in administering a nebulizer treatment, via hand-heldand mask, to a patient in respiratory distress. (P-2)4-2.21 Create a management plan to properly evaluate and treat an adultpatient in respiratory distress. (P-3)4-2.22 Create a management plan to properly evaluate and treat a pediatricpatient in respiratory distress. (P-3)PREPARATIONMotivation:Over 200,000 persons die from respiratory emergencieseach year.One large city reported 12% of their ambulance runswere respiratory emergencies. This represented threetimes the calls for heart attacks.A child with severe respiratory distress will deteriorateinto respiratory failure and circulatory collapse, eventuallyresulting in respiratory arrest. The use of oxygen canblock this progression and may even reverse it to somedegree. When possible, deliver humidified oxygen andallow the child to remain in the parent's lap. A morecomfortable, secure child will require less oxygen. Havethe parent accompany the child in the ambulance. Thereis no contraindication to high concentration oxygen in theinfant or child patient.Prerequisites:AV Equipment:EMS Equipment:BLS, Preparatory, Airway and Patient Assessment.MATERIALSUtilize various audio-visual materials relating torespiratory emergencies. The continuous design anddevelopment of new audio-visual materials relating toEMS requires careful review to determine which bestmeet the needs of the program. Materials should beedited to assure meeting the objectives of the <strong>curriculum</strong>.Metered-dose and hand-held nebulizers suitable fortraining purposes and various spacer devices.Module 4-10
State of WisconsinPrimary Instructor:Assistant Instructor:EMT-Basic: A Practice BasedApproach to EMS EducationPERSONNELOne Advanced-Level Provider or EMT-Basic instructorwho is knowledgeable in respiratory diseases andhandheld inhalers.The instructor-to-student ratio should be 1:6 forpsychomotor skill practice. Individuals used as assistantinstructors should be knowledgeable in respiratoryemergencies.PRESENTATIONDeclarative (What)I. AnatomyA. Respiratory1. Nasal cavity (humidify, filter and warm) and oral cavity (airpassage)2. Pharynx - air passagea) Nasopharynxb) Oroopharynx3. Epiglottis - a leaf-shaped structure that prevents food and liquidfrom entering the trachea during swallowing4. Trachea – air passage5. Larynxa) Thyroid cartilage – cartilage forming the upper portion ofthe larynx, providing protection for vocal cordsb) Cricoid cartilage - cartilage ring forming the lower portionof the larynx6. Bronchi, right and left main stem - two major branches of thetrachea, passing air into the lungs7. Bronchioles - subdivisions of the bronchi, responsible forcontinued air passage8. Alveoli – single celled structures within the lung where gasexchange occurs9. Diaphragm and intercostals musclesa) Inhalation (active phase)(1) Diaphragm and intercostal muscles contract,increasing the size of the thoracic cavity(a) Diaphragm moves slightly downward, flareslower portion of rib cage(b) Ribs move upward/outward(2) Air flows into the lungsb) Exhalation (relaxation phase)(1) Diaphragm and intercostal muscles relax,decreasing the size of the thoracic cavityModule 4-11
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education(a) Diaphragm moves upward(b) Ribs move downward/inward(2) Air flows out of the lungs10. Respiratory physiologya) Alveolar/capillary exchange(1) Oxygenated air enters the alveoli during eachinspiration(2) Carbondioxide from the capillaries passes into thealveoli and is eliminated during each expiration(3) Oxygen enters the capillaries as carbon dioxideenters the alveolib) Capillary/cellular exchange(1) Cells give up carbon dioxide to the capillaries(2) Capillaries give up oxygen to the cellsc) Adequate breathing(1) Normal Rate(a) Adult - 12-20/minute(b) Child - 15-30/minute(c) Infant - 25-50/minute(2) Rhythm(a) Regular(b) Irregular(3) Quality(a) Breath sounds - present and equal(b) Chest expansion - adequate and equal(c) Effort of breathing - use of accessorymuscles - predominantly in infants andchildren(4) (Depth (tidal volume) - adequated) Inadequate breathing(1) Rate - outside of normal ranges(2) Rhythm - irregular(3) Quality(a) Breath sounds - diminished or absent(b)(c)Chest expansion - unequal or inadequateIncreased effort of breathing - use ofaccessory muscles - predominantly ininfants and children(4) Depth (tidal volume) - inadequate/shallow(5) The skin may be pale or cyanotic (blue) and cooland clammy(6) There may be retractions above the clavicles,between the ribs and below the rib cage,especially in children(7) Nasal flaring may be present, especially inchildrenModule 4-12
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationII.(8) In infants, there may be "seesaw" breathing wherethe abdomen and chest move in oppositedirections(9) Agonal breathing (occasional gasping breaths)may be seen just before death11. Infant and child anatomy considerationsa) Mouth and nose - in general: All structures are smallerand more easily obstructed than in adults.b) Pharynx - infants' and children's tongues take upproportionally more space in the mouth than adultsc) Trachea(1) Infants and children have narrower tracheas thatare obstructed more easily by swelling(2) The trachea is softer and more flexible in infantsand childrend) Cricoid cartilage - like other cartilage in the infant andchild, the cricoid cartilage is less developed and less rigide) Diaphragm - chest wall is softer, infants and children tendto depend more heavily on the diaphragm for breathingB. Adequate and inadequate artificial ventilation1. An EMT-Basic is adequately artificially ventilating a patientwhen:a) The chest rises and falls with each artificial ventilation(adequate tidal volume)b) The rate is sufficient, approximately 12 per minute foradults and 20 times per minute for children and infantsc) Heart rate and skin condition return to normal withsuccessful artificial ventilation2. Artificial ventilation is inadequate when:a) The chest does not rise and fall with artificial ventilation(inadequate tidal volume)b) The rate is too slow or too fastc) Heart rate does not return to normal with artificialventilationBreathing DifficultyA. Signs and symptoms1. Shortness of breath2. Restlessness3. Increased pulse rate4. Increased breathing rate5. Decreased breathing rate6. Skin color changesa) Cyanotic (blue-gray)b) Palec) Flushed (red)7. Noisy breathingModule 4-13
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationIII.a) Crowing-upper airway compromiseb) Audible wheezing-lower airway compromisec) Gurgling-upper airway compromised) Snoring-upper airway compromisee) Stridor-upper airway compromise(1) A harsh sound heard during breathing(2) Upper airway obstruction8. Inability to speak due to breathing efforts9. Retractions - use of accessory muscles10. Shallow or slow breathing may lead to altered mental status(with fatigue or obstruction)11. Abdominal breathing (diaphragm only)12. Coughing13. Irregular breathing rhythm14. Patient positiona) Tripod positionb) Sitting with feet dangling, leaning forward15. Unusual anatomy (barrel chest)16. Nasal flaring17. Pursed-lip breathingCommon respiratory diseases – adultsA. Reactive Airway Disease (RAD)1. Asthma – occurs in acute episodes and is triggered by exposureto an irritant, resulting in inflammation and swelling of theairways, tightening of the muscles surrounding bronchi andbronchioles (bronchoconstriction) and production of mucus.Triggers include cold air, dust, strong fumes, exercise, inhaledirritants, emotional upsets and smoke.a) Signs and symptoms(1) Wheezing(2) Coughing(3) Shortness of breath(4) Anxiety(5) Tightness of the chest(6) Fever is rarely present(7) Tripod position(8) Inability to speak full sentences(9) Pursed-lip breathingb) Patient management/treatment(1) Monitor ABCs(2) Oxygen(3) Position of comfort(4) Respiratory medication administration withapproval from medical direction (albuterol,Atrovent, etc.)Module 4-14
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education2. Pneumonia – an inflammation of the lungs caused by bacteriaor viral infection, usually triggered by a simple upper respiratorytract infection or flu; associated with fever, cough and excessproduction of sputum. Fluid accumulation separates alveolifrom surrounding capillary beds, inhibiting gas exchangea) Signs and symptoms(1) Dyspnea(2) Increased respiratory rate(3) Increased pulse rate(4) Fever, chills(5) Low blood pressure(6) Pale or cyanotic skin(7) Altered LOC (advanced stage)(8) Coughing up sputum(9) Fatigueb) Patient management/treatment(1) Monitor ABCs(2) Oxygen(3) TransportB. Chronic Obstructive Pulmonary Disease (COPD) – chronic respiratorydiseases that are characterized by obstruction to airflow that severelyinterferes with normal breathing and the gas exchange process.Chronic bronchitis and emphysema typically co-exist. Smoking,second-hand smoke, industrial pollutants and history of childhoodrespiratory infections are commonly attributed to the development ofCOPD.1. Chronic Bronchitis – chronic inflammation and scarring of thelining of the bronchioles, associated with a heavy mucus buildup that restricts gas exchange.a) Signs and symptoms(1) Shortness of breath(2) Fatigue(3) Coughing(4) Fever possible(5) Production of sputum(6) Cyanosisb) Patient management/treatment(1) Monitor ABCs(2) Oxygen(3) Respiratory medications may be advised bymedical direction(4) Transport2. Emphysema – chronic disease process resulting in thedestruction of alveoli and loss of elasticity of the lungs, makingadequate gas exchange difficulta) Signs and symptomsModule 4-15
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationIV.(1) Shortness of breath(2) Barrel-shaped chest(3) Thin appearance(4) Wheezing(5) Fatigueb) Patient management/treatment3. Monitor ABCs4. Oxygen5. Respiratory medications may be advised by medical direction6. TransportC. Hyperventilation Syndrome – rapid, shallow breathing usually broughton by anxiety or emotional upset, that results in an imbalance innormal levels of carbondioxide.1. Signs and symptomsa) Shortness of breathb) Numbness and tingling around the mouth and handsc) Lightheadednessd) Spasms of the hand and feete) Fainting2. Patient management/treatmenta) Coach patient to slow breathing rate and relaxb) Transport for evaluation of underlying cause if neededCommon respiratory diseases – pediatricsA. Asthma-bronchioles spasm and constrict, swelling bronchialmembrane, reducing airway size, and producing mucus (see previousdiscussion on asthma)B. Croup-viral infection that results in swelling and inflammation of thelining of the upper airways, occurring mostly in winter months1. Signs and symptoms (occurring mostly at night or when thechild is upset or crying)a) Loud cough, sounding like a seal’s barkb) Difficulty breathingc) Gruntingd) Wheezinge) Cold-like symptomsf) Stridor (high-pitched, squeaking noise)g) Pale or cyanosish) Retractionsi) Nasal flaringj) Sick appearancek) Drooling2. Patient management/treatmenta) Monitor ABCsb) Oxygen, blow-byc) Position of comfortd) TransportModule 4-16
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationC. Epiglottitis - condition that resembles croup, caused by bacterialinfection that inflames and swells the epiglottis, closing off air passage;a true medical emergency that may result in death if not treatedrapidly; typically occurs in children ages 2-4 (can occur in adults)1. Signs and symptomsa) Feverb) Sore throatc) Difficulty breathingd) Droolinge) Difficulty swallowingf) Stridorg) Hoarsenessh) Chillsi) Cyanosis2. Patient management/treatmenta) Gentle, calm, reassuring careb) Oxygen, blow-byc) Position of comfort (usually sitting on parent’s lap)d) Rapid transportD. Cardiac arrest-almost all result from airway obstruction or respiratoryarrest; or traumatic injuryV. Emergency Medical Care-Initial AssessmentA. Establish an open airwayB. Begin positive pressure ventilations with oxygen if unconscious,administer high flow oxygen if patient is responsiveC. High priority and rapid transportVI. Emergency Medical Care - Focused History and Physical ExamA. Important questions to ask1. Onset2. Provocation3. Quality4. Radiation5. Severity6. Time7. InterventionsB. SAMPLE HistoryC. Baseline Vital SignsD. Effort of Breathing1. Complains of trouble breathinga) Apply oxygen if not already doneb) Assess baseline vital signs2. Consult medical directiona) Assist patient with metered dose inhaler or administrationof nebulizer(1) Repeat as directed(2) Continue focused assessmentModule 4-17
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationVII.VIII.(3) Document administration and effect of medicationRelationship to Airway Management - should be prepared to intervene withappropriate oxygen administration and artificial ventilation supportMedicationsA. Metered dose inhalers (MDI)1. Medication name (most commonly used)a) Generic - albuterol, isoetharine, metaproteranol, etc.b) Trade - Proventil, Ventolin, Bronkosol, Bronkometer,Alupent, Metaprel, etc.2. Indications - meets all of the following criteria:a) Exhibits signs and symptoms of respiratory emergency,b) Has physician prescribed handheld inhaler, andc) Specific authorization by medical direction3. Contraindicationsa) Inability of patient to use deviceb) Inhaler is not prescribed for the patientc) No permission from medical directiond) Patient has already met maximum prescribed dose priorto EMT-Basic arrivale) Possible allergic reactions would have previously beenruled out by the patient’s physician prior to writing aprescription4. Medication form - handheld metered dose inhaler5. Dosage - number of inhalations based upon medical direction'sorder or physician's order based upon consultation with thepatient6. Administration - inhaleda) Obtain order from medical direction either on-line oroff-lineb) Assure right medication, right patient, right route, patientalert enough to use inhalerc) Check the expiration date of the inhalerd) Check to see if the patient has already taken any dosese) Assure the inhaler is at room temperature or warmerf) Shake the inhaler vigorously several timesg) Remove oxygen nonrebreather mask from patienth) Have the patient exhale deeplyi) Have the patient put his lips around the opening of theinhalerj) Have the patient depress the handheld inhaler as hebegins to inhale deeplyk) Instruct the patient to hold his breath for as long as hecomfortably can (so medication can be absorbed)l) Replace oxygen on patientm) Allow patient to breathe a few times and repeat seconddose per medical directionModule 4-18
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Educationn) If patient has a spacer device for use with his inhaler, itshould be used. A spacer device is an attachmentbetween inhaler and patient that allows for more effectiveuse of medication.7. Action - beta agonist bronchodilator - dilates bronchiolesreducing airway resistance8. Side effectsa) Increased pulse rateb) Tremorsc) Nervousness9. Re-assessment strategiesa) Gather vital signs and focused reassessmentb) Patient may deteriorate and need positive pressureartificial ventilation10. Infant and child considerationsa) Use of handheld inhalers is very common in childrenb) Retractions are more commonly seen in children thanadults.c) Cyanosis (blue-gray) is a late finding in childrend) Very frequent coughing may be present rather thanwheezing in some childrene) Emergency care with usage of handheld inhalers is thesame if the indications for usage of inhalers are met bythe ill child11. Other MDI medications may be allowed as an assistedrespiratory medication (e.g. Atrovent). Contact medical controlfor advice regarding assisted administration.B. Hand-held and mask nebulizers1. Medication namesa) Albuterol (generic); Proventil, Ventolin (trade names)b) Ipratropium bromide (generic); Atrovent (trade name)2. Indications - meets all of the following criteria:a) Exhibits signs and symptoms of respiratory emergency,b) Specific authorization by medical direction3. Contraindicationsa) Inability of patient to use deviceb) Known allergy – NOTE: patients with allergy to soybeansor peanuts should not be administered Atroventc) Adverse effects of administration – NOTE: patients onbeta-blockers may be advised against beingadministered albuterold) No permission from medical direction4. Medication form - liquid for nebulizing5. Dosage –a) Albuterol - 2.5 mg/3mlb) Atrovent – 0.5mg/3mlModule 4-19
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education6. Route - inhaled7. Administrationa)Contact medical controlb) Report assessment findings, including a thoroughmedical historyc) Rule out allergies and contraindications for used) Report prior interventions and use of inhaler or nebulizere) Request implementation of protocolf) Confirm orders from medical controlg) Explain procedure and solicit patient consenth) Check expiration datei) Confirm right medication, right patient, right routej) Confirm dosagek) Assemble nebulizerl) Add pre-measured medication dosage to nebulizerm) Remove oxygen supply from existing patient adjunct andconnect to medication canister. Provide additionaloxygen to patient via nasal cannula at 4-6 lpmn) Adjust liter flow to 4-6 literso) Instruct patient to place the mouthpiece in their mouthand to inhale slowly and deeply (if utilizing a masknebulizer, place mask appropriately on patient’s face)p) Have patient attempt to hold their breath for 1-2 secondsbefore exhalingq) Continue in this manner until the medication canister isdepletedr) Continue to monitor patient statuss) Resume oxygen therapyt) Document administration data and time, drug name, doseand route of medication(1) Patient’s tolerance of procedure(2) Name of medical control physician authorizingadministration(3) Name of EMT administering medication8. Actiona) Albuterol - beta agonist bronchodilator - dilatesbronchioles, by relaxing surrounding smooth muscles toreduce airway resistance.b) Atrovent – anticholinergic agent - has a timed-releaseeffect and work on the smaller sections of bronchioles toreduce airway resistance9. Side effectsa) Increased pulse rateb) Tremorsc) Nervousness10. Re-assessment strategiesModule 4-20
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Educationa) Gather vital signs and focused reassessmentb) Evaluate patient response to medication administrationc) Patient may deteriorate and need positive pressureartificial ventilation11. Document administration12. Infant and child considerationsa) Use of handheld inhalers is very common in childrenb) Retractions are more commonly seen in children thanadultsc) Cyanosis (blue-gray) is a late finding in childrend) Very frequent coughing may be present rather thanwheezing in some childrene) Emergency care with usage of handheld inhalers is thesame if the indications for usage of inhalers are met bythe ill child.APPLICATIONProcedural (How)1. Show students images of adults, children and infants with breathing distress.2. Show students different types of inhalers.3. Show students how to use a metered dose inhaler.4. Show students how to use a handheld and mask nebulizer.Contextual (When, Where, Why)1. Very few situations are more frightening to a patient than not being able tobreathe. By giving oxygen and helping the patient use his/her inhaler oradministering a nebulizer treatment, the EMT-Basic will be able to relieve asignificant amount of the patient's anxiety. The sooner this is done, thebetter.STUDENT ACTIVITIESAuditory (Hear)1. The student should hear noisy breathing on an audio tape of actual patients.Visual (See)1. The student should see signs and symptoms of respiratory emergenciesusing various audio-visual aids or materials of patients exhibiting the signs.2. The student should see a demonstration of the proper steps in assisting in theusage of handheld inhalers and nebulizer.Kinesthetic (Do)1. The student should practice assessment and management of adult, child andinfant patients having a respiratory illness who have been prescribed ahandheld inhaler by their physician.Module 4-21
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education2. The student should practice the steps in facilitating the use of a handheldinhaler.3. The student should practice role play situations where appropriate andinappropriate assistance of the usage of handheld inhalers occurs.4. The student should practice role play situations where appropriate andinappropriate assistance of the usage of handheld and mask nebulizersoccurs.INSTRUCTOR ACTIVITIES1. Supervise student practice.2. Reinforce student progress in cognitive, affective, and psychomotor domains.3. Redirect students having difficulty with content (complete remediation forms).EVALUATIONWritten:Practical:Develop evaluation instruments, e.g., quizzes, verbal reviews,handouts, to determine if the students have met the cognitiveand affective objectives of this lesson.Evaluate the actions of the EMT-Basic students during role play,practice or other skill stations to determine their compliance withthe cognitive and affective objectives and their mastery of thepsychomotor objectives of this lesson.REMEDIATIONIdentify students or groups of students who are having difficulty with this subjectcontent. Complete remediation sheet from the instructor's course guide.ENRICHMENTWhat is unique in the local area concerning this topic? Complete enrichment sheetsfrom the instructor's course guide and attach with lesson plan.Module 4-22
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationMODULE 4Medical/BehavioralandObstetrics/GynecologyLesson 4-3CardiacEmergenciesModule 4-23
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationOBJECTIVES LEGENDC=Cognitive P=Psychomotor A=Affective1 = Knowledge level2 = Application level3 = Problem-solving levelOBJECTIVESCOGNITIVE OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:4-3.1 Describe the key anatomical structures and function of thecardiovascular system. (C-1)4-3.2 List common causes of cardiac compromise in the adult patient. (C-1)4-3.3 List common causes of cardiac emergencies in the pediatric patient.(C-1)4-3.4 Outline the major signs and symptoms of a patient experiencingcardiac compromise. (C-1)4-3.5 Describe the emergency medical care of the patient experiencing chestpain/discomfort. (C-1)4-3.6 Analyze the indications for automated external defibrillation (AED).(C-3)4-3.7 List the contraindications for automated external defibrillation. (C-1)4-3.8 Define the role of EMT-B in the emergency cardiac care system. (C-1)4-3.9 Explain the impact of age and weight on defibrillation. (C-1)4-3.10 Discuss the position of comfort for patients with various cardiacemergencies. (C-1)4-3.11 Establish the relationship between airway management and the patientwith cardiovascular compromise.(C-3)4-3.12 Predict the relationship between the patient experiencingcardiovascular compromise and <strong>basic</strong> life support. (C-2)4-3.13 Discuss the fundamentals of early defibrillation. (C-1)4-3.14 Discuss the use of the AED for pediatric patients. (C-1)4-3.15 Explain the rationale for early defibrillation. (C-1)4-3.16 Explain that not all chest pain patients result in cardiac arrest and donot need to be attached to an automated external defibrillator. (C-1)4-3.17 Explain the importance of prehospital ACLS intervention if it isavailable. (C-1)4-3.18 Explain the importance of urgent transport to a facility with AdvancedCardiac Life Support if it is not available in the prehospital setting.(C-1)4-3.19 Discuss the various types of automated external defibrillators. (C-1)4-3.20 Differentiate between the fully automated and the semi-automateddefibrillator. (C-3)Module 4-24
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education4-3.21 Discuss the procedures that must be taken into consideration forstandard operations of the various types of automated externaldefibrillators. (C-1)4-3.22 State the reasons for assuring that the patient is pulseless when usingthe automated external defibrillator. (C-1)4-3.23 Differentiate between apnea and agonal respirations as it pertains tothe patient who is pulseless. (C-1)4-3.24 Discuss the circumstances which may result in inappropriate shocks.(C-1)4-3.25 Explain the considerations for interruption of CPR and importance ofminimizing any interruption, when using the automated externaldefibrillator. (C-1)4-3.26 Discuss the advantages and disadvantages of automated externaldefibrillators. (C-1)4-3.27 Summarize the speed of operation of automated external defibrillation.(C-1)4-3.28 Discuss the use of remote defibrillation through adhesive pads. (C-1)4-3.29 Discuss the special considerations for rhythm monitoring. (C-1)4-3.30 List the steps in the operation of the automated external defibrillator.(C-1)4-3.31 Discuss the standard of care that should be used to provide care to apatient with a persistent shockable rhythm and no available ACLS.(C-1)4-3.32 Differentiate between the single rescuer and multi-rescuer care with anautomated external defibrillator. (C-3)4-3.33 Explain the reason for pulses not being checked between shocks withan automated external defibrillator. (C-1)4-3.34 Discuss the importance of coordinating ACLS trained providers withpersonnel using automated external defibrillators. (C-1)4-3.35 Discuss the importance of post-resuscitation care. (C-1)4-3.36 List the components of post-resuscitation care. (C-1)4-3.37 Explain the importance of frequent practice with the automatedexternal defibrillator. (C-1)4-3.38 Discuss the need to complete the Automated Defibrillator: Operator'sShift Checklist. (C-1)4-3.39 Define the function of all controls on an automated externaldefibrillator, and describe event documentation and battery defibrillatormaintenance. (C-1)4-3.40 Discuss the role of the American Heart Association (AHA) in the use ofautomated external defibrillation.(C-1)4-3.41 Explain the role medical direction plays in the use of automatedexternal defibrillation. (C-1)4-3.42 State the reasons why a case review should be completed followingthe use of the automated external defibrillator. (C-1)4-3.43 Discuss the components that should be included in a case review.(C-1)Module 4-25
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education4-3.44 Discuss the goal of quality improvement in automated externaldefibrillation. (C-1)4-3.45 Recognize the need for medical direction of protocols to assist in theemergency medical care of the patient with chest pain. (C-3)4-3.46 List the indications for the use of aspirin. (C-1)4-3.47 State the contraindications and side effects for the use of aspirin. (C-1)4-3.48 List the indications for the use of nitroglycerin. (C-1)4-3.49 State the contraindications and side effects for the use of nitroglycerin.(C-1)AFFECTIVE OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:4-3.50 Defend the reasons for obtaining initial training in automated externaldefibrillation and the importance of continuing education. (A-3)4-3.51 Defend the reason for maintenance of automated externaldefibrillators. (A-3)4-3.52 Explain the rationale for administering nitroglycerin to a patient withchest pain or discomfort. (A-3)PSYCHOMOTOR OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:4-3.53 Demonstrate the assessment and emergency medical care of a patientexperiencing chest pain/discomfort. (P-1,2)4-3.54 Demonstrate the application and operation of the automated externaldefibrillator. (P-1,2)4-3.55 Demonstrate the maintenance of an automated external defibrillator.(P-1,2)4-3.56 Demonstrate the assessment and documentation of patient responseto the automated external defibrillator. (P-1,2)4-3.57 Create a management plan to include evaluation and management foran adult patient in cardiac arrest. (P-3)4-3.58 Create a management plan to include evaluation and management fora pediatric patient in cardiac arrest. (P-3)4-3.59 Demonstrate the skills necessary to complete the AutomatedDefibrillator: Operator's Shift Checklist. (P-1,2)4-3.60 Perform the steps in administering aspirin for chest pain or discomfort.(P-2)4-3.61 Demonstrate the assessment and documentation of patient responseto aspirin. (P-1,2)4-3.62 Perform the steps in facilitating the use of nitroglycerin for chest pain ordiscomfort. (P-2)4-3.63 Demonstrate the assessment and documentation of patient responseto nitroglycerin. (P-1,2)4-3.64 Create a management plan to include evaluation and management foran adult patient experiencing cardiac compromise. (P-3)Module 4-26
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education4-3.65 Practice completing a prehospital care report for patients with cardiacemergencies. (P-2)PREPARATIONMotivation:Over 600,000 patients die each year from cardiovasculardiseases; half of those occur outside the hospital, withsudden death (collapse) being the first sign of cardiacdisease in 50%.Rapid defibrillation, which will be covered in this <strong>module</strong>,is the major determinant of survival in cardiac arrestcaused by ventricular fibrillation.Prerequisites:AV Equipment:EMS Equipment:Primary Instructor:Assistant Instructor:BLS, Preparatory, Airway and Patient Assessment.MATERIALSUtilize various audio-visual materials relating to cardiacemergencies. The continuous design and developmentof new audio-visual materials relating to EMS requirescareful review to determine which best meet the needs ofthe program. Materials should be edited to assuremeeting the objectives of the <strong>curriculum</strong>.CPR manikins, artificial ventilation manikins, automatedexternal defibrillator, aspirin and NTG placebos,defibrillation manikin.PERSONNELOne advanced-level provider with knowledge andexperience in out-of-hospital cardiac resuscitation.The instructor-to-student ratio should be 1:6 forpsychomotor skill practice. Individuals used as assistantinstructors should be knowledgeable in cardiacemergencies.PRESENTATIONDeclarative (What)I. Circulatory System Anatomy and PhysiologyA. Circulatory (Cardiovascular)1. Hearta) Structure/functionModule 4-27
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education(1) Atrium(a) Right - receives blood from the veins of thebody and the heart and pumps oxygen-poorblood to the right ventricle(b) Left - receives blood from the pulmonaryveins (lungs) and pumps oxygen-rich bloodto left ventricle(2) Ventricle(a) Right - pumps blood to the lungs(b) Left - pumps blood to the body(3) Valves prevent backflow of bloodb) Cardiac conductive system(1) Heart is more than a muscle(2) Specialized contractile and conductive tissue inthe heart(3) Electrical impulses2. Arteriesa) Function - carry blood away from the heart to the rest ofthe bodyb) Major Arteries(1) Coronary arteries - vessels that supply the heartwith blood(2) Aorta(a)(b)Major artery originating from the heart andlying in front of the spine in the thoracic andabdominal cavitiesDivides at the level of the navel into the iliacarteries(3) Pulmonary(a) Artery originating at the right ventricle(b) Carries oxygen-poor blood to the lungs(4) Carotid(a) Major artery of the neck(b) Supplies the head with blood(c) Pulsations can be palpated on either side ofthe neck(5) Femoral(a) The major artery of the thigh(b) Supplies the groin and the lower extremitieswith blood(c) Pulsations can be palpated in the groinarea(6) Radial(a) Major artery of the lower hand(b)Pulsations can be palpated at the wristthumbsideModule 4-28
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education(7) Brachial(a) An artery of the upper arm(b) Pulsations can be palpated on the inside ofthe arm between the elbow and theshoulder(c) Used when determining a blood pressure(BP) using a BP cuff and a stethoscope(8) Posterior tibial - pulsations can be palpated on theposterior surface of the medial malleolus(9) Dorsalis pedis(a)(b)An artery in the footPulsations can be palpated on the anteriorsurface of the foot3. Arterioles - the smallest branches of an artery leading to thecapillaries4. Capillariesa) Tiny blood vessels that connect arterioles to venulesb) Found in all parts of the bodyc) Allow for the exchange of nutrients and waste at thecellular level5. Venules - the smallest branches of the veins leading to thecapillaries6. Veinsa) Function - vessels that carry blood back to the heartb) Major veins(1) Pulmonary vein - carries oxygen-rich blood fromthe lungs to the left atrium(2) Venae Cavae(a)(b)(c)SuperiorInferiorCarries oxygen-poor blood back to the rightatrium7. Blood compositiona) Red blood cells(1) Give the blood its color(2) Carry oxygen to organs(3) Carry carbon dioxide away from organsb) White blood cells - part of the body's defense againstinfectionsc) Plasma - fluid that carries the blood cells and nutrientsd) Platelets - essential for the formation of blood clots8. Physiologya) Pulse(1) Left ventricle contracts sending a wave of bloodthrough the arteriesModule 4-29
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationII.III.IV.(2) Can be palpated anywhere an arterysimultaneously passes near the skin surface andover a bone(3) Peripheral(a) Radial(b) Brachial(c) Posterior tibial(d) Dorsalis pedis(4) Central(a) Carotid(b) Femoralb) Blood Pressure(1) Systolic - the pressure exerted against the walls ofthe artery when the left ventricle contracts(2) Diastolic - the pressure exerted against the wallsof the artery when the left ventricle is at restCauses of cardiac compromise in adultsA. Overview1. Arteriosclorosis2. Risk factors-modifiable and unmodifiable3. Congenital defects4. Acute coronary syndromesB. Conditions causing cardiac emergencies1. Angina pectoris – chest pain that occurs when the heart muscledoes not get enough oxygenated blood2. Acute Myocardial Infarction (AMI) – heart attack occurs whenthe heart muscle is without oxygen for an extended period oftime (ischemia), resulting in permanent damage (necrosis)3. Congestive Heart Failure (CHF) – an imbalance in the heartsability to pump properly, resulting in a back up of fluids in eitherthe lungs, extremities, or bothC. Cardiogenic Shock - A state of profound depression of the vitalprocesses of the body, due to cardiac insufficiency, resulting ininadequate circulationCauses of cardiac emergencies in pediatricsA. Airway obstructionB. Respiratory arrestC. TraumaD. Congenital defectsCardiac Compromise - signs and symptoms may include some or all of thefollowing:A. Squeezing, dull pressure, chest pain commonly radiating down thearms or to the jawB. Sudden onset of sweating (this in and of itself is a significant finding)C. Difficulty breathing (dyspnea)D. Rapid and shallow breathingModule 4-30
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationE. Restlessness, anxiety or irritabilityF. Feeling of impending doomG. Abnormal pulse rate (may be irregular or rapid)H. Abnormal blood pressureI. Cool, clammy skinJ. Pale or cyanoticK. Epigastric painL. Nausea and vomitingM. InsomniaN. Atypical presentations occur among certain patients (e.g. females)V. Emergency Medical Care - Initial Patient Assessment ReviewA. Circulation - pulse absent1. Medical patient > one year old - CPR with AED and transport2. Medical patient < one year old - CPR and transport, AED iscontraindicatedB. Responsive patient with a known history - cardiac1. Perform initial assessment2. Perform focused history and physical exam3. Place patient in position of comfort4. Cardiaca) Complains of chest pain or discomfort(1) Apply oxygen if not already done(2) Assess baseline vital signsb) Important questions to ask(1) SAMPLE history(2) O-P-Q-R-S-Tc) Has been prescribed nitroglycerin (NTG) and nitro is withthe patient(1) Blood pressure greater than 100 systolic(a) One dose, repeat in 3-5 minutes if no reliefand authorized by medical direction up to aVI.(b)maximum of three dosesReassess vital signs and chest pain aftereach dose(2) Blood pressure < 100 systolic - continue withfocused assessmentd) Does not have prescribed nitroglycerin (NTG) - continuewith focused assessmente) Transport promptlyRelationship to Basic Life SupportA. Not all chest pain patients become cardiac arrest patientsB. One Rescuer CPR - rarely done by EMT-Basics while on duty, may bedone while partner is preparing equipment, or en route to facilityC. Two Rescuer CPR - learning outcomes of a Professional Rescuer CPRCourse must be enhanced during an EMT-Basic course1. EMT-Basics must also learn:Module 4-31
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationVII.a) Use of automated external defibrillationb) To request available ALS backup to continue the Chainof Survival (as developed by AHA) when appropriatec) Use of bag-valve-mask devices with oxygen attachedd) Use of flow restricted, oxygen-powered ventilatorydevicese) Techniques of lifting and moving patientsf) Suctioning of airwaysg) Use of airway adjunctsh) Use of body substance isolation for infections whennecessaryi) Interviewing bystanders/family to obtain facts related toarrest eventsj) Technique of performing proper compressionsk) Technique involved with delivering appropriateventilationsAutomated External DefibrillationA. Importance of automated external defibrillation to the EMT-Basic1. Fundamentals of early defibrillation - successful resuscitation ofout-of-hospital arrest depends on a series of criticalinterventions which the American Heart Association calls theChain of Survivala) Early accessb) Early CPRc) Early defibrillationd) Early ACLS2. Rationale for early defibrillationa) Many EMS systems have demonstrated increasedsurvival outcomes of cardiac arrest patients experiencingventricular fibrillationb) This increased survival was after early defibrillationprograms were implemented and when all of the links inthe chain of survival were presentB. AED usage for pediatric patients1. AHA guidelines support AED for patients over 1 year of age incardiac arrest2. Pediatric defibrillation pads are preferred3. Adult defibrillation pads may be bused if pediatric pads are notavailable – use anterior/posterior placement of pads if patient’schest is small4. AED is contraindicated in patients < 1 year oldC. Overview of automated external defibrillators1. Types of automated external defibrillatorsa) Fully automated - defibrillator operates without action byEMT-Basic, except to turn on powerModule 4-32
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Educationb) Semi-automated - defibrillator uses a computer voicesynthesizer to advise EMT-Basic as to the steps to takebased upon its analysis of the patient's cardiac rhythm2. Analysis of cardiac rhythmsa) Attach defibrillator to only unresponsive, pulseless, nonbreathingpatients to avoid delivering inappropriateshocksb) Patients in cardiac arrest may present with agonalrespirations – do not delay defibrillationc) Defibrillator computer microprocessor evaluates thepatient's rhythm and confirms the presence of a rhythmfor which a shock is indicatedd) Accuracy of devices in rhythm analysis has been highboth in detecting rhythms needing shocks and rhythmsthat do not need shockse) Analysis is dependent on properly charged defibrillatorbatteries3. Inappropriate delivery of shocksa) Human errorb) Mechanical error4. Pulseless ventricular tachycardiaa) Pulselessness must be determined before attaching AEDto avoid shocking inappropriatelyb) Attach defibrillator to only unresponsive, pulseless, nonbreathingpatients to avoid delivering inappropriateshocksc) Defibrillator advises shocks for ventricular tachycardiawhen the rate exceeds a certain value, for example,above 180 beats per minute5. Interruption of CPRa) No CPR performed at times shocks are deliveredb) No person should be touching patient when rhythm isbeing analyzed and when shocks are deliveredD. Advantages of automated external defibrillation1. Initial training and continuing educationa) Easier to learn than CPR, however, must memorizetreatment sequenceb) EMS delivery system should have:(1) Necessary links in chain of survival(2) Medical direction(3) EMS system with audit and/or quality improvementprogram in place(4) Mandatory continuing education with skillcompetency review for EMS providersc) Continuing competency skill review consistent with Stateand local requirementsModule 4-33
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education2. Remote defibrillation through adhesive padsa) Defibrillation is "hands-off"b) Safer methodc) Better electrode placementd) Has larger pad surface areae) Provokes less anxiety in EMT-BasicE. Use of automated external defibrillators during resuscitation attempts1. Follow current AHA guidelines, State approved sample protocol,State Standards and Procedures and local protocols for AEDuse2. Coordination of ALS personnel or EMT-Paramedics whenEMT-Basics are using automated external defibrillatorsa) EMS system design establishes protocolsb) AED usage does not require ALS on scenec) ALS should be notified of arrest events as soon aspossibled) Considerations for EMT-Basic transporting the patient orwaiting for ALS to arrive on the scene to transport shouldbe in local protocols established by medical direction3. Safety considerations – water or rainF. Post resuscitation care1. After automated external defibrillation protocol is completed,patient may:a) Have pulsesb) Have no pulse with machine indicating "no shockindicated”c) Have no pulse with machine indicating shock2. If pulses returna) Monitor ABCsb) Oxygenc) Reevaluate vital signsd) ACLS intercepte) Rapid transportationf) Keep defibrillator device powered on and pads on patienten route in case patient re-fibrillates, and to createelectronic record of the entire eventg) Perform focused assessment and on-going assessmenten routeG. Defibrillator maintenance1. Regular maintenance for defibrillators is necessary2. Operators Shift Checklist for AEDs must be completed asrequired by local protocol and quality assurance programs3. Defibrillator failure is most frequently related to improper devicemaintenance. Older models may have rechargeable batterieswhich can be a common cause of AED failure. Newer modelshave disposable batteries which must be replaced as needed.Module 4-34
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationVIII.H. Training and sources of information - the American Heart Associationpublishes a variety of guidelines and additional information onautomated external defibrillationI. Maintenance of skills - practice drills to reassess competency must becompleted in compliance with protocolJ. Medical Direction1. Successful completion of AED training in an EMT-Basic coursedoes not permit usage of the device without approval by statelaws/rules and local medical direction authority2. Every event in which an AED is used must be reviewed by themedical director or his designated representative3. Reviews of events using AEDs may be accomplished by:a) Written reportb) Review of voice-ECG tape recorders attached to AED'sc) Solid-state memory <strong>module</strong>s and magnetic taperecordings stored in deviced) Quality improvement - involves both individuals usingAEDs and the EMS system in which the AEDs are usedMedicationsA. Aspirin1. Medication namea) Generic - aspirinb) Trade – Bayer, St. Joseph’s2. Indications - must have all of the following criteria:a) Exhibits signs and symptoms of chest painb) Has specific authorization by medical direction3. Contraindicationsa) Stomach ulcersb) Allergy (e.g. patients with aspirin-induced asthma)c) Patient unable to protect own airwayd) Patient has already met maximum prescribed dose priorto EMT-Basic arrival4. Medication form – chewable tablet5. Dosage – 162-324mg dose (2-4, 81mg), and authorized bymedical direction6. Administrationa) Obtain order from medical direction either on-line oroff-lineb) Perform focused assessment for cardiac patientc) Assess vital signsd) Contact medical control if no standing orderse) Assure right medication, right patient, right route, patientalertf) Check expiration date of aspiring) Question patient on last dose administration, effects, andassures understanding of route of administrationModule 4-35
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Educationh) Ask patient to chew, not swallow whole, tabletsi) Record activity and timej) Perform reassessment and evaluate effect of medication7. Actionsa) Anticoagulant (thrombolytic) “blood thinner”b) Decreases workload of heartc) Mild analgesic8. Side effectsa) Stomach upset9. Reassessment strategiesa) Monitor blood pressureb) Seek medical direction before re-administeringc) Record reassessment findingsB. Nitroglycerin1. Medication namea) Generic - nitroglycerinb) Trade – Nitrostat2. Indications - must have all of the following criteria:a) Patient exhibits signs and symptoms associated withcardiac compromise (e.g. chest pain, pressure ordiscomfort)b) Patient has physician prescribed nitroglycerinc) EMT has authorization by medical direction3. Contraindicationsa) History of hypotensionb) Blood pressure below 100 mmHg systolicc) Head injuryd) Infants and childrene) Patient has already met maximum prescribed dose priorto EMT-Basic arrival4. Medication form - tablet, sub-lingual spray5. Dosage - one dose, repeat in 3-5 minutes if no relief, BP > 100,and authorized by medical direction up to a maximum of threedoses6. Administrationa) Obtain order from medical direction either on-line oroff-lineb) Perform focused assessment for cardiac patientc) Evaluate blood pressure - above 100 mmHg systolicd) Contact medical control if no standing orders existe) Assure right medication, right patient, right route, patientalertf) Check expiration date of nitroglycering) Question patient on last dose administration, effects, andassures understanding of route of administrationModule 4-36
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Educationh) Ask patient to lift tongue and place tablet or spray doseunder tongue (while wearing gloves) or have patientplace tablet or spray under tonguei) Have patient keep mouth closed with tablet under tongue(without swallowing) until dissolved and absorbedj) Recheck blood pressurek) Record activity and timel) Perform reassessment and evaluate patient for effect ofdrug7. Actionsa) Relaxes blood vesselsb) Decreases workload of heart8. Side effectsa) Hypotensionb) Headachec) Pulse rate changesd) Burning or stinging sensation under the tongue9. Reassessment strategiesa) Monitor blood pressureb) Ask patient about effect on pain reliefc) Seek medical direction before re-administeringd) Record reassessmentsAPPLICATIONProcedural (How)1. Demonstrate the assessment and emergency medical care of a patientexperiencing chest pain/discomfort.2. Perform the steps in facilitating the use of aspirin for chest pain using asubstitute candy tablet.3. Perform the steps in facilitating the use of nitroglycerin for chest pain using asubstitute candy tablet and breath spray.4. Demonstrate the assessment and documentation of patient response tonitroglycerin.5. Demonstrate application and operation of the automated external defibrillator.6. Demonstrate maintenance checks of the automated external defibrillator.7. Demonstrate the assessment and documentation of patient response to theautomated external defibrillator.8. Demonstrate assessment, defibrillation, airway management, lifting andmoving a patient, and transportation out of the training laboratory of a manikinin a simulated cardiac arrest situation in which a patient does not respond todefibrillation.Module 4-37
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationContextual (When, Where, Why)1. The EMT-Basic student must prepare to assess and manage patients withcardiac emergencies.2. The training laboratory must provide simulated cardiac situations, both onconscious and unconscious patients, for the student to practice demonstratedskills.3. The student must be able to integrate many single skills into one simulatedcardiac arrest scenario in order to perform safe and effective practice aftercourse completion.STUDENT ACTIVITIESAuditory (Hear)1. The student should hear computer voice simulations made by automatedexternal defibrillators giving instructions on protocols or shocks.2. The student should hear of actual cases where cardiac arrest resuscitationefforts were successful and unsuccessful and the reasons for the outcomes.Visual (See)1. The student should see an instructor team appropriately resuscitate asimulated cardiac arrest patient using an automated external defibrillator.2. The student should see re-enactments of cardiac arrest resuscitation effortsby EMT-Basics using automated external defibrillators.3. The student should see an instructor team appropriately administer a smallcandy or breath spray sublingually to a simulated patient presenting withchest pain.4. The student should see re-enactments of EMS calls where a patient has beenassessed and assisted in the administration of aspirin.5. The student should see re-enactments of EMS calls where a patient has beenassessed and assisted in the administration of nitroglycerin.Kinesthetic (Do)1. The student should practice the assessment and emergency medical care ofa patient experiencing chest pain/discomfort.2. The student should practice the application and operation of the automatedexternal defibrillator on both pediatric and adult patients.3. The student should practice maintenance checks of the automated externaldefibrillator.4. The student should practice performing the steps in facilitating the use ofaspirin for chest pain using a suitable candy tablet.5. The student should practice performing the steps in facilitating the use ofnitroglycerin for chest pain using a suitable candy tablet and breath spray.6. The student should practice the assessment and documentation of patientresponse to the automated external defibrillator.7. The student should practice the assessment and documentation of patientresponse to aspirin and nitroglycerine.Module 4-38
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education8. The student should practice assessment, defibrillation, airway management,lifting and moving a patient, and transportation out of the training laboratory ofa manikin in a simulated cardiac arrest situation in which a patient does notrespond to defibrillation.9. The student should practice completing a prehospital care report for a patientwith a cardiac emergency.INSTRUCTOR ACTIVITIES1. Supervise student practice.2. Reinforce student progress in cognitive, affective, and psychomotor domains.3. Redirect students having difficulty with content (complete remediation forms).EVALUATIONWritten:Practical:Develop evaluation instruments, e.g., quizzes, verbal reviews,handouts, to determine if the students have met the cognitiveand affective objectives of this lesson.Evaluate the actions of the EMT-Basic students during role play,practice or other skill stations to determine their compliance withthe cognitive and affective objectives and their mastery of thepsychomotor objectives of this lesson.REMEDIATIONIdentify students or groups of students who are having difficulty with this subjectcontent. Complete remediation sheet from the instructor's course guide.ENRICHMENTWhat is unique in the local area concerning this topic? Complete enrichment sheetsfrom the instructor's course guide and attach with lesson plan.Module 4-39
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationMODULE 4Medical/BehavioralandObstetrics/GynecologyLesson 4-4DiabeticEmergencies/Altered Mental StatusModule 4-40
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationOBJECTIVES LEGENDC=Cognitive P=Psychomotor A=Affective1 = Knowledge level2 = Application level3 = Problem-solving levelOBJECTIVESCOGNITIVE OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:4-4.1 Identify types of diabetes mellitus. (C-1)4-4.2 Interpret the relationship between insulin and glucose in the productionof energy within the body’s cells. (C-3)4-4.3 List the major signs and symptoms associated with hyperglycemia(diabetic coma). (C-1)4-4.4 List the major signs and symptoms associated with hypoglycemia(insulin shock). (C-1)4-4.5 Differentiate between signs and symptoms associated withhypoglycemia from those of hyperglycemia (C-3)4-4.6 Discuss metabolic shock as it related to diabetic emergencies. (C-1)4-4.7 Discuss the signs and symptoms of a patient taking diabeticmedications, with altered mental status and the implications of adiabetes history. (C-3)4-4.8 State the steps in the emergency medical care of the patient takingdiabetic medicine with an altered mental status and a history ofdiabetes. (C-1)4-4.9 Establish the relationship between airway management and the patientwith altered mental status. (C-3)4-4.10 Establish the normal blood glucose range. (C-1)4-4.11 List the steps in obtaining a blood glucose reading. (C-1)4-4.12 State the generic and trade names, medication forms, dose,administration, action, and contraindications for oral glucose. (C-1)4-4.13 State the generic and trade names, medication forms, dose,administration, action, and contraindications for glucagon. (C-1)4-4.14 Recognize when to administer oral glucose to a hypoglycemic patient.(C-2)4-4.15 Recognize when to administer glucagon to a hypoglycemic patient.(C-2)4-4.16 Explain the need to contact medical control prior to administeringmedications to a diabetic patient with an altered mental status. (C-1)4-4.17 Explain the need for body substance isolation when providingprehopsital care for the diabetic patient. (C-1)4-4.18 Outline the management steps in caring for a hypoglycemic patient.(C-2)Module 4-41
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education4-4.19 List other causes of altered levels of consciousness besides diabeticemergencies. (C-1)4-4.20 Discuss causes, signs and symptoms and management of seizures.(C-1)4-4.21 Discuss causes, signs and symptoms and management of cerebralvascular accidents (CVA). (C-1)4-4.22 Discuss assessment and management of a geriatric patient exhibitingsigns and symptoms of neurological emergencies including dementia.(C-1)AFFECTIVE OBJECTIVES4-4.23 Explain the rationale for obtaining a blood glucose reading in patientswith altered levels of consciousness. (A-3)4-4.24 Explain the rationale for administering oral glucose. (A-3)4-4.25 Explain the rationale for administering glucagon. (A-3)4-4.26 Explain the importance of understanding why some geriatric patientsmay exhibit inappropriate behavior due to an underlying medicalcondition such as stroke, dementia, or delirium. (A-3)PSYCHOMOTOR OBJECTIVES4-4.27 Demonstrate the steps in the emergency medical care, including amanagement plan, assessment and treatment, for the patient takingdiabetic medicine with an altered mental status and a history ofdiabetes. (P-1,2)4-4.28 Demonstrate the steps in obtaining a blood glucose reading. (P-2)4-4.29 Demonstrate the steps in the administration of oral glucose. (P-1,2)4-4.30 Demonstrate the assessment and documentation of patient responseto oral glucose. (P-1,2)4-4.31 Demonstrate the proper technique in reconstituting glucagon andpreparing for its administration. (P-2)4-4.32 Demonstrate the steps in administering an IM injection of glucagon to adiabetic patient. (P-2)4-4.33 Demonstrate the assessment and documentation of patient responseto glucagon. (P-2)4-4.34 Demonstrate the proper disposal of sharps.4-4.35 Demonstrate creating a management plan for a patient exhibiting signsand symptoms of seizure. (P-2)4-4.36 Demonstrate creating a management plan for a patient exhibiting signsand symptoms of stroke. (P-2)4-4.37 Demonstrate creating a management plan for a patient exhibiting signsand symptoms of dementia. (P-2)4-4.38 Demonstrate how to complete a prehospital care report for patientswith diabetic emergencies. (P-2)Module 4-42
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationPREPARATIONMotivation:Prerequisites:AV Equipment:EMS Equipment:Primary Instructor:Assistant Instructor:Neurological emergencies, resulting in an altered level ofconsciousness, include diabetes, seizure, stroke anddementia. Diabetes is a prevalent disease in Americansociety with estimates between 2-5% of the totalpopulation having either diagnosed or undiagnoseddiabetes mellitus. Strokes can causes devastatingchanges in a patient’s quality of life. Current AHAresearch recommends rapid management by prehospitalcaregivers for patient’s exhibiting signs and symptoms ofstroke. Dementia and delirium are debilitating diseasesof the brain that effect geriatric patients.BLS, Preparatory, Airway and Patient Assessment.MATERIALSUtilize various audio-visual materials relating to diabeticemergencies. The continuous design and developmentof new audio-visual materials relating to EMS requirescareful review to determine which best meet the needs ofthe program. Materials should be edited to assuremeeting the objectives of the <strong>curriculum</strong>.Exam gloves, stethoscope (6:1), blood pressure cuff(6:1), penlight, tube of glucose, suitable glucosesubstitute, vials of normal saline, syringes, gloves, sharpscontainers, injection practice devices, 2x2 gauze pads,bandaids, glucometers, test strips, and lancets.PERSONNELOne EMT-Basic instructor knowledgeable in treatment ofdiabetic emergencies.The instructor-to-student ratio should be 1:6 forpsychomotor skill practice. Individuals used as assistantinstructors should be knowledgeable in diabeticemergencies.PRESENTATIONDeclarative (What)I. Diabetes MellitusA. Defined1. Autoimmune disorderModule 4-43
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education2. Caused by a decrease in the amount of insulin being produced3. Result is an imbalance between glucose available in thebloodstream and the cell’s need for the sugar4. Inability to metabolize glucoseB. Types1. Type I - Juvenile onset – insulin dependent2. Type II – adult onset, non-insulin dependent; inadequateamounts of insulin produced; patient may be on oralmedications that stimulate the pancreas to produce more insulin(glyburide, Diabinase, Orinase)C. Insulin and glucose1. Insulin-pancreatic hormone responsible for opening cell gatesthat allow glucose to enter2. Glucose-simple sugar that provides all living cells of the bodywith energy, for metabolismD. Signs and symptoms associated with hyperglycemia (diabetic coma)-condition where there is plenty of glucose available in the bloodstream, but insufficient insulin to allow sugar to pass into the cells1. Gradual onset2. Altered LOC – could be unresponsive or comatose3. Rapid, weak pulse4. Warm, flushed, dehydrated skin5. Thirst6. Deep, rapid respirations (Kussmaul)7. Sweet, fruity odor to breath8. Uncharacteristic behavior9. Abdominal pain, vomitingE. Signs and symptoms associated with hypoglycemia (insulin shock) –low blood sugar. Condition results when there is a low level of glucosein the blood stream. Insulin levels being adequate.1. Sudden onset2. Altered LOC – confusion, irritability, combative3. Seizures and coma possible4. Full, rapid pulse5. BP, normal6. Normal to rapid respirations7. Intense hunger, drooling, and headacheF. Metabolic Shock – caused by an imbalance between production andelimination of acids, causing fluid imbalances and weakened vessel ofthe vascular system. Patients with diabetes are susceptible tometabolic acidosis and shock.G. Normal blood glucose levels1. 70 – 120 mg/dl2. Measurement obtained by use of a glucometerH. Emergency care for a patient experiencing a diabetic emergency1. Assess LOC and ABC’sModule 4-44
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education2. High priority, rapid transport, and consider ALS intercept3. Maintain an open airway and provide oxygen4. If blood glucose is low and patient is conscious, administer oralglucose5. If blood glucose is low and patient is unresponsive, administerglucagonsI. Blood glucose measurement1. Contact medical control, if protocol necessitates2. Explain procedure and obtain consent, when possible3. Select site for obtaining sample4. Cleanse site with alcohol prep-pad and allow to dry5. Turn glucometer on, following digital prompts for directions6. Using sterile lancet, pierce the skin7. Properly dispose of lancet8. “Milk” the finger to obtain a small sample of blood9. Wipe away initial blood droplet with sterile gauze10. Deposit second blood sample on glucometer test strip11. Process the blood sample12. Bandage site as appropriate13. Obtain reading and record data14. Properly dispose of all biohazard materials15. Continue to monitor patient statusJ. Medications1. Oral Glucosea) Medication Name(1) Generic - Glucose, Oral(2) Trade - Glutose, Insta-glucoseb) Indications - patients with altered mental status with aknown history of diabetes controlled by medicationc) Contraindications(1) Unresponsive(2) Unable to swallowd) Medication form - Gel, in toothpaste type tubese) Dosage – 15-25 gf) Administration(1) Obtain order from medical direction either on-lineor off-line(2) Assure signs and symptoms of altered mentalstatus with a known history of diabetes(3) Assure patient is conscious and can swallow andprotect their airway(4) Administer glucose(a)(b)Between cheek and gumPlace on tongue depressor between cheekand gum(5) Perform ongoing assessmentModule 4-45
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Educationg) Actions - increases blood sugarh) Side effects - none when given properly. May beaspirated by the patient without a gag reflex.i) Re-assessment strategies - if patient losesconsciousness or seizes, remove tongue depressor frommouth2. Glucagona) Medication Name(1) Generic - glucagon(2) Trade - Glucagonb) Indications – unresponsive patients with a known historyof diabetes controlled by medicationc) Contraindications(1) allergy to drugd) Medication form – powdered tablet, reconstituted in 1mlof diluente) Dosage – 1mg/mlf) Administration(1) Contact medical control(2) Report assessment findings including signs andsymptoms of hypoglycemia and blood glucosemeasurement(3) Report prior interventions(4) Request implementation of glucagon protocol(5) Confirm orders from medical control(6) Obtain consent and explain procedure, if possible(7) Confirm right patient(8) Reconstitute glucagon(a) Inspect package and both vials insuringright medication, dose and expiration date(b) Remove “flip-off” seals from vials(c) Wipe rubber stoppers with alcohol prep-pad(d) Using sterile 3 ml IM syringe, removeneedle protector from syringe(e) Draw plunger back to 1ml (cc) mark(f)(syringe now contains 1ml of air)Pierce the center of the stopper of the vialcontaining the diluting solution with theneedle of the syringe(g) Turn the vial upside down and inject the 1ml of air from the syringe into the vial (thisprocedure makes it easier to withdraw fluidfrom vial)(h)Keeping the tip of the needle in the diluent,withdraw fluid from vial into the syringeModule 4-46
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education(i)(j)(k)(l)(m)(n)(o)Remove syringe from vial and pierce thecenter of the stopper of the vial, containing1mg powdered glucagon, with the syringeInject all of the diluent into the glucagonsRemove the diluent syringe from the vialand dispose of in sharps containerShake the vial gently until the glucagondissolves and the solution becomes clear.Note: glucagons should be clear and waterlikein consistency. It should be utilizedimmediately after reconstituting.Using a new syringe and appropriatelysized needle, pierce the center of therubber stopper and withdraw slightly moreof the medication than the ordered doseRemove the needle and syringe from thevialWith the needle pointing upward, gently tapthe syringe to move any air bubbles to thetop. Gently advance the syringe to the 1ml mark. (Children less than 20 kg (44 lbs)a dose of 0.5 mg is used). Note: Dosageestablished by medical control must beadministered(9) Perform the IM injection(a) Cleanse the injection site using an alcoholprep-pad(b) Raise the injection site by pinching orstretching the flesh(c) Insert the needle into the selected andcleansed injection site at a 90 degree angle(d) Aspirate slightly by attempting to withdrawthe plunger of the syringe. If no blood isseen to aspirate into the syringe, use lightpressure to depress the plunger and injectall the medication. If blood is seen toaspirate, a second site must be used(e)(f)(g)(h)Depress the plunger to administer theinjectionWithdraw the needle from the injection siteWipe the injection site with an alcohol preppadProperly dispose of the syringe and needleassembly in an appropriate sharpscontainer and place a band-aid over theinjection siteModule 4-47
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationII.III.(10) Continue to monitor patient status(11) Continue oxygen therapy(12) Repeat dosage per medical direction, if requested(13) Document administration data and time(a) Time, name, dose, route of medication(b) Patient’s tolerance of procedure(c) Name of medical control physicianauthorizing administration(d) Name of EMT administering medicationg) Actions – triggers release of stored glucose from liverand skeletal musclesh) Side effects -i) Re-assessment strategies – monitor patient’s LOC andvital signs, document and communicate patient responseto medication administrationCauses of altered mental status, in addition to diabetic emergenciesA. Varied conditions1. Syncopal episodes (fainting), also known as psychogenic shock– a self correcting episode of unresponsiveness, resulting froma sudden, temporary reduction in blood supply to the brain,induced by dilation of the blood vessels. Excessive grief, joy,fear or other emotion can cause this type of shock2. Seizures3. Stroke4. Poisoning5. Infection6. Head trauma7. Hypoxia8. Dementiaa) Brain disorder with memory impairmentb) Multiple causes, including Alzheimer’s diseasec) Gradual decline over several yearsB. Emergency medical care1. Assure patency of airway2. Be prepared to artificially ventilate/suction3. Transport4. Consider trauma as possible cause of altered mental statusSeizuresA. Causes1. Epilepsy2. High fever3. Infections4. Poisonings5. Hypoglycemia or hyperglycemia6. Head trauma7. ShockModule 4-48
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationIV.8. Hypoxia9. Stoke10. Drug or alcohol withdrawal11. Dysrhythmias12. Hypertension13. Pregnancy complications14. Unknown origin (idiopathic)B. Types1. Simple partial seizuresa) Muscle twitching localized to one part of the bodyb) Patient responsive and aware of occurrence2. Complex partial seizuresa) 1-2 minute durationb) Blank stare exhibited by patientc) No response to commands3. Absence (petit mal) seizuresa) Common in pediatricsb) Bland stare, blinking, chewing motion, lack of attention4. Febrile seizurea) Most common in children; rarely life-threateningb) Caused by high feverc) Short in duration5. Generalized Seizure-Tonic-clonic seizurea) Tonic-clonic seizures-phases(1) Aura(2) Tonic phase-muscle contraction for 15-30 sec.(3) Clonic phase-convulsions (muscles contract andrelax; approximately 1-2 minutes)(4) Postictal Phase-last 15-30 minutes; patient difficultto arouse; incontinence may occurb) Status epilepticus-prolonged seizure activity without astate of meaningful consciousness; true emergencyC. Emergency medical care1. Assure patency of airway2. Position patient on side if no possibility of cervical spine trauma3. Have suction ready4. Assist ventilations if needed5. Oxygen therapy6. Transporta) Although brief seizures are not harmful, there may be amore dangerous underlying conditionb) Rule out trauma, head injury can cause seizuresStroke (Cerebral Vascular Accident (CVA))A. Types/causes of stroke1. Ischemic strokea) ThrombosisModule 4-49
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Educationb) Embolism2. Hemorrhagic stroke3. Transient Ischemic Attack (TIA)-miniature stroke, usuallyoccurring days prior to a thrombotic strokeB. Emergency medical care for stroke1. Perform initial assessmenta) Airway managementb) Breathing – supplemental oxygen versus assistedventilationsc) Assess responsiveness carefullyd) Cincinnati Prehospital Stroke Scalee) High priority patientC. Perform focused history and physical exam1. OPQRST evaluated2. SAMPLE History3. Baseline Vitals and repeated vitals4. Obtain blood glucose readingD. Rapid transport1. AHA critical time frame to thrombolytic therapy-3 hoursV. The geriatric patient exhibiting signs and symptoms of neurologicalemergenciesA. Likely causes1. Stroke and Transient Ischemic Attack2. Delirium – sudden, rapid deterioration3. Dementia – gradual progression4. Head and spine traumaB. Assessment1. Determine level of consciousness – AVPU2. Assure airway, breathing and circulation are adequate3. Perform focused history and physical exama) Baseline vital signsb) S.A.M.P.L.E. historyc) History of the present illnessd) Limited physical exam4. More detailed assessment of mental statusa) Ask simple questions to determine if responses arelogical and appropriate5. Examine facial structures for symmetry6. Assess pupils7. Assess cranial nerve function for symmetrya) Close eyesb) Smilec) Protrude tongue8. Assess neurological function in the extremitiesC. Management1. Maintain ABCsModule 4-50
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education2. Protect against further injury or complications3. Oxygen at 15 lpm by nonrebreather4. Treat specific injuries5. Communicate with medical control as needed6. Transport to the closest appropriate hospitalAPPLICATIONProcedural (How)1. Demonstrate the steps in emergency care for the patient with altered mentalstatus and a history of diabetes who is on diabetic medication.2. Demonstrate the steps in obtaining a blood glucose reading.3. Demonstrate the steps in the administration of oral glucose.4. Demonstrate the steps in the administration of glucagon.5. Demonstrate the assessment and documentation of patient response.Contextual (When, Where, Why)1. Diabetes is a common disease affecting a large population. As the populationages, the number of people affected by diabetes will increase.2. Oral glucose, and/or glucagon, given to a patient with an altered mentalstatus and a known history of diabetes can make a difference betweendevelopment of coma (unconsciousness) and ability to maintainconsciousness.3. Evaluating blood glucose levels provides valuable information about thepatient who has an altered level of consciousness.STUDENT ACTIVITIESNone identified for this lesson.Auditory (Hear)Visual (See)1. The student should see audio-visual aids or materials of patients with alteredmental status with a known history of diabetes mellitus in the prehospitalsetting.2. The student should see obtaining a blood glucose reading.3. The student should see the administration of oral glucose (as a simulatedpaste) to a simulated patient.4. The student should see the administration of glucagons (as a simulated liquidfor injection) to a simulated patient.Kinesthetic (Do)1. The student will practice the steps in emergency care for the patient with analtered mental status and a history of diabetes and taking diabetic medication.2. The student will practice the steps in obtaining a blood glucose reading.3. The student will practice the steps in the administration of oral glucose.Module 4-51
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education4. The student will practice documentation of assessment, treatment, andpatient response to oral glucose.5. The student will practice the steps in the administration of glucagon.6. The student will practice documentation of assessment, treatment, andpatient response to glucagon.7. The student will practice completing a prehospital care report for patients withdiabetic emergencies.INSTRUCTOR ACTIVITIES1. Supervise student practice.2. Reinforce student progress in cognitive, affective, and psychomotor domains.3. Redirect students having difficulty with content (complete remediation forms).EVALUATIONWritten:Practical:Develop evaluation instruments, e.g., quizzes, verbal reviews,handouts, to determine if the students have met the cognitiveand affective objectives of this lesson.Evaluate the actions of the EMT-Basic students during role play,practice or other skill stations to determine their compliance withthe cognitive and affective objectives and their mastery of thepsychomotor objectives of this lesson.REMEDIATIONIdentify students or groups of students who are having difficulty with this subjectcontent. Complete remediation sheet from the instructor's course guide.ENRICHMENTWhat is unique in the local area concerning this topic? Complete enrichment sheetsfrom the instructor's course guide and attach with lesson plan.Module 4-52
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationMODULE 4Medical/BehavioralandObstetrics/GynecologyLesson 4-5Severe Allergic ReactionsModule 4-53
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationOBJECTIVES LEGENDC=Cognitive P=Psychomotor A=Affective1 = Knowledge level2 = Application level3 = Problem-solving levelOBJECTIVESCOGNITIVE OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:4-5.1 Define a severe allergic reaction (anaphylaxis). (C-1)4-5.2 Describe the pathophysiology involved with hypersensitivity to thepresence of an allergen. (C-1)4-5.3 List possible causes of anaphylaxis. (C-1)4-5.4 Recognize the patient experiencing an allergic reaction.(C-1)4-5.5 Describe the emergency medical care of the patient with an allergicreaction. (C-1)4-5.6 Establish the relationship between the patient with an allergic reactionand airway management. (C-3)4-5.7 Describe the mechanisms of allergic response and the implications forairway management. (C-1)4-5.8 State the generic and trade names, medication forms, dose,administration, action, and contraindications for the epinephrineauto-injector. (C-1)4-5.9 Evaluate the need for medical direction in the emergency medical careof the patient with an allergic reaction. (C-3)4-5.10 Differentiate between the general category of those patients having anallergic reaction and those patients having an allergic reaction andrequiring immediate medical care, including immediate use ofepinephrine auto-injector. (C-3)AFFECTIVE OBJECTIVES4-5.11 Explain the rationale for administering epinephrine using an autoinjector.(A-3)PSYCHOMOTOR OBJECTIVES4-5.12 Demonstrate the emergency medical care of the patient experiencingan allergic reaction. (P-1,2)4-5.13 Demonstrate the use of epinephrine auto-injector. (P-1,2)4-5.14 Demonstrate the assessment and documentation of patient responseto an epinephrine injection. (P-1,2)4-5.15 Demonstrate proper disposal of equipment. (P-1,2)Module 4-54
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education4-5.16 Create a management plan to include evaluation and treatment of anadult patient experiencing an anaphylactic reaction. (P-3)4.5-17 Create a management plan to include evaluation and treatment of apediatric patient experiencing an anaphylactic reaction. (P-3)4-5.18 Demonstrate completing a prehospital care report for patients withallergic emergencies. (P-2)PREPARATIONMotivation:Prerequisites:AV Equipment:EMS Equipment:Primary Instructor:Assistant Instructor:The ability to recognize and manage a severe allergicreaction (anaphylaxis) is possibly the only thing standingbetween a patient and imminent death.BLS, Preparatory, Airway and Patient Assessment.MATERIALSUtilize various audio-visual materials relating to allergicemergencies. The continuous design and developmentof new audio-visual materials relating to EMS requirescareful review to determine which best meet the needs ofthe program. Materials should be edited to assuremeeting the objectives of the <strong>curriculum</strong>.Epinephrine auto-injector, epinephrine auto-injectortrainer, alcohol prep pads, and sharps container.PERSONNELOne EMT-Basic instructor knowledgeable in thephysiology of severe allergic reactions and the use ofepinephrine auto-injectors.The instructor-to-student ratio should be 1:6 forpsychomotor skill practice. Individuals used as assistantinstructors should be knowledgeable in allergicemergencies.PRESENTATIONDeclarative (What)I. Allergic ReactionsA. Definition - an exaggerated immune response to a foreign substance(allergen), resulting in a systemic release of histaminesB. Possible causes1. Insect bites/stings - bees, wasps, etc.Module 4-55
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education2. Food - nuts, crustaceans, peanuts, etc.3. Plants4. Medications5. Latex6. OthersC. Assessment findings may include:1. Skina) Patient may state he has a warm tingling feeling in theface, mouth, chest, feet and handsb) Itchingc) Hivesd) Red skin (flushing)e) Swelling to face, neck, hands, feet and/or tongue2. Respiratory systema) Patient may state he feels a tightness in his throat/chestb) Coughc) Rapid breathingd) Labored breathinge) Noisy breathingf) Hoarseness (losing the voice)g) Stridorh) Wheezing (audible without stethoscope)3. Cardiaca) Increased heart rateb) Decreased blood pressure4. Generalized findingsa) Itchy, watery eyesb) Headachec) Sense of impending doomd) Runny nose5. Decreasing mental status6. Assessment findings that reveal shock or respiratory distressindicate the presence of a severe allergic reactionD. Emergency medical care of allergic reactions1. Patient has come in contact with substance that caused pastallergic reaction and complains of respiratory distress or exhibitssigns and symptoms of shock.a) Perform initial assessmentb) Perform focused history and physical exam(1) History of allergies(2) What was patient exposed to(3) How were they exposed?(4) What effects(5) Progression(6) Interventionsc) Assess baseline vital signs and SAMPLE historyModule 4-56
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationII.III.d) Administer oxygen if not already done in the initialassessmente) Determine if patient has prescribed preloadedepinephrine available. Facilitate administration ofpreloaded epinephrine.f) Contact medical directiong) Record and reassess in two minutesh) Record reassessment findingsi) If patient does not have epinephrine auto-injectoravailable - transport immediately2. Patient has contact with substance that causes allergic reactionwithout signs of respiratory distress or shocka) Continue with focused assessmentb) Patient not wheezing or without signs of respiratorycompromise or hypotension should not receiveepinephrineRelationship to Airway ManagementA. These patients may initially present with airway/respiratorycompromise or airway/respiratory compromise may develop as theallergic reaction progressesB. The airway should be managed according to the principles identified inthe airway management lesson presented earlierMedicationsA. Epinephrine auto-injector1. Medication namea) Generic - Epinephrineb) Trade - Adrenalin2. Indications - must meet the following three criteria:a) Emergency medical care for the treatment of the patientexhibiting the assessment findings of an allergic reactionb) Medication is prescribed for this patient by a physicianc) Medical direction authorizes use for this patient3. Contraindications - no contraindications when used in a lifethreateningsituation4. Medication form - liquid administered via an automaticallyinjectable needle and syringe system5. Dosagea) Adult - one adult auto-injector (0.3 mg)b) Infant and child - one infant/child auto-injector (0.15 mg,up to #60)6. Administrationa) Obtain order from medical direction either on-line oroff-lineb) Obtain patient's prescribed auto-injector. Ensure:(1) Prescription is written for the patient experiencingallergic reactionsModule 4-57
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education(2) Medication is not discolored (if able to see)c) Remove safety cap from the auto-injectord) Place tip of auto-injector against the patient's thigh(1) Lateral portion of the thigh.(2) Midway between the waist and the kneee) Push the injector firmly against the thigh until the injectoractivatesf) Hold the injector in place until the medication is injectedg) Record activity and timeh) Dispose of injector in sharps container7. Actionsa) Dilates the bronchiolesb) Constricts blood vessels8. Side effectsa) Increases heart rateb) Pallorc) Dizzinessd) Chest paine) Headachef) Nauseag) Vomitingh) Excitability, anxiousness9. Re-assessment strategiesa) Transportb) Continue focused assessment of airway, breathing andcirculatory status(1) Patient condition continues to worsen(a) Decreasing mental status(b) Increasing breathing difficulty(c) Decreasing blood pressure(d) Obtain medical direction(i) Additional dose of epinephrine(ii) Treat for shock(iii) Prepare to initiate Basic Cardiac Lifesupport measuresCPRAED(2) Patient condition improves. Provide supportivecare(a) Oxygen(b) Treat for shockModule 4-58
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationAPPLICATIONProcedural (How)The instructor will demonstrate the following steps using an epinephrine auto-injectortrainer and appropriate synthetic skin mannequin:1. Obtain medical direction.2. Obtain patient's prescribed auto injector. Ensure:a. Prescription is written for the patient experiencing allergic reactions.b. Medication is not discolored, if visible.3. Remove safety cap from the auto-injector.4. Place tip of auto-injector against the patient's thigh.a. Lateral portion of the thigh.b. Midway between the waist and the knee.5. Push the injector firmly against the thigh until the injector activates.6. Hold the injector in place until the medication is injected.7. Dispose of injector in biohazard container.Contextual (When, Where, Why)1. The EMT-Basic will now be able to assist patients with the administration ofepinephrine auto-injectors. This will make a significant difference in thosepatients exposed to an allergic agent.2. The administration of the epinephrine should be performed as soon aspossible following appropriate identification of the allergic reaction.STUDENT ACTIVITIESAuditory (Hear)1. The student should hear the assessment findings differentiating minor andsevere allergic reactions.2. The student should hear the steps required to appropriately administerepinephrine using an auto-injector.Visual (See)1. The student should see various audio-visual aids or materials showing theassessment findings relative to minor allergic reactions.2. The student should see an actual epinephrine auto-injector.3. The student should see the instructor demonstrate the appropriate steps inusing an auto-injector.4. The student should see various audio-visual aids or materials showing theassessment findings of major allergic reactions and the appropriate use of theauto-injector.Kinesthetic (Do)1. The student should practice the correct way to use an epinephrineauto-injector.2. The student should practice role play treatment of a patient experiencing anallergic reaction.Module 4-59
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education3. The student should practice re-assessment and documentation relative to theuse of a epinephrine auto-injector.INSTRUCTOR ACTIVITIES1. Supervise student practice.2. Reinforce student progress in cognitive, affective, and psychomotor domains.3. Redirect students having difficulty with content (complete remediation forms).EVALUATIONWritten:Practical:Develop evaluation instruments, e.g., quizzes, verbal reviews,handouts, to determine if the students have met the cognitiveand affective objectives of this lesson.Evaluate the actions of the EMT-Basic students during role play,practice or other skill stations to determine their compliance withthe cognitive and affective objectives and their mastery of thepsychomotor objectives of this lesson.REMEDIATIONIdentify students or groups of students who are having difficulty with this subjectcontent. Complete remediation sheet from the instructor's course guide.ENRICHMENTWhat is unique in the local area concerning this topic? Complete enrichment sheetsfrom the instructor's course guide and attach with lesson plan.Module 4-60
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationMODULE 4Medical/BehavioralandObstetrics/GynecologyLesson 4-6Poisoning/OverdoseModule 4-61
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationOBJECTIVES LEGENDC=Cognitive P=Psychomotor A=Affective1 = Knowledge level2 = Application level3 = Problem-solving levelOBJECTIVESCOGNITIVE OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:4-6.1 List various ways that poisons enter the body. (C-1)4-6.2 List signs/symptoms associated with poisoning. (C-1)4-6.3 Discuss the emergency medical care for the patient with possibleoverdose. (C-1)4-6.4 Describe the steps in the emergency medical care for the patient withsuspected poisoning. (C-1)4-6.5 Establish the relationship between the patient suffering from poisoningor overdose and airway management. (C-3)4-6.6 State the generic and trade names, indications, contraindications,medication form, dose, administration, actions, side effects andre-assessment strategies for activated charcoal.(C-1)4-6.7 Recognize the need for medical direction in caring for the patient withpoisoning or overdose. (C-3)AFFECTIVE OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:4-6.8 Explain the rationale for administering activated charcoal. (A-3)4-6.9 Explain the rationale for contacting medical direction early in theprehospital management of the poisoning or overdose patient. (A-3)PSYCHOMOTOR OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:4-6.10 Demonstrate the steps in the emergency medical care for the patientwith possible overdose. (P-1,2)4-6.11 Demonstrate the steps in the emergency medical care for the patientwith suspected poisoning.(P-1,2)4-6.12 Perform the necessary steps required to provide a patient withactivated charcoal. (P-2)4-6.13 Demonstrate the assessment and documentation of patient response.(P-1,2)4-6.14 Demonstrate proper disposal of the equipment for the administration ofactivated charcoal. (P-1,2)Module 4-62
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education4-6.15 Demonstrate completing a prehospital care report for patients with apoisoning/overdose emergency. (P-1,2)PREPARATIONMotivation:Prerequisites:AV Equipment:EMS Equipment:Primary Instructor:Assistant Instructor:Thousands of children are poisoned every year as theyexplore their environments. Many adults also overdoseon medication, either accidentally or deliberately. Withearly prehospital management, the vast majority of thesepatients have better outcomes.BLS, Preparatory, Airway and Patient Assessment.MATERIALSUtilize various audio-visual materials relating topoisoning/overdose emergencies. The continuousdesign and development of new audio-visual materialsrelating to EMS requires careful review to determinewhich best meet the needs of the program. Materialsshould be edited to assure meeting the objectives of the<strong>curriculum</strong>.Activated charcoal, suction equipment.PERSONNELOne EMT-Basic instructor knowledgeable in this area.None required.PRESENTATIONDeclarative (What)I. Emergency Medical Care of Poisoning/OverdoseA. Important questions to consider asking patient1. What substance?2. When did you ingest/become exposed?3. If an ingestion, how much did you ingest?4. Over what time period?5. Interventions?6. How much do you weigh?B. Ingested1. Signs and symptomsa) History of ingestionb) NauseaModule 4-63
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Educationc) Vomitingd) Diarrheae) Altered mental statusf) Abdominal paing) Chemical burns around the mouthh) Different breath odors2. Emergency medical carea) Remove pills, tablets or fragments with gloves frompatient's mouth, as needed, without injuring oneselfb) Consult medical direction and/or poison control center -activated charcoalc) Bring all containers, bottles, labels, etc. of poison agentsto receiving facilityC. Inhaled1. Signs and symptomsa) History of inhalation of toxic substanceb) Difficulty breathingc) Chest paind) Coughe) Hoarsenessf) Dizzinessg) Headacheh) Confusioni) Seizuresj) Altered mental status2. Emergency medical carea) Have trained rescuers remove patient from poisonousenvironment. Be aware that fumes and gases canremain on clothing or skin.b) Give oxygen, if not already done in the initial assessmentc) Bring all containers, bottles, labels, etc. of poison agentsto receiving facilityD. Toxic injection1. Signs and symptomsa) Weaknessb) Dizzinessc) Chillsd) Fevere) Nauseaf) Vomiting2. Emergency medical carea) Airway and oxygenb) Be alert for vomitingc) Bring all containers, bottles, labels, etc. of poison agentsto receiving facilityE. AbsorbedModule 4-64
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationII.III.1. Signs and symptomsa) History of exposureb) Liquid or powder on patient's skinc) Burnsd) Itchinge) Irritationf) Redness2. Emergency medical carea) Skin - remove contaminated clothing while protectingoneself from contamination(1) Powder - brush powder off patient, then continueas for other absorbed poisons(2) Liquid - irrigate with clean water for at least 20minutes (and continue en route to facility ifpossible)b) Eye - irrigate with clean water away from affected eye forat least 20 minutes and continue en route to facility ifpossibleRelationship to Airway ManagementA. Use information and skills learned in airway section of course tomanage airway difficultiesB. A patient's condition may deteriorate, so continue to assess patient forairway difficulties and manage as learned previouslyMedications – refer to local protocols for prehospital useA. Activated charcoal1. Medication namea) Generic - Activated charcoalb) Trade(1) SuperChar(2) InstaChar(3) Actidose(4) LiquiChar2. Indications - poisoning by mouth3. Contraindicationsa) Altered mental statusb) Ingestion of acids or alkalisc) Unable to swallow4. Medication forma) Pre-mixed in water, available in containers of 12.5, 25and 50 gramsb) Powder - should be avoided in field5. Dosagea) Adults and children: 1 gram activated charcoal/kg of bodyweightb) Usual adult dose: 25 - 50 gramsc) Usual infant/child dose: 12.5 - 25 gramsModule 4-65
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education6. Administrationa) Obtain order from medical direction either on-line or offlineb) Container must be shaken thoroughlyc) Since medication looks like mud, patient may need to bepersuaded to drink itd) A covered container and a straw may improve patientcompliance since the patient cannot see the medicationthis waye) If patient takes a long time to drink the medication, thecharcoal will settle and will need to be shaken or stirredagainf) Record activity, patient response to administration,complications and time7. Actionsa) Binds to certain poisons and prevents them from beingabsorbed into the bodyb) Not all brands of activated charcoal are the same; somebind much more poison than others, so consult medicaldirection about the brand to use8. Side effectsa) Black stoolsb) Some patients, particularly those who have ingestedpoisons that cause nausea, may vomitc) If the patient vomits, the dose should be repeated permedical direction9. Re-assessment strategies - the EMT-Basic should be preparedfor the patient to vomit or further deteriorateAPPLICATIONProcedural (How)1. Show the student examples of poisoning by ingestion.2. Show the student examples of poisoning by inhalation.3. Show the student examples of poisoning by injection.4. Show the student examples of poisoning by absorption.5. Show the student activated charcoal.6. Show the student how to administer activated charcoal.7. Show the student how to care for a patient with suspected poisoning oroverdose.Contextual (When, Where, Why)1. The EMT-Basic can prevent injury and illness from ingested poisoning byadministering activated charcoal. The sooner this happens, the more effect itwill have.Module 4-66
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education2. The EMT-Basic can also prevent loss of life by ensuring the patient who hasoverdosed has his airway protected.STUDENT ACTIVITIESNone identified for this lesson.Auditory (Hear)Visual (See)1. The student should see audio-visuals aids or materials of examples ofpoisoning by ingestion.2. The student should see audio-visuals aids or materials of examples ofpoisoning by inhalation.3. The student should see audio-visuals aids or materials of examples ofpoisoning by injection.4. The student should see audio-visuals aids or materials of examples ofpoisoning by absorption.5. The student should see activated charcoal.6. The student should see a demonstration of how to administer activatedcharcoal.7. The student should see a demonstration of how to care for a patient withsuspected poisoning or overdose.Kinesthetic (Do)1. The student should practice caring for a patient with suspected poisoning oroverdose.2. The student should practice the assessment and documentation of patientresponse to activated charcoal.3. The student should practice completing a prehospital care report for patientswith poisoning/overdose emergencies.INSTRUCTOR ACTIVITIES1. Supervise student practice.2. Reinforce student progress in cognitive, affective, and psychomotor domains.3. Redirect students having difficulty with content (complete remediation forms).EVALUATIONWritten:Practical:Develop evaluation instruments, e.g., quizzes, verbal reviews,handouts, to determine if the students have met the cognitiveand affective objectives of this lesson.Evaluate the actions of the EMT-Basic students during role play,practice or other skill stations to determine their compliance withthe cognitive and affective objectives and their mastery of thepsychomotor objectives of this lesson.Module 4-67
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationREMEDIATIONIdentify students or groups of students who are having difficulty with this subjectcontent. Complete remediation sheet from the instructor's course guide.ENRICHMENTWhat is unique in the local area concerning this topic? Complete enrichment sheetsfrom the instructor's course guide and attach with lesson plan. If there are localresources, for example, Poison Control Centers, utilize them.Module 4-68
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationMODULE 4Medical/BehavioralandObstetrics/GynecologyLesson 4-7EnvironmentalEmergenciesModule 4-69
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationOBJECTIVES LEGENDC=Cognitive P=Psychomotor A=Affective1 = Knowledge level2 = Application level3 = Problem-solving levelOBJECTIVESCOGNITIVE OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:4-7.1 Describe the various ways that the body loses heat.(C-1)4-7.2 List the signs and symptoms of exposure to cold.(C-1)4-7.3 Explain the steps in providing emergency medical care to a patientexposed to cold.(C-1)4-7.4 List the signs and symptoms of exposure to heat.(C-1)4-7.5 Explain the steps in providing emergency care to a patient exposed toheat.(C-1)4-7.6 Recognize the signs and symptoms of water-related emergencies.(C-1)4-7.7 Describe the complications of near drowning.(C-1)4-7.8 Discuss the emergency medical care of bites and stings.(C-1)No affective objectives identified.AFFECTIVE OBJECTIVESPSYCHOMOTOR OBJECTIVES4-7.9 Demonstrate the assessment and emergency medical care of a patientwith exposure to cold.(P-1,2)4-7.10 Demonstrate the assessment and emergency medical care of a patientwith exposure to heat.(P-1,2)4-7.11 Demonstrate the assessment and emergency medical care of a neardrowning patient.(P-1,2)4-7.12 Demonstrate completing a prehospital care report for patients withenvironmental emergencies.(P-2)PREPARATIONMotivation:Environmental emergencies include exposure to bothheat and cold. The key to effective management isrecognizing the signs and symptoms and providingprompt emergency medical care.Module 4-70
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationCold emergencies are found in varied groups ofindividuals, including hunters, sailors, skiers, climbers,swimmers, military personnel, and all others in thewilderness, rural, and urban setting. The greatestnumber of hypothermia cases are reported in the urbansetting, many involving the elderly patient.Likewise, heat emergencies are also prevalent in a largenumber of groups of individuals in many differentsettings. Heat emergencies range from very minoreffects to life threatening conditions. Heat emergenciesmay occur during any season of the year.Because of the increased popularity of water sports,there is a subsequent increase in the incidence of aquaticemergencies. Aquatic emergencies most frequentlymanaged by the EMT-Basic will involve near drowning.The EMT-Basic must be prepared to assess and managethe patient experiencing these types of emergencies.Prerequisites:AV Equipment:EMS Equipment:Primary Instructor:Assistant Instructor:BLS, Preparatory, Airway and Patient Assessment.MATERIALSUtilize various audio-visual materials relating toenvironmental emergencies. The continuous design anddevelopment of new audio-visual materials relating toEMS requires careful review to determine which bestmeet the needs of the program. Materials should beedited to assure meeting the objectives of the <strong>curriculum</strong>.Exam gloves, stethoscopes, blood pressure cuffs,penlight.PERSONNELOne EMT-Basic instructor knowledgeable in heat, coldand aquatic emergencies.None required.PRESENTATIONDeclarative (What)I. Temperature RegulationA. Based on heat loss versus heat gainedModule 4-71
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationII.III.1. Heat loss exceeds heat gained - hypothermia (low bodytemperature)a) Heat loss occurs by:(1) Radiation(2) Convection(3) Conduction(4) Evaporation(5) Breathingb) EMT-Basic must be aware of methods of heat loss whentreating patients with hypothermia to prevent further heatloss2. Heat gained exceeds heat loss - hyperthermia (high body coretemperature)Important Questions to Ask Patients Exposed to the EnvironmentA. SourceB. EnvironmentC. Loss of consciousnessD. Effects1. General2. LocalExposure to ColdA. Generalized cold emergency - generalized hypothermia1. Predisposing factorsa) Cold environment(1) Immersion(2) Non-immersionb) Age(1) Very old(a) Low income may prohibit adequate heat inhome(b) Elderly have less muscle mass andsubcutaneous tissue(c) Elderly may have chronic illnesses andfailing body systems(d) Many have poor diets(e) Many medications may contribute tohypothermia(f) Decreased activity(2) Very young(a) Infants and young children are small withlarge surface area(b) Small muscle mass, so shivering is poor inchildren and not at all in infants(c)(d)Less body fatYounger children need help to protect self.Cannot put on or take off clothes.Module 4-72
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Educationc) Medical conditions(1) Shock(2) Head injury(3) Burns(4) Generalized infection(5) Injuries to the spinal cord(6) Diabetes and hypoglycemia(7) Altered mental status from any caused) Drugs/poisons2. Signs and symptoms of generalized hypothermiaa) Environmental conditions of cold exposure(1) Obvious exposure(2) Subtle exposure(a) Ethanol ingestion(b) Underlying illness(c) Overdose/poisoning(d) Major trauma(e)(f)Outdoor resuscitationAmbient temperature decreased (e.g. homeof elderly patient)b) Cool/cold skin temperature - the EMT-Basic shouldplace the back of his hand between the clothing and thepatient's abdomen to assess the general temperature ofthe patient. The patient experiencing a generalized coldemergency will present with cool abdominal skintemperature.c) Decreasing mental status or motor function - correlateswith the degree of hypothermia(1) Poor coordination(2) Memory disturbances(3) Reduced or loss of sensation - to touch(4) Mood changes(5) Less communicative(6) Dizziness(7) Speech difficultyd) Stiff or rigid posturee) Muscle rigidityf) Shivering may be present or absentg) Breathing variations(1) Early - rapid breathing(2) Late - shallow, slow or even absent breathingh) Slowly responding pupilsi) Pulse(1) Early - rapid(2) Late - slow and barely palpable and/or irregular, orcompletely absentModule 4-73
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Educationj) Low to absent blood pressurek) Poor judgement - patient may actually remove clothingl) Complaints of joint/muscle stiffnessm) Skin(1) Red - early(2) Pale(3) Cyanotic - blue-gray(4) Stiff/hard3. Emergency medical care for generalized hypothermiaa) Remove the patient from the environment - protect thepatient from further heat lossb) Remove wet clothing and cover with blanketc) Handle the patient extremely gently. Avoid roughhandling.d) Do not allow the patient to walk or exert himselfe) Administer oxygen if not already done as part of the initialassessment - oxygen administered should be warmedand humidified, if possiblef) Assess pulses for 30-45 seconds before starting CPRg) If the patient is alert and responding appropriately,actively rewarm(1) Warm blankets(2) Heat packs or hot water bottles to the groin,axillary and cervical regions(3) Turn the heat up high in the patient compartmentof the ambulanceh) If the patient is unresponsive or not respondingappropriately, rewarm passively:(1) Warm blankets(2) Turn the heat up high in the patient compartmentof the ambulancei) Do not allow the patient to eat or drink stimulantsj) Do not massage extremitiesB. Local cold injuries - localized to specific area of body1. Predisposing factors2. Tend to occur on the extremities and exposed ears, nose, andface3. Signs and symptoms of local cold injuriesa) Local injury with clear demarcationb) Early or superficial injury(1) Blanching of the skin - palpation of the skin inwhich normal color does not return(2) Loss of feeling and sensation in the injured area(3) Skin remains soft(4) If rewarmed, tingling sensationc) Late or deep injuryModule 4-74
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationIV.(1) White, waxy skin(2) Firm to frozen feeling upon palpation(3) Swelling may be present(4) Blisters may be present(5) If thawed or partially thawed, the skin may appearflushed with areas of purple and blanching ormottled and cyanotic4. Emergency medical care for local cold injuriesa) Remove the patient from the environmentb) Protect the cold injured extremity from further injuryc) Administer oxygen if not already done as part of the initialassessmentd) Remove wet or restrictive clothinge) If early or superficial injury(1) Splint extremity(2) Cover the extremity(3) Do not rub or massage(4) Do not re-expose to the coldf) If late or deep cold injury(1) Remove jewelry(2) Cover with dry clothing or dressings(3) Do not:(a) Break blisters(b) Rub or massage area(c) Apply heat(d)(e)RewarmAllow the patient to walk on the affectedextremityg) When an extremely long or delayed transport isinevitable, then active rapid rewarming should be done(1) Immerse the affected part in warm water bath. Donot let limb touch the sides or bottom of thecontainer.(2) Monitor the water to ensure it does not cool fromthe frozen part(3) Continuously stir water(4) Continue until the part is soft and color andsensation return(5) Dress the area with dry sterile dressings. If handor foot, place dry sterile dressings between fingersor toes.(6) Protect against refreezing the warmed part(7) Expect the patient to complain of severe painExposure to HeatA. Predisposing factors1. ClimateModule 4-75
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Educationa) High ambient temperature reduces the body's ability tolose heat by radiationb) High relative humidity reduces the body's ability to loseheat through evaporation2. Exercise and activitya) Can lose more than 1 liter of sweat per hourb) Loss of electrolytes (sodium, chloride and fluid throughsweat)3. Agea) Elderly(1) Poor thermoregulation(2) Medications(3) Lack mobility - can not escape hot environmentb) Newborn/infants(1) Poor thermoregulation(2) Cannot remove own clothing4. Pre-existing illness and/or conditionsa) Heart diseaseb) Dehydrationc) Obesityd) Fevere) Fatiguef) Diabetes5. Drugs/medicationsB. Signs and symptoms1. Muscle cramps2. Weakness or exhaustion3. Dizziness or faintness4. Skina) Moist, pale, normal to cool temperatureb) Hot, dry or moist - dire emergency5. Rapid heart rate6. Altered mental status to unresponsiveC. Emergency medical care of heat emergencies - patient with moist,pale, normal to cool temperature skin1. Remove the patient from the hot environment and place in acool environment (back of air conditioned ambulance)2. Administer oxygen if not already done during the initialassessment3. Loosen or remove clothing4. Cool patient by fanning5. Put in supine position with legs elevated6. If patient is responsive and is not nauseated, have the patientdrink water7. If the patient is unresponsive or is vomiting, transport to thehospital with patient on his left sideModule 4-76
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationD. Emergency medical care of heat emergencies - patient with hot, dry ormoist skin1. Remove the patient from the hot environment and place in acool environment (back of air conditioned ambulance with airconditioner running on high)2. Remove clothing3. Administer oxygen if not already done during the initialassessment4. Apply cool packs to neck, groin and armpits5. Keep the skin wet by applying water by sponge or wet towels6. Fan aggressively7. Transport immediatelyV. Water-Related EmergenciesA. Near drowning/drowning1. Ensure the safety of the rescue personnel2. Suspect possible spine injury if diving accident is involved orunknown3. Suspect possible hypothermic conditions if immersion in coldwater or an open body of water4. Consider length of time in cold water drowning. Any pulseless,non-breathing patient who has been submerged in cold watershould be resuscitated. Check pulses for a full 60 seconds.5. Emergency medical care:a) In-line immobilization and removal from water withbackboard if spine injury is suspected and patient isresponsiveb) If there is no suspected spine injury, place patient on leftside to allow water, vomitus and secretions to drain fromupper airwayc) Suction as neededd) Administer oxygen if not already done during the initialassessmente) If gastric distention interferes with artificial ventilation, thepatient should be placed on his left side. With suctionimmediately available, the EMT-Basic should place hishand over the epigastric area of the abdomen and applyfirm pressure to relieve the distention. This procedureshould only be done if the gastric distention interfereswith the ability of the EMT-Basic to artificially ventilate thepatient effectively.f) For warm water drownings requiring resuscitation - seecardiac <strong>module</strong>B. Diving Accidents1. The Diver Alert Network (DAN) is a resource for care of divingaccident patients2. Decompression sicknessModule 4-77
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationVI.a) Caused by ascending too quickly or flying within twelvehours of divingb) Most often occurs within 3 hours of incident but mayoccur 1-48 hoursc) Signs and symptoms(1) personality changes(2) fatigue(3) muscle and joint pain (the “bends”)(4) skin blotching, mottling or rash(5) numbness and paralysis(6) choking(7) labored breathing(8) intoxicated appearance (e.g. staggering gait)(9) chest pains(10) collapse and unconsciousness3. Air embolisma) Caused by diver holding their breath due to inexperience,equipment failure, underwater emergencies, or toconserve airb) Gases leave a damaged lung and enter the bloodstreamc) Signs and symptoms(1) Blurred vision(2) Chest pains(3) Numbness and tingling(4) Weakness/paralysis(5) Frothy blood at mouth and nose(6) Convulsions(7) Unconsciousness occurs rapidly(8) Respiratory or cardiac arrest4. Emergency medical care:a) Maintain an open airwayb) Consider need or spinal immobilizationc) Administer high concentration oxygend) Rapid transport. Consider transport to a hyperbaricchamber or consult medical controle) Keep patient warmf) Position patient supine or on sideg) Transport dive gear with patientBites and StingsA. Signs and symptoms1. History of bite (spider, snake) or sting (insect, scorpion, marineanimal)2. Pain3. Redness4. Swelling5. WeaknessModule 4-78
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education6. Dizziness7. Chills8. Fever9. Nausea10. Vomiting11. Bite marks12. StingerB. Emergency medical care1. If stinger present, remove ita) Scrape stinger out; e.g., with edge of cardb) Avoid using tweezers or forceps as these can squeezevenom from the venom sac into the wound2. Wash area gently3. Remove jewelry from injured area before swelling begins, ifpossible4. Place injection site slightly below the level of the patient's heart5. Do not apply cold to snakebites6. Consult medical direction regarding constricting band forsnakebite7. Observe for development of signs and symptoms of an allergicreaction; treat as neededAPPLICATIONProcedural (How)1. Show illustrations of signs and symptoms of cold injuries.2. Demonstrate the steps in providing emergency medical care to a patientexposed to the cold.3. Describe the various ways that the body loses heat.4. Show illustrations of the signs and symptoms heat emergencies.5. Demonstrate the assessment and emergency medical care of a patient withexposure to heat.6. Demonstrate the assessment and emergency medical care of a patient withexposure to cold.7. Demonstrate the assessment and emergency medical care of a neardrowning patient.8. Demonstrate how to remove a patient from the water who has a suspectedspine injury.Contextual (When, Where, Why)1. Patients suffering from heat and cold emergencies or those involved in waterrelated emergencies must be promptly recognized through assessment ofsigns and symptoms.2. Patients with heat and cold emergencies must be rapidly moved to theambulance to remove them from the environment.Module 4-79
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education3. Warming of the cold-exposed patient and cooling of the heat-exposed patientis necessary to reduce the incidence of morbidity and mortality.4. Immediate resuscitation of the water-related patient may require rapidintervention to prevent death.STUDENT ACTIVITIESAuditory (Hear)1. The student should hear simulations involving the assessment, recognitionand emergency medical care of cold, heat and water-related emergencies.Visual (See)1. The student should see audio-visual aids or materials of signs and symptomsof cold injuries.2. The student should see a demonstration of the steps in providing emergencymedical care to a patient exposed to cold.3. The student should see an illustration or demonstration of the various waysthat the body loses heat.4. The student should see audio-visual aids or materials of the signs andsymptoms of heat emergencies.5. The student should see a demonstration of the assessment and emergencymedical care of a patient with exposure to heat.6. The student should see a demonstration of the assessment and emergencymedical care of a patient with exposure to cold.7. The student should see a demonstration of the assessment and emergencymedical care of a near drowning patient.8. The student should see a demonstration of how to remove a patient from thewater who has a suspected spinal injury.Kinesthetic (Do)1. The student should practice the steps in providing emergency medical care toa patient exposed to cold.2. The student should practice the assessment and emergency medical care ofa patient with exposure to heat.3. The student should practice the assessment and emergency medical care ofa patient with exposure to cold.4. The student should practice the assessment and emergency medical care ofa near drowning patient.5. The student should practice the skills involved in removing a patient from thewater who has a suspected spinal injury.6. The student should practice completing a prehospital report for patients withenvironmental emergencies.INSTRUCTOR ACTIVITIES1. Supervise student practice.2. Reinforce student progress in cognitive, affective, and psychomotor domains.3. Redirect students having difficulty with content (complete remediation forms).Module 4-80
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationEVALUATIONWritten:Practical:Develop evaluation instruments, e.g., quizzes, verbal reviews,handouts, to determine if the students have met the cognitiveand affective objectives of this lesson.Evaluate the actions of the EMT-Basic students during role play,practice or other skill stations to determine their compliance withthe cognitive and affective objectives and their mastery of thepsychomotor objectives of this lesson.REMEDIATIONIdentify students or groups of students who are having difficulty with this subjectcontent. Complete remediation sheet from the instructor's course guide.ENRICHMENTWhat is unique in the local area concerning this topic? Complete enrichment sheetsfrom the instructor's course guide and attach with lesson plan. Use floatingbackboards and CPR techniques in water rescue.Module 4-81
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationMODULE 4Medical/BehavioralandObstetrics/GynecologyLesson 4-8BehavioralEmergenciesModule 4-82
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationOBJECTIVES LEGENDC=Cognitive P=Psychomotor A=Affective1 = Knowledge level2 = Application level3 = Problem-solving levelOBJECTIVESCOGNITIVE OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:4-8.1 Define behavioral emergencies. (C-1)4-8.2 Discuss the general factors that may cause an alteration in a patient'sbehavior. (C-1)4-8.3 State the various reasons for psychological crises. (C-1)4-8.4 Discuss the characteristics of an individual's behavior which suggeststhat the patient is at risk for suicide. (C-1)4-8.5 Discuss special medical/legal considerations for managing behavioralemergencies. (C-1)4-8.6 Discuss the special considerations for assessing a patient withbehavioral problems. (C-1)4-8.7 Discuss the general principles of an individual's behavior whichsuggests that he is at risk for violence. (C-1)4-8.8 Discuss methods to calm behavioral emergency patients. (C-1)4-8.9 Discuss the risks for developing positional asphyxia. (C-1)AFFECTIVE OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:4-8.10 Explain the rationale for learning how to modify your behavior towardthe patient with a behavioral emergency. (A-3)PSYCHOMOTOR OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:4-8.11 Demonstrate the assessment and emergency medical care of thepatient experiencing a behavioral emergency. (P-1,2)4-8.12 Demonstrate various techniques to safely restrain a patient with abehavioral problem. (P-1,2)PREPARATIONMotivation:The EMT-Basic will respond to many situations involvingbehavioral emergencies. Some of these result from aninjury or acute illness of the patient. Others are the resultModule 4-83
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Educationof mental illness or the use of mind altering substances.Restraints are the best LAST option in a behavioralemergency.Prerequisites:AV Equipment:EMS Equipment:Primary Instructor:Assistant Instructor:BLS, Preparatory, Airway and Patient Assessment.MATERIALSUtilize various audio-visual materials relating tobehavioral emergencies. The continuous design anddevelopment of new audio-visual materials relating toEMS requires careful review to determine which bestmeet the needs of the program. Materials should beedited to assure meeting the objectives of the <strong>curriculum</strong>.Stretcher, restraints.PERSONNELOne EMT-Basic instructor knowledgeable in behavioralemergencies.None required.PRESENTATIONDeclarative (What)I. BehaviorA. Behavior - manner in which a person acts or performs; any or allactivities of a person, including physical and mental activityB. Behavioral Emergency - a situation where the patient exhibitsabnormal behavior within a given situation that is unacceptable orintolerable to the patient, family or community. This behavior can bedue to extremes of emotion leading to violence or other inappropriatebehavior or due to a psychological or physical condition such as lack ofoxygen or low blood sugar in diabetes.II. Behavioral ChangeA. General factors that may alter a patient's behavior - the number offactors which may alter a patient's behavior include situationalstresses, medical illnesses, psychiatric problems and alcohol or drugs.Below is a list of common causes for behavior alteration.1. Low blood sugar2. Lack of oxygen3. Inadequate blood flow to the brain4. Head trauma5. Mind altering substancesModule 4-84
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education6. Psychogenic - resulting in psychotic thinking, depression orpanic7. Excessive cold8. Excessive heatIII. Psychologic CrisesA. PanicB. AgitationC. Bizarre thinking and behaviorD. Danger to self - self destructive behavior, suicideE. Danger to others - threatening behavior, violenceIV. Assessment for Suicide RiskA. Depression1. Sad, tearful2. Thoughts of death or taking one's lifeB. Suicidal gestures - the EMT-Basic must recognize and intervene inself-destructive behavior before the patient commits the act of suicide.Risk factors may include:1. Individuals over 40, single, widowed or divorced, alcoholic,depressed2. A defined lethal plan of action which has been verbalized3. Unusual gathering of articles which can cause death such aspurchase of a gun, large volumes of pills, etc.4. Previous history of self-destructive behavior5. Recent diagnosis of serious illness6. Recent loss of significant loved one7. Arrest, imprisonment, loss of jobC. Assessment findings1. Patient in an unsafe environment or with unsafe objects inhands2. Displaying of self-destructive behavior during initial assessmentor prior to emergency response3. Important questions to be considereda) How does the patient feelb) Determine suicidal tendenciesc) Is patient a threat to self or othersd) Is there a medical probleme) InterventionsD. Emergency medical care1. Scene size-up, personal safety2. Patient assessment3. Calm the patient - do not leave patient alone4. Restrain if necessary. Consider need for law enforcement5. Transport6. If overdose, bring medications or drugs found to medical facilityV. Medical/Legal ConsiderationsModule 4-85
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationVI.A. Emotionally disturbed patient who consents to care - legal problemsgreatly reducedB. How to handle the patient who resists treatment1. Emotionally disturbed patient will often resist treatment2. May threaten EMT-Basics and others3. To provide care against patient's will, you must show areasonable belief the patient would harm himself or others4. If a threat to self or others, patient may be transported withoutconsent after contacting medical direction5. Usually law enforcement is requiredC. Avoiding unreasonable force1. Reasonable force depends on what force was necessary tokeep patient from injuring himself or others2. Reasonableness is determined by looking at all circumstancesinvolveda) Patients size and strengthb) Type of abnormal behaviorc) Sex of patientd) Mental state of patiente) Method of restraint3. Be aware after a period of combativeness and aggression somecalm patients may cause unexpected and sudden injury to selfand others4. Avoid acts or physical force that may cause injury to the patient5. EMS personnel may use reasonable force to defend against anattack by emotionally disturbed patientsD. Police and medical direction involvement1. Seek medical direction when considering restraining a patient2. Ask for police assistance if during scene size-up the patientappears or acts aggressive or combativeE. Protection against false accusations1. Documentation of abnormal behavior exhibited by the patient isvery important2. Have witnesses in attendance especially during transport, ifpossible3. Accusing EMT-Basics of sexual misconduct is common byemotionally disturbed patients - have help, same sexattendants, and third party witnessesPrinciples for Assessing Behavioral Emergency PatientsA. Identify yourself and let the person know you are there to helpB. Inform him of what you are doingC. Ask questions in a calm, reassuring voiceD. Allow the patient to tell what happened without being judgmentalE. Show you are listening by rephrasing or repeating part of what is saidF. Acknowledge the patient's feelingsG. Assess the patient's mental statusModule 4-86
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationVII.VIII.IX.1. Appearance2. Activity3. Speech4. Orientation for time, person, and placeAssessment of Potential ViolenceA. Scene size-upB. History - the EMT-Basic should check with family and bystanders todetermine if the patient has a known history of aggression orcombativenessC. Posture - stands or sits in a position which threatens self or others.May have fists clinched or lethal objects in hands.D. Vocal activity - is yelling or verbally threatens harm to self or othersE. Physical activity - moves toward caregiver, carries heavy orthreatening objects, has quick irregular movements, muscles tense.Methods to Calm Behavioral Emergency PatientsA. Acknowledge that the person seems upset and restate that you arethere to helpB. Inform him of what you are doingC. Ask questions in a calm, reassuring voiceD. Maintain a comfortable distanceE. Encourage the patient to state what is troubling himF. Do not make quick movesG. Respond honestly to patient's questionsH. Do not threaten, challenge or argue with disturbed patientsI. Tell the truth, do not lie to the patientJ. Do not "play along" with visual or auditory disturbances of the patientK. Involve trusted family members or friendsL. Be prepared to stay at scene for a long time. Always remain with thepatient.M. Avoid unnecessary physical contact. Call additional help if needed.N. Use good eye contactRestraining Patients - restraint should be avoided unless patient is a dangerto self and others. When using restraints have police present, if possible, andget approval from medical direction. If restraints must be used, do thefollowing:A. Be sure to have adequate helpB. Plan your activitiesC. Use only the force necessary for restraintD. Estimate range of motion of patient’s arms and legs and stay beyondrange until readyE. Once decision has been made - act quicklyF. Have one EMT-Basic talk to patient throughout restrainingG. Approach with four persons, one assigned to each limb all at the sametimeH. Secure limbs with equipment approved by medical direction1. Soft restraints are preferredModule 4-87
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education2. Rigid restraints, such as metal handcuffs, should only beapplied by law enforcement officers, who must remain availableat all times, should the restraints need adjustmentI. Place patient on stretcher. Refer to local protocol. Positioning apatient face down on stretcher may place them at risk for positionalasphyxia. EMTs should not hobble or hog-tie any patients.J. Secure to stretcher with multiple straps. Patient’s position should in noway compromise breathing or circulationK. Cover face with surgical mask if spitting on EMT-BasicsL. Reassess breathing and circulation frequentlyM. Documentation1. Reason for use of restraints2. Time applied3. Method of restraint4. Position of the patient5. Ongoing assessment findings, including LOC, airway, breathingand circulatory status6. Other management and treatmentN. Avoid unnecessary force.X. Other Behavioral ProblemsA. Always try to talk patient into cooperationB. Do not belittle or threaten patientsC. Be calm and patient in your attitudeD. Do not agree with disturbed thinkingE. Be reassuringF. Avoid arguing with irrational patientsG. Suggest appropriate steps to takeH. Lower distressing stimuliI. Avoid restraints unless necessaryJ. Treat with respectAPPLICATIONProcedural (How)1. Demonstrate the assessment and emergency medical care of the patientexperiencing a behavioral emergency.2. Demonstrate the method of restraint.Contextual (When, Where, Why)1. The EMT-Basic will frequently handle behavioral emergencies since manypeople are aware these persons need help, but are unsure what to do inemergency situations.2. Because treatment of these emergencies usually requires long termmanagement, little medical intervention can be done in the acute situation.Module 4-88
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education3. The EMT-Basic must assure his own safety in these situations, consider thelegal ramifications of his actions, and transport the patient in a safe andeffective manner.STUDENT ACTIVITIESAuditory (Hear)1. The student should hear audio tapes of patients with behavioral emergencies.Visual (See)1. The student should see audio-visual aids or materials of behavioralconditions, patient interviewing, and use of restraints.Kinesthetic (Do)1. The student should practice physically restraining another student who issimulating moderate resist.INSTRUCTOR ACTIVITIES1. Supervise student practice.2. Reinforce student progress in cognitive, affective, and psychomotor domains.3. Redirect students having difficulty with content (complete remediation forms).EVALUATIONWritten:Practical:Develop evaluation instruments, e.g., quizzes, verbal reviews,handouts, to determine if the students have met the cognitiveand affective objectives of this lesson.Evaluate the actions of the EMT-Basic students during role play,practice or other skill stations to determine their compliance withthe cognitive and affective objectives and their mastery of thepsychomotor objectives of this lesson.REMEDIATIONIdentify students or groups of students who are having difficulty with this subjectcontent. Complete remediation sheet from the instructor's course guide.ENRICHMENTWhat is unique in the local area concerning this topic? Complete enrichment sheetsfrom the instructor's course guide and attach with lesson plan.Module 4-89
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationMODULE 4Medical/BehavioralandObstetrics/GynecologyLesson 4-9Obstetrics/GynecologyModule 4-90
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationOBJECTIVES LEGENDC=Cognitive P=Psychomotor A=Affective1 = Knowledge level2 = Application level3 = Problem-solving levelOBJECTIVESCOGNITIVE OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:4-9.1 Identify the following structures: Uterus, vagina, fetus, placenta,umbilical cord, amniotic sac, perineum. (C-1)4-9.2 Identify and explain the use of the contents of an obstetrics kit. (C-1)4-9.3 Identify pre-delivery emergencies. (C-1)4-9.4 State indications of an imminent delivery. (C-1)4-9.5 Differentiate the emergency medical care provided to a patient withpre-delivery emergencies from a normal delivery. (C-3)4-9.6 State the steps in the pre-delivery preparation of the mother. (C-1)4-9.7 Establish the relationship between body substance isolation andchildbirth. (C-3)4-9.8 State the steps to assist in the delivery. (C-1)4-9.9 Describe care of the baby as the head appears. (C-1)4-9.10 Describe how and when to cut the umbilical cord. (C-1)4-9.11 Discuss the steps in the delivery of the placenta. (C-1)4-9.12 List the steps in the emergency medical care of the motherpost-delivery. (C-3)4-9.13 Summarize neonatal resuscitation procedures. (C-1)4-9.14 Describe the procedures for the following abnormal deliveries: Breechbirth, prolapsed cord, limb presentation, and shoulder dystocia. (C-1)4-9.15 Differentiate the special considerations for multiple births. (C-3)4-9.16 Describe special considerations of meconium. (C-1)4-9.17 Describe special considerations of a premature baby. (C-1)4-9.18 Discuss the emergency medical care of a patient with a gynecologicalemergency. (C-1)4-9.19 Discuss the emergency medical care of a patient who has beensexually assaulted. (C-1)4-9.20 Discuss the process of preserving evidence of an alleged sexualassault. (C-1)AFFECTIVE OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:4-9.21 Explain the rationale for understanding the implications of treating twopatients (mother and baby). (A-3)Module 4-91
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education4-9.22 Appreciate the emotions that a sexual assault victim may beexperiencing. (A-1)PSYCHOMOTOR OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:4-9.23 Demonstrate the steps to assist in the normal cephalic delivery. (P-1,2)4-9.24 Demonstrate necessary care procedures of the fetus as the headappears. (P-1,2)4-9.25 Demonstrate infant neonatal procedures. (P-1,2)4-9.26 Demonstrate post delivery care of infant. (P-1,2)4-9.27 Demonstrate how and when to cut the umbilical cord. (P-1,2)4-9.28 Attend to the steps in the delivery of the placenta. (P-1,2)4-9.29 Demonstrate the post-delivery care of the mother. (P-1,2)4-9.30 Demonstrate the procedures for the following abnormal deliveries:vaginal bleeding, breech birth, prolapsed cord, limb presentation.(P-1,2)4-9.31 Demonstrate the steps in the emergency medical care of the motherwith excessive bleeding. (P-1,2)4-9.32 Demonstrate completing a prehospital care report for patients withobstetrical/gynecological emergencies. (P-2)PREPARATIONMotivation:Prerequisites:AV Equipment:EMS Equipment:Childbirth in the prehospital setting does occur on rareoccasions. Because of the infrequency, taking care of ananxious mother and newborn infant is a stressfulemergency call for the EMT-Basic. Knowledge andpractice in simulated situations can decrease stress andlead to better mother and child care.BLS, Preparatory, Airway and Patient Assessment.MATERIALSUtilize various audio-visual materials relating toobstetrics/gynecology. The continuous design anddevelopment of new audio-visual materials relating toEMS requires careful review to determine which bestmeet the needs of the program. Materials should beedited to assure meeting the objectives of the <strong>curriculum</strong>.Childbirth kit, airway management equipment, eyeprotection, gloves.Module 4-92
State of WisconsinPrimary Instructor:Assistant Instructor:EMT-Basic: A Practice BasedApproach to EMS EducationPERSONNELOne EMT-Basic instructor familiar with childbirth who haseither delivered a child in the out-of-hospital setting orhas seen or assisted with a vaginal delivery within thehospital.The instructor-to-student ratio should be 1:6 forpsychomotor skill practice. Individuals used as assistantinstructors should be knowledgeable inobstetric/gynecological emergencies.PRESENTATIONDeclarative (What)I. Reproductive anatomy and physiologyA. Fetus - developing unborn babyB. Uterus - organ in which a fetus grows, responsible for labor andexpulsion of infantC. Birth Canal - vagina and lower part of the uterusD. Placenta - fetal organ through which fetus exchanges nourishment andwaste products during pregnancyE. Umbilical cord - cord which is an extension of the placenta throughwhich fetus receives nourishment while in the uterusF. Amniotic sac (bag of water) - the sac that surrounds the fetus insidethe uterusG. Vagina - lower part of the birth canalH. Perineum - skin area between vagina and anus, commonly torn duringdeliverI. Crowning - the bulging-out of the vagina which is opening as the fetus'head or presenting part presses against itJ. "Bloody Show" - mucus and blood that may come out of the vagina aslabor beginsK. Labor - the time and process (defined in 3 or 4 stages) beginning withthe first uterine muscle contraction until delivery of the placenta1. Delivery is imminent2. Crowning3. In the process of deliveringL. Presenting Part - the part of the infant/fetus that comes first - usuallythe headM. Abortion - miscarriage - delivery of products of conception early inpregnancyII. Contents of a childbirth delivery kitA. Surgical scissorsB. Hemostats or cord clampsC. Umbilical tape or sterilized cordModule 4-93
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationIII.IV.D. Bulb syringeE. TowelsF. 2 x 10 gauze spongesG. Sterile glovesH. One baby blanketI. Sanitary napkinsJ. Plastic bagEmergency Medical Care - Predelivery EmergenciesA. Miscarriage - Spontaneous abortion - emergency medical care1. Size up2. Initial assessment3. History and physical exam4. Assess baseline vitals5. Treatment based on signs and symptoms6. Apply external vaginal pads7. Bring fetal tissues to hospital8. Support motherB. Seizure during pregnancy - emergency medical care1. Size up2. Initial assessment3. History and physical exam4. Assess baseline vitals5. Treatment based on signs and symptoms6. Transport on left sideC. Vaginal bleeding - late pregnancy vaginal bleeding, with or withoutpain. Emergency medical care:1. Size up2. Initial assessment3. History and physical exam4. Assess baseline vitals5. Treatment based on signs and symptoms6. Apply external vaginal pads7. TransportD. Trauma - emergency medical care - same as other trauma patients1. Size up2. Initial assessment3. History and physical exam4. Assess baseline vitals5. Treatment based on signs and symptoms6. Transport on left sideNormal DeliveryA. Predelivery considerations1. It is best to transport an expecting mother, unless delivery isexpected within a few minutes based on assessment of:a) Are you pregnant?b) How long have you been pregnant?Module 4-94
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Educationc) Are there contractions or pain?d) Any bleeding or discharge?e) Is crowning occurring with contractions?f) What is the frequency and duration of contractions?g) Does she feel as if she is having a bowel movement withincreasing pressure in the vaginal area?h) Does she feel the need to push?i) Rock hard abdomen?2. Precautionsa) Use body substance isolationb) Do not touch vaginal areas except during delivery andwhen your partner is presentc) Do not let the mother go to bathroomd) Do not hold mother's legs togethere) Recognize your own limitations and transport even ifdelivery must occur during transportf) If delivery is eminent with crowning, contact medicaldirection for decision to commit to delivery on site. Ifdelivery does not occur within 10 minutes, contactmedical direction for permission to transport.B. Delivery procedures1. Apply gloves, mask, gown, eye protection for infection controlprecautions2. Have mother lie with knees drawn up and spread apart3. Elevate buttocks - with blankets or pillow4. Create sterile field around vaginal opening with sterile towels orpaper barriers5. When the infant's head appears during crowning, place fingerson bony part of skull (not fontanelle or face) and exert verygentle pressure to prevent explosive delivery. Use caution toavoid fontanelle.6. If the amniotic sac does not break, or has not broken, use aclamp to puncture the sac and push it away from the infant'shead and mouth as they appear7. As the infant's head is being born, determine if the umbilicalcord is around the infant's neck; slip over the shoulder or clamp,cut and unwrap8. After the infant's head is born, support the head, suction themouth two or three times and the nostrils. Use caution to avoidcontact with the back of the mouth.9. As the torso and full body are born, support the infant with bothhands10. As the feet are born, grasp the feet11. Wipe blood and mucus from mouth and nose with sterile gauze,suction mouth and nose againModule 4-95
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education12. Wrap infant in a warm blanket and place on its side, headslightly lower than trunk13. Keep infant level with vagina until the cord is cut14. Assign partner to monitor infant and complete initial care of thenewborn15. Clamp, tie and cut umbilical cord (between the clamps) aspulsations cease approximately 4 fingers width from infant16. Observe for delivery of placenta while preparing mother andinfant for transport17. When delivered, wrap placenta in towel and put in plastic bag;transport placenta to hospital with mother18. Place sterile pad over vaginal opening, lower mother's legs, helpher hold them together19. Record time of delivery and transport mother, infant andplacenta to hospitalC. Vaginal bleeding following delivery - up to 500 cc of blood loss isnormal following delivery1. A 500 cc blood loss is well tolerated by the mother followingdelivery. The EMT-Basic must be aware of this loss so as not tocause undue psychological stress on himself or the new mother.2. With excessive blood loss, massage the uterus.a) Hand with fingers fully extendedb) Place on lower abdomen above pubisc) Massage (knead) over aread) Bleeding continues - check massage technique andtransport immediately, providing oxygen and ongoingassessment3. Regardless of estimated blood loss, if mother appears in shock,treat as such and transport prior to uterine massage. Massageen route.D. Initial care of the newborn1. Position, dry, wipe, and wrap newborn in blanket and cover thehead.2. Repeat suctioning3. Assessment of infant - normal findingsa) Appearance - color: no central (trunk) cyanosisb) Pulse - greater than 100/minc) Grimace - vigorous and cryingd) Activity - good motion in extremitiese) Breathing effort - normal, crying4. Stimulate newborn if not breathinga) Flick soles of feetb) Rub infant's backE. Resuscitation of the newborn follows the inverted pyramid (seeAppendix K) - after assessment, if signs and symptoms require eithercardiac or pulmonary resuscitation, do the following when appropriate:Module 4-96
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education1. Breathing effort - if shallow, slow or absent provide artificialventilations:a) 60/minb) Reassess after 30 secondsc) If no improvement, continue artificial ventilations andreassessments2. Heart ratea) If less than 100 beats per minute provide artificialventilations:(1) 60/min(2) Reassess after 30 seconds(3) If no improvement continue artificial ventilationsand reassessmentsb) If less than 80 beats per minute and not responding tobag-valve-mask, start chest compressionsc) If less than 60 beats per minute, start compressions andartificial ventilations3. Color - if central cyanosis is present with spontaneous breathingand an adequate heart rate administer free flow oxygen -administer oxygen (10-15L) using oxygen tubing held as closeas possible to the newborn's faceV. Abnormal DeliveriesA. Prolapsed Cord - condition where the cord presents through the birthcanal before delivery of the head; presents a serious emergency whichendangers the life of the unborn fetus1. Size up2. Initial assessment3. Mother should have high flow oxygen4. History and physical exam5. Assess baseline vitals6. Treatment based on signs and symptoms7. Position mother with head down or buttocks raised using gravityto lessen pressure in birth canal8. Insert sterile gloved hand into vagina pushing the presentingpart of the fetus away from the pulsating cord9. Rapidly transport, keeping pressure on presenting part andmonitoring pulsations in the cordB. Breech birth presentation - breech presentation occurs when thebuttocks or lower extremities are low in the uterus and will be the firstpart of the fetus delivered1. Newborn at great risk for delivery trauma, prolapse cord morecommon, transport immediately upon recognition of breechpresentation2. Delivery does not occur within 10 minutes3. Emergency medical carea) Immediate rapid transportation upon recognitionModule 4-97
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationVI.VII.b) Place mother on oxygenc) Place mother in head down position with pelvis elevatedC. Limb presentation - occurs when a limb of the infant protrudes from thebirth canal. Is more commonly a foot when infant is in breechpresentation.1. Immediate rapid transportation upon recognition2. Place mother on oxygen3. Place mother in head down position with pelvis elevatedD. Shoulder dystocia – occurs when the infant’s shoulders get stuck in thebirth canal but the head has delivered.1. Immediate rapid transport2. Place mother on oxygen3. Support infant’s airway4. Keep pressure off the umbilical cordE. Multiple births1. Be prepared for more than one resuscitation2. Call for assistanceF. Meconium - amniotic fluid that is greenish or brownish-yellow ratherthan clear; an indication of possible fetal distress during labor1. Do not stimulate before suctioning oropharynx2. Suction3. Maintain airway4. Transport as soon as possibleG. Premature1. Always at risk for hypothermia2. Usually requires resuscitation, should be done unless physicallyimpossibleGynecological emergenciesA. Vaginal bleeding1. Body substance isolation2. AirwayB. Trauma - external genitalia - treat as other bleeding soft tissue injuries;never pack vagina, provide oxygen and on-going patient assessmentAlleged sexual assault - criminal assault situations require initial and on-goingassessment/management and psychological care. Emergency medical care:1. Body substance isolation2. Airway management3. Portray a non-judgmental attitude4. Reassure patient of their safety5. Crime scene protectiona) Minimize contamination of crime sceneb) Attempt to preserve evidencec) Minimize number of rescue personnel entering the scened) Minimize “chain of evidence”e) Enlist law enforcement assistance for evidence collection6. Evidence preservation – discourage patient from:Module 4-98
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Educationa) Bathingb) Voiding or defecatingc) Cleaning woundsd) Drinking fluids or brushing teeth. If patient insists onbrushing teeth, have them chew on gauze first andpreserve by placing in a paper bag.e) Changing clothes. If patient absolutely insists onchanging clothes, have them stand on a clean or sterilesheet to undress. Save sheet and patient’s clothing in apaper bag.7. Examine genitalia only if profuse bleeding present8. Use same gender EMT-Basic for care when possible9. Follow crime reporting requirementsAPPLICATIONProcedural (How)1. Demonstrate the steps to assist in the normal delivery.2. Demonstrate necessary care procedures of the fetus as the head appears.3. Demonstrate neonatal resuscitation procedures.4. Demonstrate how and when to cut the umbilical cord.5. Discuss the steps in delivery of the placenta.6. Demonstrate the post-delivery care of mothers and neonates.7. Demonstrate the procedures for the following abnormal deliveries: Breechbirth, prolapsed cord, limb presentation.8. Demonstrate the steps in emergency medical care of the mother withexcessive bleeding.9. Demonstrate the steps in the emergency care of the female patient withgynecological disorders.Contextual (When, Where, Why)1. Care of patients with prehospital conditions involving reproductive organs arenot common.2. This private condition to the patient requires the most professional, safe andeffective care by the EMT-Basic.3. Knowledge and skills practice in the laboratory setting, particularly for out-ofhospitalchildbirth, help the student maintain professionalism, understandthese uncommon emergency care situations and support the patient as theyseek definitive care in the receiving facility.STUDENT ACTIVITIESAuditory (Hear)1. The student should hear a video tape of a mother in the final stages of laborwhich provides samples of mother's actions during this painful process.Module 4-99
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationVisual (See)1. The student should see audio-visual aids or materials of labor and deliveryshowing: Late stages of labor normal delivery, clamping and cutting umbilicalcord, suctioning infant's head during delivery, assessment and initial care ofneonate, normal bleeding with delivery, delivery and care of placenta.Kinesthetic (Do)1. Student should practice the steps to assist in the normal delivery.2. Student should practice necessary care procedures of the fetus as the headappears during delivery.3. Student should practice neonatal resuscitation procedures.4. Student should practice how and when to cut the umbilical cord using simplepieces of rope.5. Student should practice the post-delivery care of mothers and neonates.6. Student should practice completing a prehospital care report for patients withobstetrical/gynecological emergencies.INSTRUCTOR ACTIVITIES1. Supervise student practice.2. Reinforce student progress in cognitive, affective, and psychomotor domains.3. Redirect students having difficulty with content (complete remediation forms).EVALUATIONWritten:Practical:Develop evaluation instruments, e.g., quizzes, verbal reviews,handouts, to determine if the students have met the cognitiveand affective objectives of this lesson.Evaluate the actions of the EMT-Basic students during role play,practice or other skill stations to determine their compliance withthe cognitive and affective objectives and their mastery of thepsychomotor objectives of this lesson.REMEDIATIONIdentify students or groups of students who are having difficulty with this subjectcontent. Complete remediation sheet from the instructor's course guide.ENRICHMENTWhat is unique in the local area concerning this topic? Complete enrichment sheetsfrom the instructor's course guide and attach with lesson plan.Module 4-100
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationMODULE 4Medical/BehavioralandObstetrics/GynecologyLesson 4-10Acute AbdomenModule 4-101
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationOBJECTIVES LEGENDC=Cognitive P=Psychomotor A=Affective1 = Knowledge level2 = Application level3 = Problem-solving levelOBJECTIVESCOGNITIVE OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:4-10.1 Describe the structures and function of the organs contained within theabdominal cavity. (C-1)4-10.2 Define the term acute abdomen. (C-1)4-10.3 Describe the assessment of a patient with acute abdominal pain. (C-1)4-10.4 List the signs and symptoms of acute abdominal pain. (C-1)4-10.5 Explain the steps in providing emergency care to a patient with acuteabdominal pain. (C-1)4-10.6 Discuss possible causes of acute abdominal pain. (C-1)AFFECTIVE OBJECTIVES4-10.7 Appreciate the high level of discomfort that a patient with acuteabdominal pain will likely exhibit. (A-1)PSYCHOMOTOR OBJECTIVES4-10.8 Demonstrate assessment and examination techniques used for acuteabdominal pain. (P-2)4-10.9 Create a management plan to include assessment and treatment for apatient with acute abdominal pain (C-3)4-10.10 Demonstrate completing a prehospital care report for patients withacute abdominal pain. (P-2)PREPARATIONMotivation:Prerequisites:Patients suffering from an acute abdomen should bethoroughly evaluated for the possible cause of theirabdominal pain/discomfort. Providing appropriate painmanagement and transport is part of the prehospital carefor patient’s experiencing an acute abdomen.BLS, Preparatory, Airway and Patient Assessment.Module 4-102
State of WisconsinAV Equipment:EMS Equipment:Primary Instructor:Assistant Instructor:EMT-Basic: A Practice BasedApproach to EMS EducationMATERIALSUtilize various audio-visual materials relating toenvironmental emergencies. The continuous design anddevelopment of new audio-visual materials relating toEMS requires careful review to determine which bestmeet the needs of the program. Materials should beedited to assure meeting the objectives of the <strong>curriculum</strong>.Exam gloves, stethoscopes, blood pressure cuffs,penlight.PERSONNELOne EMT-Basic instructor knowledgeable in acuteabdominal emergencies.None required.PRESENTATIONDeclarative (What)I. Structures and function of organs within the abdominal cavityA. Solid organs-liver, spleen, pancreas, kidneys, ovariesB. Hollow organs-esophagus, stomach, small intestines, large intestines,colon, ureters, urinary bladder, uterus, fallopian tubesC. Quadrants1. Right upper (RUQ)2. Left upper (LUQ)3. Right lower (RLQ)4. Left lower (LLQ)II. Definition of acute abdomen - sudden onset of severe abdominal pain,associated with a wide variety of underlying causesIII. Possible causes of acute abdominal painA. Appendicitis1. Inflammation of the appendix2. Signs and symptomsa) Nausea and vomitingb) Fever and chillsc) Anorexiad) Rebound tendernesse) Radiating pain to the umbilicusf) Abdominal guardingB. Pancreatitis1. Inflammation of the pancreas2. Signs and symptomsa) Nausea and vomitingModule 4-103
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationIV.b) Abdominal tenderness and distentionc) Severe pain with radiation for the umbilicus to the backand shouldersd) May have signs of shockC. Abdominal aortic aneyrysm (AAA)1. Weakened, ballooned, and enlarged area of the wall of theabdominal aorta2. Signs and symptomsa) Gradual onset of lower lumbar and abdominal pain.Rupture associated with sudden onset of severe,constant abdominal painb) Pain described as “tearing”, may radiate to lower back,flank and pelvis.c) Nausea and vomiting possibled) Signs of shocke) Pulsating mass may be feltD. Other causes of acute abdomen1. Cholecystitis-inflammation of the gallbladder2. Intestinal obstruction3. Hernia4. Ulcers5. Esophageal varicesEmergency managementA. Initial assessment - ABCs, look for guarded position, be alert forvomiting and aspiration, shock, prioritize patientB. Focused History and Physical Exam - SAMPLE History, O-P-Q-R-S-T,baseline vital signs, gentle palpation of 4 quadrants (leaving mostpainful area for last), assess abdomen for rigidity, tenderness, ormassesC. Keep patient quiet and place in position of comfort, usually flexing thelegs is most comfortable (fetal position)D. Appropriate transportAPPLICATIONProcedural (How)1. Show illustrations of signs and symptoms of an acute abdomen.2. Demonstrate the steps in providing emergency medical care to a patient withan acute abdomen.Contextual (When, Where, Why)1. Acute abdominal pain is a common condition that EMTs will encounter.2. Underlying causes vary greatly and may often signal a very serious medicalcondition.Module 4-104
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education3. Be certain to assess for life-threatening conditions, make the patient ascomfortable, administer oxygen and transport.STUDENT ACTIVITIESAuditory (Hear)1. The student should hear simulations involving the assessment, recognitionand emergency medical care of an acute abdomen.Visual (See)1. The student should see audio-visual aids or materials of signs and symptomsof an acute abdomen.2. The student should see a demonstration of the steps in providing emergencymedical care to a patient with an acute abdomen.Kinesthetic (Do)1. The student should practice the steps in providing emergency medical care toa patient with an acute abdomen.2. The student should practice completing a prehospital report for patients withan acute abdomen.INSTRUCTOR ACTIVITIES1. Supervise student practice.2. Reinforce student progress in cognitive, affective, and psychomotor domains.3. Redirect students having difficulty with content (complete remediation forms).EVALUATIONWritten:Practical:Develop evaluation instruments, e.g., quizzes, verbal reviews,handouts, to determine if the students have met the cognitiveand affective objectives of this lesson.Evaluate the actions of the EMT-Basic students during role play,practice or other skill stations to determine their compliance withthe cognitive and affective objectives and their mastery of thepsychomotor objectives of this lesson.REMEDIATIONIdentify students or groups of students who are having difficulty with this subjectcontent. Complete remediation sheet from the instructor's course guide.Module 4-105
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationENRICHMENTWhat is unique in the local area concerning this topic? Complete enrichment sheetsfrom the instructor's course guide and attach with lesson plan. Use floatingbackboards and CPR techniques in water rescue.Module 4-106
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationMODULE 4Medical/BehavioralandObstetrics/GynecologyLesson 4-11Practical Lab:Medical/Behavioral andObstetrics/GynecologyModule 4-107
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationOBJECTIVES LEGENDC=Cognitive P=Psychomotor A=Affective1 = Knowledge level2 = Application level3 = Problem-solving levelOBJECTIVESCOGNITIVE OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:Demonstrate the cognitive objectives of Lesson 4-1: General Pharmacology.Demonstrate the cognitive objectives of Lesson 4-2: RespiratoryEmergencies.Demonstrate the cognitive objectives of Lesson 4-3: CardiovascularEmergencies.Demonstrate the cognitive objectives of Lesson 4-4: Diabetes/ Altered MentalStatus.Demonstrate the cognitive objectives of Lesson 4-5: Severe AllergicReactions.Demonstrate the cognitive objectives of Lesson 4-6: Poisoning/Overdose.Demonstrate the cognitive objectives of Lesson 4-7: EnvironmentalEmergencies.Demonstrate the cognitive objectives of Lesson 4-8: Behavioral Emergencies.Demonstrate the cognitive objectives of Lesson 4-9: Obstetrics/Gynecology.Demonstrate the cognitive objectives of Lesson 4-10: Acute Abdomen.AFFECTIVE OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:Demonstrate the affective objectives of Lesson 4-1: General Pharmacology.Demonstrate the affective objectives of Lesson 4-2: RespiratoryEmergencies.Demonstrate the affective objectives of Lesson 4-3: CardiovascularEmergencies.Demonstrate the affective objectives of Lesson 4-4: Diabetes/Altered MentalStatus.Demonstrate the affective objectives of Lesson 4-5: Severe AllergicReactions.Demonstrate the affective objectives of Lesson 4-6: Poisoning/Overdose.Demonstrate the affective objectives of Lesson 4-8: Behavioral Emergencies.Demonstrate the affective objectives of Lesson 4-9: Obstetrics/Gynecology.Demonstrate the affective objectives of Lesson 4-10: Acute Abdomen.Module 4-108
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationPSYCHOMOTOR OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:Demonstrate the psychomotor objectives of Lesson 4-1: GeneralPharmacology.Demonstrate the psychomotor objectives of Lesson 4-2: RespiratoryEmergencies.Demonstrate the psychomotor objectives of Lesson 4-3: CardiovascularEmergencies.Demonstrate the psychomotor objectives of Lesson 4-4: Diabetes/AlteredMental Status.Demonstrate the psychomotor objectives of Lesson 4-5: Severe AllergicReactions.Demonstrate the psychomotor objectives of Lesson 4-6: Poisoning/Overdose.Demonstrate the psychomotor objectives of Lesson 4-7: EnvironmentalEmergencies.Demonstrate the psychomotor objectives of Lesson 4-8: BehavioralEmergencies.Demonstrate the psychomotor objectives of Lesson 4-9:Obstetrics/Gynecology.Demonstrate the psychomotor objectives of Lesson 4-10: Acute Abdomen.PREPARATIONMotivation:Prerequisites:AV Equipment:The practical lesson is designed to allow the studentsadditional time to perfect skills. It is of utmost importancethat the students demonstrate proficiency of the skill,cognitive knowledge of the steps to perform a skill, and ahealthy attitude towards performing that skill on a patient.This is an opportunity for the instructor and assistantinstructors to praise progress and re-direct the studentstoward appropriate psychomotor skills. The material fromall preceding lessons and <strong>basic</strong> life support should beincorporated into these practical skill sessions.BLS, Preparatory, Airway and Patient Assessment.MATERIALSTypically none required.EMS Equipment: Equipment from the lists in Lessons 4-1 through 4-10.Primary Instructor:PERSONNELOne proctor for the written evaluation.Module 4-109
State of WisconsinAssistant Instructor:EMT-Basic: A Practice BasedApproach to EMS EducationThe instructor-to-student ratio should be 1:6 forpsychomotor skill practice. Individuals used as assistantinstructors should be knowledgeable inmedical/behavioral and obstetrics/gynecology.APPLICATIONProcedural (How)1. Instructor should demonstrate the procedural activities from Lesson 4-1:General Pharmacology.2. Instructor should demonstrate the procedural activities from Lesson 4-2:Respiratory Emergencies.3. Instructor should demonstrate the procedural activities from Lesson 4-3:Cardiovascular Emergencies.4. Instructor should demonstrate the procedural activities from Lesson 4-4:Diabetic Emergencies/Altered Mental Status.5. Instructor should demonstrate the procedural activities from Lesson 4-5:Severe Allergic Reactions.6. Instructor should demonstrate the procedural activities from Lesson 4-6:Poisoning/Overdose.7. Instructor should demonstrate the procedural activities from Lesson 4-7:Environmental Emergencies.8. Instructor should demonstrate the procedural activities from Lesson 4-8:Behavioral Emergencies.9. Instructor should demonstrate the procedural activities from Lesson 4-9:Obstetrics/Gynecology.10. Instructor should demonstrate the procedural activities from Lesson 4-10:Acute Abdomen.Contextual (When, Where, Why)1. Instructor should review contextual information from Lesson 4-1: GeneralPharmacology.2. Instructor should review contextual information from Lesson 4-2: RespiratoryEmergencies.3. Instructor should review contextual information from Lesson 4-3:Cardiovascular Emergencies.4. Instructor should review contextual information from Lesson 4-4: DiabeticEmergencies/Altered Mental Status.5. Instructor should review contextual information from Lesson 4-5: SevereAllergic Reactions.6. Instructor should review contextual information from Lesson 4-6:Poisoning/Overdose.7. Instructor should review contextual information from Lesson 4-7:Environmental Emergencies.Module 4-110
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education8. Instructor should review contextual information from Lesson 4-8: BehavioralEmergencies.9. Instructor should review contextual information from Lesson 4-9:Obstetrics/Gynecology.10. Instructor should review contextual information from Lesson 4-10: AcuteAbdomen.STUDENT ACTIVITIESAuditory (Hear)1. The students should hear the auditory information from Lesson 4-1: GeneralPharmacology.2. The students should hear the auditory information from Lesson 4-2:Respiratory Emergencies.3. The students should hear the auditory information from Lesson 4-3:Cardiovascular Emergencies.4. The students should hear the auditory information from Lesson 4-5: SevereAllergic Reactions.5. The students should hear the auditory information from Lesson 4-6:Poisoning/Overdose.6. The students should hear the auditory information from Lesson 4-7:Environmental Emergencies.7. The students should hear the auditory information from Lesson 4-8:Behavioral Emergencies.8. The students should hear the auditory information from Lesson 4-9:Obstetrics/Gynecology.9. The students should hear the auditory information from Lesson 4-10: AcuteAbdomen.Visual (See)1. The students should see the visual material from Lesson 4-1: GeneralPharmacology.2. The students should see the visual material from Lesson 4-2: RespiratoryEmergencies.3. The students should see the visual material from Lesson 4-3: CardiovascularEmergencies.4. The students should see the visual material from Lesson 4-4: DiabeticEmergencies/Altered Mental Status.5. The students should see the visual material from Lesson 4-5: Severe AllergicReactions.6. The students should see the visual material from Lesson 4-6:Poisoning/Overdose.7. The students should see the visual material from Lesson 4-7: EnvironmentalEmergencies.8. The students should see the visual material from Lesson 4-8: BehavioralEmergencies.Module 4-111
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS Education9. The students should see the visual material from Lesson 4-9:Obstetrics/Gynecology.10. The students should see the visual material from Lesson 4-10: AcuteAbdomen.Kinesthetic (Do)1. The students should practice the kinesthetic activities from Lesson 4-1:General Pharmacology.2. The students should practice the kinesthetic activities from Lesson 4-2:Respiratory Emergencies.3. The students should practice the kinesthetic activities from Lesson 4-3:Cardiovascular Emergencies.4. The students should practice the kinesthetic activities from Lesson 4-4:Diabetic Emergencies/Altered Mental Status.5. The students should practice the kinesthetic activities from Lesson 4-5:Severe Allergic Reactions.6. The students should practice the kinesthetic activities from Lesson 4-6:Poisoning/Overdose.7. The students should practice the kinesthetic activities from Lesson 4-7:Environmental Emergencies.8. The students should practice the kinesthetic activities from Lesson 4-8:Behavioral Emergencies.9. The students should practice the kinesthetic activities from Lesson 4-9:Obstetrics/Gynecology.10. The students should practice the kinesthetic activities from Lesson 4-10:Acute Abdomen.INSTRUCTOR ACTIVITIES1. Supervise student practice.2. Reinforce student progress in cognitive, affective, and psychomotor domains.3. Redirect students having difficulty with content (complete remediation forms).EVALUATIONPractical:Evaluate the actions of the EMT-Basic students during role play,practice or other skills stations to determine their compliance with thecognitive and affective objectives and their mastery of the psychomotorobjectives of this lesson.REMEDIATIONIdentify students or groups of students who are having difficulty with this subjectcontent. Complete remediation sheet from the instructor's course guide.Module 4-112
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationENRICHMENTWhat is unique in the local area concerning this topic? Complete enrichment sheetsfrom the instructor's course guide and attach with lesson plan.Module 4-113
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationMODULE 4Medical/BehavioralandObstetrics/GynecologyLesson 4-12Evaluation:Medical/BehavioralandObstetrics/GynecologyModule 4-114
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationOBJECTIVES LEGENDC=Cognitive P=Psychomotor A=Affective1 = Knowledge level2 = Application level3 = Problem-solving levelOBJECTIVESCOGNITIVE OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:Demonstrate knowledge of the cognitive objectives of Lesson 4-1: GeneralPharmacology.Demonstrate knowledge of the cognitive objectives of Lesson 4-2:Respiratory Emergencies.Demonstrate knowledge of the cognitive objectives of Lesson 4-3:Cardiovascular Emergencies.Demonstrate knowledge of the cognitive objectives of Lesson 4-4: Diabetes/Altered Mental Status.Demonstrate knowledge of the cognitive objectives of Lesson 4-5: SevereAllergic Reactions.Demonstrate knowledge of the cognitive objectives of Lesson 4-6:Poisoning/Overdose.Demonstrate knowledge of the cognitive objectives of Lesson 4-7:Environmental Emergencies.Demonstrate knowledge of the cognitive objectives of Lesson 4-8: BehavioralEmergencies.Demonstrate knowledge of the cognitive objectives of Lesson 4-9:Obstetrics/Gynecological.Demonstrate knowledge of the cognitive objectives of Lesson 4-10: AcuteAbdomen.AFFECTIVE OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:Demonstrate knowledge of the affective objectives of Lesson 4-1: GeneralPharmacology.Demonstrate knowledge of the affective objectives of Lesson 4-2: RespiratoryEmergencies.Demonstrate knowledge of the affective objectives of Lesson 4-3:Cardiovascular Emergencies.Demonstrate knowledge of the affective objectives of Lesson 4-4: Diabetes/Altered Mental Status.Demonstrate knowledge of the affective objectives of Lesson 4-5: SevereAllergic Reactions.Module 4-115
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationDemonstrate knowledge of the affective objectives of Lesson 4-6:Poisoning/Overdose.Demonstrate knowledge of the affective objectives of Lesson 4-8: BehavioralEmergencies.Demonstrate knowledge of the affective objectives of Lesson 4-9:Obstetrics/Gynecological.Demonstrate knowledge of the affective objectives of Lesson 4-10: AcuteAbdomen.PSYCHOMOTOR OBJECTIVESAt the completion of this lesson, the EMT-Basic student will be able to:Demonstrate knowledge of the psychomotor objectives of Lesson 4-1:General Pharmacology.Demonstrate knowledge of the psychomotor objectives of Lesson 4-2:Respiratory Emergencies.Demonstrate knowledge of the psychomotor objectives of Lesson 4-3:Cardiovascular Emergencies.Demonstrate knowledge of the psychomotor objectives of Lesson 4-4:Diabetes/Altered Mental Status.Demonstrate knowledge of the psychomotor objectives of Lesson 4-5: SevereAllergic Reactions.Demonstrate knowledge of the psychomotor objectives of Lesson 4-6:Poisoning/Overdose.Demonstrate knowledge of the psychomotor objectives of Lesson 4-7:Environmental Emergencies.Demonstrate knowledge of the psychomotor objectives of Lesson 4-8:Behavioral Emergencies.Demonstrate knowledge of the psychomotor objectives of Lesson 4-9:Obstetrics/Gynecological.Demonstrate knowledge of the psychomotor objectives of Lesson 4-10: AcuteAbdomen.PREPARATIONMotivation:Evaluation of the students' attainment of the cognitiveand affective knowledge and psychomotor skills is anessential component of the EMT-Basic educationalprocess. The <strong>module</strong>s are presented in a "buildingblock" format. Once the students have demonstratedtheir knowledge and proficiency, the next lesson shouldbe built upon that knowledge. This evaluation will help toidentify students or groups of students having difficultywith a particular area. This is an opportunity for theinstructor to evaluate his performance, and makeappropriate modification to the delivery of material.Module 4-116
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationPrerequisites: Completion of Lessons 4-1 through 4-10.AV Equipment:EMS Equipment:Primary Instructor:Assistant Instructor:MATERIALSTypically none required.Equipment required to evaluate the students proficiencyin the psychomotor skills of this <strong>module</strong>.PERSONNELOne proctor for the written evaluation.One practical skills examiner for each 6 students.PRESENTATIONDeclarative (What)I. Purpose of the evaluationII. Items to be evaluatedIII. Feed back from evaluationAPPLICATIONProcedural (How)1. Written evaluation based on the cognitive and affective objectives of Lessons4-1 through 4-10.2. Practical evaluation stations based on the psychomotor objectives of Lessons4-1 and 4-10.Contextual (When, Where and Why)1. The final lesson in this <strong>module</strong> is designed to bring closure to the <strong>module</strong>, andto assure that students are prepared to move to the next <strong>module</strong>.2. This modular evaluation is given to determine the effectiveness of thepresentation of materials and how well students have retained the material.3. This is an opportunity for the students to make necessary adjustments instudy habits or for the instructor to adjust the manner which material ispresented.INSTRUCTOR ACTIVITIES1. Supervise student evaluation.2. Reinforce student progress in cognitive, affective, and psychomotor domains.3. Redirect students having difficulty with content (complete remediation forms).Module 4-117
State of WisconsinEMT-Basic: A Practice BasedApproach to EMS EducationREMEDIATIONIdentify students and/or groups of students who are having difficulty with this subjectcontent. Complete a remediation sheet from the instructor's course guide. Ifstudents continue to have difficulty demonstrating knowledge of the cognitive andaffective objectives, or demonstrating proficiency in psychomotor skills, the studentsshould be counseled, remediated and re-evaluated. If improvements in cognitive,affective or psychomotor skills are not achieved, consideration regarding the abilityof the student to progress in the program should be taken into account.Module 4-118