cribriform-morular variant of papillary thyroid carcinoma
cribriform-morular variant of papillary thyroid carcinoma
cribriform-morular variant of papillary thyroid carcinoma
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
CASE REPORTDennis H. Kraus, MD, Section EditorCLINICAL CURIOSITY: CRIBRIFORM-MORULAR VARIANTOF PAPILLARY THYROID CARCINOMAKimberly M. Dalal, MD, 1 Dimitrios Moraitis, MD, 1 Carlos Iwamoto, MD, 2 Ashok R. Shaha, MD, 1Snehal G. Patel, MD, 1 Ronald A. Ghossein, MD 21 Division <strong>of</strong> Head and Neck Surgery, Department <strong>of</strong> Surgery, Memorial Sloan-Kettering Cancer Center,1275 York Avenue, New York, New York 10021. E-mail: shahaa@mskcc.org2 Department <strong>of</strong> Pathology, Memorial Sloan-Kettering Cancer Center, New York, New YorkAccepted 20 October 2005Published online 13 February 2006 in Wiley InterScience (www.interscience.wiley.com). DOI: 10.1002/hed.20383Abstract: Background. There is an increasing awareness <strong>of</strong>the association <strong>of</strong> <strong>papillary</strong> <strong>thyroid</strong> <strong>carcinoma</strong> and familial adenomatouspolyposis (FAP). Although the incidence is rare, mosttend to occur in women. Several authors have described a distinctivehistologic <strong>variant</strong> <strong>of</strong> <strong>papillary</strong> <strong>thyroid</strong> <strong>carcinoma</strong>, the<strong>cribriform</strong>-<strong>morular</strong> <strong>variant</strong>, which is associated with FAP but alsomay be encountered in patients with non-FAP. This diagnosismay precede the symptoms <strong>of</strong> colorectal polyposis.Methods. A healthy 36-year-old woman was seen with a left<strong>thyroid</strong> nodule, and a 34-year-old woman with FAP was seenwith a right <strong>thyroid</strong> nodule; both masses were suspicious for<strong>papillary</strong> <strong>thyroid</strong> <strong>carcinoma</strong>. Both patients underwent total <strong>thyroid</strong>ectomy.Results. Pathologic examination <strong>of</strong> both specimens revealed<strong>papillary</strong> <strong>thyroid</strong> <strong>carcinoma</strong>, <strong>cribriform</strong>-<strong>morular</strong> <strong>variant</strong>. The firstpatient subsequently underwent colonoscopy, which was negativefor polyposis.Conclusions. Patients diagnosed with the <strong>cribriform</strong>-<strong>morular</strong><strong>variant</strong> <strong>of</strong> <strong>papillary</strong> <strong>thyroid</strong> cancer should be screened for thepresence <strong>of</strong> FAP. VC 2006 Wiley Periodicals, Inc. Head Neck28: 471–476, 2006Keywords: <strong>papillary</strong> <strong>thyroid</strong> cancer; familial adenomatouspolyposis; <strong>cribriform</strong>-<strong>morular</strong> <strong>variant</strong>Correspondence to: A. R. ShahaPresented at the Eastern Section Meeting, Triological Society, Washington,DC, January 28–30, 2005.VC2006 Wiley Periodicals, Inc.There is a growing awareness <strong>of</strong> the association <strong>of</strong><strong>papillary</strong> <strong>thyroid</strong> <strong>carcinoma</strong> (PTC) and familial adenomatouspolyposis (FAP). Although the incidence<strong>of</strong> PTC in FAP is only 1% to 2%, most tend to occurin women. 1,2 Several authors have described a distinctivehistologic <strong>variant</strong> <strong>of</strong> PTC, the <strong>cribriform</strong><strong>morular</strong><strong>variant</strong>, which includes intermingled<strong>cribriform</strong>, follicular, <strong>papillary</strong>, trabecular, and<strong>morular</strong> architecture. 1,3 Immunohistochemically,these tumors stain positively for thyroglobulin,estrogen, and progesterone receptors. 1,4 This <strong>variant</strong><strong>of</strong> <strong>papillary</strong> <strong>carcinoma</strong> is extremely unusualand occurs predominantly in patients with FAP.However, the <strong>cribriform</strong>-<strong>morular</strong> <strong>variant</strong> may alsobe encountered in patients with non-FAP. At times,this diagnosis may predate the symptoms <strong>of</strong> colorectalpolyposis. The purpose <strong>of</strong> this report is to providean example <strong>of</strong> each <strong>of</strong> these clinical situationsand to discuss the therapeutic decisions involved.CASE REPORTPatient 1. A healthy 36-year-old woman was seenwith a left <strong>thyroid</strong> mass detected by her gynecolo-Cribriform-Morular Variant <strong>of</strong> Papillary Cancer HEAD & NECK—DOI 10.1002/hed May 2006 471
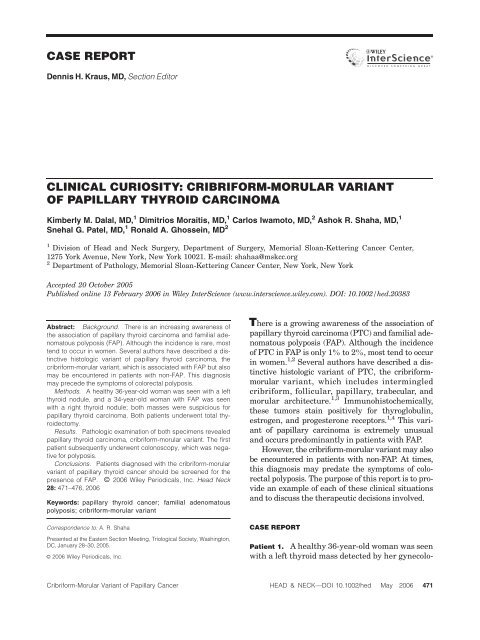
gist. Her family history was notable for memberswith both hyper<strong>thyroid</strong>ism and hypo<strong>thyroid</strong>ism; amaternal grandmother had colonic polyps at theage <strong>of</strong> 70.On physical examination, she had a 2 3 2 cm,firm, mobile nodule <strong>of</strong> the left <strong>thyroid</strong> lobe. No palpablecervical or supraclavicular lymphadenopathywas found. Ultrasound demonstrated a 2.1-cmmass in the left <strong>thyroid</strong> lobe as well as a 5-mmnodule in the isthmus. A <strong>thyroid</strong> scan revealed acold left <strong>thyroid</strong> nodule. A fine-needle aspiration(FNA) biopsy specimen demonstrated cells suspiciousfor follicular neoplasia. Thyroid functiontests were normal. On review <strong>of</strong> her disease by ourinstitution, concern was raised for a PTC. Thepatient underwent a total <strong>thyroid</strong>ectomy. Postoperatively,colonoscopy revealed a normal colonwithout polyposis.The final pathology report revealed a 2.05-cmPTC <strong>of</strong> the left <strong>thyroid</strong> lobe. The tumor was well differentiatedand did not have capsular or vascularinvasion, extra<strong>thyroid</strong>al extension, or multicentricity.Of note, the tumor was a ‘<strong>cribriform</strong>-<strong>morular</strong><strong>variant</strong>’ <strong>of</strong> PTC and demonstrated intermingled <strong>cribriform</strong>,follicular, <strong>papillary</strong>, trabecular, and <strong>morular</strong>architecture (Figure 1). The remainder <strong>of</strong> the<strong>thyroid</strong> had nodular hyperplasia. Immunohistochemically,the tumor stained positively for thyroglobulinand cytokeratin 7 and was negative for cytokeratin20, estrogen receptor, and progesteronereceptor. No nuclear staining with beta-cateninwas found.Patient 2. A 34-year-old woman with a history <strong>of</strong>FAP was found to have an enlarged <strong>thyroid</strong> glandon routine physical examination. In 1992, thepatient had undergone a proctocolectomy and excision<strong>of</strong> an abdominal wall desmoid tumor; desmoidsoccur in up to 10% <strong>of</strong> FAP patients and area manifestation <strong>of</strong> Gardner’s syndrome. 5 The desmoidwas also treated with adjuvant radiation. In1998, the desmoid tumor recurred in the pelvisand was treated with chemotherapy. In 1999, thepatient was diagnosed with duodenal tubularadenomas. Her paternal grandmother was the indexcase <strong>of</strong> FAP.Physical examination revealed a 2-cm, smoothdominant nodule <strong>of</strong> the right <strong>thyroid</strong> lobe andvague nodularity <strong>of</strong> the left <strong>thyroid</strong> lobe. Examination<strong>of</strong> the larynx revealed normal mobile vocalcords. Ultrasound demonstrated three nodules inthe right lobe and two smaller nodules in the leftFIGURE 1. The variegated histologic appearance <strong>of</strong> the <strong>cribriform</strong>-<strong>morular</strong> <strong>variant</strong>. This sporadic case (patient 1) displays <strong>cribriform</strong>(upper left), <strong>papillary</strong> (upper right), and hyalinized areas (lower left). Interspersed islands <strong>of</strong> squamoid and spindle cells (mainly spindlecells in this case) known as morules were also seen (delineated by the arrows; lower right). [Color figure can be viewed in the onlineissue, which is available at www.interscience.wiley.com.]472 Cribriform-Morular Variant <strong>of</strong> Papillary Cancer HEAD & NECK—DOI 10.1002/hed May 2006
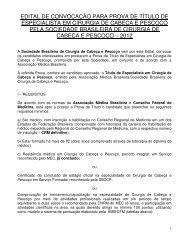
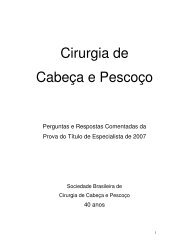
lobe. The most suspicious nodule was located inthe middle <strong>of</strong> the right <strong>thyroid</strong> lobe, had coarse,punctuate calcifications, and measured 1.6 cm indiameter. FNA cytology under ultrasonographicguidance strongly suggested PTC. The patientunderwent a total <strong>thyroid</strong>ectomy and had anuneventful postoperative recovery.The final pathology revealed a 2.3-cm PTClocated in the right <strong>thyroid</strong> lobe. The tumor wasdescribed as containing the ‘<strong>cribriform</strong>-<strong>morular</strong><strong>variant</strong>’ <strong>of</strong> PTC (Figure 2). Although the tumorwas well encapsulated and had no extra<strong>thyroid</strong>alextension, there was evidence <strong>of</strong> focal capsuleinvasion. No vascular invasion was identified. Ofinterest, the <strong>papillary</strong> <strong>carcinoma</strong> was multifocalwith three additional foci <strong>of</strong> the ‘<strong>cribriform</strong>-<strong>morular</strong><strong>variant</strong>’ ranging from 0.17 to 0.8 cm, located inboth <strong>thyroid</strong> lobes. The tumor was positive for thyroglobulinand cytokeratin 7 and was negative forcytokeratin 20. The tumor also showed diffuseaberrant nuclear staining for beta-catenin, whereasthe adjacent normal <strong>thyroid</strong> showed a membranousstaining pattern (Figure 3). In addition, there wasstrong and diffuse nuclear positivity for both estrogenand progesterone receptors.DISCUSSIONIn 1968, the relationship between FAP and <strong>thyroid</strong><strong>carcinoma</strong> was first suggested. 6 Although theincidence <strong>of</strong> PTC in patients with FAP is rare at1% to 2%, the relative risk for <strong>thyroid</strong> <strong>carcinoma</strong>in patients with FAP younger than 35 years <strong>of</strong> ageis estimated at 160 times that <strong>of</strong> the general population.2The <strong>cribriform</strong>-<strong>morular</strong> <strong>variant</strong> <strong>of</strong> <strong>papillary</strong>cancer <strong>of</strong> the <strong>thyroid</strong> is <strong>of</strong>ten associated with FAP,as was seen in our second patient. Clinically, thisentity has a female predominance, is multifocal,and tends to occur in patients under the age <strong>of</strong>30. 1,2,4,7–9 Histologically, this <strong>variant</strong> has beendescribed as having distinct features, includingan intricate blending <strong>of</strong> <strong>cribriform</strong>, trabecular,solid, follicular, <strong>morular</strong>, and <strong>papillary</strong> architecture.1,3,8 The uncharacteristic <strong>cribriform</strong> growthpattern can mislead the pathologist into diagnos-FIGURE 2. Histopathologic features <strong>of</strong> the <strong>cribriform</strong>-<strong>morular</strong> <strong>variant</strong> (CMV) in case 2. The tumor typically shows mixed architecturalfeatures with <strong>cribriform</strong> structures (upper left) and an intricate blending <strong>of</strong> empty follicles and papillae (upper right). Island <strong>of</strong> squamoidand spindle cells (morule delineated by arrows) shows the typical biotin-rich homogeneous nuclear inclusion also known as peculiarnuclear clearing (lower left). The nuclei are <strong>of</strong>ten pseudostratified and resemble those seen in <strong>papillary</strong> <strong>carcinoma</strong>, columnar cell <strong>variant</strong>,leading to the misdiagnosis <strong>of</strong> the latter <strong>variant</strong> that can be much more aggressive than CMV (lower right). [Color figure can beviewed in the online issue, which is available at www.interscience.wiley.com.]Cribriform-Morular Variant <strong>of</strong> Papillary Cancer HEAD & NECK—DOI 10.1002/hed May 2006 473
FIGURE 3. Immunostaining for beta-catenin. The <strong>cribriform</strong>-<strong>morular</strong> <strong>variant</strong> in case 2 shows aberrant nuclear and cytoplasmic staininginside and outside the morule, which is delineated by arrows (left). The adjacent normal <strong>thyroid</strong> shows membranous staining only(right). [Color figure can be viewed in the online issue, which is available at www.interscience.wiley.com.]ing more aggressive <strong>variant</strong>s <strong>of</strong> <strong>thyroid</strong> <strong>carcinoma</strong>s,such as poorly differentiated <strong>thyroid</strong> <strong>carcinoma</strong>.The <strong>cribriform</strong>-<strong>morular</strong> <strong>variant</strong> <strong>of</strong>ten showspseudostratified nuclei, leading to an erroneous diagnosis<strong>of</strong> columnar cell <strong>carcinoma</strong>, a potentiallyaggressive <strong>variant</strong> <strong>of</strong> PTC. The reverse is alsotrue, in the sense that hyalinized areas, a frequentoccurrence in the <strong>cribriform</strong>-<strong>morular</strong> <strong>variant</strong>, canpoint toward a diagnosis <strong>of</strong> hyalinizing trabeculartumor, a neoplasm with excellent prognosis (evenbetter than the <strong>cribriform</strong>-<strong>morular</strong> <strong>variant</strong>) if strictlydefined.The diagnosis <strong>of</strong> <strong>thyroid</strong> cancer can predatethe symptoms <strong>of</strong> colorectal polyposis by 4 to 12years in up to 30% <strong>of</strong> patients in some series. 8,10In one study <strong>of</strong> seven patients with the <strong>cribriform</strong><strong>morular</strong><strong>variant</strong> <strong>of</strong> PTC, two patients were foundto have polyposis; both tested positively for germlineadenomatous polyposis coli (APC) gene mutation,and both underwent subsequent colectomy. 2Because <strong>of</strong> the potential <strong>of</strong> detecting FAP early inpatients diagnosed with the <strong>cribriform</strong>-<strong>morular</strong><strong>variant</strong>, we strongly encouraged our first patientto undergo screening colonoscopy. Fortunately,colonoscopy ruled out the presence <strong>of</strong> colonicpolyposis. If screening can detect FAP, it is possibleto reduce the development <strong>of</strong> an individual’srisk <strong>of</strong> colorectal cancer.Immunohistochemically, these tumors stainpositively for estrogen and progesterone receptorsthat may correlate with the female predominancein the <strong>cribriform</strong>-<strong>morular</strong> <strong>variant</strong>. The tumorsalso stain well for thyroglobulin, cytokeratins AE1/AE3 and cytokeratin 7, and have also been shownto stain positively for cytokeratin 34betaE12,neuron-specific enolase, vimentin, bcl-2, and retinoblastomaprotein. 1,4,11 The tumor in our patientwith FAP stained for thyroglobulin and cytokeratin7 and was negative for cytokeratin 20, indicatingits lineage from the <strong>thyroid</strong> follicular epithelium.In PTC associated with FAP, genetic alterationsinclude germline APC mutations, 12 somaticmutations, 13 or loss <strong>of</strong> heterozygosity <strong>of</strong> the APCgene. 9,12,14 In addition to loss <strong>of</strong> function <strong>of</strong> theAPC gene, genetic alterations in FAP-associated<strong>thyroid</strong> cancer involve gain <strong>of</strong> function <strong>of</strong> the retproto-oncogene (ret/PTC). 15 In fact, two smallseries have shown a 80% to 100% frequency <strong>of</strong>ret/PTC rearrangement and activation <strong>of</strong> theret/PTC1 and ret/PTC3 is<strong>of</strong>orms in these patients. 7,15As seen in our first patient, the <strong>cribriform</strong><strong>morular</strong><strong>variant</strong> may be encountered in patientswith non-FAP. First described in 1999, the sporadic<strong>cribriform</strong>-<strong>morular</strong> <strong>variant</strong> <strong>of</strong> PTC tends tobe well circumscribed and solitary and also occursin women younger than 30. 16 Immunohistochemically,these tumors stain positively for thyroglobulin,as with our first patient, and for cytokeratins,vimentin, estrogen, and progesterone receptors,bcl2, and retinoblastoma protein. 16 In onestudy <strong>of</strong> seven patients diagnosed with the <strong>cribriform</strong>-<strong>morular</strong><strong>variant</strong>, four patients had no evidence<strong>of</strong> polyposis or APC gene mutation. 2 However,a somatic APC mutation was found in a474 Cribriform-Morular Variant <strong>of</strong> Papillary Cancer HEAD & NECK—DOI 10.1002/hed May 2006
patient without a germline APC mutation. 17 Thesepatients with the sporadic <strong>cribriform</strong>-<strong>morular</strong> <strong>variant</strong>have an excellent prognosis, with one reportdescribing no recurrence <strong>of</strong> tumor up to 13 yearsafter diagnosis. 16Mutant beta-catenin contributes to the development<strong>of</strong> the <strong>cribriform</strong>-<strong>morular</strong> <strong>variant</strong> <strong>of</strong> PTCin both FAP and sporadic forms. 11 APC forms amacromolecular complex with beta-catenin and isinvolved in the Wnt transduction signaling pathway,sequestering beta-catenin and targeting itfor degradation. 18,19 Mutations in the APC genelead to a truncated APC protein that lacks theability to degrade beta-catenin, leading to increasedcytoplasmic beta-catenin levels. 20 Cytoplasmicand nuclear immunolocalization <strong>of</strong> beta-cateninin FAP-associated <strong>cribriform</strong>-<strong>morular</strong> <strong>variant</strong> <strong>of</strong>PTC suggests an abnormality in the Wnt transductionsignaling pathway. 21 Xu et al 11 demonstratedsomatic mutations in the beta-catenin geneCTNNB1 in patients with either FAP-associatedor sporadic <strong>cribriform</strong>-<strong>morular</strong> <strong>variant</strong> <strong>of</strong> PTC.Cytoplasmic and nuclear immunolocalization <strong>of</strong>beta-catenin was noted in both sets <strong>of</strong> patients,suggesting that the aberrant nuclear accumulation<strong>of</strong> mutant beta-catenin can occur independentlyfrom APC mutations and may contribute tothe genesis <strong>of</strong> these tumors. 11 Beta-catenin alsoseems to be responsible for the peculiar morphology(i.e., <strong>cribriform</strong> growth and morules) seen inthese tumors. Indeed, beta-catenin accumulationhas also been found in ex-tra<strong>thyroid</strong>al neoplasmsdisplaying morules and intricate glandular growthpatterns, such as fetal lung adeno<strong>carcinoma</strong> andendometrioid-type adeno<strong>carcinoma</strong> <strong>of</strong> the endometrium.22Also, supporting a role in the morphogenesis <strong>of</strong>the <strong>cribriform</strong>-<strong>morular</strong> <strong>variant</strong> is the fact thatbeta-catenin nuclear/cytoplasmic accumulationis critical in the epithelial budding, branching,and hair follicle formation in embryogenesis. The<strong>cribriform</strong> pattern may, therefore, recapitulatethe epithelial budding seen in embryos, and themorules may recapitulate the hair formation seenin embryogenesis. 22In our patient with FAP, we found aberrantaccumulation <strong>of</strong> beta-catenin in the tumor nuclei,in agreement with previous reports. However,the tumor in our sporadic case did not show betacateninnuclear or cytoplasmic staining, and therewas no estrogen or progesterone immunoreactivity.These findings suggest alternative pathways(other than beta-catenin) may be responsible forthe formation <strong>of</strong> these neoplasms.Because <strong>of</strong> their multicentricity and bilaterality,total <strong>thyroid</strong>ectomy is the treatment <strong>of</strong> choice forthe <strong>cribriform</strong>-<strong>morular</strong> <strong>variant</strong> <strong>of</strong> PTC. 1 Althoughthe tumor in our patient with non-FAP did notreveal multicentricity, the tumor <strong>of</strong> the patientwith FAP did demonstrate multicentricity, supportingthe argument for total <strong>thyroid</strong>ectomy inthese patients. These tumors may metastasize toregional lymph nodes. Long-term prognosis isexcellent for patients with FAP-associated <strong>cribriform</strong>-<strong>morular</strong><strong>variant</strong>, with 5-year and 20-yearsurvival rates <strong>of</strong> 90% and 77%, respectively. 1CONCLUSIONSThe <strong>cribriform</strong>-<strong>morular</strong> <strong>variant</strong> <strong>of</strong> <strong>papillary</strong> <strong>thyroid</strong>cancer may be associated with familial adenomatouspolyposis. Patients with FAP in whomthere is a concern for PTC should undergo total<strong>thyroid</strong>ectomy. Although rare, when the <strong>cribriform</strong>-<strong>morular</strong><strong>variant</strong> is diagnosed, patients shouldundergo screening colonoscopy to rule out thepresence <strong>of</strong> colonic polyposis. The prognosis <strong>of</strong> this<strong>variant</strong> <strong>of</strong> PTC is similar to that <strong>of</strong> the classicaltype. This distinct histologic finding should alertphysicians to screen such patients and their familymembers for FAP, thereby facilitating early diagnosis<strong>of</strong> FAP.REFERENCES1. Perrier ND, van Heerden JA, Goellner JR, et al. Thyroidcancer in patients with familial adenomatous polyposis.World J Surg 1998;22:738–742.2. Tomoda C, Miyauchi A, Uruno T, et al. Cribriform-<strong>morular</strong><strong>variant</strong> <strong>of</strong> <strong>papillary</strong> <strong>thyroid</strong> <strong>carcinoma</strong>: clue to earlydetection <strong>of</strong> familial adenomatous polyposis-associatedcolon cancer. World J Surg 2004;28:886–839.3. Harach HR, Williams GT, Williams ED. Familial adenomatouspolyposis associated <strong>thyroid</strong> <strong>carcinoma</strong>: a distincttype <strong>of</strong> follicular cell neoplasm. Histopathology 1994;25:549–561.4. Ng SB, Sittampalam K, Goh YH, Eu KW. Cribriform<strong>morular</strong><strong>variant</strong> <strong>of</strong> <strong>papillary</strong> <strong>carcinoma</strong>: the sporadic counterpart<strong>of</strong> familial adenomatous polyposis-associated <strong>thyroid</strong><strong>carcinoma</strong>. A case report with clinical and moleculargenetic correlation. Pathology 2003;35:42–46.5. Clark SK, Phillips RK. Desmoids in familial adenomatouspolyposis. Br J Surg 1996;83:1494–1504.6. Camiel MR, Mule JE, Alexander LL, Benningh<strong>of</strong>f DL.Association <strong>of</strong> <strong>thyroid</strong> <strong>carcinoma</strong> with Gardner’s syndromein siblings. N Engl J Med 1968;278:1056–1058.7. Cetta F, Chiappetta G, Melillo RM, et al. The ret/ptc1oncogene is activated in familial adenomatous polyposisassociated<strong>thyroid</strong> <strong>papillary</strong> <strong>carcinoma</strong>s. J Clin EndocrinolMetab 1998;83:1003–1006.8. Cetta F, Pelizzo MR, Curia MC, Barbarisi A. Geneticsand clinicopathological findings in <strong>thyroid</strong> <strong>carcinoma</strong>s associatedwith familial adenomatous polyposis. Am J Pathol1999;155:7–9.Cribriform-Morular Variant <strong>of</strong> Papillary Cancer HEAD & NECK—DOI 10.1002/hed May 2006 475
9. Cetta F, Montalto G, Gori M, Curia MC, Cama A,Olschwang S. Germline mutations <strong>of</strong> the APC gene inpatients with familial adenomatous polyposis-associated<strong>thyroid</strong> <strong>carcinoma</strong>: results from a European cooperativestudy. J Clin Endocrinol Metab 2000;85:286–292.10. Plail RO, Bussey HJ, Glazer G, Thomson JP. Adenomatouspolyposis: an association with <strong>carcinoma</strong> <strong>of</strong> the <strong>thyroid</strong>.Br J Surg 1987;74:377–380.11. Xu B, Yoshimoto K, Miyauchi A, et al. Cribriform-<strong>morular</strong><strong>variant</strong> <strong>of</strong> <strong>papillary</strong> <strong>thyroid</strong> <strong>carcinoma</strong>: a pathologicaland molecular genetic study with evidence <strong>of</strong> frequentsomatic mutations in exon 3 <strong>of</strong> the beta-catenin gene.J Pathol 2003;199:58–67.12. Truta B, Allen BA, Conrad PG, et al. Genotype and phenotype<strong>of</strong> patients with both familial adenomatous polyposisand <strong>thyroid</strong> <strong>carcinoma</strong>. Fam Cancer 2003;2:95–99.13. Miyaki M, Iijima T, Ishii R, et al. Molecular evidence formulticentric development <strong>of</strong> <strong>thyroid</strong> <strong>carcinoma</strong>s in patientswith familial adenomatous polyposis. Am J Pathol 2000;157:1825–1827.14. Kameyama K, Mukai M, Takami H, Ito K. Cribriform-<strong>morular</strong><strong>variant</strong> <strong>of</strong> <strong>papillary</strong> <strong>thyroid</strong> <strong>carcinoma</strong>:ultra-structural study and somatic/germline mutationanalysis <strong>of</strong> the APC gene. Ultrastruct Pathol 2004;28:97–102.15. Soravia C, Sugg SL, Berk T, et al. Familial adenomatouspolyposis-associated <strong>thyroid</strong> cancer: a clinical, pathological,and molecular genetics study. Am J Pathol 1999;154:127–135.16. Cameselle-Teijeiro J, Chan JK. Cribriform-<strong>morular</strong> <strong>variant</strong><strong>of</strong> <strong>papillary</strong> <strong>carcinoma</strong>: a distinctive <strong>variant</strong> representingthe sporadic counterpart <strong>of</strong> familial adenomatouspolyposis-associated <strong>thyroid</strong> <strong>carcinoma</strong>? Mod Pathol 1999;12:400–411.17. Cameselle-Teijeiro J, Ruiz-Ponte C, Loidi L, Suarez-Penaranda J, Baltar J, Sobrinho-Simoes M. Somatic butnot germline mutation <strong>of</strong> the APC gene in a case <strong>of</strong><strong>cribriform</strong>-<strong>morular</strong> <strong>variant</strong> <strong>of</strong> <strong>papillary</strong> <strong>thyroid</strong> <strong>carcinoma</strong>.Am J Clin Pathol 2001;115:486–493.18. Barth AI, Nathke IS, Nelson WJ. Cadherins, cateninsand APC protein: interplay between cytoskeletal complexesand signaling pathways. Curr Opin Cell Biol 1997;9:683–690.19. Rubinfeld B, Albert I, Porfiri E, Fiol C, Munemitsu S, PolakisP. Binding <strong>of</strong> GSK3beta to the APC-beta-catenin complexand regulation <strong>of</strong> complex assembly. Science 1996;272:1023–1026.20. Peifer M. Beta-catenin as oncogene: the smoking gun.Science 1997;275:1752–1753.21. Kurihara K, Shimizu S, Chong J, et al. Nuclear localization<strong>of</strong> immunoreactive beta-catenin is specific to familialadenomatous polyposis in <strong>papillary</strong> <strong>thyroid</strong> <strong>carcinoma</strong>.Jpn J Cancer Res 2000;91:1100–1102.22. Nakatani Y, Masudo K, Nozawa A, et al. Biotin-rich, opticallyclear nuclei express estrogen receptor-beta: tumorswith morules may develop under the influence <strong>of</strong> estrogenand aberrant beta-catenin expression. Hum Pathol 2004;35:869–874.476 Cribriform-Morular Variant <strong>of</strong> Papillary Cancer HEAD & NECK—DOI 10.1002/hed May 2006