Keratoconus A clinical update - David Thomas Contact Lenses
Keratoconus A clinical update - David Thomas Contact Lenses
Keratoconus A clinical update - David Thomas Contact Lenses
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
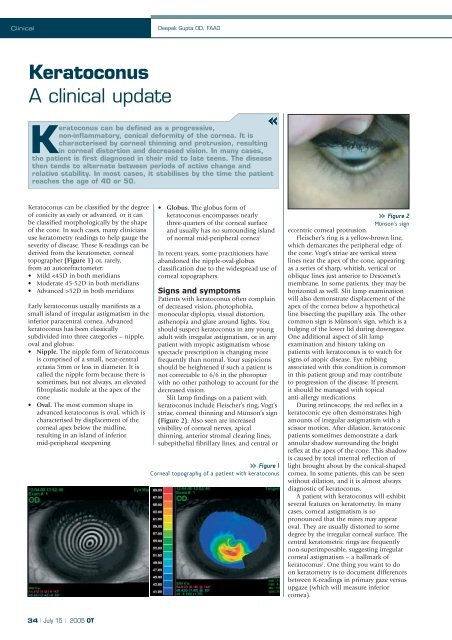
ClinicalDeepak Gupta OD, FAAO<strong>Keratoconus</strong>A <strong>clinical</strong> <strong>update</strong><strong>Keratoconus</strong> can be defined as a progressive,non-inflammatory, conical deformity of the cornea. It ischaracterised by corneal thinning and protrusion, resultingin corneal distortion and decreased vision. In many cases,the patient is first diagnosed in their mid to late teens. The diseasethen tends to alternate between periods of active change andrelative stability. In most cases, it stabilises by the time the patientreaches the age of 40 or 50.<strong>Keratoconus</strong> can be classified by the degreeof conicity as early or advanced, or it canbe classified morphologically by the shapeof the cone. In such cases, many cliniciansuse keratometry readings to help gauge theseverity of disease. These K-readings can bederived from the keratometer, cornealtopographer (Figure 1) or, rarely,from an autorefractometer:• Mild 52D in both meridiansEarly keratoconus usually manifests as asmall island of irregular astigmatism in theinferior paracentral cornea. Advancedkeratoconus has been classicallysubdivided into three categories – nipple,oval and globus:• Nipple. The nipple form of keratoconusis comprised of a small, near-centralectasia 5mm or less in diameter. It iscalled the nipple form because there issometimes, but not always, an elevatedfibroplastic nodule at the apex of thecone• Oval. The most common shape inadvanced keratoconus is oval, which ischaracterised by displacement of thecorneal apex below the midline,resulting in an island of inferiormid-peripheral steepening• Globus. The globus form ofkeratoconus encompasses nearlythree-quarters of the corneal surfaceand usually has no surrounding islandof normal mid-peripheral cornea 1In recent years, some practitioners haveabandoned the nipple-oval-globusclassification due to the widespread use ofcorneal topographers.Signs and symptomsPatients with keratoconus often complainof decreased vision, photophobia,monocular diplopia, visual distortion,asthenopia and glare around lights. Youshould suspect keratoconus in any youngadult with irregular astigmatism, or in anypatient with myopic astigmatism whosespectacle prescription is changing morefrequently than normal. Your suspicionsshould be heightened if such a patient isnot correctable to 6/6 in the phoropterwith no other pathology to account for thedecreased vision.Slit lamp findings on a patient withkeratoconus include Fleischer’s ring, Vogt’sstriae, corneal thinning and Münson’s sign(Figure 2). Also seen are increasedvisibility of corneal nerves, apicalthinning, anterior stromal clearing lines,subepithelial fibrillary lines, and central orFigure 1Corneal topography of a patient with keratoconusFigure 2Münson’s signeccentric corneal protrusion.Fleischer’s ring is a yellow-brown line,which demarcates the peripheral edge ofthe cone. Vogt’s striae are vertical stresslines near the apex of the cone, appearingas a series of sharp, whitish, vertical oroblique lines just anterior to Descemet’smembrane. In some patients, they may behorizontal as well. Slit lamp examinationwill also demonstrate displacement of theapex of the cornea below a hypotheticalline bisecting the pupillary axis. The othercommon sign is Münson’s sign, which is abulging of the lower lid during downgaze.One additional aspect of slit lampexamination and history taking onpatients with keratoconus is to watch forsigns of atopic disease. Eye rubbingassociated with this condition is commonin this patient group and may contributeto progression of the disease. If present,it should be managed with topicalanti-allergy medications.During retinoscopy, the red reflex in akeratoconic eye often demonstrates highamounts of irregular astigmatism with ascissor motion. After dilation, keratoconicpatients sometimes demonstrate a darkannular shadow surrounding the brightreflex at the apex of the cone. This shadowis caused by total internal reflection oflight brought about by the conical-shapedcornea. In some patients, this can be seenwithout dilation, and it is almost alwaysdiagnostic of keratoconus.A patient with keratoconus will exhibitseveral features on keratometry. In manycases, corneal astigmatism is sopronounced that the mires may appearoval. They are usually distorted to somedegree by the irregular corneal surface. Thecentral keratometric rings are frequentlynon-superimposable, suggesting irregularcorneal astigmatism – a hallmark ofkeratoconus 2 . One thing you want to doon keratometry is to document differencesbetween K-readings in primary gaze versusupgaze (which will measure inferiorcornea).34 | July 15 | 2005 OT
ClinicalOn corneal topography, earlykeratoconus reveals a characteristic pearshapedelongation of the central mires atthe mid-periphery, below the cornealmidline. As the condition progresses, thesteepening usually spreads nasally toinclude the inferonasal cornea. Advancedkeratoconus can demonstrate rotationalsteepening above the midline along asuperotemporal path. The last area to beaffected by keratoconus is usually thesuperior nasal quadrant of the cornea 1 .However, there is some variability in thispresentation. Some practitioners may findthat the apex of the cone is decenteredbelow the midline and temporal.Treatment optionsTreatment of keratoconus depends on theseverity of the condition. Early in thedisease, spectacles are successful inrestoring vision. However, as the diseaseprogresses, the patient will need contactlenses to provide optimal visual acuity.Lens options include soft (hydrogel)lenses, basic rigid gas permeable lenses,and specialty gas permeable lenses.• Soft lenses. Unlike rigid gaspermeable lenses, which help mask someof the corneal irregularity of keratoconus,soft lenses tend to drape over the cornea.Hence, soft lenses are used only in theearly stages of the disease. In such cases,the lenses are usually toric, and are fittedin the same manner as they would be on apatient with myopic astigmatism. With theadvent of made-to-order, high toric,planned replacement lenses and custommadeprecision of lenses, many morepatients do well with soft lenses.One criterion to use to determine if softlenses are acceptable is that they shouldinduce no scarring. Often, soft contactlenses lead to repeated corneal abrasions,which can result in scarring. Anothercriterion is if the patient is happy withtheir vision and is able to functionproperly in their daily activities.• RGP lenses. When soft lenses nolonger work, early keratoconic patientsmay achieve adequate acuity with largediameter RGP lenses or aspheric lensdesigns. Often, the large diameter isneeded to achieve sufficient centration andto obtain a good fit. Since keratoconuspatients often wear their contacts all day, itis important to use lenses with highoxygen permeability, which minimise therisk of neovascularisation. The other majorconcern is wettability. More advancedcases may require a lens designedspecifically for keratoconus.• Piggyback lenses. If a keratoconicpatient is intolerant to rigid lenses, a rigidlens fitted over a hydrogel lens issometimes a viable option. This concept isreferred to as a ‘piggyback’ fit and workswell for many patients. The patient isinitially fitted with a large diameter softlens with proper centration andmovement. Then keratometry readings aretaken of the ‘new’ corneal surface, and aRGP lens is fitted over the top of the softlens. Because the patient is wearing twolenses simultaneously, it is even morecrucial to make sure both lens materialsare highly oxygen permeable. There are afew soft lens designs for keratoconus, butthey may have less oxygen transmission.Many practitioners also find that theselenses demonstrate a tight fit.• Surgery. Once all contact lens optionshave been exhausted, surgery may beneeded to obtain adequate vision. Themost common surgical option is apenetrating keratoplasty 3 . Another optionis Intacs, which can be implanted toenhance the stability of the cornea andachieve a more stable fit. Although thisprocedure failed as a refractive surgeryoption, it has been shown to help orprevent the need for a corneal transplant inmany patients with keratoconus.One relatively experimental procedure,which is available only in Europe andMexico, is C3-R, which is collagen crosslinkingwith riboflavin. In many patients, itis combined with Intacs. Basically, itfeatures the instillation of the eyedrops,followed by UV light for 30 minutes. Thepremise is that it halts the progression ofkeratoconus by helping the cornea increasein thickness. Although initial studies lookpromising, it is still very experimental.To qualify for surgery, patients’ visionshould be poor enough to interfere withtheir ability to work or drive. Like cataractsurgery, there is no magic number at whichthe keratoconic patient needs to undergo acorneal transplant. Often the decision toproceed to surgery is based on the patient’sperception of his or her vision. Onepatient may find that they cannot do theirjob with 6/9 acuity, while another patientmay be very satisfied with their 6/18vision.If a patient has a very large area ofthinning toward the peripheral cornea, if astable contact lens fit is no longer possible,or if the patient has significant cornealneovascularisation, surgery may beperformed earlier than otherwise indicatedby visual performance alone.<strong>Contact</strong> lens fitsThree of the more common gas permeablekeratoconus fitting sets are the Soper Cone,McGuire and Rose K. What follows is abrief discussion of these sets and asummary of a suggested fitting process.The principles discussed can be appliedto any fitting set. There are a few soft lensdesigns to manage keratoconus, but theymay not all allow enough oxygen to thecornea and lack the clarity of visionprovided by RGPs. Because keratoconuspatients may need a corneal transplant inthe future, avoid lenses that might inducecorneal neovascularisation because thiscondition increases susceptibility to graftrejection.• Soper Cone. This a bicurve contactlens with a fitting approach based onsagittal depth. In this lens design, thevaulting effect of the lens increases as thebase curve decreases for a given diameter.This change in the steep central posteriorcurvature is used to fit the cone. Thisdesign is based on the notion of avoidingthe apical bearing that will ultimately leadto corneal scarring in keratoconus patients.The Soper design consists of 10 lenses,designated by the letters A to H. There arethree groups for a given diameter/opticzone relationship 4 . A, B, C and D aredesigned for mild keratoconus orK-readings of less than 48.00D in eithercorneal meridian. E, F and G are formoderate keratoconus or K-readings of48.00D to 54.00D in either cornealmeridian. H, I and J are for the advancedstage or K-readings of 54.00D or greater 3 .• McGuire. This keratoconic lenssystem was introduced in 1978 and is amodification of the Soper design 4 .It consists of three diagnostic lens sets,each formulated for the nipple, oval orglobus type of keratoconus. The fittingstrategy is aimed at achieving a three-pointtouch predicated upon the size of opticzone in relation to conical size. In thisdesign, the optical zone sizes are variedfrom 6mm for the nipple cone to 6.5mmfor the oval cone and 7mm for the globus.Each lens also incorporates a series of fourperipheral curves, which are blendedtogether to create an almost asphericrelationship. The secondary curve of theMcGuire system is 0.5mm flatter than thecentral base curve. The third curve is 1mmflatter than the secondary curve. The fourthand final peripheral curve is 2mm flatterthan the tertiary curve 4 .• Rose K. This is a lens design withcomplex, computer-generated peripheralcurves based on data collected by Dr PaulRose of Hamilton, New Zealand. In orderto achieve the ideal edge lift of 0.8mm, thelens incorporates three peripheral systems:standard, flat and steep. It is available inbase curves of 4.75-8mm and diameters of7.9-10.2mm. The design works bydecreasing the optic zone diameter as thebase curve becomes steeper. Toric curvesare available on both the front and backsurface, as well as peripherally, but they arerarely needed.Rose K lenses are traditionally made inthe Boston ES material, but they can bemade in the Boston EO material, whichprovides the added benefit of increasedoxygen permeability. The Rose Kmanufacturing process features a uniquesoftware program to help cut and blendthe multiple curves, which makesreplacement lenses easy to reproduce.The newest version of this lens, theRose K 2, incorporates a sophisticatedparabolic section on the posterior surfaceto counteract spherical aberration.Spherical aberrations occur because thefocal points of light rays far from the35 | July 15 | 2005 OT
ClinicalDeepak Gupta OD, FAAOprincipal axis in a spherical lens aredifferent from the focal points of rays thatpass through the centre of the axis. Inkeratoconus, this is exaggerated further inthe steep radius of curvatures. The rays oflight passing through the edge of the lensbend more and focus slightly in front ofthose passing through the centre. Thespherical aberration is counteracted byvarying amounts of eccentricity across theback optic zone diameter. The fittingregimen for these lenses is the same as forRose K. It remains to be seen how this lensperforms over time, to gauge how much ofan improvement it is over the originalversion.Fitting protocolOne of the most important things to dowhen starting a keratoconus fit is toidentify the morphological shape of thecone, and thus determine the stage of thecondition. Shape is easily assessed whenviewing the cornea with retro-illuminationafter dilation. The stage of the conditioncan be assessed by examining K-readings.If the mean K is less than 50.00D, thecone can be considered early stage. Amean K-reading from 50.00D to 55.00D isadvanced, and one of greater than 55.00Dis severe. Alternatively, one can usesimulated K-readings derived from atopographer.For any new fit, instill a drop ofanaesthetic in each eye prior to lensinsertion. Otherwise, patients tearexcessively, causing the lens to sit low andthe eye to yield abnormal fluoresceinpatterns. Apply the lens and let the patientsit in the waiting room for at least 20minutes before evaluating the fluoresceinpattern. As with all other lenses, look atthe central area, the mid-peripheral areaand the periphery. Be sure that the lens islocated centrally when evaluating it. If thelens lags down, use upward pressure onthe lower lid to improve centration whenjudging fit. If you can demonstrate a goodfit, you can often improve centration byincreasing lens diameter.In determining the correct base curve,start with one equivalent to the steeper ofthe two K-readings. Remember that themires are often irregular in keratoconus, sothe K-reading may provide only a roughgauge of the trial lens. Once the fit of thelens has been assessed (it should be toosteep), continue to flatten the base curveuntil you get the slightest amount ofapical touch. If you have a difficult timediscerning where the apex of the cone is,then the lens is too steep. The patient isgenerally most comfortable, and willattain the best acuity, when the weightbearingforces of the contact lens aredistributed evenly on the cornea – the socalledthree-point touch (Figure 3). Thismeans that there should be minimalbearing (touch) at the apex of the cone, aswell as an area of bearing between theperiphery of the lens and the intermediatezone of the cornea. By making sure thering of touch is incomplete, you permitfreshly oxygenated tears to the centralcornea when the patient blinks. By makingsure the bearing is minimal at the apex ofthe cone, you will decrease the risk ofscarring the cornea.When selecting an optic zone diameter,measure the pupil in average illuminationand add 1mm or 2mm. At the same time,make sure the optic zone fully covers thecone. If the cone is large and eccentric, itmay be necessary to utilise a larger opticzone than you would based solely onpupil size but, in most cases, accountingfor the pupil will cover both. If you do notfully cover the pupil, your patient willreturn complaining of decreased vision orglare and halos around lights. This willtypically result in an optic zone diameterof roughly 7-8 mm. However, be awarethat using one of the proprietary designsoften precludes the option of adjusting theoptic zone diameter.The trial lenses for the Rose K fitting setcome in an 8.7mm diameter, which worksfor most patients. When evaluatingdiameter, the upper edge of the lensshould hit the tarsal plate of the upper lid.If it does not, measure from the top of thelens to the bottom of the upper lid, andadd that number to the overall lensdiameter of the lens.When doing the over-refraction, startCentral bearingFigure 3Example of a three-point touchwith 1.00D steps initially, and then refinewith 0.50D and 0.25D increments as youget closer to the final prescription. Performthe final over-refraction in normalillumination to approximate normal lightconditions and pupil size. If you find youcannot obtain adequate vision with aspherical over-refraction, try aspherocylindrical. If a toric lens is ordered,the lens will be made 0.3mm larger thanthe diagnostic lens, and then a 0.3mmtruncation is employed with 1 1 /4 prismballast to stabilise the lens. These toricRose K lenses are not to be confused withbitoric RGPs, which are generallycontraindicated in keratoconus.The criteria for a successful keratoconiclens fit are no different than for a standardfit. The lens needs to be comfortableenough to wear all day long, and thevision and post-wear biomicroscopy needsto be acceptable. The only difference isthat acuity for the keratoconic patient maynot be 6/6, even with contact lenses, butthat is not a problem if the vision issatisfactory for the patient’s needs.All keratoconic patients should returnfor follow-up at least every six months.Examine corneal surface integrity, evaluatelens fit, and look for changes in cornealtopography. Remind them thatkeratoconus is a progressive disorder, andthere is no way to predict when and if itwill start to progress again. Also informthem they should schedule an officeappointment immediately if theyexperience decreased vision, photophobia,decreased lens comfort, decreased lenswearing time, increased difficulty insertingor removing the lenses, or any similarsymptoms. Such problems may indicatechanges in the cornea that should beevaluated as soon as possible.Common fitting problemsOne of the most common errors incontact lens management of keratoconusis fitting too tight. The CLEK study 6 foundthat the most common error was fittingexcessively flat. Your goal should be toachieve a good stable fit, while allowingfor enough movement to provideFeather touch5.75/8.7/1.0 Flat 5.65/8.7/1.0 FlatFigure 4Central bearing and feather touch36 | July 15 | 2005 OT
Clinicaladequate tear exchange. Otherwise, poortear exchange leads to poor oxygentransmission to the cornea. Poor tearexchange also leads to a pooling ofmetabolic debris underneath the opticzone, which often shows up as dimpleveiling and stipple staining around thebase of the cone. This problem can bealleviated by decreasing the optic zonediameter, by flattening the existingsecondary or peripheral curves, or byblending the junctions between theperipheral curves 5 . Conversely, a lens fittedtoo flat will move excessively and creatediscomfort. This can be fixed bysteepening the base curve or the peripheralcurves, which will decrease lensmovement.If you see coalesced staining of the apexof the cone, it is usually due to one of tworeasons – the lens is too flat or there areexcessive deposits on the posterior lenssurface. Apical staining may ultimatelylead to corneal scarring, so this should notbe permitted. If the fit is too flat, it shouldbe steepened. If the fit looks stable, havethe patient remove the lens and observethe lens alone in the slit lamp 5 . If thedeposits are heavy, advise the patient tostart a new lens and begin aggressiveenzyming and a rigorous daily cleaningschedule. In some cases, it may benecessary for patients to enzyme as oftenas once or twice a week to keep depositsdown.Sometimes you will see small bubblesunder the lens, which indicates a steep fit.This can usually be solved by flatteningthe base curve until you get the slightestapical touch, increasing the edge lift, orreducing the diameter/optic zone of thelens. If the bubbles persist, the lens can befenestrated at the juncture of the opticzone and the secondary curve.Fenestration is not something that shouldroutinely be ordered on a lens, but it is aviable last resort.If the lens is riding too low, centrationcan be improved by increasing thediameter or steepening the base curve. Ifyou decide to change the diameter, thechanges must be at least 0.3mm in mostcases to see a <strong>clinical</strong> difference. If you seesuperior limbal staining or three and nineo’clock staining, reduce the diameterand/or increase edge lift.ConclusionAlthough the standard treatment ofkeratoconus involves contact lens fitting,encourage patients to use spectacles for aslong as possible. Particularly in the earlystages of keratoconus, there is no need tohurry patients into contact lenses if theyare happy with their vision.A patient who has never worn ‘hard’lenses before must be highly motivated toget through the adaptation period ofRGPs. The best way to attain thismotivation is to keep the patient inspectacles long enough so that they willnotice the greatly improved visionobtained with RGP lenses. If the patient isrushed into RGPs and they fail to notice adramatic improvement, they may not beso willing to continue.Before referring a patient for surgery,rethink your fitting strategy or send thepatient to a colleague for a fresh approach.The vast majority of patients sent forsurgery are denied that procedure andmanaged optically.References1. Caroline P, Andre M and Norman C(1997) Corneal topography inkeratoconus. <strong>Contact</strong> Lens Spectrum12 (7): 36.2. Nordan LT (1997) <strong>Keratoconus</strong>:diagnosis and treatment. InternationalOphthalmology Clinics 37 (11): 51-63.3. Cannella A (1994) Use of contactlenses in the visual correction ofkeratoconus. Out of print.4. Cutler SI (1999) Managing keratoconuswith proprietary designs. <strong>Contact</strong> LensSpectrum 14 (10): 21.5. Edrington TB, Timothy B (1998)<strong>Keratoconus</strong> problem solving.<strong>Contact</strong> Lens Spectrum 13 (3): 18.6. Zadnik K et al (1998) CollaborativeLongitudinal Evaluation of <strong>Keratoconus</strong>(CLEK) Study group. Baseline findingsin the CLEK study. Invest. Ophthalmol.Vis. Sci. 39: 2537-46.About the authorDeepak Gupta is the Clinical Director for the Center for <strong>Keratoconus</strong> at Stamford Ophthalmology, Stamford, USA.37 | July 15 | 2005 OT