IMAGING & ONCOLOGY - Society of Radiographers
IMAGING & ONCOLOGY - Society of Radiographers
IMAGING & ONCOLOGY - Society of Radiographers
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
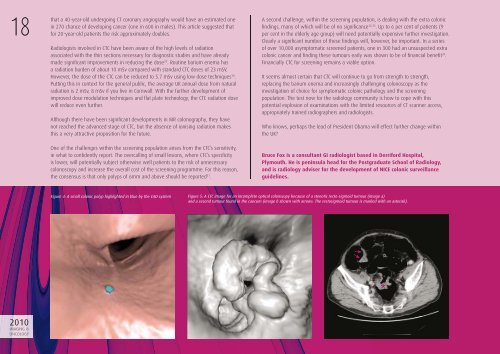
18that a 40-year-old undergoing CT coronary angiography would have an estimated onein 270 chance <strong>of</strong> developing cancer (one in 600 in males). This article suggested thatfor 20-year-old patients the risk approximately doubles.Radiologists involved in CTC have been aware <strong>of</strong> the high levels <strong>of</strong> radiationassociated with the thin sections necessary for diagnostic studies and have alreadymade signifi cant improvements in reducing the dose 29 . Routine barium enema hasa radiation burden <strong>of</strong> about 10 mSv compared with standard CTC doses <strong>of</strong> 23 mSV.However, the dose <strong>of</strong> the CTC can be reduced to 5.7 mSv using low dose techniques 30 .Putting this in context for the general public, the average UK annual dose from naturalradiation is 2 mSv, 8 mSv if you live in Cornwall. With the further development <strong>of</strong>improved dose modulation techniques and fl at plate technology, the CTC radiation dosewill reduce even further.Although there have been signifi cant developments in MR colonography, they havenot reached the advanced stage <strong>of</strong> CTC, but the absence <strong>of</strong> ionising radiation makesthis a very attractive proposition for the future.One <strong>of</strong> the challenges within the screening population arises from the CTC’s sensitivity,ie what to confi dently report. The overcalling <strong>of</strong> small lesions, where CTC’s specifi cityis lower, will potentially subject otherwise well patients to the risk <strong>of</strong> unnecessarycolonoscopy and increase the overall cost <strong>of</strong> the screening programme. For this reason,the consensus is that only polyps <strong>of</strong> 6mm and above should be reported 31 .A second challenge, within the screening population, is dealing with the extra colonicfi ndings, many <strong>of</strong> which will be <strong>of</strong> no signifi cance 32,33 . Up to 6 per cent <strong>of</strong> patients (9per cent in the elderly age group) will need potentially expensive further investigation.Clearly a signifi cant number <strong>of</strong> these fi ndings will, however, be important. In a series<strong>of</strong> over 10,000 asymptomatic screened patients, one in 300 had an unsuspected extracolonic cancer and fi nding these tumours early was shown to be <strong>of</strong> fi nancial benefi t 34 .Financially CTC for screening remains a viable option.It seems almost certain that CTC will continue to go from strength to strength,replacing the barium enema and increasingly challenging colonoscopy as theinvestigation <strong>of</strong> choice for symptomatic colonic pathology and the screeningpopulation. The test now for the radiology community is how to cope with thispotential explosion <strong>of</strong> examinations with the limited resources <strong>of</strong> CT scanner access,appropriately trained radiographers and radiologists.Who knows, perhaps the lead <strong>of</strong> President Obama will effect further change withinthe UK?Bruce Fox is a consultant GI radiologist based in Derriford Hospital,Plymouth. He is peninsula head for the Postgraduate School <strong>of</strong> Radiology,and is radiology adviser for the development <strong>of</strong> NICE colonic surveillanceguidelines.Figure 4: A small colonic polyp highlighted in blue by the CAD system Figure 5: A CTC image for an incomplete optical colonscopy because <strong>of</strong> a stenotic recto-sigmoid tumour (image a)and a second tumour found in the caecum (image b shown with arrows. The rectosigmoid tumour is marked with an asterisk).2010<strong>IMAGING</strong> &<strong>ONCOLOGY</strong>