Investigations for Coeliac Disease
Investigations for Coeliac Disease
Investigations for Coeliac Disease
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
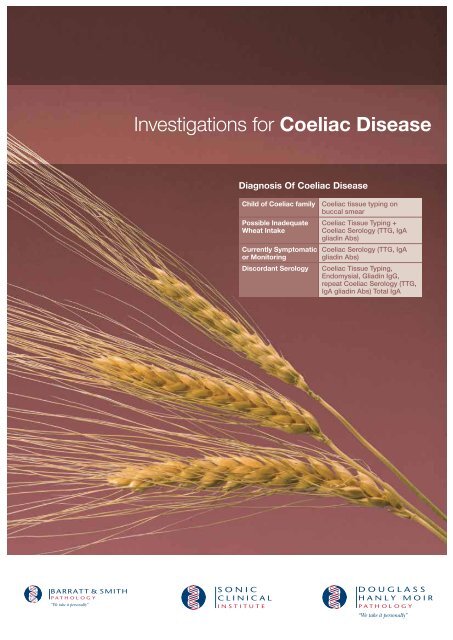
<strong>Investigations</strong> <strong>for</strong> <strong>Coeliac</strong> <strong>Disease</strong>Diagnosis Of <strong>Coeliac</strong> <strong>Disease</strong>Child of <strong>Coeliac</strong> family <strong>Coeliac</strong> tissue typing onbuccal smearPossible InadequateWheat IntakeCurrently Symptomaticor MonitoringDiscordant Serology<strong>Coeliac</strong> Tissue Typing +<strong>Coeliac</strong> Serology (TTG, IgAgliadin Abs)<strong>Coeliac</strong> Serology (TTG, IgAgliadin Abs)<strong>Coeliac</strong> Tissue Typing,Endomysial, Gliadin IgG,repeat <strong>Coeliac</strong> Serology (TTG,IgA gliadin Abs) Total IgA
<strong>Investigations</strong> <strong>for</strong> <strong>Coeliac</strong> <strong>Disease</strong>The modern discovery of coeliac disease or glutensensitiveenteropathy followed wartime observations thatsome chronically unwell children improved with wheatdeprivation and then deteriorated with improved foodsupplies including wheat. The enteropathy is characterisedby small intestinal lesions of variable severity which areprovoked in genetically susceptible individuals by ingestionof gluten. Additional external trigger factors appear to benecessary. Almost all persons with coeliac disease haveimmune system genes (tissue types) coding <strong>for</strong> HLA-DQ2or HLA-DQ8. The identification of these genotypes asbeing necessary permissive factors <strong>for</strong> coeliac diseasehas helped the development of additional strategies inthe investigation of patients who have, or are at risk ofdeveloping, coeliac disease.A variety of autoantibody tests have been developedto facilitate the diagnosis of coeliac disease which isconfirmed by small bowel biopsy. Tissue transglutaminase(TTG) has recently been identified as the main, if notsole, autoantigen in coeliac disease. This enzyme ispresent in many different cell types, mainly in intracellularcompartments. Tissue injury results in release of thisenzyme where it has a role in tissue repair. Over the lastfew years, the per<strong>for</strong>mance of tests measuring antibodiesto TTG has been improved so that they are now thepreferred screening and monitoring test over gliadin orendomysial antibody tests.Recent enhancements to gliadin antibody tests haveresulted in new tests with fewer false positives. IgAantibodies to F-Actin have recently been described asmarkers with utility to identify individuals more likely tohave difficult to resolve or more serious disease. Thepurpose of this article is to put these advances intoa clinical context to assist you in the diagnosis andmanagement of patients who may have coeliac disease.Doctor, do I have coeliac disease?Since coeliac disease can have quite diverse manifestationsand somewhat insidious features in some individuals, it isnot uncommon that patients may have a relative or friend inwhom the diagnosis of coeliac disease and introduction ofa gluten-free diet has trans<strong>for</strong>med their life. Internet sites ofvariable quality abound and awareness of coeliac disease ishigh amongst patients.You should have some tests <strong>for</strong>coeliac disease.A decision to investigate coeliac disease is easy whenpatients report diarrhoea with steatorrhoea and recurrentmouth ulcers. When patients are generally unwell, haveincreased frequency of bowel actions and increasedfrequency of mouth ulcers, features of malabsorptionincluding iron deficiency or unexplained neutropenia, coeliacdisease should be considered. Thus the question may arisein many patients in whom there is not a strong initial case <strong>for</strong>referral <strong>for</strong> endoscopy.What laboratory tests do we haveavailable and can you tell me a bit moreabout them?IgA and IgG Gliadin Antibody AssaysIgA and IgG antibodies can be detected by ELISA tests. Theresults are reported in units over a “cut-off”. The numbersor values of these results exhibit a good dynamic range ofvalues. They mainly have utility <strong>for</strong> monitoring compliancewith gluten-free diets in patients. Usually IgA gliadinantibodies are negative after 6-9 months of a gluten-free diet(normal
IgA Tissue Transglutaminase Antibody AssaysThis antibody is detected by ELISA assays. Although humanTTG has been identified as “the autoantigen” in coeliacdisease, the slight differences of the TTG used in theseassays may account <strong>for</strong> the observation that this assay doesnot achieve 100% sensitivity and specificity. The resultsexhibit a reasonable dynamic range, and the results arereported in units over a “cut-off” value. Although this assay isnot perfect, it has very high sensitivity and specificity. Somemanufacturers have sought to enhance the per<strong>for</strong>mance ofthese assays by including peptides from gliadin, or gliadinin these assays. IgA antibodies to TTG become negative9-24 months after commencement of a gluten-free diet. Likeall IgA-based tests, the assay is useless in IgA-deficientindividuals.There are some common pitfalls in theselaboratory tests. What should I rememberabout these laboratory tests when I amtalking to patients about the results?IgA-dependent serology is useless in patients with IgAdeficiency, which occurs in 1:300 of the population, someasuring total IgA is a necessary part of the laboratoryinvestigation.Gluten restriction will result in lowering and subsequentdisappearance of all of the lab markers.Do not <strong>for</strong>get clinical syndromes from wheat exposuremay result from other mechanisms including IgE-mediatedwheat allergy, non-immunological intolerance of wheat orpreservatives used in wheat products (propionates).IgG Tissue Transglutaminase Antibody AssaysThis assay has much less sensitivity <strong>for</strong> coeliac disease thanall the other assays. A substantial number of patients withcoeliac disease may be negative <strong>for</strong> TTG-IgG antibodies buthave untreated coeliac disease. In general, most patients withIgA deficiency will have TTG-IgG antibodies. At present wefeel the per<strong>for</strong>mance characteristics are not sufficient <strong>for</strong> usto offer this assay.Combined IgA-IgG Tissue TransglutaminaseAntibody AssaysOne strategy to simplify testing and reduce the likelihood ofmissed cases of coeliac disease could use a combined assay<strong>for</strong> IgA and IgG antibodies to TTG. Such an assay might beexpected to be less likely to miss both IgA deficient patientsas well as “Picarelli” patients. Un<strong>for</strong>tunately, this enhancedsensitivity comes at the price of occasional false positives,but we recommend it as our primary screening assay <strong>for</strong><strong>Coeliac</strong> <strong>Disease</strong>.IgA F-Actin Antibody AssaysA small number of patients with coeliac disease have a muchmore adverse prognosis, with extensive mucosal ulcerationand damage, and preliminary studies indicate that thesepatients are more likely to have F-Actin antibodies. At presentthis assay is not widely available. It may have clinical utility <strong>for</strong>identifying patients at risk of more severe disease.<strong>Coeliac</strong> Tissue TypingTissue typing <strong>for</strong> HLA-DR and HLA-DQ is presently availablethrough the laboratory and is reimbursed by Medicare. Thedetection of genes encoding HLA-DQ2 or HLA-DQ8 identifiesindividuals at risk of coeliac disease. The absence of thesealmost absolutely excludes coeliac disease. Genotyperesults are not affected by wheat consumption in the dietand are usually per<strong>for</strong>med on a dedicated EDTA specimen.Clinical studies to determine the best use of tissue typing <strong>for</strong>including or excluding individuals at risk of coeliac diseaseare presently underway.The likely clinical utility of these tests is that they will be useful<strong>for</strong> identifying individuals from familes known to have coeliacdisease who will need longer term surveillance.The risk status of persons with indeterminate or equivocalserology, discordant serology and biopsy results orinadequate dietary intake of gluten can also be established.A particularly attractive feature of genotyping is that gentlyscraping the buccal mucosa with an appropriate collectiondevice will provide sufficient DNA <strong>for</strong> testing young children,obviating the need <strong>for</strong> venepuncture. We offer this test in ourSonic Clinical Institute Genetics laboratory.What is a “Picarelli” patient?A small series of patients were described with biopsy provencoeliac disease who had no evidence of IgA antibodies togliadin, endomysium or TTG. These patients were not IgAdeficient.Although they occurred in a geographically andpresumably genetically restricted environment, such patientsmay occur occasionally elsewhere, although other serieshave not been described.What tests should I request when I amconsidering coeliac disease?Laboratory Tests <strong>for</strong> the Diagnosis of <strong>Coeliac</strong> <strong>Disease</strong>There are at present quite different but perhaps equallyeffective strategies <strong>for</strong> the serodiagnosis of patients withcoeliac disease. Acceptable strategies should include eitherestimation of total IgA to exclude coeliac disease or asensitive IgG coeliac marker. Our current recommendationsare that a new generation IgA-IgG TTG assay should beper<strong>for</strong>med. At present we recommend “<strong>Coeliac</strong> serology” andwe per<strong>for</strong>m IgA-IgG TTG Antibody and Gliadin IgA antibody<strong>for</strong> a symptomatic person.In a young child from a family known to have coeliac disease,a buccal swab <strong>for</strong> coeliac genotyping will be able to “include”the child as being at risk of coeliac disease or “exclude”the child from the need <strong>for</strong> longer term clinical review andserologic monitoring. There<strong>for</strong>e in a person with minimalsymptoms or inadequate wheat intake, <strong>Coeliac</strong> Serologyand <strong>Coeliac</strong> Tissue Typing should be requested. Althoughgenotyping studies are more expensive than the serologicassay, their power to exclude persons from longer termmonitoring and anxiety about risk of coeliac disease mayresult in their becoming the most economical frontline test <strong>for</strong>coeliac disease.Laboratory Tests <strong>for</strong> the Monitoring of<strong>Coeliac</strong> <strong>Disease</strong>Genotyping studies are not useful <strong>for</strong> the monitoring ofpatients with known coeliac disease. Either IgA-IgG TTGantibodies or IgA-IgG TTG and Gliadin antibodies should berequested in this setting.Endoscopy and BiopsyPatients with adequate gluten intake (at least four weeksof regular wheat) with abnormal coeliac markers should bereferred <strong>for</strong> serology be<strong>for</strong>e biopsy, as negative serologicmarkers may raise the index of suspicion <strong>for</strong> other clinicalproblems! Patients with unequivocal positive coeliac markersor IgA deficiency should be referred <strong>for</strong> endoscopy andbiopsy (Figure 2,3) to document the extent of mucosalabnormality and confirm a histological diagnosis.
Are the lab tests going to be helpfulif I am going send the patient <strong>for</strong> anendoscopy anyway?If the laboratory tests <strong>for</strong> coeliac disease are negative, youwill not have to refer a patient <strong>for</strong> an endoscopy to diagnosecoeliac disease. Endoscopy may still be appropriate whenclinical entities other than coeliac disease may be considered.Not all patients may need to have follow up endoscopies ifthey have a good clinical response to gluten restriction anddemonstrate normalisation of laboratory markers of coeliacdisease (gliadin, endomysial or tissue-transglutaminaseantibodies) and its consequences (iron deficiency, changes inblood count at presentation). For most patients, a progressendoscopy after introduction of gluten restriction is notunreasonable.The patient said “I stopped eating wheata long time ago, and now I want to knowif I have coeliac disease!” What can Iadvise?This is perhaps the most difficult situation in that suchpatients may be very reluctant to eat wheat again.For the diagnosis of coeliac disease, endoscopy is not likelyto be rewarding if the laboratory markers are negative.When patients have avoided wheat products <strong>for</strong> a longperiod of time, coeliac markers are often negative orindeterminate. It is reasonable to check the laboratorymarkers and negotiate a period of wheat ingestion withrepeat laboratory tests and consideration of referral <strong>for</strong>endoscopy. <strong>Coeliac</strong> HLA-DR/DQ genotyping can be used toinclude or exclude patients in this setting.If I have to persuade the patient to eatwheat again <strong>for</strong> the sake of some tests,how long do they have to do this <strong>for</strong>?It is difficult to provide clear evidence-based advice onthis but a minimum of four weeks would be a reasonable“rechallenge” period.We have done all the coeliac tests andthey are negative. The patient asks “OK,so I don’t have coeliac disease but whydo I feel better if I avoid wheat?” What doI say?Some people have IgE-mediated allergy to wheat, othercereal grain proteins, legumes (soy, lupins), or even seeds,such as sesame or poppy seeds, which they might encounterin bakery products. Allergens in these foods are often moreconcentrated in the seeds or grains. These symptoms maybe tested by RAST or skin prick tests as well as avoidanceand challenge.Wheat intolerances result in clinical symptoms, commonly“irritable bowel symptoms”, and sometimes in less specificsymptoms that can result from wheat ingestion, be alleviatedby wheat avoidance, and recur with wheat challenge.Many bakery products also contain preservatives (mostcommonly propionic acid) and this can result in a broadrange of symptoms in some persons including angioedema,urticaria, irritable bowel symptoms as well as headaches,“fuzzy heads” and fatigue. There are no laboratory tests <strong>for</strong>these “intolerances” which are best characterised by dietaryrestriction and challenge.We have done the tests <strong>for</strong> coeliacdisease and they are positive. The patientasks “So I have coeliac disease – is thereanything else wrong with me?”In the investigation of patients with coeliac disease, a numberof other tests are useful <strong>for</strong> the assessment of nutritionalstatus. These might include estimations of B12, folate, ironstudies, vitamin D, blood count, and biochemistry, as well asa serum EPG. An important association of coeliac disease istype 1 diabetes. Some other autoimmune disorders are morecommon, such as pernicious anaemia, thyroid disease andvitiligo.Diagnosis Of <strong>Coeliac</strong> <strong>Disease</strong>Child of <strong>Coeliac</strong> family <strong>Coeliac</strong> tissue typing onbuccal smearFigure 2: Normalduodenal mucosa.Note the long“finger-like” villi onthe surface.Possible InadequateWheat IntakeCurrently Symptomaticor MonitoringDiscordant Serology<strong>Coeliac</strong> Tissue Typing +<strong>Coeliac</strong> Serology (TTG, IgAgliadin Abs)<strong>Coeliac</strong> Serology (TTG, IgAgliadin Abs)<strong>Coeliac</strong> Tissue Typing,Endomysial, Gliadin IgG,repeat <strong>Coeliac</strong> Serology (TTG,IgA gliadin Abs) Total IgAFigure 3: Duodenalmucosa in coeliacdisease. The surfaceis almost flat showingsub-total villousatrophy. Thesemucosal changescan revert to normalor near normal on agluten-free diet.If you have any enquiries regarding <strong>Coeliac</strong> <strong>Disease</strong>,please contact Dr Karl Baumgart, Director ofMolecular Genetics - Sonic Clinical Institute, on(02) 98 555 286 or email: kbaumgart@dhm.com.auSONIC CLINICAL INSTITUTE • ABN 98 100 145 748A subsidiary of SONIC HEALTHCARE14 GIFFNOCK AVENUE • MACQUARIE PARK • NSW 2113 • AUSTRALIATEL (02) 98 555 369 • FAX (02) 98 555 446 • TOLL FREE 1800 004 029MAIL ADDRESS • LOCKED BAG 145 • NORTH RYDE • NSW 1670 • AUSTRALIA