Download PDF - College of Licensed Practical Nurses of Alberta
Download PDF - College of Licensed Practical Nurses of Alberta
Download PDF - College of Licensed Practical Nurses of Alberta
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
PRACTICAL NURSING DIPLOMAMaja thought the state <strong>of</strong> health care back in her homecountry left a lot to be desired. When she arrived in Canada,she knew she could be part <strong>of</strong> something bigger and <strong>of</strong>fer morethan band-aid solutions. She knew it was time to get serious…Maja <strong>of</strong>fers MOREthan band-aid solutionsand get a career. Maja knows that if you want to be the best,you train with the best. She did her research and found outthat Bow Valley <strong>College</strong>, along with <strong>of</strong>fering more than 50career programs, is a leader in <strong>Practical</strong> Nurse education. Shealso found out that she can earn up to $35 an hour. She pickedup the phone, called a BVC advisor, and discovered she couldtake the program on a full-time in-class basis or part-time in anonline and classroom blend. She filled out her online applicationand is now on her way to learning how to provide real care.She’ll even do her practicum at a local health-care facility.Maja knows with the right training and the right attitude, she’llsucceed as a nurse and <strong>of</strong>fer more than band-aid solutions.LEARN MORE. EARN MORE. DO MORE.FIND OUT MORE:bowvalleycollege.ca/more403-410-1402care | SUMMER 2011 5
6 care | VOLUME 25 ISSUE 2
transformThe University <strong>of</strong> <strong>Alberta</strong> Hospital (UAH) is one <strong>of</strong>Canada’s leading clinical, research, and teachinghospitals located in Edmonton, <strong>Alberta</strong>. Thehospital <strong>of</strong>fers a wide range <strong>of</strong> diagnostic andtreatment services, including specialized serviceswithin cardiac sciences, neurosciences, surgery,medicine, renal, critical care, emergency andtrauma care, and a state-<strong>of</strong>-the-art burn unit.The UAH site embarked on a venture to advancethe role <strong>of</strong> <strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong> in July2010. This story showcases the comprehensiveplanning and preparation process, and how suchwork literally transformed care delivery in theirmedical unit nursing teams, with planning toproceed throughout the site in the near future.8 care | VOLUME 25 ISSUE 2
The floor is bustling on inpatient unit 5E2, a General Internal Medicine Unit at the University <strong>of</strong><strong>Alberta</strong> Hospital. Staff are moving efficiently from patient rooms with medications and IV poles, thephone keeps ringing, and families gather around patient beds. Watch the action closely and you’llsee a nurse patting another nurse reassuringly on the shoulder, smiles being exchanged in themed room, and gentle joking in the hallways.The buzz on the unit is busy, but the energy is all positive. This group works together as a team,and it shows their belief in the capacity <strong>of</strong> all the nurses who work there. This past year, all fourUniversity <strong>of</strong> <strong>Alberta</strong> Hospital General Internal Medicine inpatient units (5E2, 5D2, 5D3 and 5D4)are the first units to embark on a journey to expand the role <strong>of</strong> LPNs in their facility, as part <strong>of</strong> asite wide project.ing care by Sue RobinsroLE cHANGES AT UAHBuilding the FoundationExpanding a pr<strong>of</strong>essional role in a hospital requires a great deal <strong>of</strong> careful planning, and that includeshaving the right people around the table. The LPN Expanded Role Working Group began in July 2010,and right from the beginning, it was an inclusive group that included representation from LPNs, RNs,Clinical Nurse Educators, Managers, and the <strong>College</strong> <strong>of</strong> <strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong> <strong>of</strong> <strong>Alberta</strong> (CLPNA).“The scope <strong>of</strong> this group was to look at what LPNs needed at the University <strong>of</strong> <strong>Alberta</strong> Hospital toexpand their role,” says Christine Lauerman, Chair <strong>of</strong> the Working Group and Project Coordinator,Northern <strong>Alberta</strong> Renal Program, Medicine and Family Medicine.They first looked at what skills LPNs could do according to HPA and CLPNA competency and comparedit to the restrictions outlined in hospital policies. The gaps between the two are the differences that arebeing addressed through role changes for the LPNs. A Policy Review Sub-Committee is makingrecommendations to update the policies, and an Education Sub-Committee is designing modules to teachthe skills needed to expand the scope.Tammy Dianocky was an LPN voice on the Working Group and Education Sub-Committee. “I’m pro-LPN,” Tammy firmly states, “And I think we can do more than we’ve been allowed to do in the past.”She cheerfully admits that she likes to share her opinions and is a front line cheerleader for her LPNcolleagues. That’s one <strong>of</strong> the reasons she was asked to sit on the LPN Expanded Role Working Group,and contribute to the Education Sub-Committee. As an LPN with diverse experience – from dialysis tosurgery to palliative care – Tammy brought her ‘pro-LPN’ perspective to the meeting room table. Shealso is in the unique position <strong>of</strong> having an expanded role when she works at Covenant Health, and nowan evolving expanded role at the University <strong>of</strong> <strong>Alberta</strong> Hospital.>care | SUMMER 2011 9
Expanding the LPN role is not new;there was a lot <strong>of</strong> work done in theprevious Capital Health region by theRoyal Alexandra Hospital andCovenant Health to increase the LPNrole in their hospitals. They generouslyshared their teaching materials with theUniversity <strong>of</strong> <strong>Alberta</strong> Hospital, and ateam <strong>of</strong> educators – including Tammy asthe LPN representative – worked veryhard to create learning materials for theUniversity <strong>of</strong> <strong>Alberta</strong> Hospital site.“We wanted to make sure the materialswere understandable to our learners,and having the LPN on the committeereally helped with that,” shares BrendaBond, the chair <strong>of</strong> the Education Sub-Committee, “We looked at all the workthat was done and built on the modulesfrom the other sites. ““I felt honoured to be asked toparticipate, and definitely felt like myopinions were listened to,” says Tammy,“CLPNA really paved the way to haveLPNs included in the planning <strong>of</strong>the LPN expanded role.”Working with seniormanagement’s strongsupport, and with thenurses’ practical input, aplan was developed thatwould soon change atypical day in the life <strong>of</strong> anLPN on the medicine units.Brenda Bond is a ClinicalNurse Educator, but likeTammy, she too is acheerleader for all nurses.Brenda chaired theEducation Sub-Committeeand taught the LPN skill training, alongwith her colleague Glenna Welykochy.The University <strong>of</strong> <strong>Alberta</strong> Hospital hasa great number <strong>of</strong> LPNs working ontheir medicine units, and there wasmuch interest and many champions onthe units who believed in the value <strong>of</strong>expanding the LPN role.“We looked at every skill, and created alist that needed to have both policy andprocedure changes, and education <strong>of</strong> thenurses to make sure they could practicewith skill and safety. We prioritized thelist according to what would give us thebiggest bang for the buck,” says Brenda,“The training for the LPNs began witha lot <strong>of</strong> management support. Theywanted us to do it right, so the LPNscould fly on their own safely.”The first skill chosen was intermittentmedication through peripheral IV sitesbecause it is very common for patientson medicine units to have this type <strong>of</strong>medication. This would have a bigimpact on nursing practice for both theLPNs and RNs, and the group chose theskills that would be used a lot, andtherefore practiced, on medicine.“When you teach a new skill, thereneeds to be ample opportunity fornurses to solidify their skills. If youdon’t have the opportunity to practice,then it is difficult to sustain thatknowledge,” explains Brenda. The Sub-Committee added taking critical labresults and accepting patient care ordersto the list <strong>of</strong> expanding LPN skills.There was some natural hesitation fromsome <strong>of</strong> the nurses about learning newskills, but Brenda saw the trepidationtransform into confidence as theypracticed their new skills. “We wantedto provide them with support to makesure they felt comfortable, and I feelstrongly that you cannot rush skilltraining,” Brenda states. The educatorsand the nurses kept working togetheruntil they felt safe and comfortable withtheir new skills.10 care | VOLUME 25 ISSUE 2
So what did the nurses think?S<strong>of</strong>t spoken and quiet, Mary RoseVelez’s face lights up when she talksabout the new skills she’s acquiredthrough the Expanded LPN Role on5E2. She moved to Canada from thePhilippines three years ago, and saysdiplomatically, “I like living in Canada,except for the weather, but I’m learningto cope with it.”Mary Rose took the two-day trainingfor IV medication, taking critical labresults, and accepting patient careorders. “It is a good change because wecan function more autonomously,”she explains. “Some nurses had a hardtime adjusting at first, but with thesupport <strong>of</strong> the Clinical NurseEducators and the training, they’vebecome more confident.”LPNs were brought together forclassroom and lab sessions. Thestudents ranged from brand new gradsto nurses with over 20 years experience.The Educators started with apresentation on IV medicationadministration, reviewed the ParenteralDrug Manual and gave them exercisesto practice calculation and rates for IVmedication administration.Next, they had a labsession with infusionpumps and vials, wherethe nurses were able tosimulate drawing upmeds into a bag, andwork with secondarymed lines and smartpumps. At the end <strong>of</strong>the day, the nurseshad knowledge pluspsychomotor practicelearning the new skill.Next up was practicetaking critical labresults, and takingverbal and telephonepatient care orders.Prior to being trained, ifa patient was nauseated, an LPN couldnot phone the physician to get amedication order. She had to find anRN to place the call. The teaching <strong>of</strong>taking orders was especially significantWhen youteach a newskill, thereneeds to beampleopportunityfor nursesto solidifytheir skills.because the new <strong>Alberta</strong> Health Servicespolicies were incorporated into theteaching – so all trained LPNs are up todate in their practice.“I would say I feel really supported if Ihave any questions – I can ask the othernurses, or the Educator, and I try to helpothers as much as I can,” says MaryRose. “I can do lab orders on my own,and don’t have to find an RN if aphysician is giving verbal orders,because I can take it myself.”“I think it has made our teamworkmore efficient, especially if we have lots<strong>of</strong> patients on IV medication,” shecontinues. “I think it is a good change.I’m looking forward tolearning future skills.”The staff on the unitswere delighted to havethe LPNs come onto theward during theirsupervised practice, tohang IV medications,and each nurse practicedwith support until theywere comfortableperforming their newskill. “This was the funpart <strong>of</strong> the training”,says Brenda. “Weencouraged them to askquestions and seek helpif they needed it, andafter that they were goodto go on their own.”What impressed Brenda most about herLPN students is their critical thinkingskills were evident immediately after the>care | SUMMER 2011 11
We Need <strong>Licensed</strong><strong>Practical</strong> <strong>Nurses</strong>!FULL TIME, PART TIME AND CASUAL POSITIONSAre you a LPN looking for a position that <strong>of</strong>fers competitivewages, comprehensive benefits, a variety <strong>of</strong> shifts, and theopportunity to improve the quality <strong>of</strong> life for individualsand their families?The Good Samaritan Society is always looking for skilledLPNs who can deliver quality resident care. As one <strong>of</strong>Western Canada’s largest voluntary, not-for-pr<strong>of</strong>it,caregiving providers, we believe that a balanced worklife contributes to healthy and happy employees,who in turn provide the best care to our residents,which is what matters to us the most.• Visit www.gss.org to view all our jobopportunities• Please submit all resumes to:careers@gss.orgThe Good Samaritan Society is an equal opportunity employer.We encourage applications from all qualified individuals registeredwith CLPNA who have current First Aid and CPR.DEMENTIA CARE – Interactive and Online!LEARN THE BASICS OF DEMENTIA CARE – WHEN AND WHERE YOU WANTThis dynamic course is designed for caregivers in a variety <strong>of</strong>settings. Whether you’re part <strong>of</strong> a multi-disciplinary teamor caring for a loved one at home, you will acquire skills toenhance your care giving.“Our residents have benefited from the strategies I learnedin this course. I feel more confident and am able to helpmake this facility more <strong>of</strong> a home for them.”For more information about Dementia Care ONLINE –CALL 780-644-6361EMAIL dementia.program@norquest.caAPPLY TODAY!780-644-60001-866-534-7218info@norquest.cawww.norquest.cacare | SUMMER 2011 13
MagicMomentsForging Our Future One Moment at a TimeThis article was extracted from Donna Devlin’s 2011 CLPNA Spring Conferencekeynote address and Donna’s Magic Moments in Health Care book.“Magic is about transforming our self andwork in health care from one moment tothe next.” — Donna Devlin“There is huge potential in small things.” Ilike to use metaphors to help us look ataspects <strong>of</strong> our lives from a greatertransformative lens. The pine cone that iscaptured on my books cover illustratesour potential to grow, touch andinfluences ourselves, colleagues andpatients through the tiniest gestures. Thepine cone is also a medical symbol thatdates back to the early 14th century. Theheart symbol in early medical illustrationswas first shaped like pine cones in theHippocratic School by Galen.We sometimes forget or devalue thepr<strong>of</strong>oundness in simplicity and maybeeven mitigate our healing presence withpatients. Part <strong>of</strong> our journey as nurses isin supporting each other to reflect andseek out knowledge and inspiration as weforge our future in health care. We arecreative beings and we all have a hand increating our work environment. I believewho you are and what you bring into yourwork will always be the best tool in healthcare.We are seeing more <strong>of</strong> the “perfectstorm” <strong>of</strong> fatigue, frustration and burn-outin health care workers across thespectrum, along with higher rates <strong>of</strong> jobvacancy, injury, disability and stress leave.Healthcare workers are searching forways to continue the human-side <strong>of</strong> theirwork among the technological, diseaseoriented, hospital-based approaches andother healthcare challenges. Thedemands on health care staff areenormous. Pressures from limitedresources, increasing expectations frompatients and families, and technologicaladvances are affecting the ability <strong>of</strong> healthcare workers to derive meaning andsatisfaction from their work.I have worked twenty-seven years as ahealthcare pr<strong>of</strong>essional. For the pastfourteen years, I have had the privilege <strong>of</strong>working with healthcare staff in aneducational, staff development capacity.Like you, I am on a journey <strong>of</strong> finding andcreating meaning in my life and work. Notwo journeys are alike, but there arecommon threads that bind healthcarepr<strong>of</strong>essionals together. Those <strong>of</strong> us in thehelping pr<strong>of</strong>ession are continually facedwith increasing pressure, strain, and amore hectic pace. The hurdles we mustconstantly overcome sometimes cause usto feel frustrated, exhausted andinadequate. There are times when webecome depleted and disillusioned withour work.our patients need to feel human contactand connection. This is not always aneasy thing to achieve. We sometimesbecome so focused on our tasks,technology and routines that our jobsbecome mechanical and meaningless. Itseems to me that what is fundamentallylacking is honoring the sacredness <strong>of</strong> ourmere presence. We need to truly honorthose moments when we know we areconnecting with someone or have doneeverything we possibly can to make aconnection. There may be times, because<strong>of</strong> the nature <strong>of</strong> a patient’s illness, whenwe feel like we’re not making a meaningfulconnection because our experience isn’tas positive and warm as we think itshould be. But I believe in all thesecases, we do make a connection—one <strong>of</strong>understanding and compassion. This isespecially important with our so-called“difficult” or “challenging” patients andfamilies.This process <strong>of</strong> honoring the magicmoments must begin with defining theterm “magic” and understanding our roleas healthcare workers. I believe each <strong>of</strong>us yearn for that connection where we14 care | VOLUME 25 ISSUE 2
know we are making a difference in the life <strong>of</strong> anotherhuman being. I also believe that there are certain hurdlesin healthcare that can hinder our helping journey.Acknowledging and identifying hurdles like “the helper’shole,” the difficult patient, our fears, worries, doubts andegos will set the stage toward honoring the mode <strong>of</strong>magic moments on our healthcare journey. I refer tothese as “Magic Moment Modes,” which are natural,conscious, transformative, replenishing processesinvolving perspective and knowledge. The modes <strong>of</strong>magic moments involve bringing conscious awarenessinto our work and creating an environment that honorsthe significance <strong>of</strong> serving others. Ultimately, this is wherewe derive our meaning as health care pr<strong>of</strong>essionals.Whether you are in the beginning, middle or end <strong>of</strong> yourjourney as a nursing pr<strong>of</strong>essional we are all searching forways to create meaning and healing at work. As nursingpr<strong>of</strong>essionals, we walk a line involving sorrow, joy,frustration and amazement. Every day we find ourselvesin the humbling position <strong>of</strong> making a difference in thelives <strong>of</strong> others. And that is no small accomplishment.Many blessings to you, and may you continue to growin your work. Know that you alone can make a differencein the lives <strong>of</strong> others. And that is no small wonder…it is magic! nJoin us.We are one <strong>of</strong><strong>Alberta</strong>’s Top 50 EmployersMentoringProgramsWatch for more articles from Donna Devlin.RewardingnursingcareersWork/LifeBalanceMeaningfulrelationshipsDonna is an author, speaker, facilitator andeducator. Donna Devlin’s passion is peopleand the human spirit. She is the author <strong>of</strong>“Magic Moments in Health care- Making aDifference one Moment to the Next.” Sheis also a contributing author <strong>of</strong> the book“Awakening the Work Place Volume 2”.Donna is a registered Psychiatric Nursewith over twenty-seven years <strong>of</strong> communityexperience and has a Bachelors degree inGeneral Studies from the University <strong>of</strong>calgary. She is presently working towardsher MEd in adult and workplace learning atUniversity <strong>of</strong> calgary. To learn more aboutDonna or to invite her to your next workplacelearning event, please refer to herwebsite www.donnadevlin.com.403.210.HOME1.888.410.4679humanresources@bethanycare.comwww.bethanycare.comCreating Caring CommunitiesAirdrie Calgary Cochrane Red Deer Sylvan Lakecare | SUMMER 2011 15
ReconnectDid you graduatefrom Bow Valley <strong>College</strong> lege or AVC Calgary?Would you like toreconnect with former classmates and faculty?Would you like the opportunity to planLPN alumni events and activities?If you answered yes to these questions, the Bow Valley <strong>College</strong> Alumni Associationis looking for you!Contact us by July 15 if you would like to find out moreabout Bow Valley <strong>College</strong>’s first <strong>of</strong>ficial alumni chapter.403-355-4666| alumni@bowvalleycollege.ca16 care | VOLUME 25 ISSUE 2
Patient CenteredLeadershipSecond in a series on Leadership with a focus on the autonomyand responsibility <strong>of</strong> the <strong>Licensed</strong> <strong>Practical</strong> Nurse.Listening on the Front LinesBy rachel Foster, MN cMc cEc<strong>Nurses</strong> are great at ‘fixing’ people,situations, and almost anythingbroken! It comes naturally to us. Theproblem is that <strong>of</strong>ten it is not ourproblem to fix, and many timespeople don’t want or need a solution,they just need a safe place to have avoice and be heard.Most have heard <strong>of</strong> Stephen Covey, theauthor <strong>of</strong> 7 Habits <strong>of</strong> Highly EffectivePeople. Habit 5 is “Seek first tounderstand, then be understood”. Thinkabout this for a moment and consider howmany times you have wished thatsomeone really listened to you, or took thetime to clarify and understand what youwere really saying. Reading his book andthinking about this Habit was a turningpoint in my learning and development as anurse leader. I actually had to stop, slowdown my thoughts, tune in, and listen towhat others were saying, without buttingin, finishing their sentences, or thinking Ihad the solutions.Become a Listening Partnerin Nursing<strong>Nurses</strong> are typically very task focused, andso we are always in the doing rather thanbeing mode. The challenge with being sotask focused and busy is that we misscrucial opportunities to connect as humanbeings in a caring and compassionate way.Workload and patient acuity is increasingon almost a weekly basis, however whenyou pause for a moment to consider whatyou would want if you were in a vulnerableplace in your life, I suspect it would not bethe nurse or colleague who was rushing<strong>of</strong>f in their busyness somewhere to dosomething. I suspect you would value theperson who could take a moment to bewith you and really listen.As you ponder this for a moment, considerhow you could engage in meaningfulconversations with your colleagues orclients, and become a listening partner.Perhaps it would be by asking curiousquestions, helping them seek resolution fortheir issue, if that is what’s needed, ratherthan <strong>of</strong>fering advice. If you could take aminute to do that, what would be theimpact on you personally andpr<strong>of</strong>essionally? Perhaps a clearerunderstanding and respect for their model<strong>of</strong> the world? Perhaps a betterunderstanding <strong>of</strong> them as a fellow humanbeing and the challenges they are facing?How would it be if you did not have to haveall the answers? Would you travel lighter?Step into their shoes for a moment andponder what their experience <strong>of</strong> theinteraction would be like? What do youthink would be the impact on them?Learning Partners in NursingCommunicating our feelings and ourneeds is one <strong>of</strong> the biggest challenges weface as individuals and as pr<strong>of</strong>essionals.Often times, we wind up in situationswhere what we say isn’t what we reallymean, and what we mean isn’t what endsup coming out <strong>of</strong> our mouths! Coupled withour ineffective use <strong>of</strong> verbal language isthe challenging issue <strong>of</strong> our body languageor non-verbal communication, whichcomplicates everything. Only about 7%<strong>of</strong> our communication is verbal so thatleaves about 93% for all the non-verbalmessages we send, so it is hardlysurprising that there is <strong>of</strong>ten mismatchbetween our words and our intent! This isthe beginning <strong>of</strong> conflict.I know that you can think <strong>of</strong> numerouspersonal examples where you, or someoneyou know, have been misunderstood. Ispend a significant amount <strong>of</strong> time dealingwith conflict and misunderstandingbetween individuals and teams, and whatI have learned is that it is all avoidable bylistening, clarifying, and taking the time tolearn what is really going on. It is alsoimportant to create a safe space whereothers feel they can show up and beheard. As well, each one <strong>of</strong> us has to bemindful <strong>of</strong> what we say and the impact <strong>of</strong>our words and actions have on thosearound us.How then can we become betterlearning partners as we partner inlistening?Perhaps the biggest single thing that any<strong>of</strong> us can do is come into a conversationprepared to be 100% present. Considerfor a moment what would it be like to bereally heard, with no judgment? It wouldbe refreshing – right? Now be honest andask yourself how <strong>of</strong>ten you enter aconversation with a whole laundry list <strong>of</strong>to-do’s going on inside your head. I knowyou are smiling! We all do it, and thepractice is to put the lists away and committo being with the other person absolutelyand completely, whomever it is, whether ornot we like them or agree with them.Perhaps they have never experiencedanything like this before. Perhaps you havenever experienced this before, however,are you willing to give it a try and givethem the gift <strong>of</strong> being present, and reallylistening for what they have to say? Canyou leave your agenda outside the door?>care | SUMMER 2011 17
The next most significant practice for developing as alistening and learning partner in nursing is one <strong>of</strong>mindfulness. As I mentioned earlier, most conflict andangst can be avoided if we are aware <strong>of</strong> the impact ourwords and actions have on those around us. Too <strong>of</strong>ten weget caught up in the busyness <strong>of</strong> our life and work and webecome short, blunt, and impatient with our colleagues,clients, and their families (not to mention our own), andforget that we wear our behaviors like our scrubs. Theyare there for everyone to see in a vast array <strong>of</strong> patterns,colors, and in a range <strong>of</strong> conditions! So, what are youchoosing to wear today? Pastel, calming andapproachable, or strong, fiery, and brusque? Will you noticewith grace and compassion or charge through your dayunaware <strong>of</strong> the trail <strong>of</strong> devastation behind you?I will finish with a quote from Susan Scott who says in herbook Fierce Conversations, “The Conversation IS theRelationship ® ” nAction Plan• If you were to share what you have learned fromthis article with a colleague, what would you say?• Looking ahead 90 days from now, please writedown:• What would you like to be different in yourpr<strong>of</strong>essional life as an emerging nurse leader?• What three things will you work on tosupport your goal?References:Covey, S (2004) 7 Habits <strong>of</strong> Highly Effective PeopleScott, S (2004) Fierce Conversations: Achieving Success at Work & in Life,One Conversation at a TimeMacEwan’s Centre for Pr<strong>of</strong>essional NursingEducation <strong>of</strong>fers distance certificate programsto help you take your career to the next level.Wound ManagementPost-Basic Certificate –Get your post-diploma certificate bycompleting five courses specialized inmanaging complex wounds.www.MacEwan.ca/WoundPerioperative Nursing for LPNs –Complete this four-course certificate andacquire the skills you need to work in thechallenging and team-oriented environment<strong>of</strong> the operating room.www.MacEwan.ca/PeriopLPNRachel Foster, MN CMC CECrachel has over thirtyyears diverse experiencein healthcare in canadaand the UK. She workedas nurse in rural andacute care settings, continuingcare and publichealth, as well as teachingat the University <strong>of</strong> <strong>Alberta</strong>.For the past tenyears, she has been fascinatedwith leadershipand mentoring and in2009 earned a Graduatecertificate in Executivecoaching from royal roads University. rachelnow coaches leaders and executives to havecourageous conversations and discover possibilities.She keeps her nursing skills current atcovenant Health.For more, see www.rachelfoster.com orinfo@rachelfoster.com.rachel is donating her writing fee to the EducationFoundation to support LPN Leadership education.Centre for Pr<strong>of</strong>essional Nursing Educationwww.MacEwan.ca/RN18 care | VOLUME 25 ISSUE 2
Carewest Career Opportunities<strong>Licensed</strong> <strong>Practical</strong> NurseAs a <strong>Licensed</strong> <strong>Practical</strong> Nurse (LPN) with Carewest, you will utilize your full scope <strong>of</strong> practice, conductclient assessments and medication administration, while working within an interdisciplinary team.Carewest is a leading-edge public organization for adults who requirecontinuing care and rehabilitation services, which <strong>of</strong>fers<strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong> a wide range <strong>of</strong> career opportunities.We have 10 sites in Calgary, <strong>Alberta</strong> and are growing.Please refer to the Carewest website forjob opportunities at www.carewest.caAdvanced d Education inOrthopedics Certificatefor LPNsNorQuest’s Advanced Education in Orthopedics certificatewill open doors for youand provide many opportunities.Learn about advanced orthopedic assessment, traumaaand specialized procedures including casting.Formore information, call 780-644-63666or emaillaura.milligan@norquest.caTo register, call780-644-6000or toll-free1-866-534-7218-7218www.norquest.cacare | SUMMER 2011 19
2011 CLPNA SPRING CONFERENCE RECAPConnection, celebration, inspiration, and information highlighted the 2011 Spring Conference <strong>of</strong> the <strong>College</strong> <strong>of</strong><strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong> <strong>of</strong> <strong>Alberta</strong> (CLPNA). More than 330 LPNs, RNs, and other health pr<strong>of</strong>essionals gatheredat the Deerfoot Inn and Casino in Calgary on April 6-8, 2011 to hear expert keynotes and concurrentsessions, attend the CLPNA’s Annual General Meeting, enjoy the Celebration and Awards Dinner, andreturn home informed and encouraged. It was a unique year, with many LPNs and colleagues presentingat the event.Keynotes from some <strong>of</strong> Canada’s leading healthcare experts provided updates on Canada’s healthcaresystem, nurse staffing research, and forging the future <strong>of</strong> nursing and health care. Diverse session topicsincluded the LPNs role in triage, new career paths, continuing competency, end <strong>of</strong> life planning, nursingresearch, inner-city health issues, person-centered care, dementia care strategies, and thriving at work.Annual General MeetingDuring the Annual General Meeting on April 6, CLPNA Executive Director Linda Stanger gave acomprehensive overview <strong>of</strong> the 2010 Annual Report. Stanger spoke passionately on the necessity forresearch involving <strong>Alberta</strong> LPNs; national and international collaboration and mentoring; the growth <strong>of</strong>LPN leadership; and the need for advocacy <strong>of</strong> the pr<strong>of</strong>ession by all LPNs. The evening ended with arecognition <strong>of</strong> 25 years <strong>of</strong> self-regulation for the LPN pr<strong>of</strong>ession in <strong>Alberta</strong>.Celebration & Awards DinnerThe Celebration and Awards Dinner capped Thursday with fun and festivities as local improv group “Scratch” kept everyonein stitches. Host sponsor Bow Valley <strong>College</strong>’s President Sharon Carry spoke about “LPNs forging ahead with spine andspunk” during her opening comments. A shocked Ted Langford received an Honorary Membership for his long-time support<strong>of</strong> the CLPNA and the LPN pr<strong>of</strong>ession. The recipients <strong>of</strong> the three Awards <strong>of</strong> Excellence and the Interpr<strong>of</strong>essional DevelopmentAward received their accolades, and all nominees were recognized.Canada’s Health Care System with André PicardThe Globe and Mail’s award-winning health policy writer, AndréPicard, grounded his keynote speech, “Critical Care - What’sHappening in Canada’s Health Care System”, in the premisethat there are only two things Canadians are passionate about:the weather and healthcare. With a political poke, Picard cheekilypromised that by the end <strong>of</strong> the morning, attendees wouldknow more about Canada’s health care system than most healthministers. “<strong>Nurses</strong> are the glue that holds the (healthcare) systemtogether,” he stated. Picard challenged LPNs that everyone hasa part to play in shaping public healthcare policy: “You have topromote your pr<strong>of</strong>ession. You have to be squeaky!”Research Basics with Dr. Sean ClarkeResearcher Dr. Sean Clarke explained “It’s Complicated:Truth and Myths in Nurse Staffing Research” in his Fridaymorning keynote. “Nursing is expensive, important, andinvisible, which puts it under scrutiny by administrators tryingto cut costs and improve systems,” described Clarke.Because research is used as a tool to implement change,it is “intrinsically political”. Clarke showed how researchimpacts every nurse, with reminders that context is everythingand correlation is not causation.20 care | VOLUME 25 ISSUE 2
The 2011 CLPNA Spring Conferencewishes to thank all conferencedelegates, speakers, partners, andsponsors for your involvement andsupport. Your contributions andattendance helped to make thisyear’s conference a memorableand successful event for all involved.SPECIAL THANKS TO OURGENEROUS SPONSORS:DIAMONDBow Valley <strong>College</strong>PLATINUMNorquest <strong>College</strong>AUPEGOLDLakeland <strong>College</strong>Covenant HealthSILVERCarewestColumbia <strong>College</strong>Grant MacEwanThe Good Samaritan SocietyThe PersonalField LawCLPNA SpringConference 2012May 2 - 4 at theEdmonton Marriott atRiver Cree ResortBRONZEPhilips LifelineLloyd Sadd Insurance Brokers Ltd(co-sponsor: Encon)MCI The Doctor’s OfficeIN KINDION Print SolutionsMr. Pin ManGraphic Overloadcare | SUMMER 2011 21
2011Awards <strong>of</strong> EWinners <strong>of</strong> the 2011 Awards <strong>of</strong> Excellence werehonored at the college <strong>of</strong> <strong>Licensed</strong> <strong>Practical</strong><strong>Nurses</strong> <strong>of</strong> <strong>Alberta</strong>’s (cLPNA) celebration andAwards Dinner on April 6, 2011 in calgary, <strong>Alberta</strong>. A specialHonorary Membership was also announced during theevening. Nominees and delegates waited in suspense withfamily, friends, and co-workers, while enjoying a lovely mealand engaging entertainment.Award recipients are selected by a committee <strong>of</strong> theFredrickson-McGregor Education Foundation for LPNs.The Foundation is a non-pr<strong>of</strong>it society supporting cLPNAmembers through education grants, bursaries, andawards <strong>of</strong> merit. Each LPN recipient received a commemorativecrystal award and $1000.HONORARY MEMBERSHIPrEcIPIENT: TED LANGForDTed Langford received anHonorary Membership from thecLPNA for his nearly 20 years <strong>of</strong>service to the LPN pr<strong>of</strong>ession.Executive Director Linda Stangerdescribed Langford as “a person<strong>of</strong> exemplary ethic and integrity, whose belief in andsupport for the LPN Pr<strong>of</strong>ession in <strong>Alberta</strong> has significantlyimpacted our evolution”. A teacher by training andPresident <strong>of</strong> Portage college in Lac La Biche for 24years, his relationship with cLPNA began when hebecame President <strong>of</strong> NorQuest college in the early1990’s. Langford was appointed by Government to thecLPNA council from 2002 to 2010. The council <strong>of</strong> thecLPNA grants the privilege <strong>of</strong> Honorary Membership tonon-LPNs who have rendered distinguished service orvaluable assistance to the pr<strong>of</strong>ession or to the collegeresulting in positive recognition for the pr<strong>of</strong>ession.PAT FREDRICKSON EXCELLENCE INLEADERSHIP AWARDWINNEr: cHLoE SILVEr, LPNAs she stepped up to the podiumto receive her award, an emotionalchloe Silver, LPN, reflected thatshe “can’t believe” she’s paid todo what she loves: caring forpeople. Her nominators describe her as a dedicated, outstanding,and exceptional LPN, leader and pr<strong>of</strong>essional.chloe has been an LPN since 2004 and is currentlyemployed as the Wellness coordinator in a continuingcare facility. As a dedicated resident advocate, chloetreats each client as she treats her own family. For thisLPN, success is not measured by the amount <strong>of</strong> moneyshe makes or the status she attains. “I love what I do.I love being an LPN. I would not change a thing.”RITA MCGREGOR EXCELLENCE INNURSING EDUCATION AWARDWINNEr:coLLEEN SWENSoN, LPNcolleen Swenson, LPN, hasalways been well respected andrecognized within the communitystream <strong>of</strong> nursing as an Educatorand Leader. She holds certification as an Instructor/Trainer in many courses such as Acquired Brain Injury,Non-Violent crisis Intervention and cPr, and is alsoa NorQuest college Tutor for the Health care Aideprogram. recently, colleen joined <strong>Alberta</strong> HealthServices’ Integrated Supportive Living, clinical &consultative Services and her manager states, “She wastruly a rare find!” “Her enthusiasm and energy arepr<strong>of</strong>oundly contagious,“ she continues. “It is gratifying t<strong>of</strong>ind a leader/educator that is so keen to learn from thoseshe leads, as she is to share her own ideas!”22 care | VOLUME 25 ISSUE 2
xcellenceLAURA CRAWFORD EXCELLENCE INNURSING PRACTICE AWARDWINNEr: cHrISTINE WELLS, LPNchristine Wells, LPN is described as aproud and capable member <strong>of</strong> theLPN pr<strong>of</strong>ession who has become the“nursing glue” <strong>of</strong> her medical clinic. Herboss states, “What once was ‘my’practice has become ‘our’ practice and it is shared withmedical students, family medicine residents, nursing studentand observers.” He continues, “Each <strong>of</strong> these learners is welcomedinto our practice due to the outstanding ability <strong>of</strong> thisLPN to be clinically proactive and passionate about patientadvocacy and education.” The family practice residentsshared exemplary examples <strong>of</strong> christine’s value to the clinic,their patients, and the team.INTERPROFESSIONALDEVELOPMENT AWARDWINNEr: LILIE EIKENBErrY, rNLilie Eikenberry, rN, leads by exampleand has elevated her teams to placesnot otherwise possible. She hasrecently opened two transition/rehabunits in calgary, and it was clear on dayone that Eikenberry had a different approach. She encouragedfeedback on her presentation <strong>of</strong> teamwork and load sharing.Each team member works to full scope to utilize education,experience, and knowledge. LPNs are empowered to makecritical decisions and work in a leadership role, even as chargenurse when needed. The cLPNA thanks Eikenberry for hercommitment to collaborative practice and helping LPNs growas pr<strong>of</strong>essionals and individuals.2011 AWARDS NOMINEES& BURSARY RECIPIENTSThe cLPNA and Fredrickson-McGregorEducation Foundation for LPNs congratulatesthe Nominees for the 2011 Awards <strong>of</strong>Excellence. These exceptional LPNs werenominated by employers and colleaguesacross <strong>Alberta</strong>. In the Foundation’sopinion, they are all winners.Laura Crawford Excellence inNursing Practice AwardWinner: christine Wells, calgaryNominees:cathy campbell, calgarySharon christman, Brooksrebecca Elkew, EdmontonJacintha Gabriel, calgaryPetra Gallerno, calgaryWendyAnn Keeton, NantonHawa Koumane, EdmontonElaine Lake, calgaryDeborah McDonald, EdmontonLori Palasty, Edmontonrosemarie Pinson, EdmontonLisa Powell, Stettlercarolyn Quong, DrumhellerDaniel Sweti, calgarycathy Ullyott, calgaryPat Fredrickson Excellence inLeadership AwardWinner: chloe Silver, red DeerNominees:charles Michael cutler, claresholmcheryl Kelly, PonokaSylvia Harkema, Jasperryan reynolds, EdmontonRita McGregor Excellence inNursing Education AwardWinner: colleen Swenson, EdmontonNominees:rhonda Lush, EdmontonAdrianna Moline, BeaumontLaura Pratt, calgaryInterpr<strong>of</strong>essional Development AwardWinner: Lilie Eikenberry, rN, calgaryDavid King Educational Bursaryrecipients:Jody Misunis, EdmontonDorothy Wurst-Thurn, Grande Prairiecare | SUMMER 2011 23
Build on yourNursingSkills atBow Valley <strong>College</strong>…and save*Bow Valley <strong>College</strong> Alumni working as LPNs are eligible le for a 10%discount on select Continuing Education courses thatqualify ascontinuing competencyactivities upon annual licencee renewal. Leadership for <strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong> - Online Care <strong>of</strong> an Agitated Client * Documentation Refresher * Infusion Therapy – Fluid, Blood and Medication * Intramuscular and Intradermal Injections * Intravenous Medication Administration * Immunization – Online or Homestudy * Basic Foot Care ** BVC Alumni eligible for 10% discount on select coursesFor more information about our medical courses please call 403-410-1499410-1499 or emaillpn@bowvalleycollege.caYour Bow Valley <strong>College</strong> tuition may be eligible for a grant from the Fredrickson-McGregorEducation Foundation for LPNs. For more information visit: foundation.clpna.comBow Valley <strong>College</strong>’s <strong>Practical</strong> Nursing Diploma is recognized as one <strong>of</strong> Western Canada’sbest. We <strong>of</strong>fer full- and part-time programs in class and online, as well as specializedprograms for internationally educated nurses and those re-entering ng the pr<strong>of</strong>ession. We arealso activein applied research– advancing ancing nursing practice and keeping our programsrelevant and up to date.24 care | VOLUME 25 ISSUE 2
esearchNursing Team DynamicsIt’s Time for a Social Revolution!A Masters Degree study recentlyconducted by a CLPNA staff memberhopes to gain insight into nursingteam dynamics and use the informationto benefit the <strong>Licensed</strong><strong>Practical</strong> Nurse pr<strong>of</strong>ession. TeresaBateman, Director <strong>of</strong> Pr<strong>of</strong>essionalPractice, is completing a Masters<strong>of</strong> Arts in Pr<strong>of</strong>essional Communicationat Royal Roads Universityand is in the final stages <strong>of</strong> completionat time <strong>of</strong> press. In Spring2011, she met with LPNs and keyexternal leaders from across <strong>Alberta</strong>to gather information regardingnursing communication.Following is an abstract <strong>of</strong> her study:There is abundant evidence verifying thatpatients benefit when nurses communicatebetter; therefore by improving teamdynamics, patient care will surely be positivelyimpacted, not to mention improvingnurse engagement. Nursing and otherhealth pr<strong>of</strong>essions have been establishedin a hierarchical manner, based on a historicalmodel. In the past, this hierarchywas very evident from the classroom tothe bedside, within the different levels <strong>of</strong>nursing and throughout the interpr<strong>of</strong>essionalhealth care team. Today, healthpr<strong>of</strong>essions and governments focus onthe importance <strong>of</strong> interdisciplinary collaboration,which includes core principles<strong>of</strong> trust and respect among all members<strong>of</strong> the health care team. However, a gapexists between what health pr<strong>of</strong>essionsand organizations say they want for collaborativepractices, and what is occurringin the practice setting.The nursing pr<strong>of</strong>ession must collectivelyexamine and unearth the cultural issuesthat exist at its core to enable a productiveand supportive workforce for the future.Transformation within each nurseand throughout teams is necessary to enacta social revolution in the nursingworld, creating a culture that no longertolerates infighting and counterproductivebehaviors that limit and negativelyimpact nursing careers, patient experiences,and collaborative practice. Thisstudy performs a micro view <strong>of</strong> a macrosized topic area. Through appreciativeinquiry, opportunity for open dialogueemerged, with discussion <strong>of</strong> multiple issuesrelated to team dynamics. A goal <strong>of</strong>this research is to help nurses and teamsunderstand the importance <strong>of</strong> their individualand collective role in creating thenursing culture within their practice environment.Through assessment <strong>of</strong> the dynamics <strong>of</strong>teams, organizational culture, and transformativelearning within the context <strong>of</strong>a health care team, this study examineshow nursing teams communicate by exploringthe experiences <strong>of</strong> licensed practicalnurses (LPNs), key external leaders(KELs), and current literature in the field.The research question: “What is the experience<strong>of</strong> team work and team dynamicsamong members <strong>of</strong> a multidisciplinarynursing team from a <strong>Licensed</strong> <strong>Practical</strong>Nurse perspective?” was posed to 24 licensedpractical nurses (LPNs) and fourkey external leaders (KELs). This teamdynamic study has the potential to impactthe way leaders, managers, pr<strong>of</strong>essionals,and other stakeholders considerhow teams work together.Sincere thanks to all participants, forwithout such eager participation in thedialogue, this research would not havehappened. nA full report on this study and futurerecommendations will be available atwww.clpna.com in the Fall.care | SUMMER 2011 25
esourcesDEMENTIA ANDSLEEP rESoUrcESA team <strong>of</strong> researchers from the University <strong>of</strong> <strong>Alberta</strong> has completeda structured review <strong>of</strong> the evidence for non-pharmacological sleepinterventions for persons with dementia. The review was supportedby the Canadian Dementia Knowledge Translation Network(www.lifeandminds.ca).Shortly, the full report will be available on the website.www.sleep-dementia-resources.ualberta.caThe website will contain a collection <strong>of</strong> evidence-based sleepresources for healthcare providers and caregivers <strong>of</strong> persons withdementia. <strong>Download</strong>able patient education brochures aboutevidence-based sleep interventions will also provided. A PowerPointpresentation on the findings <strong>of</strong> this project and on sleep problemsin persons with dementia can be accessed in the archives <strong>of</strong> theCanadian Dementia Resource and Knowledge Exchange website.www.dementiaknowledgebroker.caFREE pr<strong>of</strong>essionaldevelopment.PROFESSIONAL DEVELOPMENTTRACHelp peoplequit tobacco.TRAC is a two-day program forAHS health pr<strong>of</strong>essionals.LEARN how to talk with your patientsand clients about quitting tobacco.DOUBLE their chances <strong>of</strong> success.SAVE LIVES.Register now!780-422-1350tru@albertahealthservices.caTRAC sessions are availablethroughout <strong>Alberta</strong>.26 care | VOLUME 25 ISSUE 2
at issueReducethe RiskUnderstanding OccupationalHealth & SafetyThere is an increased focus on improvinghealth pr<strong>of</strong>essional’s understanding<strong>of</strong> workplace safety. High injuryclaims by those employed in <strong>Alberta</strong>’shealth service industries shows more education,programs, and partnerships arenecessary to keep nurses safe. However,LPNs who understand their responsibilitiesunder the Occupational Health andSafety Act can help reduce these rates, byprotecting themselves and others.There is always risk <strong>of</strong> injury in nursing.According to “Occupational Injuries andDiseases in <strong>Alberta</strong>” (Government <strong>of</strong> <strong>Alberta</strong>,Summer 2010), within the HealthService sector:• The occupational group in whichLPNs are categorized “AssistingOccupations in Support <strong>of</strong> HealthServices” had twice as many claimsas the next highest group, “NurseSupervisors and Registered <strong>Nurses</strong>”.• Employees in the Long Term Careindustry had the highest lost-timeclaim and disabling injury rates.• Claims for infectious and parasiticdisorders are 12 times the averagecompared with all other sectors.• A high incidence <strong>of</strong> sprains, strains,and tears, especially to the back,accounted for 65% <strong>of</strong> all reportedinjuries. This is 2.4 times greaterthan the average for all sectors in theprovince for lost-time claims.The purpose <strong>of</strong> the Occupational Health& Safety (OH&S) Act is to ensure a safeand healthy workplace through legislation,ensuring compliance, and providingeducation to employees and employers.Employers are responsible to tell employeesabout any workplace hazards, andprovide steps to avoid injury. This willinclude creating and implementing policiesand procedures regarding workplacesafety and injury reporting, WHMIS instructions,and providing Material SafetyData Sheets (MSDS) for hazardous substances.Employees are responsible for obeyingthe health and safety rules for the job,and report any safety concerns to theiremployer. “You can’t be disciplined orfired for following the rules <strong>of</strong> the OccupationalHealth and Safety Act”, statesthe “Occupational Health and Safety Act- Worker’s Guide” (2009: Government<strong>of</strong> <strong>Alberta</strong>, Employment and Immigration)OH&S’s purpose is quite different fromthe Workers’ Compensation Board. TheWCB provides workplace insuranceand rehabilitation services for injuredworkers.LEARN MOREThe Government <strong>of</strong> <strong>Alberta</strong> provides alarge number <strong>of</strong> resources for workers toeducate themselves about workplacesafety at www.worksafely.org:• eLearning Programs:Short interactive videos describing anumber <strong>of</strong> OH&S initiatives. Startwith the “<strong>Alberta</strong> OHS LegislationAwareness eLearning Program”.• Books, Bulletins & Manuals: Readthose oriented to the health serviceindustry such as “Overview <strong>of</strong> BestPractices in Occupational Health andSafety in the Healthcare Industry” or“No Unsafe Lifts”, an importantinitiative designed to reduce thenumber <strong>of</strong> back injuries amongstnurses and care workers.• Video Library: Check out titles like“Be Sure...Be Safe: Safety in theHealthcare Workplace” which usesreenactments to show the hazards <strong>of</strong>working alone in the communitywith aggressive clients and needleuse.• Guidebooks: Guidebooks explaincomplex legislation in simplerlanguage. Try “Occupational Healthand Safety Act - Worker’s Guide”and “Working Alone Safely: A Guidefor Employers and Employees”.• OH&S Magazine: Current andpractical articles about preventinginjury, safety tips, and OH&S newsis released three times per year.Learning more about these issues can beused as a part <strong>of</strong> an LPN’s annual continuingcompetence commitment. SeeCompetency Code C-13 “Safe WorkPractices” and C-14 “Safety Reports andDocumentation” from the CLPNA’s“Competency Pr<strong>of</strong>ile for LPNs – 2ndEdition”. nThis article was funded by an Occupational Health & Safety grant, “Increasing OH&S Knowlege Base in Regulated Health Pr<strong>of</strong>essionals”.care | SUMMER 2011 27
NURTURING NURSES NOWOvercome e the 3 biggestchallenges that keep youOverwhelmed, Over-stressed and Drained! Join “ListenFrom the Inside Out” Author Sharon Carne atthis 2-hourworkshop where you’ll learn scientifically vali-dated Secrets Behind How Soundand Music Can:•RevitalizeeYour OverallEnergy.•Quickly RelieveYourStress.•Significantly ntly BoostYourourImmuneSystem.Tickets are $15FREE when youPre-Register NowCall800.748.4082to leave youremail addressUpcoming Workshops inCalgary, Edmonton, Red DeerWorkshops run 7–9pmHELPING YOU CAREFOR YOURSELFSOYOU CAN CONTINUE TO CAREFOROTHERS. 28 care | VOLUME 25 ISSUE 2
life & death mattersAnorexiaandCachexiaatEnd <strong>of</strong> LifeByKatherine Murray, BSN MA CHPCN(C)andJoshua Shadd, MD CCFPThis is the fourth in a series <strong>of</strong>articles about caring for thedying. Kath Murray, RN, is ahospice palliative care nursewith a passion for education.For further information andonline education, contact her atkath@lifeanddeathmatters.ca orsee www.lifeanddeathmatters.caJoshua Shadd, MD CCFP, isAssistant Pr<strong>of</strong>essor, Centre forStudies in Family Medicine,University <strong>of</strong> Western OntarioDepartment <strong>of</strong> Family Medicine.Jack, 84 years old, was admitted a monthago with declining condition, repeatedchest infections, frequent falls,progressive dementia and lung cancer.Since admission Jack is sleeping more,withdrawn, refusing food and has somedifficulty swallowing.Megan, Jack’s wife, visits daily, bringshomemade custard and encourages Jackto eat. Megan is concerned that if Jackdoes not eat he will die.Jack’s daughter Mary arrived today fromout <strong>of</strong> town. Alarmed by his weight loss,Mary promptly declared, “He is starving!”She believes that decreased nutritionalintake is responsible for his decliningcondition.Eating is a fundamental preoccupation <strong>of</strong>human beings. Food is a basic humanneed. Eating is an indicator <strong>of</strong> life andliving. Many social gatherings andcultural rituals revolve around food andeating as a way <strong>of</strong> “being together”.Feeding someone can communicate love.In light <strong>of</strong> all this, it is to be expected that“food” and “decreasing intake” willfrequently be the center <strong>of</strong> discussion,and sometimes the cause <strong>of</strong> contentionwithin families, between family and thehealth care team, and within the healthcare team in the last months/weeks/days<strong>of</strong> a person’s life. This article gives ideasfor discussing changing needs fornourishment and decreased intake.Need for nourishment changesIt is interesting to see a group <strong>of</strong> peopleeat at a restaurant or at a family reunion.We all require nourishment, but ourneeds change throughout life. The typeand quantity <strong>of</strong> food required to nourishand satisfy a twenty-five year old malewould cause a newborn to choke, and anolder adult to feel bloated or nauseated.Reflect on a time when you had the flu.How was your appetite affected? Wereyou able to eat full meals? How did youfeel if someone pressed you to eat?Statements like the “Simple TruthsAbout Nutrition” (below) remind us thatdeclining intake is a normal part <strong>of</strong>living-dying. Weaving these truths intoconversations about food and intakemay help to normalize the changes.What are anorexia and cachexia?Anorexia at end <strong>of</strong> life is defined as thedecreased interest in food and eating.Cachexia is defined as involuntaryweight loss (more than 5% <strong>of</strong> baseline)with a greater loss <strong>of</strong> muscle than fat.Cachexia is common in advanced cancerand some other severe progressiveillnesses.What causes cachexia?The body’s inflammatory response andtumors produce proteins that decreasemotility <strong>of</strong> the stomach and intestines aswell as increase muscle breakdown. Thisresults in reduced intake and acceleratedweight loss.Do anorexia and cachexiaoccur together?In palliative care, anorexia and cachexiausually occur together. People <strong>of</strong>tenassume that the anorexia (decreasedappetite) causes cachexia (involuntary>care | SUMMER 2011 29
weight loss), but in many cases it appears that the chemistryassociated with cachexia contributes to anorexia.Is this the same as starvation?No. In starvation, the body seeks to conserve energy andnutrients. In cancer-related cachexia, the body spends them evenfaster than usual. In starvation the body uses mostly fat stores toproduce energy, seeking to preserve protein and muscle. Incachexia the body uses mostly protein/muscle stores to produceenergy. In starvation the metabolic efficiency increases and theperson gets “more kilometers per liter <strong>of</strong> gas”. In cachexia, themetabolism is less efficient and the person gets “fewer kilometersper liter <strong>of</strong> gas”.Do nutritional supplements and/or tube feeding help?A review <strong>of</strong> the literature looking at patients undergoing nonsurgicalcancer treatments found that parenteral nutritionresulted in net harm, and voluntary supplements had no effecton mortality.Multiple factors contribute to decreasedappetite and decreased intake:Fatigue, dry mouth, sore mouth, difficulty or painwith swallowing, aversion to food odors/tastes,side effects <strong>of</strong> medications, depression, anxiety,stress, cognitive impairment, and uncontrolledsymptoms such as pain and dyspnea.Gastrointestinal symptoms include: nausea,vomiting, constipation, belching, abdominal pain,smell changes, bloating, food aversions,indigestion, hiccups, taste changes, early satietyand anorexia and cachexia.Dr. Edwardo Bruera,“Tell your patients their stomach is on strike.”Does this mean that it does not matterwhat food we feed Jack?Changes in metabolism mean that the muscles cannot use theavailable nutrients properly. It is useful to encourage patients toeat foods that give them the most nutritious ‘bang for their buck’.Later in the disease, however, when the focus is on food forenjoyment rather than nutrition, it will be more important tocater to the person’s preferences. Food should not become asource <strong>of</strong> stress or conflict.Would medications help increase appetite and energy?Medications can help increase appetite and energy for the shortterm, but do not actually increase muscle and strength. Becausecachexia is caused by a combination <strong>of</strong> many things no singlemedication or treatment will fix all the causes <strong>of</strong> anorexia andcachexia.Will he die sooner because he is not eating?Length <strong>of</strong> life appears to be less about what we do, and moreabout how the disease is affecting the body. Cachexia andanorexia are part <strong>of</strong> his dying process, but will not be the cause<strong>of</strong> Jack’s death. Family may worry that he is dying because heisn’t eating. The reality is that he is not eating because he is dying.Will he be hungry?As healthy adults we may associate decreased intake with hungerpangs and feeling faint. This is not the same for people who aredying. In caring for the dying, we may cause discomfort if food isforced into a gastrointestinal system no longer able to handle it.What else can we do for Dad?Just as you have nurtured your dad through sharing food, youcan nurture him through other shared activities that he enjoys.Massages, music, reading, recording memories, are but a fewsamples. Never underestimate the value <strong>of</strong> just ‘being with’ yourdad.SummaryThe ideas provided here are samples <strong>of</strong> ways nurses might weaveknowledge into conversations with family to help themunderstand decreased appetite and intake. nFull references available at www.clpna.comTRUTHS OF NUTRITIONAT END OF LIFE• What a patient can eat now will become less.• What a patient can drink now will become less.• Both eating and drinking will become zero.• Cessation <strong>of</strong> eating and drinking is natural to thedying process, so also is the ‘fighting’ against it.• What is nutritionally <strong>of</strong> value at one stage is notat another.• ‘Aggressive nutrition’ in the advanced phase <strong>of</strong>tencontributes to difficult symptom control.• ‘What one likes’ becomes more important than‘what is <strong>of</strong> nutritional value’.• ‘What works’ is not necessarily either ‘what onelikes’ or ‘what is nutritional’.• What works is not necessarily what one likes orwhat is ‘right’.• The atmosphere around eating is more importantthat what is ingested.• What is nutritionally right at one stage may be verywrong at another.• Aggressive nutritional therapy in advanced disease<strong>of</strong>ten contributes to difficulty in symptom control.• Food can cause more discomfort than pleasure.Downing, Wainwright (2006).Medical Care <strong>of</strong> the Dying (4th ed.) Victoria Hospice.30 care | VOLUME 25 ISSUE 2
care | SUMMER 2011 31
With CLPNAyou have privilegesFOR YOUR HOME AND AUTO INSURANCE,ENJOY PREFERRED RATES AND EXPERIENCE THE VALUEThanks to The Personal and your association, you haveaccess to home and auto group insurance.Take advantage <strong>of</strong> your benefit.Call or click1-888-476-8737thepersonal.com/clpnaCertain conditions apply.Auto insurance is not available in Manitoba, Saskatchewan or British Columbia due to government-run plans.® Registered trademark <strong>of</strong> The Personal Insurance Company.Finding the right balance for you.Proud to act as legal counsel for the<strong>College</strong> <strong>of</strong> <strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong> <strong>of</strong> <strong>Alberta</strong>32 care | VOLUME 25 ISSUE 2
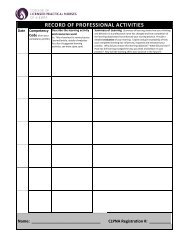
the operations roomMember Information - <strong>College</strong> Activity - Best Practices1 in 5 MembersChosen for ValidationContinuing Competency Program2011 ValidationIn June 2011, this year’s Continuing Competency Program Validation(CCPV) launched. 20% <strong>of</strong> eligible CLPNA members were randomlyselected to complete the program by August 2011. The CCPV annuallymonitors LPN participation in the Continuing Competency Programcompleted during the Registration Renewal process.In keeping with CLPNA’s objective to be environmentally responsible,this year marks the beginning <strong>of</strong> online CCPV. For selected participantswith a valid email address, the CCPV information package was sentby email. Those without an email address will receive the CCPVinformation package by mail.For those requiring copies <strong>of</strong> Continuing Competency Learning Plansfrom 2009 and 2010 Registration Renewal Forms to complete theValidation process, complete the Consent to Release InformationForm from www.clpna.com and enclose the $11 processing fee.Support for members requiring additional help with this year’s CCPV isavailable through several resources. A step-by-step instructional videoand other detailed CCPV information is available at www.clpna.com.If you have further questions or require assistance in completing theCCPV, please contact info@clpna.com or 780-484-8886.2010 ANNUAL REPORT RELEASEDThe enhanced 2010 Annual Report features more informationthan ever about the work <strong>of</strong> the <strong>College</strong> <strong>of</strong> <strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong><strong>of</strong> <strong>Alberta</strong> (CLPNA). Catch the triple-sized Provincial, National andInternational Initiatives starting on page 8. Or read all the detailsfrom the Executive Director, President, Regulatory Services,Conduct, Education, Continuing Competency Program, Practiceand Communications. Highlights were shared at the CLPNA’sAnnual General Meeting on April 6, 2011 in Calgary.Read the 2010 Annual Report online at www.clpna.com on the“Resources” page, or request a complimentary printed copy frominfo@clpna.com, 780-484-8886 or 1-800-661-5877 (<strong>Alberta</strong> only).clpna.comcare | SUMMER 2011 33
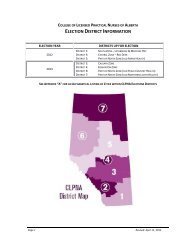
the operations roomLONGTIME LPNINSTRUCTOR & SUPPORTERLAURA CRAWFORD PASSESIt is with great sadness that we share the passing <strong>of</strong>Laura Crawford on Saturday, April 9, 2011. Laura wasa strong, beautiful nurse, who shared her gifts withmany LPNs through teaching and guiding ourpr<strong>of</strong>ession over many years. Since 1994,the Laura Crawford Excellence inNursing Practice Award hashonoured Laura for hercommitment to LPNs.Memorial donationsmay be made to theALS Society <strong>of</strong> <strong>Alberta</strong>.COUNCILELECTIONUNDERWAYDue to a rotating strike by Canada Post,CLPNA District Election ballots were distributedby email in mid-June to CLPNAmembers with Active Practice Permits. There aresix nominees for the Calgary Zone (District 2), sixfor the Edmonton Zone (District 4), and two forPart <strong>of</strong> North Zone (former Peace CountryHealth) (District 6). One nomination was receivedfor Part <strong>of</strong> North Zone (former Northern LightsHealth) (District 7), and will be granted theposition by acclamation. Email ballots must becompleted by June 30.6742531Eligible members who did not receive an emailballot by June 20 should contact Carolyn atcblack@clpna.com or 780-638-6711 with youremail address, full name and CLPNA registrationnumber. Election coverage is available atwww.clpna.com.NOTICEOF 2012REGISTRATIONFEE INCREASEMembers are reminded that the fee for annual Registration Renewal with CLPNA for the2012 registration year will increase to $350 from the current fee <strong>of</strong> $300. This is thesecond <strong>of</strong> two fee increases directed by the Council <strong>of</strong> the <strong>College</strong> <strong>of</strong> <strong>Licensed</strong> <strong>Practical</strong><strong>Nurses</strong> <strong>of</strong> <strong>Alberta</strong> in March 2010. The first fee increase was implemented for the 2011registration year. The Council understands that no one appreciates increased expense;however, the current fee structure has not kept pace with the cost <strong>of</strong> providing mandatedservices. A notification letter with complete details was mailed to members in March 2010.Questions or concerns can be directed to the CLPNA at info@clpna.com, 780-484-8886or 1-800-661-5877 (<strong>Alberta</strong> only).RenewalFor 2012Fees Paid Before December 1 Fees Paid December 2 - 31 Fees Paid January 1$350 $380 $40034 care | VOLUME 25 ISSUE 2
the operations roomLPN RecognitionProgram Launched<strong>Alberta</strong> NursingEducation AdministratorsPreceptor AwardThe <strong>Alberta</strong> Nursing Education Administrators are pleasedto congratulate Laura Pratt, LPN for being the 2011recipient <strong>of</strong> the Leadership in Education Preceptor Award.Laura is currently employed at the Rockyview General Hospitalin Calgary and was nominated for this award by the Coordinator<strong>of</strong> Health Care Aide and <strong>Practical</strong> Nurse Programs at BowValley <strong>College</strong>.For over 4 years, Laura has been preceptoring practical nursingstudents with respect and accountability. Laura’s high standards<strong>of</strong> nursing care make her an exemplary role model. Laurais a true believer in lifelong learning and stimulates her studentsto push themselves to be successful. Her strong clinical backgroundhas allowed Laura the ability to quickly assess students’capabilities and progress in knowledge, critical-thinking, andclinical judgment. She seeks to find learning opportunities forthe student which enhances and supplements the knowledgeand experience they have gained prior to their final practicumwith her. Laura’s students love her. They understand that shehas their best interest at heart, encouraging them to learn moreand work harder. She stimulates them to be self-reflective andabove all, to give excellent nursing care. She is indeed anexemplary leader in nursing education as a preceptor.Congratulations Laura and thank you for the important role youplay in the development <strong>of</strong> capable and confident nurses in<strong>Alberta</strong>.As part <strong>of</strong> the celebrations for NationalNursing Week in May, CLPNA commencedan LPN Recognition Program acknowledgingmembers on significant anniversary datessince graduation and upon notification <strong>of</strong>retirement provided during the annual RegistrationRenewal process. Current memberswill receive a Certificate <strong>of</strong> Recognitionsigned by the Executive Director and thePresident at regular intervals commencingin their 25th year since graduation.Fredrickson-McGregor Education Foundation for LPNsTAKE A COURSE,GET A GRANT!Taking a course to enhance your LPN practice?CLPNA members holding an Active Practice Permit may qualify for anEducation Grant, and receive funding for the cost <strong>of</strong> tuition.APPLICATION DEADLINES FOR COURSE COMPLETION DATES BETWEENJuly 31, 2011 February 1, 2011 and January 31, 2012October 31, 2011 May 1, 2011 and April 30, 2012January 31, 2012 August 1, 2011 and July 31, 2012Grant FAQs (Frequently Asked Questions) and Grant Application Forms atHTTP://FOUNDATION.CLPNA.COMFoundation@CLPNA.com or (780) 484-8886care | SUMMER 2011 35
the operations roomQ.I work in the emergency department <strong>of</strong> the localhospital. Recently my manager asked me to givea tetanus injection to a patient. Is administration<strong>of</strong> tetanus vaccines within my scope <strong>of</strong> practiceas a <strong>Licensed</strong> <strong>Practical</strong> Nurse?The following arefrequently asked questions toCLPNA’s Practice Consultantsby our members, managers,educators, or the general publicthat could provide valuableinformation for you in yourpractice environment.Administration <strong>of</strong> tetanus, flu, and pneumococcal vaccines and allother immunizing agents is a restricted activity under the HealthPr<strong>of</strong>essions Act. LPNs must complete the formal, approvedimmunization course and provide pro<strong>of</strong> <strong>of</strong> certification to receiveauthorization from CLPNA. This advanced education is availablethrough distance or home study. As prerequisites for this course,applicants must have successfully passed an intramuscular andintradermal injection course. Further information on the Immunizationcourse is available on the CLPNA website under “Members”,“Continuing Education”, and “Post-Basic Programs”.Q.We will be expanding our endoscopy capacitywithin our hospital. Can LPNs administerconscious sedation and provide care andmonitoring to clients?<strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong> have a comprehensive competencybase in:1. Health assessment2. Continuous patient assessment, monitoring, andinterventions3. Knowledge, skills, attitudes, and clinical judgment toadminister medicationsLPNs work in complex health care environments as part <strong>of</strong> a team<strong>of</strong> health care providers. When a nursing manager is assigningcare there are three important considerations: The nurse needsto have the knowledge, skills and competence in the care beingassigned; the client assignment must be appropriate to thecompetencies <strong>of</strong> the nurse; and supports must be in place in thepractice setting to ensure quality care. Depending on the nurse,conscious sedation may be a new competency and therefore,employer-led education with theory, supervised lab, and clinicalsupport is important to ensure safe practice.Contact our Practice Consultants atpractice@clpna.com or 780.484.888636 care | VOLUME 25 ISSUE 2
the operations roomMATTERSCONDUCTThis feature is intended toeducate cLPNA membersregarding unpr<strong>of</strong>essionalconduct-related issuesadministered by cLPNA’sconduct Departmentunder the authority <strong>of</strong> theHealth Pr<strong>of</strong>essions Act.*This is a fictionalized casestudy. Any informationassociated with realpeople or events hasbeen changed.A CASE OF SUbSTANCE AbUSEJane Smith’s*co-workers are worried.Smith, a <strong>Licensed</strong> <strong>Practical</strong> Nurse, arrivedat work at XYZ Hospital*looking tired, her speech slurred, andwavering on her feet. She fell asleep duringreport. Her supervisor questionedher and discovered that Smith had takenan unknown number <strong>of</strong> sleeping pills thenight before, far more than prescribed.The supervisor sent her home beforeSmith began working with patients.XYZ Hospital examined Smith’s situation.It quickly came to light that Smithmay be dependent not only upon thesleeping pills but also upon another medicationprescribed to ease panic attacks.Side effects from these medications includedmemory difficulties and cognitiveimpairment. She had also been recentlydiagnosed with depression and anxietydisorders, in addition to substance abuse.The hospital suspended Smith while shedealt with her health issues. Due to thesuspension, XYZ Hospital was compelledto notify the <strong>College</strong> <strong>of</strong> <strong>Licensed</strong><strong>Practical</strong> <strong>Nurses</strong> <strong>of</strong> <strong>Alberta</strong> (CLPNA) asrequired by the Health Pr<strong>of</strong>essions Act.The CLPNA conducted its own investigationinto the complaint. At the sametime, the Complaints Director encouragedSmith to take control <strong>of</strong> her substanceabuse problem. Smith showedresponsibility by completing a residentialtreatment program and by agreeing notto work as an LPN until the disciplinematter was resolved.Smith appeared before a Hearing Tribunal<strong>of</strong> her peers and a government-appointedmember <strong>of</strong> the public. Prior tothe Hearing, Smith and the CLPNAsigned a Joint Agreement regarding thebasic facts <strong>of</strong> the situation and Smithagreed to one allegation <strong>of</strong> unpr<strong>of</strong>essionalconduct, therefore, no witnesseswere called.The Hearing Tribunal reviewed the JointAgreement, deliberated, and returned averdict <strong>of</strong> guilty to the one allegation <strong>of</strong>unpr<strong>of</strong>essional conduct. They agreed tothe orders proposed in the Joint Agreement,to ensure protection <strong>of</strong> the publicand rehabilitation <strong>of</strong> the nurse. The orderswere extensive, including drugscreenings, counselling and follow upfrom Smith’s physicians.This fictional situation shows how personalhealth issues can impact a <strong>Licensed</strong><strong>Practical</strong> <strong>Nurses</strong> pr<strong>of</strong>essional status.First, a suspension from work led to acomplaint to the CLPNA for alleged unpr<strong>of</strong>essionalconduct. The Health Pr<strong>of</strong>essionsAct (HPA) states, “If, because <strong>of</strong> (unpr<strong>of</strong>essional)conduct that in the opinion <strong>of</strong> theemployer <strong>of</strong> a regulated member is terminatedor suspended or the regulated memberresigns, the employer must give notice<strong>of</strong> that conduct to the complaints director.”For more, see the HPA Employer’s Handbookavailable at http://www.health.alberta.ca/documents/HPA-Employers-Handbook-2004.pdf.In this case, the allegation <strong>of</strong> “unpr<strong>of</strong>essionalconduct” related to several HPA definitions.First, “displaying a lack <strong>of</strong>…judgment in the provision <strong>of</strong> pr<strong>of</strong>essionalservices” (HPA, Section 1(1)(pp)(i)). Second,“contravention <strong>of</strong>… a code <strong>of</strong> ethics orstandards <strong>of</strong> practice” (ii), especially Smith’sability to be “accountable to monitor andmaintain (her) own fitness to practice”(CLPNA Standards <strong>of</strong> Practice). Andfinally, “conduct that harms the integrity <strong>of</strong>the regulated pr<strong>of</strong>ession” (HPA, Section1(1)(pp)(xii).Health pr<strong>of</strong>essionals are not immune tosubstance abuse problems. Prescriptiondrugs and alcohol are the most commonlyabused substances among women and forthose in health care positions. The goodnews is that substance abuse is treatable.By taking accountability and action, impacton a health pr<strong>of</strong>essional’s work or registrationstatus can be reduced.If you or someone you know is dealingwith any substance abuse issues, contact<strong>Alberta</strong> Health Services’ 24-hourHelpline at 1-866-332-2322. An extensivelist <strong>of</strong> resources may be found on<strong>Alberta</strong> Health Services website bysearching for “addiction”. ncare | SUMMER 2011 37
the operations roomCLPNA CouncilPresidentHugh PedersenExecutive Director/RegistrarLinda Stangerlstanger@clpna.comDistrict 1 (South Zone)Carla KoyataDistrict 2 (Calgary Zone)Donna Adams - Vice PresidentDistrict 3 (Central Zone)Jo-Anne Macdonald-WatsonDistrict 4 (Edmonton Zone)Sheana MahlitzDistrict 5 (Part <strong>of</strong> North Zone)Lorraine StrelezkiDistrict 6 (Part <strong>of</strong> North Zone)Roberta BeaulieuDistrict 7 (Part <strong>of</strong> North Zone)Alona FortierPublic MembersRobert Mitchell / Allan BuckRalph WestwoodTo contact Council members pleasecall the CLPNA <strong>of</strong>fice and yourmessage will be forwarded to them.CLPNA StaffTamara RichterDirector <strong>of</strong> Operationstrichter@clpna.comTeresa BatemanDirector <strong>of</strong> Pr<strong>of</strong>essional Practicetbateman@clpna.comSharlene StandingDirector <strong>of</strong> Regulatory Servicessstanding@clpna.comOUR MISSIONTo lead and regulate the pr<strong>of</strong>ession in a manner thatprotects and serves the public throughexcellence in <strong>Practical</strong> Nursing.OUR VISION<strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong> are a nurse <strong>of</strong> choice, trustedpartner and a valued pr<strong>of</strong>essional in the healthcare system.The CLPNA embraces change that serves the best interests <strong>of</strong>the public, the pr<strong>of</strong>ession and a quality healthcare system.By 2015, the CLPNA expects to see:• Increased demand for <strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong>generating continuous growth in the pr<strong>of</strong>ession.• Full utilization <strong>of</strong> <strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong> throughout thehealth care system.• All <strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong> embrace and fully enact theirpr<strong>of</strong>essional scope <strong>of</strong> practice.• Increased public understanding <strong>of</strong> the role andcontributions <strong>of</strong> <strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong>.• The <strong>College</strong> initiate and support research relevant to the<strong>Licensed</strong> <strong>Practical</strong> Nurse pr<strong>of</strong>ession and health care system• Enhanced collaborative opportunities provincially, nationallyand internationally.• The <strong>College</strong> and <strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong> fully engagedin all decisions affecting the pr<strong>of</strong>ession.COLLEGE OF LICENSED PRACTICAL NURSES OF ALBERTALinda FindlayPractice Consultant/CCPlfindlay@clpna.comLog Onto clpna.com38 care | VOLUME 25 ISSUE 2• CLPNA Publications• Learning Modules• Competency Pr<strong>of</strong>ile• Job Listings• 2010 Annual Reportand more…CLPNA Office HoursRegular Office HoursMonday to Friday8:30am to 4:30pmClosed forStatutory Holidays
ISSN 1920-633X CAREPublications Mail AgreementNumber 40050295St. Albert Trail Place, 13163 - 146 Street Edmonton, <strong>Alberta</strong> T5L 4S8Telephone (780) 484-8886 Toll Free 1-800-661-5877 Fax (780) 484-9069Return Undeliverable Canadian Addresses To:St. Albert Trail Place, 13163 - 146 StreetEdmonton, <strong>Alberta</strong> T5L 4S8email: care@clpna.comwww.clpna.comCelebrate your chosen pr<strong>of</strong>essionby committing to Talk-the-Walk!Social Media has a pr<strong>of</strong>ound impact today, allowing a forum fordynamic and engaging messaging that you can be involved in.Join the CLPNA via our Social Media campaign.This is about YOU, be part <strong>of</strong> the discussion by:• joining the discussion on our Bloghttp://blog.clpna.com<strong>Licensed</strong><strong>Practical</strong> <strong>Nurses</strong>Talk-the-Walk• following us on Twitterwww.twitter.com/CLPNA• watching us on YouTubewww.youtube.com/CLPNA• liking us on Facebookwww.facebook.com/CLPNAWear your P.I.N.and join the Pr<strong>of</strong>essional Information Network.Your connection with Your Pr<strong>of</strong>ession and Your <strong>College</strong>.