Download PDF - College of Licensed Practical Nurses of Alberta
Download PDF - College of Licensed Practical Nurses of Alberta
Download PDF - College of Licensed Practical Nurses of Alberta
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Come home for a visitWe’re planning a special night for you and your friends.Come sneak-a-peek at the new South Campus.Visit with old friends and make a few new ones.Catch up with your favourite nursing instructor.Come home to your new Bow Valley <strong>College</strong>.RSVP:facebook.com/BVCAA403-355-4666SOUTH CAMPUS GRAND OPENINGAlumni Sneak-a-Peek NightWednesday, April 10 • 4:30 p.m. - 6:30 p.m.345-6 Avenue SE, Calgary AB2 care | volume 27 issue 1
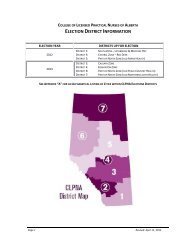
insidespring 2013VOLUME 27 ISSUE 18cover storyRural Nursing in Oyenand Drumheller4 From the <strong>College</strong>6National Nursing ReportGrowth and Untapped PotentialRural nursing blends challengeswith remarkable practice opportunities.This story showcases twoLPNs who have found balancein rural nursing practice, withresulting job satisfaction andcommunity connection.61831Be a Great (and Fun) LeaderDo it Well. Make it Fun.The Operations RoomStay Informed with Member InformationCover Photo:Patricia Stober, LPN - by Chris Fields14featureLPN Research UnveiledThis unique study examinedindividual, team, and organizationalfactors that impact thework <strong>of</strong> LPNs in <strong>Alberta</strong>. Readmore about possible implicationsfor the health care system in<strong>Alberta</strong> and across Canada.CARE is published quarterly and is the <strong>of</strong>ficial publication <strong>of</strong>the <strong>College</strong> <strong>of</strong> <strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong> <strong>of</strong> <strong>Alberta</strong>. Reprint/copy <strong>of</strong> any article requires prior consent <strong>of</strong> the Editor <strong>of</strong>Care magazine. Editor - T. BatemanSigned articles represent the views <strong>of</strong> the author and notnecessarily those <strong>of</strong> the CLPNA.The editor has final discretion regarding the acceptance <strong>of</strong>notices, courses or articles and the right to edit any material.Publication does not constitute CLPNA endorsement <strong>of</strong>, orassumption <strong>of</strong> liability for, any claims made in advertisements.Subscription: Complimentary for CLPNA members, $21.00for non-members.8care | spring 2013 3
from the collegeSYSTEM FOLLOW-UP REQUIREDManaging human resources, especially nurses, in healthcare is a difficult taskmade more difficult by outdated legislation and the lack <strong>of</strong> full-utilization <strong>of</strong> staff.In January, <strong>Alberta</strong> Health Services (AHS) announced a new ‘Patient CareBased Funding’ model for long term care centres. Also announced was the loss<strong>of</strong> 48 <strong>Licensed</strong> <strong>Practical</strong> Nurse (LPN) positions at CapitalCare, Edmonton withimplementation <strong>of</strong> the new model. On January 24, 2013, the Edmonton Journal ireports that Health Care Aides (HCAs) would be hired in place <strong>of</strong> the 48 LPNs,with existing Registered <strong>Nurses</strong> (RNs) taking on the medication administrationand other specific nursing duties.After careful consideration we believe there are core issues that require systemfollow-up.Managing human resources is an ongoing challenge. At the <strong>College</strong> <strong>of</strong> <strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong> <strong>of</strong> <strong>Alberta</strong>(CLPNA), we regularly receive calls from LPNs working in long term/continuing care facilities. These LPNsexpress concerns regarding the high demands in the work setting, ongoing staffing issues, and sheer volume <strong>of</strong>workload that impacts safe quality care by the nursing team. Many LPNs report working short staffed and are<strong>of</strong>ten mandated to do overtime just to maintain regulated nursing care on site. With these issues reported as‘routine’ in some settings, it is difficult to understand why funding changes designed to improve a system wouldcause nursing lay<strong>of</strong>fs in a system already seemingly stressed.<strong>Nurses</strong> should beworking in rolesthat utilize thefull extent <strong>of</strong> theirknowledge, skilland ability.Full utilization <strong>of</strong> care providers is not yet achieved. LPNs have consistently reported that they areunderutilized throughout the system, and although there is a move in <strong>Alberta</strong> to increase utilization,we aren’t there yet. IF LPNs are working in roles that can appropriately be assumed by a HCA thenthe roles should be filled by HCAs. <strong>Nurses</strong> should be working in roles that utilize the full extent <strong>of</strong>their nursing knowledge, skill and ability. CapitalCare CEO Iris Neuman assures CLPNA that theLPNs remaining in their system will be working to full scope. Issues around full utilization are notexclusive to the LPN. <strong>Alberta</strong> research (2009) ii revealed that when LPNs did not work to full scopeon particular care units, neither did the RNs on these same units. Supported by this evidence thequestion should be, if LPNs are doing work that can be done by HCA’s, then are the RNs doing workthat could be appropriately done by the LPN?Legislation guiding decisions is dated. The <strong>Alberta</strong> Nursing Homes Act, Nursing Homes Operation Regulation iii258/1985 (amended 193/2012) guides operators <strong>of</strong> nursing homes in many areas including appropriatestaffing. This regulation, written in 1985, is now a barrier to effective staff utilization, as it does not accountfor the evolution in education, competencies and regulation for all nurses since then. Specifically for LPNs,the Nursing Homes Operation Regulation does not even consider an LPN as a ‘nurse’, but still refers to ourpr<strong>of</strong>ession as Nursing Assistants as per the 1986 Registered Nursing Assistants Regulation. A needed changeto this regulation was highlighted by CLPNA in our presentation to the Ministers Advisory Committee on Healthin October 2009. The 2012 amendment did not address this issue.A funding system based on patient need is logical. Sustainability and equitable access are non-negotiable. Criticalto making it all work is a current legislative framework that recognizes and promotes the unique contribution <strong>of</strong>each nursing pr<strong>of</strong>essional and utilizes the full extent <strong>of</strong> knowledge, skills and ability <strong>of</strong> each member <strong>of</strong> the team.Jo-Anne Macdonald-Watson, President and Linda Stanger, Executive Directori Edmonton Journal. (2013). $3M cut means loss <strong>of</strong> 48 nursing positions at Edmonton’s Capital Care. Retrieved from http://www.edmontonjournal.com/health/means+loss+nursing+positions+Edmonton+Capital+Care/7863115/story.html.ii White, D., Jackson, K., Besner, J., Suter, E., Doran, D., McGillis, L., Parent, K. (2009). Enhancing nursing role effectiveness through job redesign. Calgary Health Region:<strong>Alberta</strong> Health Services. Retrieved from: http://www.calgaryhealthregion.ca/hswru/documents/reports/JobRedesignReportFeb2009.pdfiii Government <strong>of</strong> <strong>Alberta</strong>. (2012). Nursing Homes Act, Nursing Homes Operation Regulation, <strong>Alberta</strong> Regulation 258/1985, with amendments up to and including<strong>Alberta</strong> Regulation 193/2012.4 care | volume 27 issue 1
You stand up for your patients.We stand up for you.<strong>Alberta</strong> Union <strong>of</strong> Provincial Employees. Your Working People.CLIENT:FILE NAME:AD NAME:AUPEAUPE 0760 7x9.625 CLPNA Mag AdWe Stand Up For YouSEND DATE: Feb 07, 2013PUBLICATION: CLPNA MagazineAD SIZE: 7” x 9.625”care | spring 2013 5AD SPECS: 300 DPI, 4C, HI-RES <strong>PDF</strong>DESIGN/PRODUCT: ER
at issueNational Nursing Report ShowsUntapped Potential for <strong>Alberta</strong> LPNs<strong>Licensed</strong> practical nurses (LPNs)employed in nursing grew 29% in<strong>Alberta</strong> in a five year period, yetthe province has the second lowestnumber <strong>of</strong> LPNs per population <strong>of</strong> anyCanadian jurisdiction and fewer thanhalf work full time. These statisticsare according to the annual report onnursing workforce trends from 2007-2011 by the Canadian Institute forHealth Information (CIHI) releasedJanuary 10, “Regulated <strong>Nurses</strong>:Canadian Trends, 2007 to 2011”.GROWING, BUTUNDEREMPLOYED“<strong>Alberta</strong>’s LPNs are highly educated,and have one <strong>of</strong> the most advancedscopes <strong>of</strong> practice in Canada, so we’repleased to see the number employedhas increased nearly 30% in five years,though this report shows they areunder-employed compared to otherprovinces,” states Linda Stanger,Executive Director <strong>of</strong> the <strong>College</strong> <strong>of</strong><strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong> <strong>of</strong> <strong>Alberta</strong>(CLPNA).There were 204 LPNs per 100,000population in <strong>Alberta</strong> in 2011, 17%lower than the Canadian average <strong>of</strong>245. Only British Columbia has fewerat 186. Newfoundland leads with 486LPNs per 100,000.The LPN workforce experienced moregrowth than other nursing pr<strong>of</strong>essions,growing 21% across Canada from2007 to 2011.According to the report, the totalnumber <strong>of</strong> all regulated nurses eligibleto practice “grew almost 10% inCanada between 2007 and 2011”while the “Canadian labour forcegrew by less than 5%”. The numberin <strong>Alberta</strong> grew slightly more, 13%, inthe same period.HIGH PART-TIMEEMPLOYMENT RATELPNs working full-time haveconsistently fallen short <strong>of</strong> nationalaverages since at least 2007. Only44% <strong>of</strong> <strong>Alberta</strong> LPNs worked full-timein 2011, while the national average forall nursing pr<strong>of</strong>essionals is 57%. InOntario, 61% <strong>of</strong> Registered <strong>Practical</strong><strong>Nurses</strong> work full time.With less than average full-timeemployment, <strong>Alberta</strong> LPNs are thesecond largest group in Canada tobe working part time at 42%. TheCanadian average is 35%.“Since most LPNs are working parttime, we see an untapped capacityfor increasing the hours <strong>of</strong> alreadyemployed nurses to ease currentpressures on <strong>Alberta</strong>’s health caresystem,” Stanger emphasizes.CIHI reports that direct patient care isthe responsibility <strong>of</strong> 97% <strong>of</strong> <strong>Alberta</strong>’slicensed practical nurses.“Patients deserve excellence in bedsidenursing, and that’s the forte <strong>of</strong> theLPN pr<strong>of</strong>ession. Increased growthsupports increased quality <strong>of</strong> care for<strong>Alberta</strong>ns,” shares Jo-Anne Mcdonald-Watson, President <strong>of</strong> the CLPNA.YOUNG ANDRECENTLY EDUCATED<strong>Alberta</strong> LPNs remain some <strong>of</strong> theyoungest nursing pr<strong>of</strong>essionals withthe average age <strong>of</strong> 42 years comparedto 44.8 years nationally. A secondindicator <strong>of</strong> youth, years sincegraduation, shows <strong>Alberta</strong> in the leadwith the highest percentage <strong>of</strong> the LPNworkforce under age 30 at 22%. Bothnationally and within the province,LPNs aged 30 or younger were thelargest group within the workforce.Nationally, slightly more than half(52%) <strong>of</strong> all LPNs in the workforcehad graduated within the last 10 years.<strong>Licensed</strong> practical nurses in <strong>Alberta</strong>graduate from a two-year diploma inpractical nursing <strong>of</strong>fered at the collegelevel and are one <strong>of</strong> three regulatednursing pr<strong>of</strong>essions in <strong>Alberta</strong>.MOBILITY TRENDSOnly 5% <strong>of</strong> Canadian LPNs relocatedafter graduation, with most registeringin <strong>Alberta</strong>, British Columbia andOntario in 2011.Internationally educated nursesincreased slightly between 2007 and2011, but comprise less than 3% <strong>of</strong> theCanadian workforce, and only 2.5% in<strong>Alberta</strong>.The <strong>College</strong> <strong>of</strong> <strong>Licensed</strong> <strong>Practical</strong><strong>Nurses</strong> <strong>of</strong> <strong>Alberta</strong> (CLPNA) is theregulatory (licensing) organization for<strong>Alberta</strong>’s 10,000 <strong>Licensed</strong> <strong>Practical</strong><strong>Nurses</strong> (LPNs). CLPNA regulatesthe pr<strong>of</strong>ession by setting entry-topracticerequirements, establishing,promoting and enforcing standards forregistration, practice, and pr<strong>of</strong>essionalconduct. n6 care | volume 27 issue 1
LPN Workforce per 100,000 Populationby Jurisdiction, Canada, 2011YT219CANADA246BC186NWT211NL486*2nd lowestin CanadaAB*204SK265 MB227ON235QU268NB385PEI426NS392LPN WorkforceCanada, 2007 - 2011Percentage <strong>of</strong> LPN Workforce Under Age 30by Jurisdiction and Canada, 201121.5% 22.3% 18.6%69,70974,38076,94481,22484,5879.9%7.7%11.3% 12.0% 18.1%16.3%10.7%10.5% 10.9% 16.9%2007 2008 2009 2010 2011NLPEINSNBQUONMBSKABBCYTNWTCanadacare | spring 2013 7
8Care8by Chris Fields8 care | volume 27 issue 1
Asmall town is like a still pond and big cities like the ocean.Throw a small pebble into the pond and the ripples arenoticeable. Throw a boulder into the ocean and no onewould even notice. You can do small things in small towns thathave more impact and effect than large things you can do inlarge cities.Jason Hull, Blogger, Idaho (paraphrased)Big Country Hospital, Oyen“I thought I would be here for a year,” Patricia (Pat) Stober, LPN says with a laugh asshe talks about working at Big Country Hospital in Oyen for 21 years. “My husbandis from Hanna, and found a job in Oyen ‘close to home.’ In Oyen you don’t leave, oryou leave and come back. It feels like a big extended family: sometimes frustratingbut always there….people who have your back.”There is an irony inherent in working as an LPN in rural healthcare today: “big city”perspective can be tempted to think the rural LPN workload is a bit easier, or tasksaren’t as complex. The truth is more revealing as Pat describes an incident with acomatose diabetic patient in seizure. “I was asked to assist. I quickly got a glucosekit, injected a gluco gun, and got an IV running.” The patient was soon on the mend.“It’s empowering when you know what your role is, your role is deeply respectedwhere you work, you know what to do, and you do it,” Pat says. “It feels really goodwhen you make an immediate difference for a patient.”That doesn’t mean rural healthcare doesn’t have a distinctly rural flavour. Pat talksabout one <strong>of</strong> the nurses walking down the hall one day. “I asked her what the thingthat looked like a tassel was on the back <strong>of</strong> her leg. Turns out it was antelope fur. Amotorcyclist hit an antelope and she had been picking the fur out <strong>of</strong> the chaps.”>care | spring 2013 9
What distinguishes a rural setting is arequirement to work seamlessly as a teamand be a jack <strong>of</strong> all trades – or a “Pat <strong>of</strong>all trades” if you will. Pat mentions acase where a patient came in on a C-spinefollowing an accident. After being sent toMedicine Hat for emergency treatment,the ongoing care provided in Oyen meansPat now has experience with halo care. “Ina rural hospital, your job is like workingin all wards <strong>of</strong> an urban hospital at once,”Pat says.A rural environment means workingwith what you have…and don’t have.Big Country Hospital’s ER is like aregional triage. The hospital doesn’thave equipment like CT/MRI/Scopes,and there are no surgical procedures(sent to Medicine Hat two hours away).Conscious sedation/setting <strong>of</strong> brokenbones, dislocations, biopsies, and theusual coughs and colds are managedlocally. Those sent away for surgeryare typically sent back to Big CountryHospital to recuperate. Home care ismanaged through the facility.But it’s not a quiet ER. Oyen’s locationat the intersection <strong>of</strong> a busy highwayintersection generates many car accidents.A location midway between Calgary andSaskatoon generates stops for those whohave health issues while driving. Somestop at the hospital because the ER waitis 15 to 30 minutes as opposed to a typicalseveral hour wait in urban centres. Pattalks about really busy recent years, wherethe presence <strong>of</strong> 1000 person oil and gasconstruction camps generates injuriesfrom broken bones to burns.The Big Country Hospital’s 10 acutecare beds, 30 long term care beds, and 24hour ER generates a day in the work lifethat feels like those oatmeal variety packboxes in the grocery store. For Pat thattranslates to a 12 hour shift (one LPN andone RN), report first thing in the morningto cover patient needs, breakfast and medsat 8 am, assessment and treatment <strong>of</strong> 8-10outpatients in the ER (shared with RN),all inpatient care including assessments,vitals, charting, meds, injections, ordering<strong>of</strong> lab work if required – and answeringthe phone and doing all departmentpaperwork when the <strong>of</strong>fice staff goeshome at 4 pm. The LPN role has comea long way since 1990 when Pat started,describing her role at that time as a “washand transfer caregiver.” “We had to locatean RN to even take a doctor’s order,” Patsays.<strong>Nurses</strong> play a coordinating role within asmall collaborative team consisting <strong>of</strong> aphysician, RN manager, physiotherapist,and dietary technician. An occupationaltherapist, dietitian, and respiratorytechnician visit once a month fromMedicine Hat. “The team shares thewhole hospital together,” Pat says. “In10 care | volume 27 issue 1
ural environments there’s no one else todo things, and the team has to be strongbecause anything can come throughthe front door.” The fabric <strong>of</strong> workingrelationships is tight knit. Pat has workedwith the same RN for many years, andshe describes their working relationshipas “a left hand for the right hand and viceversa.”The physician in a small town is valued asgold, as evidenced by loss <strong>of</strong> the obstetricsfunction from the hospital when a seconddoctor in Oyen moved away from thecommunity. To the rest <strong>of</strong> the team thatmeans taking on as much responsibilityas possible to lighten the doctor’s loadduring his early morning presence at thehospital and otherwise avoid burnout.One thing that feels more rooted in ruralhealthcare is the human relationship. It’sbeen said that people in small towns,much more than cities, share a destiny.With a resident population <strong>of</strong> 1000 and along history <strong>of</strong> pioneering values whereword is honour, looking one in the eyeis measure <strong>of</strong> honesty and integrity,reputation is everything, and loyalty isgenerational - relationship lies at the soul<strong>of</strong> community life.Given nursing is a heartfelt pr<strong>of</strong>ession,community bonds have a number <strong>of</strong>pr<strong>of</strong>ound implications in a rural setting.“You treat the person you know on afirst name basis (even family members)and then see them downtown or at thepost <strong>of</strong>fice,” Pat says. “People see howyou helped them as a big deal. Trust isimmediate…because it’s been earned byhow people know you in the community,and what you do at the hospital is respectedas core to the fabric <strong>of</strong> community.” Onthe other side <strong>of</strong> the coin, there is noanonymity and you can’t take work hometo your spouse. As Pat says, “Your spousewill know the 70 year old who broke theirarm.”Given nursingis a heartfeltpr<strong>of</strong>ession,community bondshave a number<strong>of</strong> pr<strong>of</strong>oundimplications ina rural setting.Feedback feels more direct and immediate,and appreciation more enduring in a ruralsetting, Pat notes. “Just the other day, aMom I ran into said she had been thinkingabout the day her child was injured…howshe remembered I had climbed on the bedand held her arm to X-ray. She wanted meto know she was glad I was there.”Rural healthcare delivery has a uniqueform <strong>of</strong> patient perspective. “An averagestay might be a little longer than an urbanhospital,” Pat says. “You <strong>of</strong>ten knowwhether they have supports at home ornot or whether they can personally cope.And so sometimes you make a decision todelay a return home just a little, becausethe health <strong>of</strong> the total person in a completecontext is more known.”Emotionally, death touches closer tohome. “Chances are you know a patientoutside the hospital,” Pat says. “You makesure a person doesn’t die alone. You go toevery funeral.”Emotionally, there are also momentselevated by seeing life through the eyes <strong>of</strong>the well-experienced. “I sit by the bed <strong>of</strong>elderly people and they share stories,” Patsays. “They talk about life so different thanours….simpler and more connected…without all the electronic gadgetry thatconfuses our lives….the stories <strong>of</strong> warbrides can be heart wrenching….a womanwho lived in a concentration camptroubled to talk about it even all theseyears later…stories like one would readabout in a book.”That the wise ultimately gauge successfullife by the value <strong>of</strong> friends and familysays something about rural healthcare.Here, there’s time to listen to stories,and “patient” takes on deeper meaninggrounded in small town values. Everyonewants to be heard, with humanity, tohelp bridge over fear <strong>of</strong> being scared andfaceless when most vulnerable.>care | spring 2013 11
The value <strong>of</strong> this form <strong>of</strong> time in healthcarecan’t be described in a chart, but it can bedescribed by heart.Drumheller Health CentreAnother facet <strong>of</strong> the dynamism <strong>of</strong> ruralhealthcare can be seen in the provision <strong>of</strong>home care services. Jackie Wiffen-Peters,an LPN who delivers home care servicesin Drumheller, would like to clear up amisconception that home care is all aboutpill delivery and housekeeping. “Homecare is complex, it’s more acute thanpeople think it is, and it’s becoming morecomplex over time as length <strong>of</strong> hospitalstays are reduced with increasing relianceon home care visits,” Jackie says.Jackie describes a variety <strong>of</strong> home carecases: senior’s health, post-op dressings,cancer follow up, children’s injury trauma,palliative care tube feed dressings, andpalliative medication surveillance. Themajority <strong>of</strong> the job involves wound careand treatment <strong>of</strong> post-op infections.In other words, think <strong>of</strong> home care as “amillion little hospitals,” where peopleare being treated in their homes withconditions that just a few years ago theywould have remained in the hospital for.Jackie notes, “A few years ago, we wouldsee a knee replacement patient twicea week. There would be no injectionsrequired, no dressing, no personal care,and a spouse at home to care for thepatient. Today, we <strong>of</strong>ten treat V.A.C.dressing patients three times a week, andit takes two people an hour to change thedressing given its complexity…purelyhospital treatment not long ago.” Jackiecites other examples <strong>of</strong> more complexhome care treatment, including tube feedsfor cancer patients, PleurX drains for lungcancer patients, wound care for those withmultiple surgeries, those at home betweenHome care is thebridge between- a vital part <strong>of</strong>healthcare thatcares about people’swellness, lifestyle,and frame <strong>of</strong> mind.chemo treatments, post-op crush injurieswith difficult dressings that navigatearound surgical pins and plates, and evena case where a patient whose multiplesurgeries to repair an arm caught in farmmachinery had all post-surgery woundcare done at home.Jackie feels the complexity in home careand the rising numbers receiving theservice is a good thing. “Home care iswellness-driven and thoughtful,” Jackiesays. “Sure – it has a positive bottom lineimpact on healthcare costs, but it’s alsogood for patients. At home people arehappier, less anxious, more comfortable,sleep better, and are where they want tobe….connected to friends, family andthings that matter.” Jackie indicates onecould infer it generates better outcomes.That doesn’t mean our perception <strong>of</strong> homecare is keeping up with reality. “We hada situation recently where we requesteda vitals monitor, and a large monitoron wheels was sent to us,” Jackie says.“Everything we use needs to travel in thetrunk <strong>of</strong> my car.” Jackie adds, “Think <strong>of</strong>healthcare as having three pillars: acutecare; long term care; and home care.Home care is the bridge between - a vitalpart <strong>of</strong> healthcare that cares about people’swellness, lifestyle, and frame <strong>of</strong> mind.”While some patients come into theDrumheller Health Centre for treatment,Jackie’s car is her workhorse, deliveringher to eight or nine home visits per day onfarms, and in towns and villages coveringa swath <strong>of</strong> geography around Drumheller.She says when you first start this kind<strong>of</strong> work the adjustment is a social one.“It feels strange knocking on a door andheading in to someone’s private space. Allpeople are different. You always have tohave eyes open to total home environment,12 care | volume 27 issue 1
isk assessment, and treatment <strong>of</strong> wholeperson not just condition.” “After sixyears, I haven’t seen it all, but I feel atease with what I do,” Jackie adds.“Ease” is a product <strong>of</strong> a strong healthcaredelivery team consisting <strong>of</strong> RNs, LPNs,and Health Care Aides, where Jackieis one <strong>of</strong> a four to five person team onany given day and the “high number<strong>of</strong> years <strong>of</strong> combined experience,” inJackie’s words, yields open, honest andtrusted communication and collaboration.Perhaps reflecting the unique nature<strong>of</strong> home care, but also its increasingcomplexity, the team comes from alldifferent backgrounds and has a wideage range. “It’s like Who Wants To Be AMillionaire,” Jackie says. “Phone a friendis a speed dial function on our phonesif we’re not sure. We fully leverage ourcollective experience.” Jackie jokes theteam is so tight there’s a verbal rule thattwo years notice is required if anyone isleaving.Trust is an important pre-condition foran empowered LPN. One can say Jackiehas earned it with skill, but also the hardearnedway as someone who has seen justabout everything in her 32 years as anLPN – including 15 years in Drumhellerwhere her work experience prior to her sixyear stint in home care looks like a bootcamp for home care fundamentals: acutecare, satellite hemo-dialysis program,nursing home.“Our team are experts in our domain,”Jackie says. “Wound care products havebeen improving and we are on the frontedge <strong>of</strong> knowledge in the area. So we havea kind-hearted chuckle when a doctor’snote requests gauze dressings, and welove it when doctors say ‘please assesswound and treat as required’.”Like Oyen, Drumheller is a place <strong>of</strong>names, faces, and easy recognition. Thenature <strong>of</strong> the work itself – with somecases requiring only one or two visits butmost requiring visits over a span <strong>of</strong> weeksand months, forges more connectivitywith patients. “I’ve had people thankme, while I’m out at a local restaurant,”Jackie says. “People show direct gratitudeand appreciation – which raises your selfperception<strong>of</strong> value and feels good. Buteven as a matter <strong>of</strong> work we do thingsa little differently in rural areas. I leavecards behind after visits and patientsphone me directly and leave a messageon my work cell if they have an inquiryor something they need to discuss. We’reaccessible, accountable, easy to find, andrun with first names….by nature.”Personalized healthcare does haveits challenges, and Jackie’s job has asignificant element <strong>of</strong> palliative care. “Youtake those cases home,” Jackie says. Thatsaid, Jackie is an advocate for patients,helping them get what they need from themedical system, and helping them enablea pathway for inner peace – making thejob as much psychological managementas it is technical caregiving. In Jackie’swords, “I always ask what’s one thing Ican do to make peace for you?” Lots <strong>of</strong>times they just want someone to ask thequestion. Whatever the answer is, I try tomake it happen and no two people havethe same response. Being a peacemakeris so important because the person maybe dying, but life goes on, and that’sespecially important if there are kids inthe house.”Jackie has some parting words <strong>of</strong> wisdomfor young LPNs that reflects the ruralbedrock <strong>of</strong> “treat how you would liketo be treated”: do the whole assessment.“You can’t think you know more thanthe person with a healthcare need,”Jackie says. “And you will never knoweverything. So keep asking questionsbecause one problem may reveal others.Treat the whole person.”Simply complex is a contradictionwith meaning in rural healthcare. It’scomplex acute care that fully stretchestechnical skills. It’s the beauty <strong>of</strong> asimpler life represented by Pat’s eightminute walking commute, or Pat’squestion “You didn’t lock the doorsdid you?” following free parking <strong>of</strong> acar mere metres from the front door<strong>of</strong> the ER entrance. Most deeply, thecomplexity <strong>of</strong> rural healthcare’s “smallpond” ripples with the simplicity <strong>of</strong>earthy human connection we allcrave. n>care | spring 2013 13
Executive Summary:Understanding <strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong>’Full Scope <strong>of</strong> Practice Research StudyIn February 2011, the Office <strong>of</strong>Applied Research at Bow Valley<strong>College</strong> was commissioned by the<strong>College</strong> <strong>of</strong> <strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong><strong>of</strong> <strong>Alberta</strong> (CLPNA) to conducta research study: Understanding<strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong>’ Full Scope<strong>of</strong> Practice. The study was funded by<strong>Alberta</strong> Health (AH), with the goal<strong>of</strong> providing objective, research-basedevidence focused on LPNs in typicalhealth care settings and exploring thefactors that promote and/or inhibitsuccessful LPN scope utilization. Thefollowing questions were investigated:1. What can we learn about LPNs’or inhibits their ability to practiceto full scope? How can supportsbe enhanced? How can barriers bereduced?2. What can we learn about LPNs’work teams and systems thatpromote or inhibit their abilityto practice to full scope? Howcan supports be enhanced? Howcan barriers be reduced?3. What can we learn about LPNs’organizations that promote orinhibit their ability to practiceto full scope? How can supportsbe enhanced? How can barriers bereduced?4. How do these practice-based,system-based, or administrativefactors affect the quality <strong>of</strong> patientcare?The research was guided by a steeringcommittee made up <strong>of</strong> senior representativesfrom <strong>Alberta</strong> Health Services(AHS), AH, the <strong>Alberta</strong> ContinuingCare Association (ACCA), leaders innursing research and nursing education,LPN representatives, and thethree pr<strong>of</strong>essional nursing organizations:the CLPNA, the <strong>College</strong> &Association <strong>of</strong> Registered <strong>Nurses</strong> <strong>of</strong><strong>Alberta</strong> (CARNA) and the <strong>College</strong> <strong>of</strong>Registered Psychiatric <strong>Nurses</strong> <strong>of</strong> <strong>Alberta</strong>(CRPNA). The study involved thefollowing research activities:1. Literature Review: A literaturereview was used to inform themethodological approach forthis study and to identify a range<strong>of</strong> factors most likely to influenceLPNs’ ability to work to their fullscope. Based on findings from theliterature, a Scope <strong>of</strong> PracticeFactors Model was designed,highlighting the role <strong>of</strong> individual,team, client, and organizationalfactors that can influence scopeutilization.2. Survey: Online and mail-in surveyswere distributed to all practicingLPNs who were current members<strong>of</strong> the CLPNA. Based on the Scope<strong>of</strong> Practice Factors Model, thesurvey obtained currentinformation on LPNs in <strong>Alberta</strong>by asking a range <strong>of</strong> questionsabout their practices andperceptions. A total <strong>of</strong> 2313LPNs responded to the survey.3. Case Studies: Six comparative casestudies were performed at sitesacross <strong>Alberta</strong>. Sites were chosenbased on a Scope Indicatorvariable produced from thesurveys. Sites were selected torepresent areas <strong>of</strong> high and lowLPN scope, acute and long termcare, urban and rural settings, andlarge and small facilities. Validatedinstruments used for datacollection at the sites includedinterview and focus groupprotocols for senior managers,team leaders, LPNs, and teammembers. A standardized surveyinstrument was adapted for usewith patients.4. Policy Review: Policy documentswere reviewed and interviews wereconducted with leaders in the<strong>Alberta</strong> Health System, in order toshed light on the policy context <strong>of</strong>the research.The Research ProcessThe study received formal approvalfrom the Community Research EthicsBoard <strong>of</strong> <strong>Alberta</strong> (CREBA), the BowValley <strong>College</strong> Research Ethics Board,and from the five zones in which thecase studies took place. The findingsfrom case studies were validated by thesenior site administrators, and findingswere rolled up in a cross case analysis.After all components <strong>of</strong> the study werecompleted, a data triangulation tablewas constructed, which illustrated the14 care | volume 27 issue 1
consistency <strong>of</strong> findings from the fourdata sources and provided opportunity tosee where findings were congruent withprevious research, while also highlightingnew and contradictory results.Study FindingsStudy results were categorizedaccording to the individual, team,organizational, and system factorsfound to affect LPN scope utilization.Key findings are presented below:Individual factors• There has been an increase in bothperceived and actual LPN scopeutilization compared with earlierstudies, yet a gap between LPNs’perceptions <strong>of</strong> skill utilization and theiractual practice exists.• LPNs varied in terms <strong>of</strong> theircertification (certificate or diploma)and the amount and content <strong>of</strong> postbasiceducation they had attained.More formal education was associatedwith improved nursing competencies,confidence, critical thinking, and mathskills. In long term care facilities,more education was also linked to animproved ability to communicate withresidents and families.• Overall job satisfaction among LPNswas found to be quite high. LPNswho reported using more <strong>of</strong> theircompetencies had a significantly higherlevel <strong>of</strong> job satisfaction. A higherproportion <strong>of</strong> LPNs at low scope casestudy sites reported dissatisfactionwith their job compared with LPNs athigh scope sites.• LPNs were generally motivated totake advantage <strong>of</strong> opportunities forpr<strong>of</strong>essional development, includingtaking on additional competenciesand responsibilities in the workplace.Conversely, a lack <strong>of</strong> motivation onthe part <strong>of</strong> some LPNs to expand theirskill set was seen by coworkers to posea barrier to full scope utilization.Team factors• A lack <strong>of</strong> time and a heavy workloadinterfered with the range <strong>of</strong> skills LPNscould perform. LPNs tended to takeon more responsibilities, in instanceswhere fewer RNs were available onthe unit, such as during night shiftsor when LPNs were called in by unitmanagement as a financial strategy toavoid going into overtime with an RN.• Variability in assignment was usuallylinked to individual team leaders.In acute care settings in particular,assignment was based largely on thepatient’s level <strong>of</strong> complexity• By and large, LPNs were seen bycoworkers as valued members <strong>of</strong> theircare teams. Though there was somevariation in the degree to which greaterLPN scope utilization was embracedby RNs, a number <strong>of</strong> them describedhigher LPN scope utilization as aneffective workforce strategy.• Management and leaders <strong>of</strong>tenprovided opportunities for LPNs topractice new and infrequently usedskills. Variation in understanding andacceptance <strong>of</strong> LPN scope was evidentamong team members and managers.• Collaboration and communicationwere related to the optimization <strong>of</strong> careteam roles, and poor communicationwas a significant barrier. LPNs at highscope sites received guidance, teaching,and mentoring from RNs and otherteam leaders. The value <strong>of</strong> peer supportwas also noted.Organizational factors• Role ambiguity remains a keybarrier to LPN scope utilization.Inconsistencies in the accuracy <strong>of</strong> LPNjob descriptions in relation to their dayto-daywork were frequently noted.• Managerial encouragement for LPNsto enrol in post basic training wasnot always matched by funding and/or formal approval to participate.Post-basic training, pr<strong>of</strong>essionaldevelopment opportunities, andorganizational support for these variedby site.System factors• There is a lack <strong>of</strong> clarity with regardto regulations and policy throughoutthe system, and more direction fromgovernment and/or governing bodieswas sought.• Senior leaders indicated a strongcommitment to policy change withregard to the expanded capabilities<strong>of</strong> the LPN role, and describe it as “awork in progress”.RecommendationsAs a result <strong>of</strong> discussion with the studysteering committee, five broad-basedrecommendations were proposed.These are expected to enable a number<strong>of</strong> strategies related to the utilization<strong>of</strong> LPNs to their full scope <strong>of</strong> practice,which are outlined in the full report. Itis recommended that:1. A strong case to be made to<strong>Alberta</strong> Health to lead the creationand articulation <strong>of</strong> a clear,compelling and shared vision <strong>of</strong>differentiated nursing practice in<strong>Alberta</strong>.2. Regulatory bodies, employers,and individual LPNs assume jointresponsibility and accountability toidentify, provide, and accesslearning opportunities.3. A detailed strategic plan andimplementation plan be developedto assist all players with theirrole in implementing andfacilitating change.4. Research be conducted to studythe roles and opportunities forLPNs in emergency care, familycare clinics and primary care,labour and delivery, mental health,home care, and leadership.5. A knowledge translation plan becreated with input from allstakeholders to ensure that thefindings <strong>of</strong> the study and itsrecommendations are widelydisseminated and used.Authors:Rena Shimoni, PhDProject Director and Co-Principal InvestigatorGail Barrington, PhDCo-Principal InvestigatorContact:Russ WildeDirector, Learning Resource ServicesBow Valley <strong>College</strong>Email: rwilde@bowvalleycollege.caThe full research report can beaccessed at www.clpna.com.CLPNA extends sincere appreciation to theresearch team, steering committee, employers,and participants in this valuable research about<strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong> in <strong>Alberta</strong>.care | spring 2013 15
16 care | volume 27 issue 1
at issueNationalStandard onPsychologicalHealth andSafety in theWorkplaceCanada’s first National Standard on Psychological Health andSafety in the Workplace was released January 16 by the MentalHealth Commission <strong>of</strong> Canada, the Bureau de normalisation duQuébec, and the Canadian Standards Association Group.This is a voluntary standard for employers to promote and preventharm to the psychological well-being <strong>of</strong> workers, including innegligent, reckless or intentional ways. It is not a legal requirement.The Standard was developedfor both employers andemployees, and the principlescan be adapted for any size<strong>of</strong> organization or situation.The <strong>College</strong> <strong>of</strong> <strong>Licensed</strong><strong>Practical</strong> <strong>Nurses</strong> <strong>of</strong> <strong>Alberta</strong>(CLPNA) is developing aPractice Guideline on “Co-Worker Abuse in the Workplace”for release in Springthat will address the NationalStandard.According to the MentalHealth Commission, nearly30% <strong>of</strong> short and longtermdisability claims aredue to mental health problems. The processes to develop a healthypsychological work environment are becoming as necessary as thosefor physical health and safety.“The business case is clear: a work environment that promotes goodmental health is socially responsible, cost effective, and helps attractand keep good employees. It also helps an employer’s bottom lineand contributes to economic prosperity,” states the document’sFrequently Asked Questions.Similar to how employers have legal liability for physical safety,the FAQ’s state that increasingly “employers may be held liableto claims, for example, if an employee is harassed or bullied orchronically overworked.”Several additional tools for employers were also released in support<strong>of</strong> the National Standard, including an animated video and aneducational webinar.The National Standard and related tools are available fromwww.mentalhealthcommission.ca/English/Pages/workplace_guide.aspxcare | spring 2013 17
Managing to Be a Great(and Fun) LeaderBy Ron Culberson, MSW, CSP“Do it Well. Make it Fun.”One <strong>of</strong> the toughest jobs I ever hadwas being a member <strong>of</strong> a committeecharged with cutting ten percent <strong>of</strong>the workforce. Reimbursements weredown and costs were up. The seniormanagement team determined that theonly option left was to eliminate staff.I quickly found that it’s very easy tosee “unnecessary” positions in otherdepartments but it’s very hard to getrid <strong>of</strong> your own people.After several weeks <strong>of</strong> gruelingdecisions, we presented our proposedcuts to the CEO and then he scheduleda series <strong>of</strong> meetings to present the newsto the staff. At the beginning <strong>of</strong> hispresentation, he showed a cartoon <strong>of</strong>a man chasing his head with a butterflynet. The CEO said, “This representsthe senior management team over thepast few weeks.”We sat in stunned silence.The CEO had intended to show, witha touch <strong>of</strong> humor, how difficult thisprocess was. Instead, he insultedeveryone who had been in on theprocess because it made us look like wedidn’t know what we were doing. Thisis a perfect example <strong>of</strong> bad leadershipand bad humor. When combined, itwill sink a leader-ship quicker than amutiny.I believe that humor is one <strong>of</strong> the mostpowerful leadership tools available.Yet most leaders believe that, in orderto be respected, they must be serious.It is certainly important to be a goodleader but not so serious that youare unapproachable and detached.Someone once said, “A leader withouthumor is like a mower <strong>of</strong> a cemetery.He may be doing a good job butnobody underneath is paying muchattention.” The following are someways to add excellence and humor toyour leadership repertoire.LEADERSHIP SKILLSBeing an Excellent LeaderEarly in our lives we are encouraged to“grow up” and to “act our age”. These“encouragements” lead us to believethat we must serious to get the respectand admiration <strong>of</strong> our elders and peers.Unfortunately, getting respect has moreto do with being excellent than serious.An excellent leader is good at leading.An excellent leader works at beinggood at leading. An excellent leadertakes responsibility for the values andskills with which he/she leads. Beforeyou can add humor to your leadershiptoolkit, you must be good at your job.Otherwise, humor will work againstyou.President Dwight D. Eisenhowersaid, “Leadership is the art <strong>of</strong> gettingsomeone else to do what you wantdone because he/she wants to do it.”If you want people to follow your lead,you must have the values and skillsthat inspire them. Know your business.Know your organization. Know yourpeople. And most importantly, knowwhat you do well and what you need toimprove. Then, humor is your friend.UnderstandingWhen First Lady Barbara Bush wasasked to speak to the graduating class<strong>of</strong> Wellesley <strong>College</strong>, a number <strong>of</strong> thegraduates protested because they feltthat Mrs. Bush’s success was a result<strong>of</strong> her husband’s position rather thanher own work. Knowing the discontentshe faced, the First Lady opened herpresentation by saying, “Somewhereout in this audience may be someonewho will one day follow in myfootsteps and preside over the WhiteHouse as the President’s spouse. I wishhim well.”Barbara Bush understood her audiencewell and then used a bit <strong>of</strong> humor towin them over. She received a standingovation and her opponents no longerresented her participation. Greatleaders understand those they lead.By connecting with compassion anda touch <strong>of</strong> humor, those in the rankswill see you as a human being worthfollowing.Communicating EffectivelyWhen my daughter was born, ourpediatrician was explaining the breastfeeding process to my wife and me(not that I had a whole lot to do withit). He said that it usually took a dayor two for the milk to come in. Mywife asked, “What if it doesn’t?” Thedoctor calmly replied, “Then we’ll giveyour daughter to someone whose milkdid come in.”I looked at my wife and gave her a smileand the thumbs up. This doctor was akeeper! With one humorous comment,he communicated that he understoodour concern but that there was no needto be concerned. He also showed usthat he was relaxed and comfortablewith us. We always appreciated thatand looked forward to his care <strong>of</strong> ourchildren.A good leader is able to communicateeffectively in a way that instillsconfidence in those being led. Humoris a wonderfully human way tocommunicate that confidence.18 care | volume 27 issue 1
Role ModelingMany leaders do not realize the power<strong>of</strong> their actions. The CEO <strong>of</strong> a ratherlarge organization was floored whena comment she made to an employeeabout a possible new program fed therumor mill to the point that an all-staffmeeting had to be held to explain thatthis was just an idea mentioned duringa casual conversation and not a planfor the organization.Leaders must set the example for thestaff in the organization. A tense leaderwill have tense staff. A leader with aneffective open door policy will havereceptive staff. A leader with a sense <strong>of</strong>humor will encourage humor amongthe staff.Show staff that you can have funwhile still getting the job done. At astaff retreat, we had developed groundrules for our behavior which includedthings like “Be respectful”, “Don’tinterrupt” and “Give others the benefit<strong>of</strong> the doubt”. In order to reinforce theground rules, our CEO purchased aNerf gun. Each <strong>of</strong> us took a turn beingthe “enforcer” <strong>of</strong> the ground rules.Every time someone broke a groundrule, they were shot! It was a great funway to avoid the tension associatedwith the confrontation.The Work EnvironmentA FUN MissionWhen I worked in hospice care,we spent two years working on theMission, Vision, and Values. It was animportant process because it wouldguide the organization into the future.As one <strong>of</strong> the values, we picked joiede vi which is French for “joy <strong>of</strong> life”.This phrase included fun, humor, joy,happiness, etc. and captured the essence<strong>of</strong> what we wanted our organization tobe. Whereas we provided care for thedying, we valued living.Consider incorporating some humorrelated value in your mission. If yourorganization strives to be a “fun placeto work” or you encourage staff to have“fun with those we serve” or to “neverlose our sense <strong>of</strong> humor”, you will findthat the organization will continue tomove forward with a positive attitude.Hiring the Right PeopleSouthwest Airlines CEO Herb Kellehersaid, “We hire for attitude and thenteach the skill.” Kelleher knew theimportance <strong>of</strong> the right attitude forthe work environment. An employeecan always improve upon his/her skillswhile attitudes are hard to change. Andan employee with a bad attitude willquickly disrupt the work environment.When hiring new staff, most employerswant to know what degrees they have,where they have worked and whatskills they have. Rarely do we askpeople if they have a sense <strong>of</strong> humoror how they might use humor to copewith a stressful situation.Which <strong>of</strong> the following qualificationsdo you think is more important in newemployee?• Graduated magna cum laude atriple major.• Scored in the top 25% on all <strong>of</strong>their aptitude tests.• Has excellent writing skills.• Has a sense <strong>of</strong> humor and managesstress well.Interestingly, research has shown thatemployees with a sense <strong>of</strong> humor areperceived to do a better job becausethey are less rigid, more flexible and lessstressed out. It’s definitely something toconsider in every job interview.Making the WorkplaceMore FUNctionalIn addition to finding the right people,you must create a work environmentthat both embraces excellence and isa fun place to work. One definition<strong>of</strong> work I saw recently was, “If you’drather be doing anything else.” It’sa shame that we spend so much timeat work and still view its drudgery asnormal.There are several things you can do tomake the work environment more funfor your employees. Consider theseideas:• Create humor respite centers.Allow your staff to create a placefor humorous materials such ascartoon boards, bookshelves andprops (Koosh balls, stress balls,yo-yos, etc.). They can visit theseplaces when the stress gets too high.• Party hearty. Celebrate thosespecial events in your work lives.Celebrate employment anniversaries,pr<strong>of</strong>essional months (fornurses, social workers, administrativeassistants, etc.), accomplishments,and anytime you getthrough a tough situation. Makesure the celebrations include games,prizes, fun, food and fellowship.• The signs <strong>of</strong> humor. An easy wayto make the workplace more funis by putting up humorous signs. Amanager put a “Mood Meter” onhis door with an arrow that pointedto a picture <strong>of</strong> a river when he wascalm and a volcano when he wasstressed. It was a fun way to say“keep away”! Another organizationused baby pictures on the staff<strong>of</strong>fice doors. These fun signs createa nice environment for employees.• Reward humor. Rewarding goodbehavior encourages it to continue.Even if there is no budget forrewards, make sure you recognizegood behavior, new employees andthose who move on (assumingthey’re not being fired!). Considercreative recognitions such asnaming a hallway for the employee<strong>of</strong> the month, making a donationto a charity, baking brownies oreven washing the person’s car.Make the reward specific and fun.Excellence combined with humor isa powerful leadership duo because itproves the competence <strong>of</strong> the leaderwhile bringing out his/her humanity.Once you have established the valuesand skills needed to be a great leader,humor can be just the added benefit toinspire and motivate those you lead. n© 2012 Ron Culberson. This information maybe copied and shared as long as the followinginformation is included:Ron Culberson, MSW, CSP is a formerhospice social worker, middle manager, andsenior manager who helps mission drivenorganizations tap into the power <strong>of</strong> combiningexcellence with humor. Ron is the author <strong>of</strong> Doit Well. Make it Fun., Is Your Glass Laugh Full?,and My Kneecap Seems Too Loose.Find out more by visitingwww.RonCulberson.comcare | spring 2013 19
2013 CLPNA SPRING CONFERENCEApril 17-19, 2013Rimrock Resort Hotel - Banff, <strong>Alberta</strong>This year’s conference promises to bring togethernurses, colleagues, and stakeholders to uniquelyexamine the whole patient through mental, physical,spiritual, emotional, and psychosocial elements.Participants will breathe the fresh spring mountain airin Banff, <strong>Alberta</strong>; explore deeper components <strong>of</strong> healthcare best practices; and consider the connections <strong>of</strong>body, mind, and spirit.CLPNAAnnual GeneralMeetingApril 17, 2013 at 4:30 pmRimrock Resort Hotel – Banff, <strong>Alberta</strong>20 care | volume 27 issue 1
Speaker HighlightsOnline Registrationcloses April 10thwww.clpnaconference.comLPN ‘Full Scope <strong>of</strong> Practice Research’ – A Stakeholder Panel DiscussionIn this panel presentation, the lead researchers for the CLPNA research project “Understanding <strong>Licensed</strong><strong>Practical</strong> <strong>Nurses</strong> Full Scope <strong>of</strong> Practice” will present the study findings, and the recommendations will beposed for discussion to key leaders in health care administration, including government, employers, regulatorycolleges, and educators. An open microphone will allow questions and comments during this session.Dr. Arya SharmaBe sure to catch Dr. Arya Sharma’s plenary address, 5As <strong>of</strong> ObesityManagement: The Body – Mind – Spirit Connection, a practical approachto obesity assessment and management. Dr. Sharma is a Pr<strong>of</strong>essor andChair in Obesity Research and Management at the University <strong>of</strong> <strong>Alberta</strong>,the Medical Director <strong>of</strong> the Edmonton Regional Bariatric Program andScientific Director <strong>of</strong> the Canadian Obesity Network.Tammy RobertsonTammy Robertson, Calgary motivational speaker and lifecoach, believes that the essence <strong>of</strong> our challenge today iscaptured in one simple message, “Get Your Heart in theGame!” Tammy inspires you to step into your best life andto be more purposeful and passionate about your life andleadership.Apply for $100 OffYour Registration Feemore info onlinewww.clpnaconference.comcare | spring 2013 21
Advanced Education inOrthopaedics Certificatefor LPNsNorQuest’s Advanced Education in Orthopaedics certificatewill open doors for you and provide many opportunities.Learn about advanced orthopaedic assessment, traumaand specialized procedures including casting.For more information, call 780.644.6366 or emailortho@norquest.caTo register, call 780.644.6000 or toll-free 1.866.534.7218Step Forward | norquest.cawww.gss.orgWe Need <strong>Licensed</strong><strong>Practical</strong> <strong>Nurses</strong>!FULL TIME, PART TIME AND CASUAL POSITIONSAre you a LPN looking for a position that <strong>of</strong>fers competitivewages, comprehensive benefits, a variety <strong>of</strong> shifts, and theopportunity to improve the quality <strong>of</strong> life for individualsand their families?The Good Samaritan Society is always looking for skilledLPNs who can deliver quality resident care. As one <strong>of</strong>Western Canada’s largest voluntary, not-for-pr<strong>of</strong>it,caregiving providers, we believe that a balanced worklife contributes to healthy and happy employees,who in turn provide the best care to our residents,which is what matters to us the most.• Visit www.gss.org to view all our jobopportunities• Please submit all resumes to:careers@gss.orgThe Good Samaritan Society is an equal opportunity employer.We encourage applications from all qualified individuals registeredwith CLPNA who have current First Aid and CPR.22 care | volume 27 issue 1
esearchUnderstanding Healthcare Provider Barriers to Prescribingand Recommending Non-pharmacological SleepInterventions for Persons Diagnosed with DementiaBy CA Brown (PI) 1 , P Wielandt 1 , D M Wilson 2 , A Jones 3 , M Bullock 1 , K Crick 3(1Department <strong>of</strong> Occupational Therapy, 2 Faculty <strong>of</strong> Nursing, 3 Department <strong>of</strong> Physical Therapy, University <strong>of</strong> <strong>Alberta</strong>, Edmonton, Canada)This project was completed by theSleep and Function InterdisciplinaryGroup (SAFIG) <strong>of</strong> the Faculty <strong>of</strong>Rehabilitation Medicine, University <strong>of</strong><strong>Alberta</strong>. This research group was ledby Dr Cary Brown, Associate Pr<strong>of</strong>essor,Department <strong>of</strong> Occupational Therapy,Faculty <strong>of</strong> Rehabilitation Medicine,University <strong>of</strong> <strong>Alberta</strong> (cary.brown@ualberta.ca). The project was fundedthrough the Addiction & Mental HealthResearch Partnership Program: <strong>Alberta</strong>Health Services (AHS) (http://www.albertahealthservices.ca/2770.asp).Executive SummaryFor persons with dementia (PWD),sleeping problems are <strong>of</strong>tenunrecognized and undertreated. This isa concern for two reasons: disorderedsleep may contribute to the onset <strong>of</strong>their dementia and a lack <strong>of</strong> restorativesleep can negatively impact the healthand functioning <strong>of</strong> both the personliving with dementia and their familycaregivers. Early identification andappropriate intervention for sleepproblems can help reduce the risk<strong>of</strong> dementia onset and/or slow theacceleration <strong>of</strong> the illness.Presently, the relationship between sleepand dementia is not well understood bymost healthcare providers and familycaregivers <strong>of</strong> PWD. Traditionally,sleep problems have been treatedwith medication, but this can cause arange <strong>of</strong> side effects. Although thereare evidence-based interventionsfor sleep disorders that are nonpharmacologicalthese interventionsare not routinely recommended knownto healthcare workers because <strong>of</strong>a prevalent research-to-action gap.Consequently healthcare providerslack the knowledge required to makerecommendations to family membersabout pragmatic sleep interventionsfor PWD. Addressing this gap throughevidence-based knowledge translationand exchange (KTE) strategies willultimately contribute to improvedhealth and quality <strong>of</strong> life for bothPWD and their family caregivers. Inturn, optimal health and functioningare positive influences supporting thepriority goal <strong>of</strong> PWD and their familycaregivers remaining able to live safelyand with quality in their own homes.The first step in addressing thisknowledge-to-action gap is todetermine the current state <strong>of</strong> sleepassessment and intervention practice<strong>of</strong> healthcare providers workingwith PWD. Knowing this helps laya strengths-based foundation formore targeted KTE and educationalstrategies addressing sleep problemsfor PWD. This study, Understandinghealthcare provider barriers toprescribing and recommending nonpharmacologicalsleep interventionsfor persons diagnosed with dementiagathered quantitative and qualitativesurvey data from 2,027 healthcareproviders from across Canada. Therespondents to the survey representeda wide range <strong>of</strong> pr<strong>of</strong>essional groups>care | spring 2013 23
working in both institutional and community settings.These findings present a clear picture <strong>of</strong> current knowledgeand practices. Additionally, the findings illustrate whathealthcare providers perceive to be barriers and facilitatorsto applying the sleep and dementia evidence-base to theirpractice. Finally, and very importantly, the survey highlightswhat KTE strategies healthcare providers identify as beingmost effective for helping reduce the sleep and dementiaresearch-to-action gap that currently exists.The full report reviews the background literaturehighlighting the impact <strong>of</strong> disordered sleep on dementia,outlines the study design, presents the findings <strong>of</strong> the surveyand discusses the implications <strong>of</strong> these findings. A series <strong>of</strong>sixteen action points (Table 13 in the full report and at theend <strong>of</strong> this report) emerged to help guide further evidencebasedaction targeting the sleep and dementia KTE needs <strong>of</strong>Canadian healthcare providers.Encouragingly, the study shows healthcare providerswant to learn more about disordered sleep and nonpharmacologicalsleep interventions. This is a key strengthupon which efforts to address sleep KTE needs <strong>of</strong> healthcareproviders can move forward and thereby improve healthand well-being <strong>of</strong> PWD and their families.Implications <strong>of</strong> the Study:• There is a research-to-knowledge gap regarding howinterventions for disordered sleep can reduce the risk orlessen the severity <strong>of</strong> dementia, possibly leading togreater independent living in the community.• Healthcare providers are not well informed aboutthe risk factors <strong>of</strong> disordered sleep in older adults withdementia.• The present practice for assessment is not routine, sleeprelated issues may be followed up if they emergein other assessments but little awareness <strong>of</strong> existing,standardized assessment exists.• Barriers and facilitators exist to incorporatingassessment and treatment <strong>of</strong> disordered sleep into thedaily practice <strong>of</strong> healthcare providers. With knowledge<strong>of</strong> the range <strong>of</strong> facilitators and barriers KT strategiescan be selected and modified within the parameters <strong>of</strong>local context so as to increase the likelihood <strong>of</strong>meaningful change.• Healthcare providers lack awareness about thepublic health and societal implications <strong>of</strong> untreatedsleep problems in older adults with dementia.• Learning new information regarding disordered sleepneeds to be contextualized and reflect individuallearning preferences.• Healthcare providers are eager to learn aboutassessment and treatment <strong>of</strong> disordered sleep in olderadults with dementia with non-pharmacologicalmethods.This study can inform the topic by:1. Targeting specific areas within and across healthcarepr<strong>of</strong>essions where information is significantly lacking.2. Linking the recommendations to build on the existingstrengths <strong>of</strong> healthcare providers.Our findings align with the Canadian Institute for HealthResearch (CIHR) Knowledge-to-Action Cycle andparticularly the taxonomy <strong>of</strong> barriers and facilitators forknowledge use that Légare developed based on his review<strong>of</strong> the extant KT conceptual models. These foundationalworks helped us identify the key findings from our surveyas they relate to the goal <strong>of</strong> recommendations to increasehealthcare providers’ knowledge and use <strong>of</strong> NPSI forpersons with dementia. nSummary <strong>of</strong> Action Points to ImproveSleep and Dementia KTE Outcomes:• Build sleep problem screening and advocacycapacity in the healthcare providers who spend themost time with persons with dementia.• Make sleep a higher priority topic for education <strong>of</strong>healthcare providers.• Educate healthcare providers about the effect<strong>of</strong> caregiver beliefs and co-morbid conditions ondisordered sleep for persons with dementia.• Educate healthcare providers about effectivenon-drug sleep interventions.• Tailor healthcare providers’ education to fill thespecific knowledge gaps <strong>of</strong> each discipline.• Educate caregivers to facilitate a change intheir beliefs and awareness <strong>of</strong> effective non-druginterventions for disordered sleep.• Improve sleep screening and assessment by: 1)embedding sleep-related questions in genericelder-care screening tools, and 2) improving accessto appropriate sleep assessment tools.• The priority requirements for delivering effectiveknowledge translation strategies to reduce theresearch-to-practice gap are:a. Customize to local context.b. Incorporate a range <strong>of</strong> formats for learners’preferences.c. Develop strategies based on an awareness <strong>of</strong>organizational culture.d. Respect and build on prior knowledge.e. Avoid ageist assumptions <strong>of</strong> communicationmethods.f. Focus on evidence-based principles forincreased health literacy.g. Focus on practicality <strong>of</strong> the information.These recommendations can be applied by policymakers and healthcare educators to develop specificeducational strategies and care guidelines to improvehealthcare providers’ ability to provide the best,research informed, care for older adults living withsleep problems and dementia.For a full copy <strong>of</strong> the report and references go tohttp://www.sleep-dementia-resources.ualberta.caand click on the “new” button on the home page.24 care | volume 27 issue 1
care | spring 2013 25
esources<strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong> in <strong>Alberta</strong>A Career GuideLPN CareerGuide solvesnewcomer’sconfusionA48-page Career Guide was released in March by the CLPNA to inform potential students,internationally educated nurses, and applicants from other provinces about the <strong>Licensed</strong><strong>Practical</strong> Nurse pr<strong>of</strong>ession in <strong>Alberta</strong>. The guide provides foundational information about thepr<strong>of</strong>ession, the work, the regulations, the province, and discovering the opportunities in nursing.“In 2012, we registered 620 applicants coming from outside <strong>Alberta</strong>, communicated withhundreds more, and that number is rising. Pursuing a nursing career is difficult when you don’tknow how everything fits together leaving people with many questions: What colleges providenursing education? What competencies areexpected on the job? How do you register?How do you find work? The Career Guidetakes the puzzle out <strong>of</strong> those questions,” saysLinda Stanger, CLPNA Executive Director.Rounding out the guide are five storiesabout LPNs on the job. Ranging from bigcityhospitals and rural mental health, toassisted living facilities and primary carecentres, the articles show the breadth <strong>of</strong><strong>Alberta</strong> LPN roles. “Some may be surprisedat what <strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong> can do in<strong>Alberta</strong>. We have one <strong>of</strong> the broadest scopes <strong>of</strong> practice in Canada which leads to all kinds <strong>of</strong>opportunities,” Stanger reveals.Production <strong>of</strong> the guide was made possible through a grant from <strong>Alberta</strong> Employment andImmigration, Foreign Qualification Recognition branch.Discover it at www.clpna.com or directly at http://issuu.com/clpna/docs/career_guide.The online edition contains links to additional resources.26 care | volume 27 issue 1
Source: <strong>Alberta</strong> Centre for Active Living, reprinted with permission.care | spring 2013 27
Educate. Inspire. Engage.The next generation <strong>of</strong> nurses are looking toyou. Red Deer <strong>College</strong> has excellent teachingopportunities available within our NursingDepartment for 2013/2014. We <strong>of</strong>fer:• Bachelor <strong>of</strong> Science in Nursing, <strong>Practical</strong> Nurseand Health Care Aide programs• Small class and clinical group sizes• Mentoring and coaching for new instructors• Exceptional pr<strong>of</strong>essional developmentJoin our Learning Community– Apply today!403.314.2451 | www.rdc.ab.ca/employmentFor the right fit, switch to The Personalfor your home and auto insurance.For every insurance quotecompleted by a CLPNA member,The Personal is donating $5to the Fredrickson-McGregorEducation Foundation for LPNs.Get a quote1-888-476-8737thepersonal.com/clpnaYour exclusivegroup rate in as littleas 10 minutes.As a member <strong>of</strong> the <strong>College</strong> <strong>of</strong> <strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong><strong>of</strong> <strong>Alberta</strong>, you already qualify for exclusive group rates andbenefits on your home and auto insurance.Certain conditions apply. The Personal refers to The Personal General Insurance Inc. in Quebec and The PersonalInsurance Company in all other provinces and territories. Auto insurance is not available in Manitoba, Saskatchewanor British Columbia due to government-run plans.The right fit.28 care | volume 27 issue 1
esearchHQCA finds 64% <strong>Alberta</strong>ns Satisfied with Healthcare ServicesThe Health Quality Council <strong>of</strong> <strong>Alberta</strong>(HQCA) released the results <strong>of</strong> itsbiennial survey <strong>of</strong> <strong>Alberta</strong>ns’ satisfactionand experience with healthcareservices. Overall, 64% <strong>of</strong> <strong>Alberta</strong>ns weresatisfied with healthcare services, comparedto 62% in 2010. Most results in the2012 survey remain relatively unchangedcompared to the 2010 survey.The survey <strong>of</strong> 4,803 <strong>Alberta</strong>ns consists<strong>of</strong> more than 100 questions garnering respondents’general perceptions <strong>of</strong> healthcareand actual healthcare experiences, aswell as satisfaction with specific healthservices province-wide.The factors that most influence <strong>Alberta</strong>ns’overall satisfaction, in order <strong>of</strong> influence,are:• ease <strong>of</strong> access to healthcare services(51% rated access as easy)• quality <strong>of</strong> healthcare services (77%rated quality as good or excellent)• how well all healthcare pr<strong>of</strong>essionalscoordinate their efforts to servepatient needs (49% rated coordinationas very good or excellent)• handling <strong>of</strong> serious complaints (20%are satisfied with complaintshandling)• satisfaction with emergency departmentservices (59% are satisfied withemergency department services)• satisfaction with family doctorservices (84% are satisfied withfamily doctors)• satisfaction with specialist services(80% are satisfied with specialistservices)“It is important to examine the factors thatinfluence <strong>Alberta</strong>ns’ satisfaction so thathealth policy makers and health serviceproviders can take into considerationwhat <strong>Alberta</strong>ns are saying about theirhealthcare experiences,” says Dr. JohnCowell, Chief Executive Officer, HQCA.“Coordination <strong>of</strong> care, for example,is one <strong>of</strong> the top three most influentialfactors driving overall satisfaction, andyet we have not seen improvements inthis area in any <strong>of</strong> the six surveys we haveconducted since 2003.”Less than 50% <strong>of</strong> respondents in 2012rated how well healthcare pr<strong>of</strong>essionalscoordinated their efforts to servetheir needs as very good or excellent.Information in a recent Health Council<strong>of</strong> Canada (HCC) report from a survey <strong>of</strong>primary care physicians complements theHQCA findings. For example, the reportstated that only 13% <strong>of</strong> <strong>Alberta</strong> primarycare physicians receive information forcontinued management <strong>of</strong> their patientswithin 48 hours <strong>of</strong> hospital discharge.Information from the HCC report inrelation to access to healthcare servicesalso mirrored the HQCA’s patientexperience results. The report stated thatonly 41% <strong>of</strong> primary care physicians in<strong>Alberta</strong> say they have an arrangement fortheir patients to see a physician or nursewhen the practice is closed, other than ahospital or emergency department.“In the almost 10-year history the HQCAhas been conducting this biennial survey,we have seen a change from 52% to 64%in how <strong>Alberta</strong>ns rate their satisfactionwith healthcare services,” adds Dr.Cowell. “It is worthy to note that atthe same time, while the populationhas grown 22%, adjusted public healthexpenditures per person in <strong>Alberta</strong>,reported by the Canadian Institute forHealth Information, have increased from$3,994 per capita in 2003 to a forecast<strong>of</strong> $6,570 per capita in 2011 - a 64%increase.”Other key findings:• Respondents in <strong>Alberta</strong> Health Services’North zone were significantly less likelyto be satisfied with healthcare services(56%) as compared to the overall ratingfor <strong>Alberta</strong> (64%).• When asked about experiences <strong>of</strong>unexpected harm, 11% <strong>of</strong> respondentsreported that they or an immediatefamily member experienced harm whilereceiving healthcare sometime in the pastyear, which is significantly more than2010 (9%), but less than 2003, 2004,and 2006.• 28% <strong>of</strong> <strong>Alberta</strong>ns have never had a flushot. The North zone has significantlymore respondents who have never had aflu shot (38%) compared to Edmonton(27%), Central (31%), Calgary (26%)and South (26%) zones. The mostcommon reason respondents reportedthey did not have the flu shot in the pastyear is because they did not think it wasnecessary (47%), followed by they hadnot gotten around to it (21%).• Results were analyzed by <strong>Alberta</strong>ns’self-reported health status to comparethe experience <strong>of</strong> those categorized as lesshealthy to those categorized as to be ingood health. The respondents’ state <strong>of</strong>health greatly influenced how they ratedtheir experience. For example, <strong>Alberta</strong>nsin good health were most likely to besatisfied with healthcare services received(71%), and respondents consideredthe least healthy were less likely to besatisfied (56%) – both ratings differedsignificantly from the overall satisfactionrating <strong>of</strong> 64%.Satisfaction and Experience withHealthcare Services: A Survey <strong>of</strong><strong>Alberta</strong>ns 2012 measured responsesfrom 4,803 <strong>Alberta</strong>ns who were 18 years<strong>of</strong> age and older, and had a land-linetelephone. To ensure respondents wererepresentative <strong>of</strong> <strong>Alberta</strong>ns, quotas wereset for age and gender groups within each<strong>of</strong> the five <strong>Alberta</strong> Health Services’ zones.Some questions were limited to only therespondents who had an experience withthe healthcare system in the previous12 months. Survey weights were usedto make the results more representative<strong>of</strong> the population. Where possible, theHQCA’s independent survey comparesthe 2012 results with those from 2010,2008, 2006, 2004 and 2003.The 2012 survey is <strong>of</strong> interest becauseit can be compared against benchmarkresults from 2010, which was the firstyear the HQCA measured satisfactionand experience since the formation <strong>of</strong><strong>Alberta</strong> Health Services. nThe technical report and a summary <strong>of</strong> thefindings are available at www.hqca.ca.care | spring 2013 29
CLPNA sends out the majority <strong>of</strong> its noticesand nursing news by email. Don’t miss out!12STEPS TO GET CLPNA EMAIL:GO to “Members/Applicants Login” atwww.clpna.com. “View Pr<strong>of</strong>ile”.“Edit” your email address.CLICK THE “Sign Up for Email Updates”button at www.clpna.com.>> LEARNINGLINKS<strong>Alberta</strong> Gerontological <strong>Nurses</strong> Associationwww.agna.ca<strong>Alberta</strong> Hospice Palliative Care Associationhttp://ahpca.ca<strong>Alberta</strong> Innovateswww.albertainnovates.ca/healthCanadian Agency for Drugs andTechnologies in Healthwww.cadth.caCanadian Association <strong>of</strong> Neonatal <strong>Nurses</strong>www.neonatalcann.caCanadian Association <strong>of</strong> Wound Carewww.cawc.netYou’ve Got Mail!Canadian Orthopaedic <strong>Nurses</strong> Associationwww.cona-nurse.orgCanadian Hospice Palliative Care <strong>Nurses</strong> Groupwww.chpca.netCanadian Virtual Hospicewww.virtualhospice.caCommunity Health <strong>Nurses</strong> <strong>of</strong> <strong>Alberta</strong>www.chnalberta.caCreative Aging Calgary Societywww.creativeagingcalgary.caEducation Resource Centre for Continuing Carewww.educationresourcecentre.caJohn Dossetor Health Ethics Centrewww.ualberta.ca/bioethicseducation grants for post-basic courses.• Foot Care• Gerontology• IM/ID InjectionsMental• ImmunizationHealth• Infusion TherapyspyOrthopedicsPalliative CareApply Today!Research& MORE!FOUNDATION.CLPNA.COMpply today!$1000/YRin LPN education grantsAvailable to <strong>Alberta</strong> LPNs in education grants for post-basic courses.Some <strong>of</strong> the eligible courses include:• Leadership• Mental Health• Orthopedics• Palliative Care• ResearchApplication Forms & FAQ’s atFoundation@CLPNA.com or 780.484.8886Fredrickson-McGregor Education Foundation for LPNsMount Royal Universitywww.mtroyal.caNational Institutes <strong>of</strong> Health Informaticswww.nihi.caProvincial Health Ethics Networkwww.phen.ab.caReach Trainingwww.reachtraining.caSelkirk <strong>College</strong> – School <strong>of</strong> Health & HumanServiceswww.selkirk.ca/hhsUBC Interpr<strong>of</strong>essional Continuing Educationwww.interpr<strong>of</strong>essional.ubc.caication Forms & FAQ’s atTION.CLPNA.COMCLPNA.com or 780-484-8886regor Education Foundation for LPNs30 care | volume 27 issue 1
the operations roomMember Information - <strong>College</strong> Activity - Best PracticesSpecial Event Kits available forNational Nursing Week – May 6-12Planning an event for National Nursing Week?Hundreds <strong>of</strong> events will be held throughout <strong>Alberta</strong> during NationalNursing Week, May 6-12, and once again, the CLPNA is supportingthese celebrations with complimentary Special Event Kits. SpecialEvent Kits contain LPN-branded items, such as lip balms, pens, bags,etc., for distribution to LPNs as door prizes or other gifts at theseevents.National Nursing Week is an opportunity for nurses, their employersand the public to stop, reflect and celebrate the contribution <strong>of</strong> thenursing pr<strong>of</strong>ession.In 1971, the International Council <strong>of</strong> <strong>Nurses</strong> (ICN) designated May12 – Florence Nightingale’s birthday – as International <strong>Nurses</strong> Day.In 1985, in recognition <strong>of</strong> the dedication and achievements <strong>of</strong> thenursing pr<strong>of</strong>ession, the Canadian minister <strong>of</strong> health proclaimed thesecond week <strong>of</strong> May as National <strong>Nurses</strong> Week.Special Event Kits are available on a first-come, first-serve basis.Product type and number <strong>of</strong> items in each Kit depends on thenumber <strong>of</strong> expected LPN attendees and number <strong>of</strong> requests receivedby CLPNA. NOTE: There is no guarantee <strong>of</strong> receiving one item perattendee.Special Event Kit Request Forms are available fromwww.clpna.com or by contacting info@clpna.com or 780-484-8886.Request Deadline is April 5 with delivery <strong>of</strong> packages in mid-April.Council Welcomes NEW Public MemberOn January 23, 2013, a Government <strong>of</strong> <strong>Alberta</strong> Order <strong>of</strong> Council appointed Gary Christophersonto a three-year term as a public member to the Council <strong>of</strong> the <strong>College</strong> <strong>of</strong> <strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong><strong>of</strong> <strong>Alberta</strong> (CLPNA). Christopherson has extensive board experience and a Masters in PublicAdministration. His background includes business economic development, marketing and innovation.The Health Pr<strong>of</strong>essions Act requires the provincial government to appoint public representatives to sit onCLPNA Council to represent the views <strong>of</strong> the people <strong>of</strong> <strong>Alberta</strong>.clpna.comcare | spring 2013 31
the operations roomA Massive NewData Tool for LPNs– an itty-bitty USB keyAre you tired <strong>of</strong> packing around your Continuing CompetencyProgram (CCP) Binder? Are you ready to start tracking and usingelectronic tools to track your pr<strong>of</strong>essional practice?Well it’s here!! A new tool for LPNs to manage and maintain all the ‘nitty-gritty’ pr<strong>of</strong>essionalinformation you need in one place…an itty bitty USB key – the “LPN Key to Self-Regulation”The Key is a convenient 4GB USB that includes dozens <strong>of</strong> <strong>Alberta</strong> LPN legislative and resource documents suchas <strong>Alberta</strong> Legislation & Regulation; Code <strong>of</strong> Ethics and Standards <strong>of</strong> Practice; and <strong>Alberta</strong> LPN CompetencyPr<strong>of</strong>ile.The “LPN Key to Self-Regulation” (LPN Key) is a portable way to carry and consult documents that, until now,were only available in the CLPNA’s 400-page Continuing Competency Program (CCP) Binder or in variouslocations at www.clpna.com. The LPN Key contains more information than the CCP Binder, and is easily updatedby downloading online documents. For the convenience <strong>of</strong> members, some documents are included in Wordformat, such as the “Record <strong>of</strong> Pr<strong>of</strong>essional Activities” where personal continuing education info can be enteredand saved.New CLPNA applicants receive the “LPN Key to Self-Regulation” as part <strong>of</strong> the initial registration process.The Key is available for current members to purchase for $30.Get Ready!You maybe Chosenthis yearContinuing Competency Program Validation 2013Each year in June, approximately 20% <strong>of</strong> eligible membership is randomly selected toparticipate in the Continuing Competency Program Validation (CCPV).If you are chosen to participate, you will be required to validate your learning forthe previous two years by completing an online CCPV submission. Through selfassessment,reflection and/or peer review you will verify how this learning hasenhanced your knowledge and competence in your pr<strong>of</strong>essional practice.It is possible to be chosen for CCPV every year through the random selection process.To be prepared, CLPNA recommends that you keep track <strong>of</strong> your learning. Tracking iseasy using the CLPNA Record <strong>of</strong> Pr<strong>of</strong>essional Activities or other organized method.Any learning that applies to your practice as an LPN is applicable to the CCP andCCPV, whether you complete a certificate course, read a best practice article, orresearch pertinent information online (a list <strong>of</strong> suggested learning activities can befound at www.clpna.com).Get ready for CCPV - Don’t delay! Organize today. Be prepared.You may be a “chosen one”.32 care | volume 27 issue 1
the operations roomCLPNA CouncilNominations OpenFirst Co-Worker Abuse SurveyGathers Data; EducatesThe first survey regarding the experience <strong>of</strong>intimidation and bullying in the workplace from theperspective <strong>of</strong> LPNs in <strong>Alberta</strong> was conducted inFebruary. The confidential “Co-Worker Abuse Survey”was completed by approximately 1000 CLPNAmembers.Besides gaining insight into negative workplaceinteraction, the Survey included an educationcomponent related to the variety <strong>of</strong> terms andbehaviours that describe bullying and other forms <strong>of</strong>abusive behaviour. This behaviors include: sarcasm;rolling the eyes; raising eyebrows; using an aggressiveor intimidating tone <strong>of</strong> voice (vocal intonation); makingfun <strong>of</strong> or humiliating the nurse; running the nurse downbehind her back; ignoring the nurse’s requests for help;criticizing the nurse in front <strong>of</strong> colleagues, patientsand families; isolating the nurse from social or workactivities; directing pr<strong>of</strong>anities or other unwelcomecomments <strong>of</strong> a racial, sexual, age or religious natureto the nurse; any other form <strong>of</strong> perceived verbal oremotional abuse toward a nursing colleague.Additionally, questions were asked about witnessingand experiencing abusive behavior, and on reportingabusive behaviour and deterrents.Initial data collection indicates a high majority <strong>of</strong> thesurvey respondents have seen or experienced bullying inits multiple forms, it is highly under-reported due to fear,intimidation and concern that nothing would be doneanyway, and there is a lack <strong>of</strong> individual pr<strong>of</strong>essionalconfidence in managing an abusive situation.The survey results will inform the upcoming PracticeGuideline on “Addressing Co-Worker Abuse Among<strong>Nurses</strong> in the Workplace”, set for release in Spring2013, and be used as part on ongoing dialoguebetween CLPNA and stakeholders. CLPNA will alsobe presenting the new Practice Guideline and surveyresults at the upcoming Spring Conference.An opportunity to guide the pr<strong>of</strong>ession as a member <strong>of</strong> theCouncil <strong>of</strong> the <strong>College</strong> <strong>of</strong> <strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong> <strong>of</strong><strong>Alberta</strong> (CLPNA) comes available in March with the opening<strong>of</strong> nominations for District Representatives.Members residing in Districts 2, 4, 6 or 7 are invited to let theirname stand in the June Election for the September 2013 toAugust 2015 term. Nomination Packages must be submitted byMay 31, 2013. In June, LPNs in the election Districts will selecttheir representative by electronic ballot.The Council is responsible for the overall general direction <strong>of</strong>the CLPNA and through Policy Governance, the Council isresponsible for:• establishing, maintaining and monitoring Bylaws,Regulations, Standards <strong>of</strong> Practice, and Code <strong>of</strong> Ethics and• approving practical nurse education programsThe Council does not manage the day-to-day operations <strong>of</strong> theCLPNA, which is administered by the Executive Director andstaff.Council members attend one to two day meetings quarterly toreview reports <strong>of</strong> <strong>College</strong> business and plan upcoming goals, fora total <strong>of</strong> 10 days attendance per year. Travel expenses and anhonorarium for meeting attendance is provided.2013 ELECTION DISTRICTS:675432Nomination Packages1DISTRICT 2:CALGARY ZONE(Calgary & area)DISTRICT 4:EDMONTON ZONE(Edmonton & area)DISTRICT 6:PART OF NORTH ZONE(Grande Prairie & area)DISTRICT 7:PART OF NORTH ZONE(Fort McMurray & area)Job Descriptions, Nomination Packages and information to findyour Election District are available on www.clpna.com under“About CLPNA”, “Council”. Or contact the CLPNA <strong>of</strong>fice at info@clpna.com, or 780-484-8886 or 1-800-661-5877 (toll free in<strong>Alberta</strong>).care | spring 2013 33
the operations roomMATTERSCONDUCTWhat is Abandonment <strong>of</strong> Care?Joyce was scheduled to work a 12hour dayshift at the Regional Hospital.When Joyce arrived for her scheduled shift, she was upset and tired. Mid-waythrough the morning, Joyce and a co-worker engaged in a heated argumentat the nursing station. Joyce walked away crying and abruptly left the unitwithout informing anyone.Has Abandonment <strong>of</strong> Care occurred?Like Joyce, other nurses may find themselves in a similar situation where theyhave made a decision which could potentially compromise client care. Is itconsidered Abandonment <strong>of</strong> Care since Joyce left the unit because she was inan emotional state?To fully answer this question, it is important to examine the meaning <strong>of</strong> Abandonment<strong>of</strong> Care and how it applies to your nursing practice. According tothe CLPNA’s Practice Statement 13: Abandonment <strong>of</strong> Care, the definition is:For abandonment <strong>of</strong> care to occur, the <strong>Licensed</strong> <strong>Practical</strong> Nurse (LPN)must have:a. Accepted the client assignment, thus establishing a nurse-clientrelationship, and thenb. Severed that nurse-client relationship without giving reasonablenotice to the appropriate person (e.g., employer, supervisor) so thatarrangements can be made for continuation <strong>of</strong> nursing care byothers.A nurse-client relationship begins when the LPN accepts the careassignment. Abandonment <strong>of</strong> care occurs when the LPN leaves theclient assignment without transferring client care and / orcommunicating information to an appropriate caregiver.*This feature is intended toenlighten LPNs in conductrelatedconcerns throughfictionalized case studies.Any information associatedto real people or actualevents has been changed,however the context <strong>of</strong> thecase study representsreal life situations.When an LPN accepts a client assignment a nurse-client relationship is established.When the assignment is accepted a transfer <strong>of</strong> care is required; thisoccurs when either a written or oral report is given between qualified healthcare providers. This report includes information surrounding the client(s) andtheir needs. When transfer <strong>of</strong> care occurs, it is the LPN’s pr<strong>of</strong>essional responsibilityto provide care that will fulfill the client’s needs.Go back and review the scenario and ask yourself did Joyce abandon careaccording to the definition? The answer is “Yes”. Joyce left the unit abruptlywithout reasonable notice or explanation or giving report to another qualifiedhealth care provider to ensure continuous nursing care was provided to herclient(s). In the scenario, Joyce has not met her pr<strong>of</strong>essional obligation to herclient(s) and her co-workers. “Abandonment <strong>of</strong> Care” has occurred.As a LPN, it is important to recognize your pr<strong>of</strong>essional responsibilities tomake a suitable decision that promotes safe and competent care. It is essentialfor an LPN to be aware and understand situations that constitute “Abandonment<strong>of</strong> Care”. Situations include:• Leaving abruptly, in the absence <strong>of</strong> a reasonable explanation, with>care | spring 2013 35
the operations roomout giving the employer or supervisoradequate notice for replacingthe LPN.• Leaving without reporting to the oncoming shift.• Accepting a client care assignmentand then leaving without notifyingthe appropriate person(s).• Sleeping during an unscheduledbreak; thus, being unavailable toassigned clients.If an employer disciplines an LPN for abandoningcare, they are obligated to report the matter toCLPNA. CLPNA is charged with the responsibility<strong>of</strong> protecting the public from unethical, unskilled orunsafe nursing practice. In doing so, a complaint <strong>of</strong>this nature is processed in accordance with Part 4 <strong>of</strong>the Health Pr<strong>of</strong>essions Act. This includes completingan objective investigation to determine if “Abandonment<strong>of</strong> Care” has occurred.If the Complaints Director finds evidence to determineabandonment <strong>of</strong> care has occurred, the mattercan be referred to hearing. During the hearingprocess, the Hearing Tribunal will consider whetherthere is sufficient evidence to prove unpr<strong>of</strong>essionalconduct as defined in Section 1(1)(pp) <strong>of</strong> the HealthPr<strong>of</strong>essions Act. The Hearing Tribunal can determineif the conduct displays <strong>of</strong> a lack <strong>of</strong> knowledgeor skill or judgment and/or contravenes the Code<strong>of</strong> Ethics, Standards <strong>of</strong> Practice, other relevant legislation;or if the conduct harms the integrity <strong>of</strong> theregulated pr<strong>of</strong>ession.If the Hearing Tribunal determines the LPN did infact abandon care and the conduct is proven to beunpr<strong>of</strong>essional, the next step in the process is for theHearing Tribunal to consider the appropriate penaltyto address the conduct. The types <strong>of</strong> penalty ordersthat are considered include, but are not limitedto, any <strong>of</strong> the following: hearing cost, fines, reflectivepapers, reprimand, caution, publication (CAREmagazine), and remedial education. nResources –• Practice Statement 13: Abandonment <strong>of</strong> Care• CLPNA Code <strong>of</strong> Ethics and Standards <strong>of</strong> Practice• Health Pr<strong>of</strong>essions ActIn future fictionalized stories, we’ll share other commonexamples <strong>of</strong> the wide range <strong>of</strong> behaviours and situationswhich may be reported to CLPNA’s Conduct Department.Accepting Donationsfor Silent AuctionFundraiserIndividuals and businesses can support <strong>Licensed</strong><strong>Practical</strong> <strong>Nurses</strong> and their on-going post-basiceducation by donating goods or services to thelargest fundraising event <strong>of</strong> the year, the SilentAuction held April 17-18 at the 2013 CLPNA SpringConference in Banff. Over 350 enthusiastic attendeesparticipate in the annual Silent Auction held by theFredrickson-McGregor Education Foundation forLPNs. This year, attendees will have more time to seeand bid on the items because, for the first time, theAuction will be held over two days from April 17 at8:45pm to April 18 at 3pm.Popular donations items include garden/yardaccessories, handcrafted items, jewellery, giftcertificates, gift baskets, and electronics. To donate,contact the Foundation for a Donation Form atfoundation@clpna.com or 780-484-8886. Donationswill be accepted at the CLPNA <strong>of</strong>fice until April 10,and at the Spring Conference’s Registration Desk onApril 17 after 4pm.In 2012, the Foundation raised $6470 through theevent. Proceeds are distributed through educationgrants to eligible <strong>Alberta</strong> LPNs.The Fredrickson-McGregor Education Foundation forLPNs is a non-pr<strong>of</strong>it that provides educational grants,awards and bursaries to CLPNA members to enhancetheir nursing knowledge, skills and ability, and honortheir achievements.36 care | volume 27 issue 1
membership9.8%103418.0%1919 14.8%1575 11.8%1256 10.9%9.1%11629649.2%9808.0%8508.4%883statistics2012 CLPNA Registration Data19-25 26-30 31-35 36-40 41-45 46-50 51-55 56-60 61-65+AGE GROUPSRegistrations2011 2012<strong>Alberta</strong> NEW Graduate Applicants 769 938International NEW Applicants 40 40Other Canadian NEW Applicants 442 580Reinstatements (Less than 4 Years) - 305Reinstatements (More than 4 Years) - 15Re-Entry LPNs 1 5Renewals 8400 8740Courtesy Applicants 0 0TOTAL 9652 10623LPN GenderDistributionAge <strong>of</strong> Active LPNs93.5%Average Age: 2010 - 41.42011 - 41.12012 - 40.76.5%9.8%103418.0%1919 14.8%1575 11.8%1256 10.9%1162LPN Registration Trends2012201120102009200820072006200520042003200220012000199919981997199619951994199319921991199019891988198719869.1%9649.2%9808.0%8508.4%88319-25 26-30 31-35 36-40 41-45 46-50 51-55 56-60 61-65+AGE GROUPSNumber<strong>of</strong> LPNs1062396529015853178597264686365336037557551724848443143424606472349635562619663786545665167366956722578948643Percentage <strong>of</strong>Loss/Increase10.0%7.0%5.7%8.6%8.1%5.8%5.0%8.2%8.3%7.8%6.7%9.4%2.0%-5.7%-2.5%-4.8%-10.8%-10.0%-2.9%-2.6%-1.6%-1.3%-3.2%-3.7%-8.5%-8.7%Out <strong>of</strong> Province& InternationalRegistrations60141348262053 34 411998 1999 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012BC|304SK|16MN|1074 90 80 81ON|204QC|812420524729820122011YEAR 20102009In Migration Breakdown 2008200720062005200420032002NB NS PEI NL NT YK NU USA2001| | | | | | | |13 16 0 8 1 2000 0 0 311999*Jamaica TOTAL - 6201998199719961995OTHER*|9Distribution <strong>of</strong> Active LPNs*Number<strong>of</strong> LPNs106239652AHS AreaArea 0 - Out <strong>of</strong> Province/CountryArea 1 - South Zone (Lethbridge & Medicine Hat)Totals681904% 90156.4% 85318.5% 78597264Area 2 - Calgary Zone 2754 25.9%6863Area 3 - Central Zone (Red Deer) 1508 14.2%6533Area 4 - Edmonton Zone 3626 34.1%6037Area 5 - North Zone 1150 10.9%55755172*By LPN mailing addressTOTAL 106234431434246064723100%4848care -4.8% | spring 2013 3749635562Percentage <strong>of</strong>Loss/Increase10.0%7.0%5.7%8.6%8.1%5.8%5.0%8.2%8.3%7.8%6.7%9.4%2.0%-5.7%-2.5%-10.8%-10.0%
the operations roomCLPNA CouncilPresidentJo-Anne Macdonald-WatsonExecutive Director/RegistrarLinda Stangerlstanger@clpna.comDistrict 1 (South Zone)Carla KoyataDistrict 2 (Calgary Zone)Linda CoatsworthDistrict 3 (Central Zone)Valerie PaiceDistrict 4 (Edmonton Zone)Joshua MartynuikDistrict 5 (Part <strong>of</strong> North Zone)Doris KuelkenDistrict 6 (Part <strong>of</strong> North Zone)Roberta BeaulieuDistrict 7 (Part <strong>of</strong> North Zone)Dieda JohnPublic MembersGary Christopherson / Allan BuckRalph WestwoodTo contact Council members please call the CLPNA<strong>of</strong>fice and your message will be forwarded to them.CLPNA StaffTamara RichterDirector <strong>of</strong> Operationstrichter@clpna.comTeresa BatemanDirector <strong>of</strong> Pr<strong>of</strong>essional Practicetbateman@clpna.comSharlene StandingDirector <strong>of</strong> Regulatory Servicessstanding@clpna.comLinda FindlayPractice Consultant/CCPlfindlay@clpna.comSandy Davis / Susan BlatzComplaints Consultantssdavis@clpna.com / sblatz@clpna.comOUR MISSIONTo lead and regulate the pr<strong>of</strong>ession in a manner thatprotects and serves the public throughexcellence in <strong>Practical</strong> Nursing.OUR VISION<strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong> are a nurse <strong>of</strong> choice, trustedpartner and a valued pr<strong>of</strong>essional in the healthcare system.The CLPNA embraces change that serves the best interests <strong>of</strong>the public, the pr<strong>of</strong>ession and a quality healthcare system.By 2015, the CLPNA expects to see:• Increased demand for <strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong>generating continuous growth in the pr<strong>of</strong>ession.• Full utilization <strong>of</strong> <strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong> throughout thehealth care system.• All <strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong> embrace and fully enact theirpr<strong>of</strong>essional scope <strong>of</strong> practice.• Increased public understanding <strong>of</strong> the role andcontributions <strong>of</strong> <strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong>.• The <strong>College</strong> initiate and support research relevant to the<strong>Licensed</strong> <strong>Practical</strong> Nurse pr<strong>of</strong>ession and health care system• Enhanced collaborative opportunities provincially, nationallyand internationally.• The <strong>College</strong> and <strong>Licensed</strong> <strong>Practical</strong> <strong>Nurses</strong> fully engagedin all decisions affecting the pr<strong>of</strong>ession.COLLEGE OF LICENSED PRACTICAL NURSES OF ALBERTALog Onto clpna.com38 care | volume 27 issue 1• CLPNA Publications• Learning Modules• Competency Pr<strong>of</strong>ile• Job Listings• 2011 Annual Reportand more…CLPNA Office HoursRegular Office HoursMonday to Friday8:30am to 4:30pmClosed forStatutory Holidays
Step Forwardwith NorQuest <strong>College</strong>Explore the continuing education opportunitieswith courses designed specifically for LPNs.You have lots <strong>of</strong> choices:• Advanced Education in Orthopaedics for LPNs Certificate• Adult Health Assessment (AHAN 1000)• Infusion Therapy (IVTH 1010)• Math Refresher for Medication Administration(MRMA 1000)• Medical Administration – IM/ID (MEDA 1001)• Insertion <strong>of</strong> a Nasogastric Tube (NASO 1000)• Pharmacology Therapeutics and MedicationAdministration (PTMA 1000)• Urinary Catheterization and Bladder Irrigation (UCBI 1000)• Wound Care – Using a Standard Approach (WCSA 1001)Find out more today!LPN.ConEd@norquest.ca | 780.644.6470For information about orthopaedic classes, please contact:ortho@norquest.ca | 780.644.6366To register, call 780.644.6000 or toll-free 1.866.534.7218www.norquest.caProud supporter <strong>of</strong> thecare | spring 2013 39
ISSN 1920-633X CAREPublications Mail AgreementNumber 40050295St. Albert Trail Place, 13163 - 146 Street Edmonton, <strong>Alberta</strong> T5L 4S8Telephone (780) 484-8886 Toll Free 1-800-661-5877 Fax (780) 484-9069Return Undeliverable Canadian Addresses To:St. Albert Trail Place, 13163 - 146 StreetEdmonton, <strong>Alberta</strong> T5L 4S8email: care@clpna.comwww.clpna.comSee theConference onFacebook & Twitter(#ABLPN)2013 CLPNA SPRING CONFERENCEApril 17-19, 7 19 2013Rimrock Resort Hotel - Banff, , <strong>Alberta</strong>bApply plyfor $100 OffYour ur Registration gtioFeemore info online.www.clpnaconference.comw coe nce.comn